Threat of Antimicrobial Resistance among Pilgrims with Infectious Diseases during Hajj: Lessons Learnt from COVID-19 Pandemic
Abstract
1. Introduction
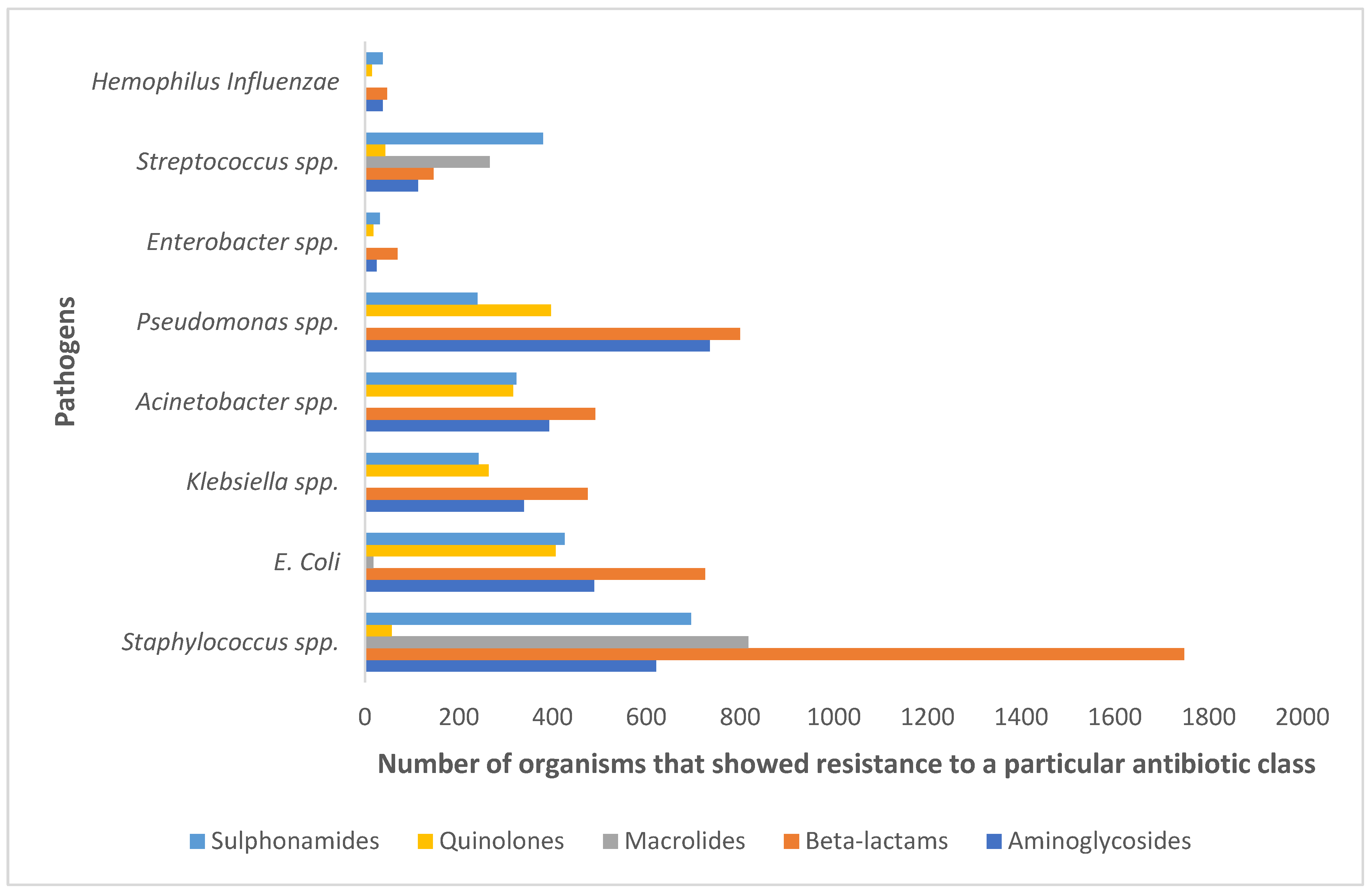
2. Results and Discussion
2.1. Pattern and Prevalence of Infectious Diseases during Hajj
2.2. Patterns of Antimicrobial Use among Hajj Pilgrims
| Author Year | Study Population (N) | Study Design | Prevalence of Antimicrobial Use | Top 3 Antimicrobials | Findings | ||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | |||||
| Harimurti et al., 2021 [100] | Indonesian pilgrims (N = 813) | Prospective longitudinal study | 47.8% | - | - | - | Pneumococcal vaccine should be administered before departure to KSA. |
| Alahmadi et al., 2020 [97] | Pilgrims from 7 different countries (N = 675) | Prospective point prevalence survey | 49.18% | Penicillin (20%) | Amoxiclav (12%) | Pipercillin-tazobactum (88.0%) | The rational use of antimicrobial should be assessed by standardized methodology. |
| Hoang et al., 2019 [96] | French pilgrims (N = 783) | Prospective cohort study | 47.6% | Beta-lactams (35.0%) | Macrolides (11.4%) | Cephalosporins (2.3%) | Educational training and sessions are required to control the irrational use of antimicrobials. |
| Alqahtoni et al., 2019 [101] | Pilgrims (N = 344) | Cross-sectional study | 6% | - | - | - | Pre-travel education training related with health and use of preventive measure should be addressed. |
| Dzaralay et al., 2017 [98] | Malaysian Pilgrims (N = 91) | Cross-sectional study | 100% | Levofloxacin (44%) | Azithromycin (40.7%) | Cefuroxime (23.1%) | The proper guidelines regarding antimicrobial use for the pilgrims with CAP should be introduced to improve healthcare services during Hajj. |
| Hashim et al., 2016 [70] | Malaysian pilgrims (N = 468) | Cross-sectional study | 61.8% | - | - | - | Preventive measures including social distancing, wearing face mask, hand hygiene should be practice to prevent the spread of infectious diseases. |
| Metanat et al., 2015 [94] | Irani pilgrims (N = 422) | Prospective, cross-sectional study | 58.5% | - | - | - | The meningococcal vaccine was effective in reducing the number of carriers among pilgrims after travel. |
| Azeem et al., 2014 [92] | Australian pilgrims (N = 229) | Cross-sectional study | 34.9% | - | - | - | Educational sessions and campaign regarding rational use of antimicrobials is required. |
| Alborzi et al., 2008 [102] | Irani pilgrims (N = 674) | - | 58.2% | - | - | - | The administration of vaccine was effective for reduction the number of carriers among pilgrims. |
| Mustafa et al., 2003 [93] | Malaysian pilgrims (N = 820) | Cohort study | 84% | - | - | - | Immunization programs for Hajj pilgrims should be supported by KSA government |
| Qureshi et al., 2000 [95] | Pakistani pilgrims (N = 100) | Randomized blinded study | 17% | - | - | - | Influenza vaccination should be recommended for the pilgrims before arrival to KSA. |
2.3. Interventions and Recommendations
2.3.1. Local and International Guidelines and Policies for Infection Prevention and Control
2.3.2. Restricting the Number of Hajj Pilgrims
2.3.3. Provision and Implementation of Adequate Healthcare Services
Vaccination
Hand Hygiene
Social Distancing and Contact Avoidance
Face Masks
2.4. Impact of Antibiotic Prescribing Patterns during the COVID-19 Pandemic on AMR
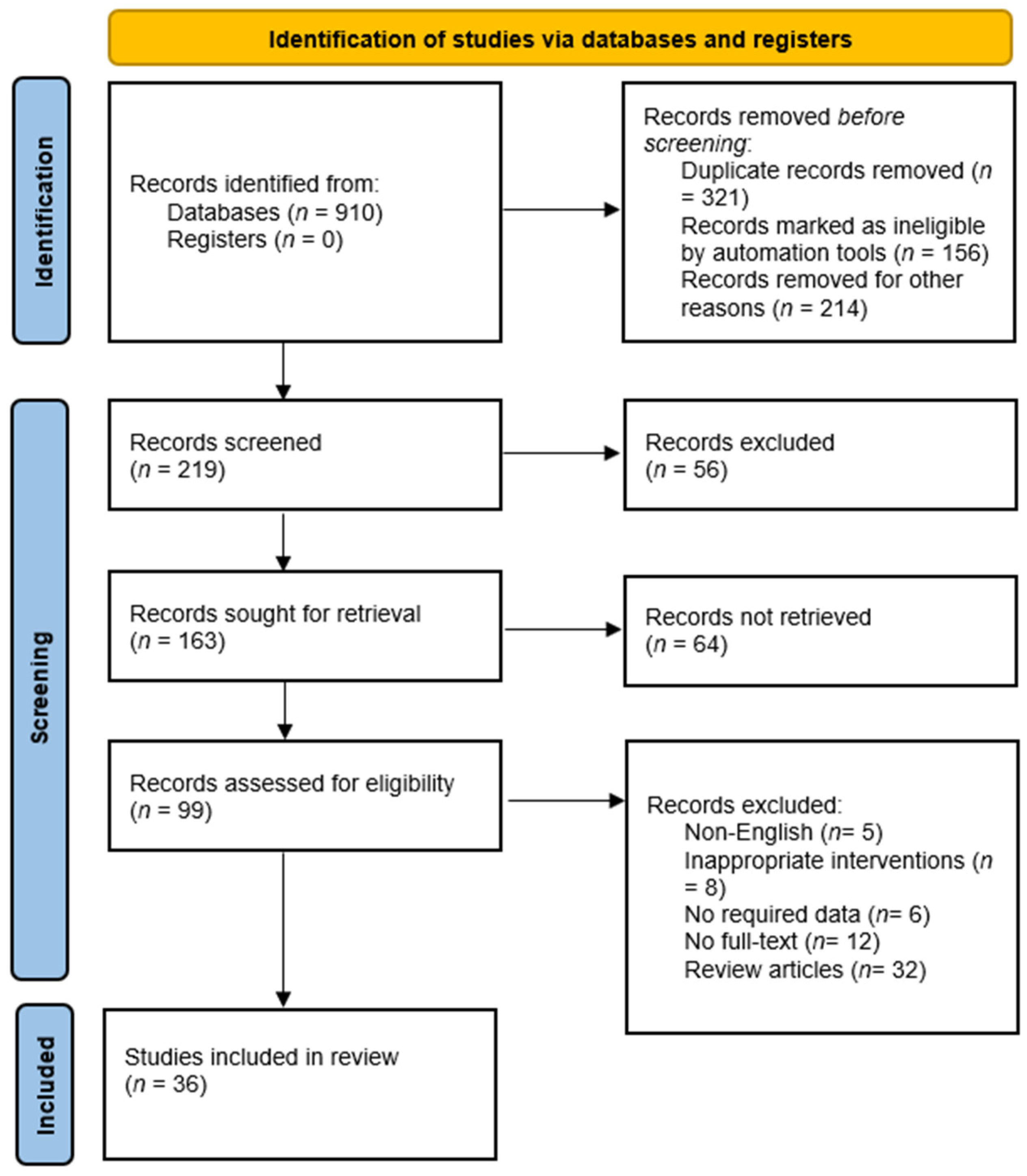
3. Materials and Methods
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yezli, S.; Alotaibi, B.M. Mass gatherings and mass gatherings health. Saudi Med. J. 2016, 37, 729. [Google Scholar] [CrossRef] [PubMed]
- Coltart, C.E.; Behrens, R.H. The new health threats of exotic and global travel. Br. J. Gen. Pr. 2012, 62, 512–513. [Google Scholar] [CrossRef] [PubMed]
- Saleem, Z.; Hassali, M.A. Travellers take heed: Outbreak of extensively drug resistant (XDR) typhoid fever in Pakistan and a warning from the US CDC. Travel Med. Infect. Dis. 2019, 27, 127. [Google Scholar] [CrossRef] [PubMed]
- Hoang, V.-T.; Gautret, P. Infectious diseases and mass gatherings. Curr. Infect. Dis. Rep. 2018, 20, 44. [Google Scholar] [CrossRef]
- Bokhary, H.; Rashid, H.; Hill-Cawthorne, G.A.; Abd El Ghany, M. The rise of antimicrobial resistance in mass gatherings. In Handbook of Healthcare in the Arab World; Springer: Berlin/Heidelberg, Germany, 2021; pp. 1199–1214. [Google Scholar]
- Shafi, S.; Azhar, E.; Al-Abri, S.; Sharma, A.; Merali, N.; Al-Tawfiq, J.A.; El-Kafrawy, S.A.; Zumla, A.; Lee, S.S. Infectious diseases threats at the Arba’een–a neglected but one of the largest annually recurring mass gathering religious events. Int. J. Infect. Dis. 2022, 123, 210–211. [Google Scholar] [CrossRef]
- Lami, F.; Amiri, M.; Majeed, Y.; Barr, K.M.; Nsour, M.A.; Khader, Y.S. Real-time surveillance of infectious diseases, injuries, and chronic conditions during the 2018 Iraq Arba’een mass gathering. Health Secur. 2021, 19, 280–287. [Google Scholar] [CrossRef]
- Sweileh, W.M. Health-related research publications on religious mass gatherings of Muslims: A bibliometric analysis (1980–2020). Trop. Dis. Travel Med. Vaccines 2022, 8, 1. [Google Scholar] [CrossRef]
- Alshammari, S.M.; Gwalani, H.; Helsing, J.E.; Mikler, A.R. Disease spread simulation to assess the risk of epidemics during the global mass gathering of Hajj pilgrimage. In Proceedings of the 2019 Winter Simulation Conference (WSC), National Harbor, MD, USA, 8–12 December 2019; pp. 215–226. [Google Scholar]
- Haseeb, A.; Faidah, H.S.; Bakhsh, A.R.; Malki, W.H.A.; Elrggal, M.E.; Saleem, F.; Rahman, S.u.; Khan, T.M.; Hassali, M.A. Antimicrobial resistance among pilgrims: A retrospective study from two hospitals in Makkah, Saudi Arabia. Int. J. Infect. Dis. 2016, 47, 92–94. [Google Scholar] [CrossRef]
- Haseeb, A.; Faidah, H.S.; Algethamy, M.; Alghamdi, S.; Alhazmi, G.A.; Alshomrani, A.O.; Alqethami, B.R.; Alotibi, H.S.; Almutiri, M.Z.; Almuqati, K.S. Antimicrobial Usage and Resistance in Makkah Region Hospitals: A Regional Point Prevalence Survey of Public Hospitals. Int. J. Environ. Res. Public Health 2022, 19, 254. [Google Scholar] [CrossRef]
- Memish, Z.A.; Stephens, G.M.; Steffen, R.; Ahmed, Q.A.J.T.L.i.d. Emergence of medicine for mass gatherings: Lessons from the Hajj. Lancet Infect. Dis. 2012, 12, 56–65. [Google Scholar] [CrossRef]
- Haseeb, A.; Faidah, H.S.; Al-Gethamy, M.; Iqbal, M.S.; Barnawi, A.M.; Elahe, S.S.; Bukhari, D.N.; Noor Al-Sulaimani, T.M.; Fadaaq, M.; Alghamdi, S. Evaluation of a Multidisciplinary Antimicrobial Stewardship Program in a Saudi Critical Care Unit: A Quasi-Experimental Study. Front. Pharmacol. 2021, 11, 2222. [Google Scholar] [CrossRef]
- Haseeb, A.; Faidah, H.S.; Al-Gethamy, M.; Iqbal, M.S.; Alhifany, A.A.; Ali, M.; Abuhussain, S.S.A.; Elrggal, M.E.; Almalki, W.H.; Alghamdi, S.; et al. Evaluation of Antimicrobial Stewardship Programs (ASPs) and their perceived level of success at Makkah region hospitals, Kingdom of Saudi Arabia. Saudi Pharm. J. 2020, 28, 1166–1171. [Google Scholar] [CrossRef]
- Degeling, C.; Johnson, J.; Kerridge, I.; Wilson, A.; Ward, M.; Stewart, C.; Gilbert, G. Implementing a One Health approach to emerging infectious disease: Reflections on the socio-political, ethical and legal dimensions. BMC Public Health 2015, 15, 1307. [Google Scholar] [CrossRef]
- Saleem, Z.; Godman, B.; Azhar, F.; Kalungia, A.C.; Fadare, J.; Opanga, S.; Markovic-Pekovic, V.; Hoxha, I.; Saeed, A.; Al-Gethamy, M. Progress on the national action plan of Pakistan on antimicrobial resistance (AMR): A narrative review and the implications. Expert Rev. Anti-Infect. Ther. 2022, 20, 71–93. [Google Scholar] [CrossRef]
- Memish, Z.A.; Steffen, R.; White, P.; Dar, O.; Azhar, E.I.; Sharma, A.; Zumla, A. Mass gatherings medicine: Public health issues arising from mass gathering religious and sporting events. Lancet 2019, 393, 2073–2084. [Google Scholar] [CrossRef]
- Mantoro, T.; Aris, M.F.M.; Ayu, M.A. Hajjlocator: A hajj pilgrimage tracking framework in crowded ubiquitous environment. In Proceedings of the 2011 International Conference on Multimedia Computing and Systems, Ouarzazate, Morocco, 7–9 April 2011; pp. 1–6. [Google Scholar]
- Goni, M.D.; Hasan, H.; Wan-Arfah, N.; Naing, N.N.; Deris, Z.Z.; Arifin, W.N.; Baaba, A.A.; Aliyu, A.; Adam, B.M.J.F.i.p.h. Health Education Intervention as an Effective Means for Prevention of Respiratory Infections Among Hajj Pilgrims: A Review. Front. Public Health 2020, 8, 449. [Google Scholar] [CrossRef]
- Shafi, S.; Dar, O.; Khan, M.; Khan, M.; Azhar, E.I.; McCloskey, B.; Zumla, A.; Petersen, E. The annual Hajj pilgrimage—Minimizing the risk of ill health in pilgrims from Europe and opportunity for driving the best prevention and health promotion guidelines. Int. J. Infect. Dis. 2016, 47, 79–82. [Google Scholar] [CrossRef]
- Razavi, S.M.; Mardani, M.; Salamati, P. Infectious Diseases and Preventive Measures During Hajj Mass Gatherings: A Review of the Literature. Arch. Clin. Infect. Dis. 2018, 13, e62526. [Google Scholar] [CrossRef]
- Almeleebia, T.M.; Alhifany, A.A.; Almutairi, F.; Alshibani, M.; Alhossan, A.M. Regulating antimicrobial sales in Saudi Arabia: Achievements and challenges. Int. J. Clin. Pract. 2021, 75, e13833. [Google Scholar] [CrossRef]
- Petersen, E.; Memish, Z.A.; Zumla, A.; Al Maani, A. Transmission of respiratory tract infections at mass gathering events. Curr. Opin. Pulm. Med. 2020, 26, 197–202. [Google Scholar] [CrossRef]
- Yezli, S.; Shibl, A.M.; Livermore, D.M.; Memish, Z.A. Prevalence and antimicrobial resistance among Gram-negative pathogens in Saudi Arabia. J. Chemother. 2014, 26, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Hadi, M.A.; Karami, N.A.; Al-Muwalid, A.S.; Al-Otabi, A.; Al-Subahi, E.; Bamomen, A.; Mohamed, M.M.A.; Elrggal, M.E. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): A cross-sectional survey in Makkah Province, Saudi Arabia. Int J Infect Dis. 2016, 47, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Zowawi, H.M.; Balkhy, H.H.; Walsh, T.R.; Paterson, D.L. β-Lactamase production in key gram-negative pathogen isolates from the Arabian Peninsula. Clin. Microbiol. Rev. 2013, 26, 361–380. [Google Scholar] [CrossRef] [PubMed]
- Leangapichart, T.; Rolain, J.-M.; Memish, Z.A.; Al-Tawfiq, J.A.; Gautret, P. Emergence of drug resistant bacteria at the Hajj: A systematic review. Travel Med. Infect. Dis. 2017, 18, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Yousef, S.A.; Mahmoud, S.Y.; Eihab, M.T. Prevalence of methicillin-resistant Staphylococcus aureus in Saudi Arabia: Systemic review and meta-analysis. Afr. J. Clin. Exp. Microbiol. 2013, 14, 146–154. [Google Scholar] [CrossRef][Green Version]
- Nazeer, A.; Al-Tawfiq, J.A. Methicillin-resistant Staphylococcus aureus metrics for patients in Saudi Arabia. J. Infect. Dev. Ctries. 2012, 6, 223–233. [Google Scholar] [CrossRef][Green Version]
- Memish, Z.A.; Zumla, A.; Alhakeem, R.F.; Assiri, A.; Turkestani, A.; Al Harby, K.D.; Alyemni, M.; Dhafar, K.; Gautret, P.; Barbeschi, M.J.T.L. Hajj: Infectious disease surveillance and control. Lancet 2014, 383, 2073–2082. [Google Scholar] [CrossRef]
- Alotaibi, B.M.; Yezli, S.; Bin Saeed, A.-A.A.; Turkestani, A.; Alawam, A.H.; Bieh, K. Strengthening health security at the Hajj mass gatherings: Characteristics of the infectious diseases surveillance systems operational during the 2015 Hajj. J. Travel Med. 2017, 24, taw087. [Google Scholar] [CrossRef]
- Gautret, P.; Benkouiten, S.; Al-Tawfiq, J.A.; Memish, Z.A. The spectrum of respiratory pathogens among returning Hajj pilgrims: Myths and reality. Int. J. Infect. Dis. 2016, 47, 83–85. [Google Scholar] [CrossRef]
- Ameen, L.; Assaggaf, H.; Alsafi, R.; Minshawi, F.; Alghamdi, S.; Alharbi, A.; Qashqaric, F.; Makhdoomd, H.; Refaata, B.; Alsaife, B.; et al. Analysis of the Clinical Characteristics of COVID-19 Patient Severity Amongst Saudi Hospital Admission in 2020. Journal of Umm Al-Qura University for Medical Sciences. J. Umm Al-Qura Univ. Med. Sci. 2022, 8, 18–23. [Google Scholar]
- Alhifany, A.A.; Alqurashi, A.F.; Al-Agamy, M.H.; Alkhushaym, N.; Alhomoud, F.; Alhomoud, F.K.; Almangour, T.A. Employment of mapping technology in antimicrobial resistance reporting in Saudi Arabia. Geospat. Health 2020, 15, 1. [Google Scholar] [CrossRef]
- Muniz Junior, R.L.; Godói, I.P.; Reis, E.A.; Garcia, M.M.; Guerra-Júnior, A.A.; Godman, B.; Ruas, C.M. Consumer willingness to pay for a hypothetical Zika vaccine in Brazil and the implications. Expert Rev. Pharm. Outcomes Res. 2019, 19, 473–482. [Google Scholar] [CrossRef]
- Aldossari, M.; Aljoudi, A.; Celentano, D. Health issues in the Hajj pilgrimage: A literature review. East. Mediterr. Health J. 2019, 25, 744–753. [Google Scholar] [CrossRef]
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Dadgostar, P. Antimicrobial resistance: Implications and costs. Infect. Drug Resist. 2019, 12, 3903–3910. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- Pulingam, T.; Parumasivam, T.; Gazzali, A.M.; Sulaiman, A.M.; Chee, J.Y.; Lakshmanan, M.; Chin, C.F.; Sudesh, K. Antimicrobial resistance: Prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur. J. Pharm. Sci. 2022, 170, 106103. [Google Scholar] [CrossRef] [PubMed]
- Al-Tawfiq, J.; Memish, Z.J.C.M. Infection. Potential risk for drug resistance globalization at the Hajj. Clin. Microbiol. Infect. 2015, 21, 109–114. [Google Scholar] [CrossRef]
- Leangapichart, T.; Gautret, P.; Griffiths, K.; Belhouchat, K.; Memish, Z.; Raoult, D.; Rolain, J.-M.J.A.A. Acquisition of a high diversity of bacteria during the Hajj pilgrimage, including Acinetobacter baumannii with blaOXA-72 and Escherichia coli with blaNDM-5 carbapenemase genes. Chemotherapy 2016, 60, 5942–5948. [Google Scholar]
- Shirah, B.H.; Zafar, S.H.; Alferaidi, O.A.; Sabir, A.M. Mass gathering medicine (Hajj Pilgrimage in Saudi Arabia): The clinical pattern of pneumonia among pilgrims during Hajj. J. Infect. Public Health 2017, 10, 277–286. [Google Scholar] [CrossRef]
- Simpson, I.J.; Aburizaiza, O.S.; Siddique, A.; Barletta, B.; Blake, N.J.; Gartner, A.; Khwaja, H.; Meinardi, S.; Zeb, J.; Blake, D.R. Air quality in Mecca and surrounding holy places in Saudi Arabia during Hajj: Initial survey. Environ. Sci. Technol. 2014, 48, 8529–8537. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Benkouiten, S.; Al-Tawfiq, J.A.; Memish, Z.A. Hajj-associated viral respiratory infections: A systematic review. Travel Med. Infect. Dis. 2016, 14, 92–109. [Google Scholar] [CrossRef] [PubMed]
- van Doorn, H.R.; Yu, H. Viral respiratory infections. In Hunter’s Tropical Medicine and Emerging Infectious Diseases; Elsevier: Amsterdam, The Netherlands, 2020; pp. 284–288. [Google Scholar]
- Dauda Goni, M.; Hasan, H.; Naing, N.N.; Wan-Arfah, N.; Zeiny Deris, Z.; Nor Arifin, W.; Abubakar Baaba, A. Assessment of Knowledge, Attitude and Practice towards Prevention of Respiratory Tract Infections among Hajj and Umrah Pilgrims from Malaysia in 2018. Int. J. Environ. Res. Public Health 2019, 16, 4569. [Google Scholar] [CrossRef]
- Alfelali, M.; Barasheed, O.; Badahdah, A.-M.; Bokhary, H.; Azeem, M.I.; Habeebullah, T.; Bakarman, M.; Asghar, A.; Booy, R.; Rashid, H. Influenza vaccination among Saudi Hajj pilgrims: Revealing the uptake and vaccination barriers. Vaccine 2018, 36, 2112–2118. [Google Scholar] [CrossRef]
- Balkhy, H.H.; Memish, Z.A.; Bafaqeer, S.; Almuneef, M.A. Influenza a common viral infection among Hajj pilgrims: Time for routine surveillance and vaccination. J. Travel Med. 2004, 11, 82–86. [Google Scholar] [CrossRef][Green Version]
- Benkouiten, S.; Al-Tawfiq, J.A.; Memish, Z.A.; Albarrak, A.; Gautret, P. Clinical respiratory infections and pneumonia during the Hajj pilgrimage: A systematic review. Travel Med. Infect. Dis. 2019, 28, 15–26. [Google Scholar] [CrossRef]
- Dzaraly, N.D.; Rahman, N.I.A.; Simbak, N.B.; Ab Wahab, S.; Osman, O.; Ismail, S.; Haque, M. Patterns of communicable and non-communicable diseases in Pilgrims during Hajj. Res. J. Pharm. Technol. 2014, 7, 12. [Google Scholar]
- Algaissi, A.A.; Alharbi, N.K.; Hassanain, M.; Hashem, A.M. Preparedness and response to COVID-19 in Saudi Arabia: Building on MERS experience. J. Infect. Public Health 2020, 13, 834–838. [Google Scholar] [CrossRef]
- Shang, W.; Wang, Y.; Yuan, J.; Guo, Z.; Liu, J.; Liu, M. Global excess mortality during COVID-19 pandemic: A systematic review and meta-analysis. Vaccines 2022, 10, 1702. [Google Scholar] [CrossRef]
- Shabrawishi, M.; Al-Gethamy, M.M.; Naser, A.Y.; Ghazawi, M.A.; Alsharif, G.F.; Obaid, E.F.; Melebari, H.A.; Alamri, D.M.; Brinji, A.S.; Al Jehani, F.H. Clinical, radiological and therapeutic characteristics of patients with COVID-19 in Saudi Arabia. PLoS ONE 2020, 15, e0237130. [Google Scholar] [CrossRef]
- Ayouni, I.; Maatoug, J.; Dhouib, W.; Zammit, N.; Fredj, S.B.; Ghammam, R.; Ghannem, H. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health 2021, 21, 1015. [Google Scholar] [CrossRef] [PubMed]
- Atique, S.; Itumalla, R. Hajj in the Time of COVID-19. Infect. Dis. Health 2020, 25, 219–221. [Google Scholar] [CrossRef]
- Sambas, M.F.M.K.; Rabbani, U.; Al-Gethamy, M.M.M.; Surbaya, S.H.; Alharbi, F.F.I.; Ahmad, R.G.A.; Qul, H.K.H.; Nassar, S.M.S.; Maddah, A.K.M.A.; Darweesh, B.A.K. Prevalence and determinants of multidrug-resistant tuberculosis in Makkah, Saudi Arabia. Infect. Drug Resist. 2020, 2020, 4031–4038. [Google Scholar] [CrossRef]
- Al-Hayani, A.M.; Kamel, S.A.; Almudarra, S.S.; Alhayani, M.; Abu-Zaid, A.; Al-Hayani, A.; Kamel, S., Jr.; Al-Hayani, M.M. Drug resistance to anti-tuberculosis drugs: A cross-sectional study from Makkah, Saudi Arabia. Cureus 2021, 13, 8. [Google Scholar] [CrossRef]
- Yezli, S.; Zumla, A.; Yassin, Y.; Al-Shangiti, A.M.; Mohamed, G.; Turkistani, A.M.; Alotaibi, B. Undiagnosed Active Pulmonary Tuberculosis among Pilgrims during the 2015 Hajj Mass Gathering: A Prospective Cross-sectional Study. Am. J. Trop. Med. Hyg. 2017, 97, 1304–1309. [Google Scholar] [CrossRef][Green Version]
- Yezli, S.; Memish, Z.A. Tuberculosis in Saudi Arabia: Prevalence and antimicrobial resistance. J. Chemother. 2012, 24, 1–5. [Google Scholar] [CrossRef]
- Memish, Z.A.; Balkhy, H.H.; Almuneef, M.A.; Al-Haj-Hussein, B.T.; Bukhari, A.I.; Osoba, A. Carriage of Staphylococcus aureus among Hajj pilgrims. Saudi Med. J. 2006, 27, 1367. [Google Scholar]
- Al-Saleh, A.; Shahid, M.; Farid, E.; Bindayna, K. Trends in methicillin-resistant Staphylococcus aureus in the Gulf Cooperation Council countries: Antibiotic resistance, virulence factors and emerging strains. East. Mediterr. Health J. 2022, 28, 434–443. [Google Scholar] [CrossRef]
- Yezli, S.; Assiri, A.M.; Alhakeem, R.F.; Turkistani, A.M.; Alotaibi, B. Meningococcal disease during the Hajj and Umrah mass gatherings. Int. J. Infect. Dis. 2016, 47, 60–64. [Google Scholar] [CrossRef]
- Mahdi, H.A.; Qashqari, F.S.; Hariri, S.H.; Bamerdah, S.; Altayyar, S.A.; Almalki, H.M.; Alwadani, F.A.; Alabbasi, R.A.; Alqahtani, M.H.; Alfelali, M.; et al. Low Prevalence of Syndromic Respiratory Tract Infections among Returning Hajj Pilgrims Amidst the COVID-19 Pandemic: A Post-Hajj Survey. Trop. Med. Infect. Dis. 2022, 7, 182. [Google Scholar] [CrossRef]
- Mahdi, H.A.; Rashid, H.; Qashqari, F.S.; Hariri, S.H.; Marglani, O.A.; Barasheed, O.; Albutti, A.; Alwashmi, A.S.; Shaban, R.Z.; Booy, R. Syndromic surveillance of respiratory-tract infections and hand hygiene practice among pilgrims attended Hajj in 2021: A cohort study. BMC Infect. Dis. 2022, 22, 578. [Google Scholar] [CrossRef] [PubMed]
- Alasmari, A.; Houghton, J.; Greenwood, B.; Heymann, D.; Edwards, P.; Larson, H.; Assiri, A.; Ben-Rached, F.; Pain, A.; Behrens, R. Meningococcal carriage among Hajj pilgrims, risk factors for carriage and records of vaccination: A study of pilgrims to Mecca. Trop. Med. Int. Health 2021, 26, 453–461. [Google Scholar] [CrossRef] [PubMed]
- AboEl-Magd, G.H.; Alkhotani, N.; Elsawy, A. The prevalence and pattern of pneumonia among Hajj pilgrims: A study of two successive Hajj seasons. Chest 2020, 69, 407. [Google Scholar]
- Raja, W.; Aziz, A.; Hassan, T.B.; Jalil, M.; Niazi, I.U.; Jawaid, N.; Tariq, M. Disease patterns among Hajj pilgrims attending medical facilities of Pakistan Hajj medical mission 2016 (1437 HIJRI). Pak. Armed Forces Med. J. 2017, 67, 825–831. [Google Scholar]
- Dhafar, K.O.; Baljoon, M.J.; Gazzaz, Z.J.; Al-Hothali, F.T.; Deyab, B.A.; Imran, M. Disease Pattern of Patients Admitted during Hajj Time and Provision of Health Service to Fulfill the Necessary Pillars of Hajj. Leukemia 2016, 7, 946–950. [Google Scholar]
- Hashim, S.; Ayub, Z.N.; Mohamed, Z.; Hasan, H.; Harun, A.; Ismail, N.; Rahman, Z.A.; Suraiya, S.; Naing, N.N.; Aziz, A.A. The prevalence and preventive measures of the respiratory illness among Malaysian pilgrims in 2013 Hajj season. J. Travel Med. 2016, 23, tav019. [Google Scholar] [CrossRef]
- Bakhsh, A.R.; Sindy, A.I.; Baljoon, M.J.; Dhafar, K.O.; Gazzaz, Z.J.; Baig, M.; Deiab, B.A.; Al Hothali, F.T. Diseases pattern among patients attending Holy Mosque (Haram) medical centers during Hajj 1434 (2013). Saudi Med. J. 2015, 36, 962. [Google Scholar] [CrossRef]
- Memish, Z.A.; Almasri, M.; Turkestani, A.; Al-Shangiti, A.M.; Yezli, S. Etiology of severe community-acquired pneumonia during the 2013 Hajj—Part of the MERS-CoV surveillance program. Int. J. Infect. Dis. 2014, 25, 186–190. [Google Scholar] [CrossRef]
- Memish, Z.; Al Hakeem, R.; Al Neel, O.; Danis, K.; Jasir, A.; Eibach, D. Laboratory-confirmed invasive meningococcal disease: Effect of the Hajj vaccination policy, Saudi Arabia, 1995 to 2011. Eurosurveillance 2013, 18, 20581. [Google Scholar] [CrossRef]
- Barasheed, O.; Almasri, N.; Badahdah, A.-M.; Heron, L.; Taylor, J.; McPhee, K.; Ridda, I.; Haworth, E.; Dwyer, D.E.; Rashid, H.; et al. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like illness transmission among Australian Hajj pilgrims in 2011. Infect. Disord.-Drug Targets 2014, 14, 110–116. [Google Scholar] [CrossRef]
- Alzahrani, A.G.; Choudhry, A.J.; Al Mazroa, M.A.; Turkistani, A.H.M.; Nouman, G.S.; Memish, Z.A. Pattern of diseases among visitors to Mina health centers during the Hajj season, 1429 H (2008 G). J. Infect. Public Health 2012, 5, 22–34. [Google Scholar] [CrossRef]
- Mandourah, Y.; Al-Radi, A.; Ocheltree, A.H.; Ocheltree, S.R.; Fowler, R. Clinical and temporal patterns of severe pneumonia causing critical illness during Hajj. BMC Infect. Dis. 2012, 12, 1–8. [Google Scholar] [CrossRef]
- Alherabi, A.Z. Impact of pH1N1 influenza A infections on the otolaryngology, head and neck clinic during Hajj 2009. Saudi Med. J. 2011, 32, 933–938. [Google Scholar]
- Al-Ghamdi, A.S.; Kabbash, I. Awareness of healthcare workers regarding preventive measures of communicable diseases among Hajj pilgrims at the entry point in Western Saudi Arabia. Saudi Med. J. 2011, 32, 1161–1167. [Google Scholar]
- Baharoon, S.; Al-Jahdali, H.; Al Hashmi, J.; Memish, Z.A.; Ahmed, Q.A. Severe sepsis and septic shock at the Hajj: Etiologies and outcomes. Travel Med. Infect. Dis. 2009, 7, 247–252. [Google Scholar] [CrossRef]
- Ibrahim, N.K. Epidemiological pattern of diseases and risk behaviors of pilgrims attending mina hospitals, hajj 1427 h (2007 g). J. Egypt Public Health Assoc. 2008, 83, 15–33. [Google Scholar]
- Madani, T.A.; Ghabrah, T.M.; Albarrak, A.M.; Alhazmi, M.A.; Alazraqi, T.A.; Althaqafi, A.O.; Ishaq, A.H. Causes of admission to intensive care units in the Hajj period of the Islamic year 1424 (2004). Ann. Saudi Med. 2007, 27, 101–105. [Google Scholar]
- Madani, T.A.; Ghabrah, T.M.; Al-Hedaithy, M.A.; Alhazmi, M.A.; Alazraqi, T.A.; Albarrak, A.M.; Ishaq, A.H. Causes of hospitalization of pilgrims during the Hajj period of the Islamic year 1423 (2003). Ann. Saudi Med. 2006, 26, 346–351. [Google Scholar] [CrossRef]
- Karima, T.M.; Bukhari, S.Z.; Fatani, M.I.; Yasin, K.A.A.; Al-Afif, K.A.; Hafiz, F.H. Clinical and microbiological spectrum of meningococcal disease in adults during Hajj 2000: An implication of quadrivalent vaccination policy. J.-Pak. Med. Assoc. 2003, 53, 3–7. [Google Scholar]
- Zowawi, H.M. Antimicrobial resistance in Saudi Arabia: An urgent call for an immediate action. Saudi Med. J. 2016, 37, 935. [Google Scholar] [CrossRef]
- Saleem, Z.; Hassali, M.A.; Godman, B.; Fatima, M.; Ahmad, Z.; Sajid, A.; Rehman, I.U.; Nadeem, M.U.; Javaid, Z.; Malik, M. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: A simulated client study. J. Pharm. Policy Pract. 2020, 13, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Saleem, Z.; Hassali, M.A.; Hashmi, F.K.; Godman, B.; Saleem, F. Antimicrobial dispensing practices and determinants of antimicrobial resistance: A qualitative study among community pharmacists in Pakistan. Fam. Med. Community Health 2019, 7, e000138. [Google Scholar] [CrossRef] [PubMed]
- Alrasheedy, A.A.; Alsalloum, M.A.; Almuqbil, F.A.; Almuzaini, M.A.; Aba Alkhayl, B.S.; Albishri, A.S.; Alharbi, F.F.; Alharbi, S.R.; Alodhayb, A.K.; Alfadl, A.A. The impact of law enforcement on dispensing antibiotics without prescription: A multi-methods study from Saudi Arabia. Expert Rev. Anti-Infect. Ther. 2020, 18, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Alyamani, E.J.; Khiyami, A.M.; Booq, R.Y.; Majrashi, M.A.; Bahwerth, F.S.; Rechkina, E. The occurrence of ESBL-producing Escherichia coli carrying aminoglycoside resistance genes in urinary tract infections in Saudi Arabia. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- Marglani, O.A.; Alherabi, A.Z.; Herzallah, I.R.; Saati, F.A.; Tantawy, E.A.; Alandejani, T.A.; Faidah, H.S.; Bawazeer, N.A.; Marghalani, A.A.; Madani, T.A. Acute rhinosinusitis during Hajj season 2014: Prevalence of bacterial infection and patterns of antimicrobial susceptibility. Travel Med. Infect. Dis. 2016, 14, 583–587. [Google Scholar] [CrossRef]
- Yezli, S.; Zaraa, S.; Yassin, Y.; Mushi, A.; Stergachis, A.; Khan, A. Medication utilization pattern among outpatients during the Hajj mass gathering. Saudi Pharm. J. 2020, 28, 1122–1128. [Google Scholar] [CrossRef]
- Memish, Z.A.; Arabi, Y.M.; Ahmed, Q.A.; Shibl, A.M.; Niederman, M.S. Management and Prevention Strategies for Community-Acquired Pneumonia in the Gulf Corporation Council. J. Chemother. 2007, 19, 33–46. [Google Scholar] [CrossRef]
- Azeem, M.; Tashani, M.; Barasheed, O.; Heron, L.; Hill-Cawthorne, G.A.; Haworth, E.; Dwyer, D.E.; Rashid, H.; Booy, R. Knowledge, Attitude and Practice (KAP) Survey Concerning Antimicrobial Use among Australian Hajj Pilgrims. Infect Disord Drug Targets 2014, 14, 125–132. [Google Scholar] [CrossRef]
- Mustafa, A.N.; Gessner, B.D.; Ismail, R.; Yusoff, A.F.; Abdullah, N.; Ishak, I.; Abdullah, N.; Merican, M.I. A case-control study of influenza vaccine effectiveness among Malaysian pilgrims attending the Haj in Saudi Arabia. Int. J. Infect. Dis. 2003, 7, 210–214. [Google Scholar] [CrossRef][Green Version]
- Metanat, M.; Sharifi-Mood, B.; Sanei-Moghaddam, S.; Rad, N.S. Pharyngeal carriage rate of Neisseria meningitidis before and after the Hajj pilgrimage, in Zahedan (southeastern Iran), 2012. Turk J. Med. Sci. 2015, 45, 1317–1320. [Google Scholar] [CrossRef]
- Qureshi, H.; Gessner, B.D.; Leboulleux, D.; Hasan, H.; Alam, S.E.; Moulton, L.H. The incidence of vaccine preventable influenza-like illness and medication use among Pakistani pilgrims to the Haj in Saudi Arabia. Vaccine 2000, 18, 2956–2962. [Google Scholar] [CrossRef]
- Hoang, V.-T.; Ali-Salem, S.; Belhouchat, K.; Meftah, M.; Sow, D.; Dao, T.-L.; Ly, T.D.A.; Drali, T.; Ninove, L.; Yezli, S. Respiratory tract infections among French Hajj pilgrims from 2014 to 2017. Sci. Rep. 2019, 9, 17771–17778. [Google Scholar] [CrossRef]
- Yaser, M.; Aljabri, A.K.; Alsaadi, F.N.; Rizk, L.M.; Alahmadi, R.Y.; Aljuhani, S.R.; Aljohani, S.H.; Al Thagfan, S.S.; Alamuddin, W.A.; Alonazie, W.S. A prospective antibiotic point prevalence survey in two primary referral hospitals during and after pilgrims stay in Madinah, Saudi Arabia. Trop. J. Pharm. Res. 2020, 19, 391–399. [Google Scholar] [CrossRef]
- Dzaraly, D.; Rahman, N.I.A.; Haque, M.; Ab Wahab, M.S.B.; Simbak, N.B.; Abd Aziz, A.; Ismail, S.; Muttalif, A.R.A. Antibiotic therapy of choice for community-acquired pneumonia in Malaysian Hajj pilgrims: The pattern and associated factors. Med. Stud. 2017, 33, 199–207. [Google Scholar] [CrossRef]
- Alreeme, S.; Bokhary, H.; Craig, A.T. Transmission of Antimicrobial Resistant Bacteria at the Hajj: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 14134. [Google Scholar] [CrossRef]
- Harimurti, K.; Saldi, S.R.F.; Dewiasty, E.; Alfarizi, T.; Dharmayuli, M.; Khoeri, M.M.; Paramaiswari, W.T.; Salsabila, K.; Tafroji, W.; Halim, C.; et al. Streptococcus pneumoniae carriage and antibiotic susceptibility among Indonesian pilgrims during the Hajj pilgrimage in 2015. PLoS ONE 2021, 16, e0246122. [Google Scholar] [CrossRef]
- Alqahtani, A.S.; Althimiri, N.A.; BinDhim, N.F. Saudi Hajj pilgrims’ preparation and uptake of health preventive measures during Hajj 2017. J. Infect. Public Health 2019, 12, 772–776. [Google Scholar] [CrossRef]
- Alborzi, A.; Oskoee, S.; Pourabbas, B.; Alborzi, S.; Astaneh, B.; Gooya, M.M.; Kaviani, M.J. Meningococcal carrier rate before and after hajj pilgrimage: Effect of single dose ciprofloxacin on carriage. East. Mediterr. Health J. 2008, 14, 277–282. [Google Scholar]
- Minhas, S.; Kotwal, A.; Singh, M. Infection Control in Health Care Facilities. Med. J. Armed India 2011, 67, 7–8. [Google Scholar] [CrossRef]
- Shafi, S.; Booy, R.; Haworth, E.; Rashid, H.; Memish, Z.A. Hajj: Health lessons for mass gatherings. J. Infect. Public Health 2008, 1, 27–32. [Google Scholar] [CrossRef]
- Ahmed, Q.A.; Barbeschi, M.; Memish, Z.A. The quest for public health security at Hajj: The WHO guidelines on communicable disease alert and response during mass gatherings. Travel Med. Infect. Dis. 2009, 7, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Alahmari, A.A.; Khan, A.A.; Alamri, F.A.; Almuzaini, Y.S.; Alradini, F.A.; Almohamadi, E.; Alsaeedi, S.; Asiri, S.; Motair, W.; Almadah, A. Hajj 2021: Role of Mitigation Measures for Health Security. J. Infect. Public Health 2022, 15, 1350–1354. [Google Scholar] [CrossRef] [PubMed]
- Jokhdar, H.; Khan, A.; Asiri, S.; Motair, W.; Assiri, A.; Alabdulaali, M. COVID-19 mitigation plans during Hajj 2020: A success story of zero cases. Health Secur. 2021, 19, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Basahel, S.; Alsabban, A.; Yamin, M. Hajj and Umrah management during COVID-19. Int. J. Inf. Technol. 2021, 13, 2491–2495. [Google Scholar] [CrossRef]
- Alamri, F.A.; Khan, A.; Badokhan, A.H.; Abogazalah, F.N.; Alhraiwil, N.J.; Amer, S.A. Common Health Complains Among Pilgrims during Manasik El Hajj; Season 1439H (2018). Merit. Res. J. Med. Med. Sci. 2020, 8, 351–360. [Google Scholar]
- Aljohani, A.; Nejaim, S.; Khayyat, M.; Aboulola, O. E-government and logistical health services during Hajj season. Bull. Natl. Res. Cent. 2022, 46, 112. [Google Scholar] [CrossRef]
- Abolfotouh, M.A.; Almutairi, A.F.; Banimustafa, A.; Hagras, S.A.; Al Jeraisy, M. Behavior Responses and Attitude of the Public to COVID-19 Pandemic During Movement Restrictions in Saudi Arabia. Int. J. Gen. Med. 2021, 14, 741–753. [Google Scholar] [CrossRef]
- Haworth, E.; Barasheed, O.; Memish, Z.A.; Rashid, H.; Booy, R. Prevention of influenza at Hajj: Applications for mass gatherings. J. R. Soc. Med. 2013, 106, 215–223. [Google Scholar] [CrossRef]
- Haridi, H.K.; Salman, K.A.; Basaif, E.A.; Al-Skaibi, D.K. Influenza vaccine uptake, determinants, motivators, and barriers of the vaccine receipt among healthcare workers in a tertiary care hospital in Saudi Arabia. J. Hosp. Infect. 2017, 96, 268–275. [Google Scholar] [CrossRef]
- Abd El Ghany, M.; Sharaf, H.; Hill-Cawthorne, G.A. Hajj vaccinations—Facts, challenges, and hope. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2016, 47, 29–37. [Google Scholar] [CrossRef][Green Version]
- Riedmann, E.M. Report: State of the Worlds Vaccines and Immunization; Taylor & Francis: Abingdon, UK, 2010. [Google Scholar]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef]
- Dagan, R.; Klugman, K.P. Impact of conjugate pneumococcal vaccine on antibiotic resistance. Lancet Infect. Dis. 2008, 8, 369–385. [Google Scholar] [CrossRef]
- Cohen, R. Approaches to reduce antibiotic resistance in the community. Pediatr. Infect. Dis. J. 2006, 25, 977–980. [Google Scholar] [CrossRef]
- Kwong, J.C.; Maaten, S.; Upshur, R.E.; Patrick, D.M.; Marra, F. The effect of universal influenza immunization on antibiotic prescriptions: An ecological study. Clin. Infect. Dis. 2009, 49, 750–756. [Google Scholar] [CrossRef]
- Badahdah, A.-M.; Alfelali, M.; Alqahtani, A.S.; Alsharif, S.; Barasheed, O.; Rashid, H.; the Hajj Research Team. Mandatory meningococcal vaccine, and other recommended immunisations: Uptake, barriers, and facilitators among health care workers and trainees at Hajj. World J. Clin. Cases 2018, 6, 1128. [Google Scholar] [CrossRef]
- Prevention, I. Control of Epidemic-and Pandemic-Prone Acute Respiratory Infections in Health Care; World Health Organization: Geneva, Switzerland, 2014.
- Nieradko-Iwanicka, B. Hygiene–gold standard not only in prevention of COVID-19 infection. Reumatol./Rheumatol. Suppl. 2020, 58, 191. [Google Scholar] [CrossRef]
- Ahmed, Q.A.; Memish, Z.A.; Allegranzi, B.; Pittet, D. Muslim health-care workers and alcohol-based handrubs. Lancet 2006, 367, 1025–1027. [Google Scholar] [CrossRef]
- Balaban, V.; Stauffer, W.M.; Hammad, A.; Afgarshe, M.; Abd-Alla, M.; Ahmed, Q.; Memish, Z.A.; Saba, J.; Harton, E.; Palumbo, G. Protective practices and respiratory illness among US travelers to the 2009 Hajj. J. Travel Med. 2012, 19, 163–168. [Google Scholar] [CrossRef][Green Version]
- Sahin, M.K.; Aker, S.; Tuncel, E.K. Knowledge, attitudes and practices concerning Middle East respiratory syndrome among Umrah and Hajj pilgrims in Samsun, Turkey, 2015. Eurosurveillance 2015, 20, 30023. [Google Scholar] [CrossRef]
- Sen-Crowe, B.; McKenney, M.; Elkbuli, A. Social distancing during the COVID-19 pandemic: Staying home save lives. Am. J. Emerg. Med. 2020, 38, 1519–1520. [Google Scholar] [CrossRef]
- Sayed, A.A. The Progressive Public Measures of Saudi Arabia to Tackle COVID-19 and Limit Its Spread. Int. J. Environ. Res. Public Health 2021, 18, 783. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, M.; Alotaibi, F.; Ahmed, H.; Alharbi, F.; Bukhari, O.; Youssef, A.-R. Effect of medical education on the knowledge, attitude and compliance regarding infection control measures among dental students in Makkah. J. Umm Al-Qura Univ. Med. Sci. 2021, 7, 14–17. [Google Scholar] [CrossRef]
- Shahrul Anuwar, M.Y.; Imran, A.; Irfan, M. The issues of facemask among hajj pilgrims: A critical review. Int. J. Sci. Environ. Technol. 2014, 3, 1528–1534. [Google Scholar]
- Smith, J.D.; MacDougall, C.C.; Johnstone, J.; Copes, R.A.; Schwartz, B.; Garber, G.E. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: A systematic review and meta-analysis. CMAJ 2016, 188, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Saunders-Hastings, P.; Crispo, J.A.G.; Sikora, L.; Krewski, D. Effectiveness of personal protective measures in reducing pandemic influenza transmission: A systematic review and meta-analysis. Epidemics 2017, 20, 1–20. [Google Scholar] [CrossRef]
- Liang, M.; Gao, L.; Cheng, C.; Zhou, Q.; Uy, J.P.; Heiner, K.; Sun, C. Efficacy of face mask in preventing respiratory virus transmission: A systematic review and meta-analysis. Travel Med. Infect. Dis. 2020, 36, 101751. [Google Scholar] [CrossRef]
- Coclite, D.; Napoletano, A.; Gianola, S.; Del Monaco, A.; D’Angelo, D.; Fauci, A.; Iacorossi, L.; Latina, R.; La Torre, G.; Mastroianni, C. Face mask use in the Community for Reducing the Spread of COVID-19: A systematic review. Front. Med. 2020, 7, 594269. [Google Scholar] [CrossRef]
- Getahun, H.; Smith, I.; Trivedi, K.; Paulin, S.; Balkhy, H.H. Tackling antimicrobial resistance in the COVID-19 pandemic. Bull. World Health Organ. 2020, 98, 442. [Google Scholar] [CrossRef]
- Bednarčuk, N.; Golić Jelić, A.; Stoisavljević Šatara, S.; Stojaković, N.; Marković Peković, V.; Stojiljković, M.P.; Popović, N.; Škrbić, R. Antibiotic Utilization during COVID-19: Are We Over-Prescribing? Antibiotics 2023, 12, 308. [Google Scholar] [CrossRef]
- Hsu, J. How COVID-19 is accelerating the threat of antimicrobial resistance. Bmj 2020, 369, m1983. [Google Scholar] [CrossRef]
- Alshaikh, F.S.; Godman, B.; Sindi, O.N.; Seaton, R.A.; Kurdi, A. Prevalence of bacterial coinfection and patterns of antibiotics prescribing in patients with COVID-19: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0272375. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Soucy, J.-P.R.; Westwood, D.; Daneman, N.; MacFadden, D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 520–531. [Google Scholar] [CrossRef]
- Saleem, Z.; Haseeb, A.; Godman, B.; Batool, N.; Altaf, U.; Ahsan, U.; Khan, F.U.; Mustafa, Z.U.; Nadeem, M.U.; Farrukh, M.J. Point prevalence survey of antimicrobial use during the COVID-19 pandemic among different hospitals in Pakistan: Findings and implications. Antibiotics 2022, 12, 70. [Google Scholar] [CrossRef]
- Sasaki, K.; Fujita, I.; Hamasaki, Y.; Miyazaki, S. Differentiating between bacterial and viral infection by measuring both C-reactive protein and 2′-5′-oligoadenylate synthetase as inflammatory markers. J. Infect. Chemother. 2002, 8, 76–80. [Google Scholar] [CrossRef]
- Sproston, N.R.; Ashworth, J.J. Role of C-reactive protein at sites of inflammation and infection. Front. Immunol. 2018, 9, 754. [Google Scholar] [CrossRef]
- Knight, G.M.; Glover, R.E.; McQuaid, C.F.; Olaru, I.D.; Gallandat, K.; Leclerc, Q.J.; Fuller, N.M.; Willcocks, S.J.; Hasan, R.; van Kleef, E.J.E. Antimicrobial resistance and COVID-19: Intersections and implications. Elife 2021, 10, e64139. [Google Scholar] [CrossRef]
- Egyir, B.; Obeng-Nkrumah, N.; Kyei, G.B. COVID-19 pandemic and antimicrobial resistance: Another call to strengthen laboratory diagnostic capacity in Africa. Afr. J. Lab. Med. 2020, 9, 1302. [Google Scholar] [CrossRef]
- Sharland, M.; Gandra, S.; Huttner, B.; Moja, L.; Pulcini, C.; Zeng, M.; Mendelson, M.; Cappello, B.; Cooke, G.; Magrini, N. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use—The new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect. Dis. 2019, 19, 1278–1280. [Google Scholar] [CrossRef]
- Sharland, M.; Zanichelli, V.; Ombajo, L.A.; Bazira, J.; Cappello, B.; Chitatanga, R.; Chuki, P.; Gandra, S.; Getahun, H.; Harbarth, S. The WHO essential medicines list AWaRe book: From a list to a quality improvement system. Clin. Microbiol. Infect. 2022, 28, 1533–1535. [Google Scholar] [CrossRef]
- Almangour, T.A.; Alenazi, B.; Ghonem, L.; Alhifany, A.A.; Aldakheel, B.A.; Alruwaili, A. Inhaled colistin for the treatment of nosocomial pneumonia due to multidrug-resistant Gram-negative bacteria: A real-life experience in tertiary care hospitals in Saudi Arabia. Saudi Pharm. J. 2020, 28, 1009–1013. [Google Scholar] [CrossRef]
- Nathwani, D.; Varghese, D.; Stephens, J.; Ansari, W.; Martin, S.; Charbonneau, C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Saleem, Z.; Godman, B.; Cook, A.; Khan, M.A.; Campbell, S.M.; Seaton, R.A.; Siachalinga, L.; Haseeb, A.; Amir, A.; Kurdi, A. Ongoing efforts to improve antimicrobial utilization in hospitals among African countries and implications for the future. Antibiotics 2022, 11, 1824. [Google Scholar] [CrossRef] [PubMed]
- Siachalinga, L.; Mufwambi, W. Impact of antimicrobial stewardship interventions to improve antibiotic prescribing for hospital inpatients in Africa: A systematic review and meta-analysis. J. Hosp. Infect. 2022, 129, 124–143. [Google Scholar] [CrossRef] [PubMed]
- Godman, B.; Fadare, J.; Kwon, H.-Y.; Dias, C.Z.; Kurdi, A.; Dias Godoi, I.P.; Kibuule, D.; Hoxha, I.; Opanga, S.; Saleem, Z. Evidence-based public policy making for medicines across countries: Findings and implications for the future. J. Comp. Eff. Res. 2021, 10, 1019–1052. [Google Scholar] [CrossRef]
- Mwita, J.C.; Ogunleye, O.O.; Olalekan, A.; Kalungia, A.C.; Kurdi, A.; Saleem, Z.; Sneddon, J.; Godman, B. Key issues surrounding appropriate antibiotic use for prevention of surgical site infections in low-and middle-income countries: A narrative review and the implications. Int. J. Gen. Med. 2021, 14, 515. [Google Scholar] [CrossRef]
- Godman, B.; Haque, M.; McKimm, J.; Abu Bakar, M.; Sneddon, J.; Wale, J.; Campbell, S.; Martin, A.P.; Hoxha, I.; Abilova, V.; et al. Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: Findings and implications for the future. Curr. Med Res. Opin. 2019, 36, 301–327. [Google Scholar] [CrossRef]
- Godman, B.; Egwuenu, A.; Wesangula, E.; Schellack, N.; Kalungia, A.C.; Tiroyakgosi, C.; Kgatlwane, J.; Mwita, J.C.; Patrick, O.; Niba, L.L. Tackling antimicrobial resistance across sub-Saharan Africa: Current challenges and implications for the future. Expert Opin. Drug Saf. 2022, 21, 1089–1111. [Google Scholar] [CrossRef]
- Godman, B.; Egwuenu, A.; Haque, M.; Malande, O.O.; Schellack, N.; Kumar, S.; Saleem, Z.; Sneddon, J.; Hoxha, I.; Islam, S. Strategies to improve antimicrobial utilization with a special focus on developing countries. Life 2021, 11, 528. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Bmj 2021, 372, n160. [Google Scholar] [CrossRef]
| Author Year | Geographical Origin | Study Design | Sample Size | Prevalence of Infection | Top 3 Infections | Findings | ||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||||
| Mahdi et al., 2022 [64] | Makkah | Cross-sectional study | 476 | 2.3% | RTIs (2.3%) | - | - | Low prevalence of RTIs among pilgrims was observed as compared to those documented in pre-pandemic studies. |
| Mahdi et al., 2022 [65] | Makkah | Cohort study | 445 | 4.7% | RTIs (4.7%) | - | - | Hand hygiene practice could play an important role to reduce the prevalence of RTIs. |
| Alasmari et al., 2021 [66] | Jeddah | Cross-sectional study | 2973 | 4.6% | Neisseria meningitidis (4.6%) | - | - | Vaccination is required to prevent meningococcal disease outbreaks during and after Hajj. |
| Al-Hayani et al., 2021 [58] | Makkah | Cross-sectional study | 472 | 100% | Pulmonary tuberculosis (91.7%) | - | - | Epidemiological studies are needed to validate the findings. |
| Sambas et al., 2020 [57] | Makkah | Cross-sectional study | 158 | 100% | Tuberculosis (100%) | - | - | TB control programs are required to prevent emergence and spread of MDR TB. |
| AboEl-Magd et al., 2020 [67] | Makkah | Cohort study | 614 | 39.2% | Pneumonia (39.2%) | - | - | Upgradation of antibiograms is required to enable selection of appropriate antibiotic. |
| Raja et al., 2017 [68] | Makkah, Madina, Jeddah | Descriptive, cross-sectional study | 184496 | 30.0% | RTIs (29%) | - | - | Structured policies and legislation, training sessions of HCWs should be introduced to prevent the spread of infections. |
| Yezli et al., 2017 [59] | Makkah | Cross-sectional study | 1063 | 1.4% | Tuberculosis (1.4%) | - | - | Undiagnosed TB poses a risk to other pilgrims. Consequently, proactive screening is needed. |
| Shirah et al., 2017 [43] | Madina | Retrospective study | 1059 | 23% | Pneumonia (23%) | - | - | Specific adjustment in the guidelines is required for the treatment of pneumonia. |
| Dhafar et al., 2016 [69] | Makkah | Descriptive, observational study | 217 | - | RTIs (12.9%) | Skin and soft tissue infections (9.2%) | - | Policies and legislation are required to improve the quality life of patients. |
| Hashim et al., 2016 [70] | Makkah, Arafat | Cross-sectional study | 468 | 93.4% | - | - | - | Preventive measures should be practiced. |
| Bakhsh et al., 2015 [71] | Makkah | Observational study | 1008 | - | RTIs (17.6%) | Skin and soft tissues infections (15.7%) | - | Improvement in healthcare facilities during Hajj is required. |
| Memish et al., 2014 [72] | Makkah and Madina | Observational study | 38 | 68.4% | CAP (68.4%) | - | - | Improved respiratory tract infection surveillance is needed. |
| Memish et al., 2013 [73] | Makkah and Madina | Observational study | 1103 | 100% | Invasive meningococcal disease (100%) | - | - | The number of cases has declined. Regular monitoring is necessary to monitor the trends during upcoming hajj seasons. |
| Barasheed et al., 2014 [74] | Makkah, Mina | Randomized controlled trial | 1038 | 38% | Rhinovirus (25%) | Influenza (2%) | Adenovirus (2%) | Appropriate vaccination and infection control are required to reduce the risk of transmission of respiratory virus. |
| Alzahrani et., 2012 [75] | Mina | Descriptive study | 4136 | 67% | RTIs (60.8%) | Infectious skin diseases (4.7%) | UTIs (1.5%) | Best possible healthcare service should be given to Hajj pilgrims by Saudi healthcare authorities. |
| Mandourah et., 2012 [76] | Mina, Makkah, Arafat, Madina | Cohort study | 452 | 27.2% | CAP (66.7%) | Aspiration-related pneumonia (25.2%) | Tuberculosis (4.9%) | Increased efforts for the prevention of infectious diseases among Hajj pilgrim is required. |
| Alherabi et al., 2011 [77] | Makkah | Cross-sectional study | 3087 | 92% | Pharyngitis (45.7%) | URTIs (42.1%) | Influenza (2.5%) | Misuse of antimicrobials should be discouraged by guiding pilgrims regarding rational use of antimicrobials. |
| Al-Ghamdi et al., 2011 [78] | Mina, Arafat | Cohort study | 160 | 57% | Pneumonia (39.4%) | URTIs (3.3%) | - | Structured policies and strategies regarding infection prevention and control should be initiated. |
| Baharoon et al., 2009 [79] | Makkah | Cross-sectional study | 165 | 71% | CAP (54.8%) | Intra-abdominal source (16.6%) | Skin and soft issue infection (14.3%) | Initiation and implementation of infection prevention and control programs are required. |
| Ibrahim et al., 2008 [80] | Mina | Cross-sectional study | 248 | - | RTIs (29.8%) | UTIS (1.6%) | - | Intensified health education campaigns should be conducted for all pilgrims in their home countries and KSA. |
| Madani et al., 2007 [81] | Mina, Arafat | Cross-sectional Study | 140 | 26.4% | Pneumonia (22%) | Sepsis (4.3%) | - | Cost-effective and optimal healthcare services are urgently needed for Hajj pilgrims. |
| Madani et al., 2006 [82] | Mina, Arafat | Cross-sectional study | 808 | 36.4% | Pneumonia (19.7%) | URTIs (3.3%) | Cellulitis (1.6%) | Cost-effective and optimal healthcare services are urgently needed for Hajj pilgrims. |
| Memish et al., 2006 [61] | Mina | Cohort study | 411 | 20.6% | - | - | - | Susceptibility testing should be performed so that antimicrobials could be used when needed. |
| Balkhy et al., 2004 [49] | Mina | Cross-sectional study | 500 | 10.8% | Influenza (55.6%) | HSV (24.1%) | RSV (12.9%) | Vaccination should be required for every Hajj pilgrim. |
| Karima et al., 2003 [83] | Makkah | Cross-sectional study | 105 | 100% | Meningitis (64%) | Meningococcemia (36%) | - | Quadrivalent Vaccine is required for all pilgrims before coming to KSA. |
| Strategies | Potential Barriers |
|---|---|
| Public Awareness | Language barriers. Illiteracy. Scarcity of resources for educational programs. Concerns with misinformation from authorities |
| Adequate sanitation facilities | Limited access to clean water and sanitation facilities. Overcrowding. Insufficient availability of handwashing stations. Lack of awareness of hand hygiene. |
| Respiratory Etiquettes | Culture norms. Lack of awareness about respiratory hygiene practices. |
| Vaccination campaign | Limited access to vaccines. Vaccines hesitancy. Inadequate healthcare infrastructure. |
| Infectious Disease surveillance | Lack of resources for surveillance. Delays in reporting and response. |
| Crowd management and planning | Lack of infrastructure for crowd control. Logistical challenges. |
| Food Safety Measures | Poor food handling practices. Lack of proper food inspection and regulation. |
| Healthcare Services availability | Insufficient healthcare facilities and personnels. Overwhelmed healthcare systems. |
| # | Search Terms |
|---|---|
| 1 | (Hajj) OR (Pilgrims)-{MeSH Terms} OR/AND {Text Word} |
| 2 | (Antimicrobial resistance) OR (Antimicrobial sensitivity) - {MeSH Terms} OR/AND {Text Word} |
| 3 | (Infectious diseases) AND (Antimicrobial use)-{MeSH Terms} OR/AND {Text Word} |
| 4 | (COVID)-{MeSH Terms} OR/AND {Text Word} |
| 5 | #1 AND #2 |
| 6 | #1 AND #3 |
| 8 | #2 AND #3 |
| 9 | #1 AND #2 AND #3 AND #4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haseeb, A.; Saleem, Z.; Faidah, H.S.; Saati, A.A.; AlQarni, A.; Iqbal, M.S.; Alghamdi, S.; Elrggal, M.E.; AlGethamy, M.; Radwan, R.M.; et al. Threat of Antimicrobial Resistance among Pilgrims with Infectious Diseases during Hajj: Lessons Learnt from COVID-19 Pandemic. Antibiotics 2023, 12, 1299. https://doi.org/10.3390/antibiotics12081299
Haseeb A, Saleem Z, Faidah HS, Saati AA, AlQarni A, Iqbal MS, Alghamdi S, Elrggal ME, AlGethamy M, Radwan RM, et al. Threat of Antimicrobial Resistance among Pilgrims with Infectious Diseases during Hajj: Lessons Learnt from COVID-19 Pandemic. Antibiotics. 2023; 12(8):1299. https://doi.org/10.3390/antibiotics12081299
Chicago/Turabian StyleHaseeb, Abdul, Zikria Saleem, Hani Saleh Faidah, Abdullah A. Saati, Abdullmoin AlQarni, Muhammad Shahid Iqbal, Saleh Alghamdi, Mahmoud E. Elrggal, Manal AlGethamy, Rozan Mohammad Radwan, and et al. 2023. "Threat of Antimicrobial Resistance among Pilgrims with Infectious Diseases during Hajj: Lessons Learnt from COVID-19 Pandemic" Antibiotics 12, no. 8: 1299. https://doi.org/10.3390/antibiotics12081299
APA StyleHaseeb, A., Saleem, Z., Faidah, H. S., Saati, A. A., AlQarni, A., Iqbal, M. S., Alghamdi, S., Elrggal, M. E., AlGethamy, M., Radwan, R. M., Mahrous, A. J., Abuhussain, S. S. A., Khayyat, S. M., Ibrahim, K., Godman, B., & Sheikh, A. (2023). Threat of Antimicrobial Resistance among Pilgrims with Infectious Diseases during Hajj: Lessons Learnt from COVID-19 Pandemic. Antibiotics, 12(8), 1299. https://doi.org/10.3390/antibiotics12081299








