Carbapenem-Resistant Klebsiella pneumoniae in COVID-19 Era—Challenges and Solutions
Abstract
1. Introduction
2. Results
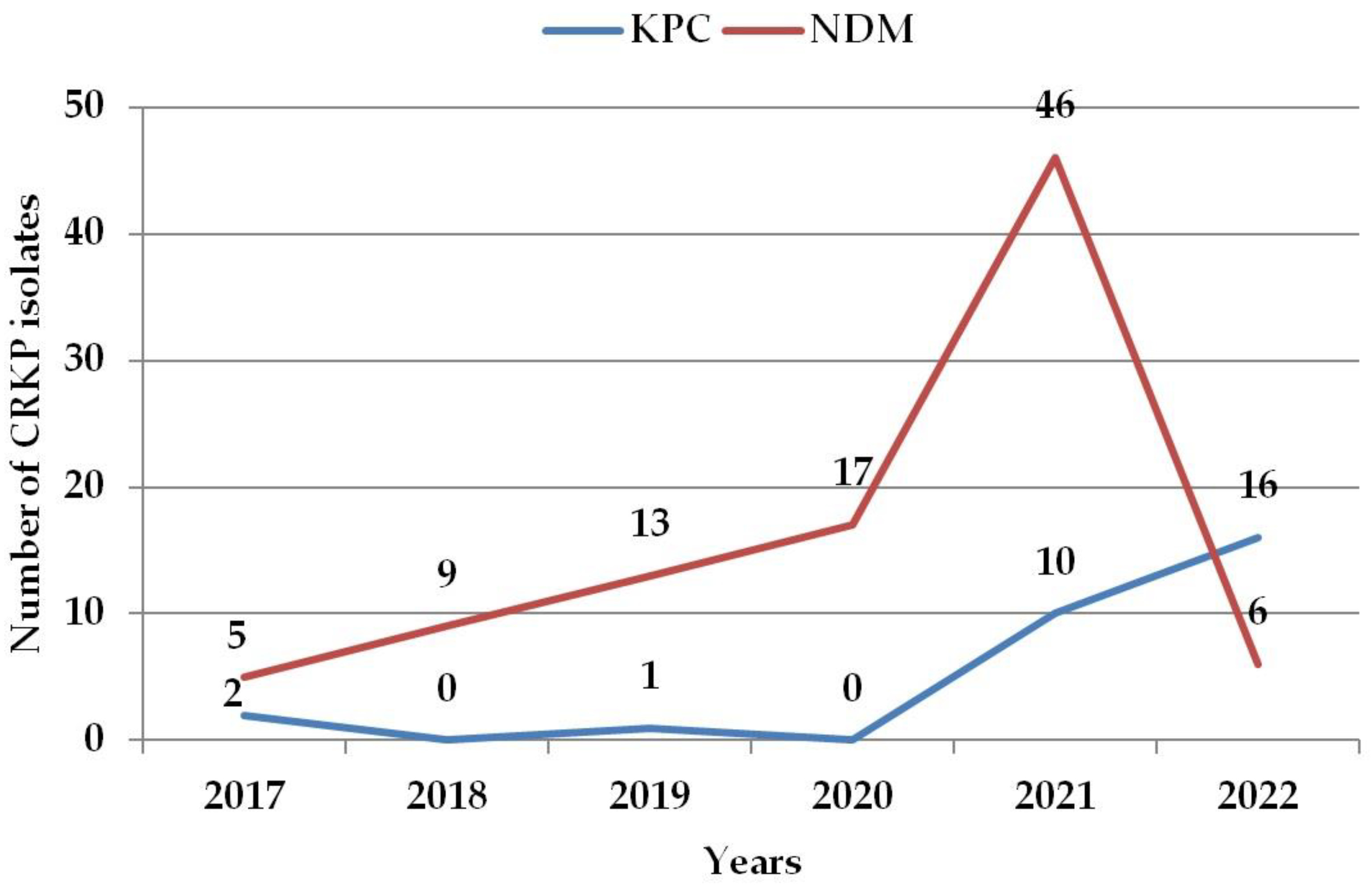
2.1. The Incidence of Carbapenemase-Producing Klebsiella pneumoniae
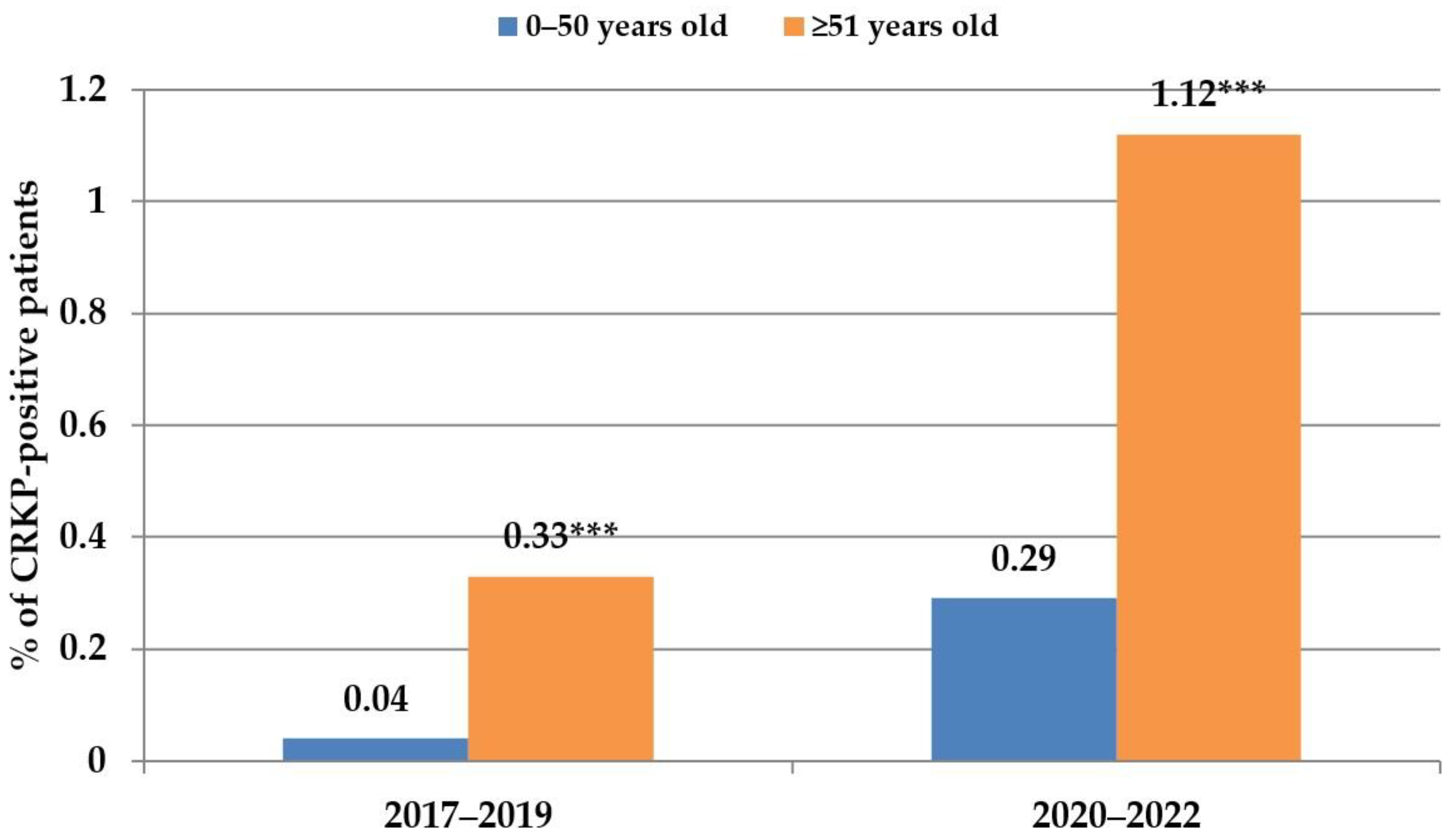
2.2. Carbapenemase-Producing Klebsiella pneumoniae Distribution in Different Age Groups, Hospital Units, and Clinical Samples
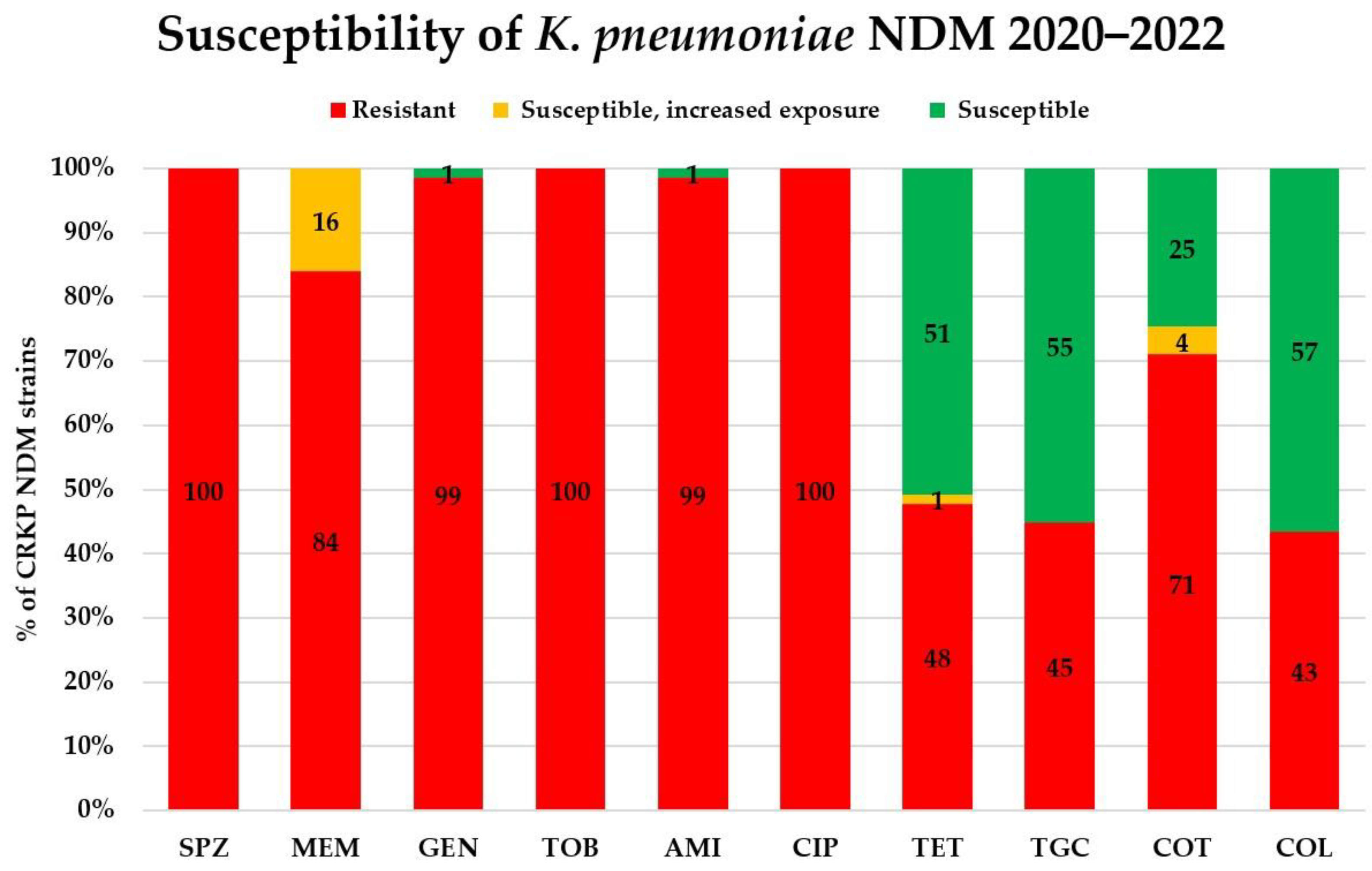
2.3. Antimicrobial Susceptibility of Carbapenemase-Producing Klebsiella pneumoniae
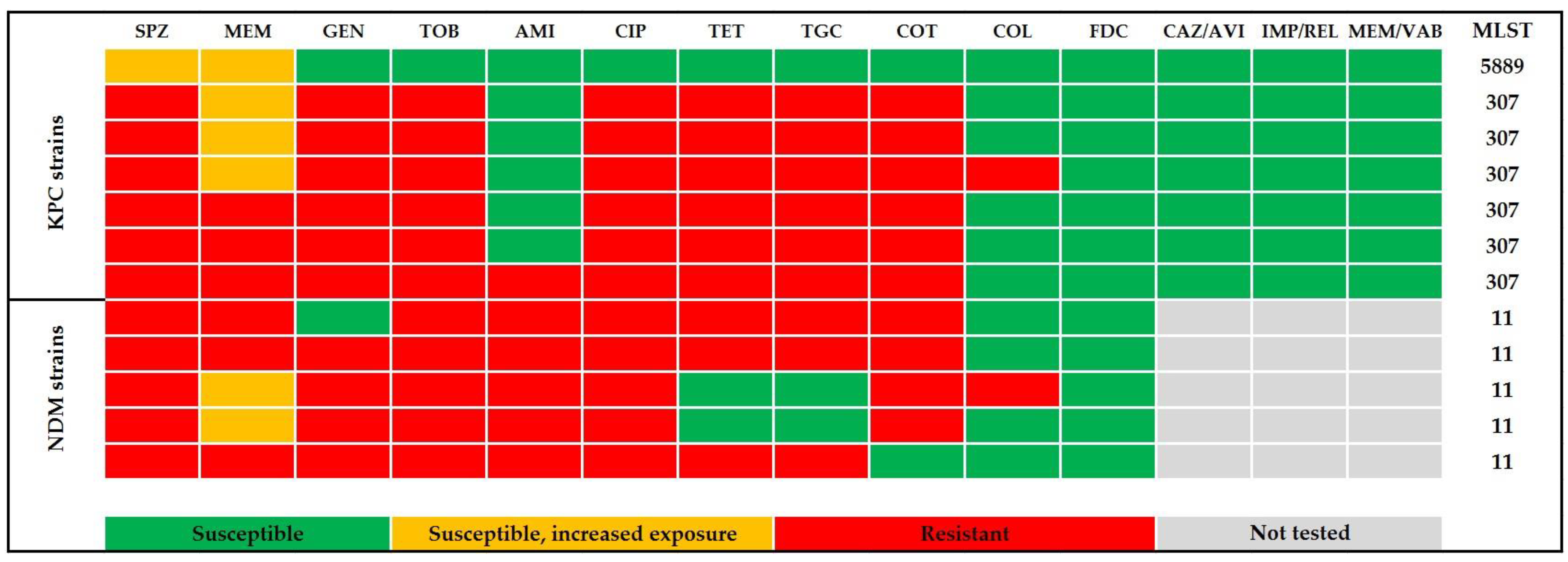
2.4. In Vitro Activity of the New Beta-Lactams
2.5. Genome Sequencing of Selected Carbapenem-Resistant Klebsiella pneumoniae Strains
3. Discussion
4. Materials and Methods
4.1. Data Resources
4.2. Bacterial Strains Isolation, Identification and Long-Term Preservation
4.3. Antimicrobial Susceptibility Testing and Carbapenemase Type Detection
4.4. Genome Analysing of Klebsiella pneumoniae Isolates
4.5. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- David, S.; Reuter, S.; Harris, S.R.; Glasner, C.; Feltwell, T.; Argimon, S.; Abudahab, K.; Goater, R.; Giani, T.; Errico, G.; et al. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat. Microbiol. 2019, 4, 1919–1929. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Zhan, M.; Liu, J.; Wang, Y.; Hou, Y.; Li, C.; Li, J.; Han, X.; Liu, J.; Chen, Y.; et al. Prevalence of Carbapenem-Resistant Klebsiella pneumoniae Infection in a Northern Province in China: Clinical Characteristics, Drug Resistance, and Geographic Distribution. Infect. Drug Resist. 2022, 15, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Koreň, J.; Andrezál, M.; Drahovská, H.; Hubenáková, Z.; Liptáková, A.; Maliar, T. Next-Generation Sequencing of Carbapenem-Resistant Klebsiella pneumoniae Strains Isolated from Patients Hospitalized in the University Hospital Facilities. Antibiotics 2022, 11, 1538. [Google Scholar] [CrossRef] [PubMed]
- Koren, J.; Hubenakova, Z.; Drahovska, H.; Ozaee, E.; Markuskova, B.; Lichvarikova, A. Emergence of extended-spectrum beta-lactamase (ESBL) and/or carbapenemase producing Enterobacteriaceae (CPE) and their antimicrobial resistance. Bratisl. Lek. Listy 2019, 120, 935–940. [Google Scholar]
- Avendano, E.E.; Raman, G.; Chan, J.; McCann, E. Burden of carbapenem non-susceptible infections in high-risk patients: Systematic literature review and meta-analysis. Antimicrob. Resist. Infect. Control 2020, 9, 193. [Google Scholar] [CrossRef]
- Wang, F.; Zou, X.; Zhou, B.; Yin, T.; Wang, P. Clinical characteristics of carbapenem-resistant Klebsiella pneumoniae infection/colonisation in the intensive care unit: A 9-year retrospective study. BMJ Open 2023, 13, e065786. [Google Scholar] [CrossRef]
- Zhen, X.; Stålsby Lundborg, C.; Sun, X.; Gu, S.; Dong, H. Clinical and Economic Burden of Carbapenem-Resistant Infection or Colonization Caused by Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii: A Multicenter Study in China. Antibiotics 2020, 9, 514. [Google Scholar] [CrossRef]
- Dandachi, I.; Azar, E.; Hamouch, R.; Maliha, P.; Abdallah, S.; Kanaan, E.; Badawi, R.; Khairallah, T.; Matar, G.M.; Daoud, Z. Acinetobacter spp. in a Third World Country with Socio-economic and Immigrants Challenges. J. Infect. Dev. Ctries 2019, 13, 948–955. [Google Scholar] [CrossRef]
- Arcari, G.; Raponi, G.; Sacco, F.; Bibbolino, G.; Di Lella, F.M.; Alessandri, F.; Coletti, M.; Trancassini, M.; Deales, A.; Pugliese, F.; et al. Klebsiella pneumoniae infections in COVID-19 patients: A 2-month retrospective analysis in an Italian hospital. Int. J. Antimicrob. Agents 2021, 57, 106245. [Google Scholar] [CrossRef]
- Chatterjee, N.; Nirwan, P.K.; Srivastava, S.; Rati, R.; Sharma, L.; Sharma, P.; Dwivedi, P.; Jaggi, N. Trends in carbapenem resistance in Pre-COVID and COVID times in a tertiary care hospital in North India. Ann. Clin. Microbiol. Antimicrob. 2023, 22, 1. [Google Scholar] [CrossRef]
- Despotovic, A.; Milosevic, B.; Cirkovic, A.; Vujovic, A.; Cucanic, K.; Cucanic, T.; Stevanovic, G. The Impact of COVID-19 on the Profile of Hospital-Acquired Infections in Adult Intensive Care Units. Antibiotics 2021, 10, 1146. [Google Scholar] [CrossRef] [PubMed]
- Karataş, M.; Yaşar-Duman, M.; Tünger, A.; Çilli, F.; Aydemir, Ş.; Özenci, V. Secondary bacterial infections and antimicrobial resistance in COVID-19: Comparative evaluation of pre-pandemic and pandemic-era, a retrospective single center study. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 51. [Google Scholar] [CrossRef] [PubMed]
- Karruli, A.; Boccia, F.; Gagliardi, M.; Patauner, F.; Ursi, M.P.; Sommese, P.; De Rosa, R.; Murino, P.; Ruocco, G.; Corcione, A.; et al. Multidrug-Resistant Infections and Outcome of Critically Ill Patients with Coronavirus Disease 2019: A Single Center Experience. Microb. Drug Resist. 2021, 27, 1167–1175. [Google Scholar] [CrossRef] [PubMed]
- Belvisi, V.; Del Borgo, C.; Vita, S.; Redaelli, P.; Dolce, P.; Pacella, D.; Kertusha, B.; Carraro, A.; Marocco, R.; De Masi, M.; et al. Impact of SARS CoV-2 pandemic on carbapenemase-producing Klebsiella pneumoniae prevention and control programme: Convergent or divergent action? J. Hosp. Infect. 2021, 109, 29–31. [Google Scholar] [CrossRef]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial Stewardship Program, COVID-19, and Infection Control: Spread of Carbapenem-Resistant Klebsiella Pneumoniae Colonization in ICU COVID-19 Patients. What Did Not Work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef]
- Yang, X.; Liu, X.; Li, W.; Shi, L.; Zeng, Y.; Xia, H.; Huang, Q.; Li, J.; Li, X.; Hu, B.; et al. Epidemiological Characteristics and Antimicrobial Resistance Changes of Carbapenem-Resistant Klebsiella pneumoniae and Acinetobacter baumannii under the COVID-19 Outbreak: An Interrupted Time Series Analysis in a Large Teaching Hospital. Antibiotics 2023, 12, 431. [Google Scholar] [CrossRef]
- Pascale, R.; Bussini, L.; Gaibani, P.; Bovo, F.; Fornaro, G.; Lombardo, D.; Ambretti, S.; Pensalfine, G.; Appolloni, L.; Bartoletti, M.; et al. Carbapenem-resistant bacteria in an intensive care unit during the coronavirus disease 2019 (COVID-19) pandemic: A multicenter before-and-after cross-sectional study. Infect. Control Hosp. Epidemiol. 2022, 43, 461–466. [Google Scholar] [CrossRef]
- Barek, M.A.; Aziz, M.A.; Islam, M.S. Impact of age, sex, comorbidities and clinical symptoms on the severity of COVID-19 cases: A meta-analysis with 55 studies and 10,014 cases. Heliyon 2020, 6, e05684. [Google Scholar] [CrossRef]
- Montrucchio, G.; Corcione, S.; Sales, G.; Curtoni, A.; De Rosa, F.; Brazzi, L. Carbapenem-resistant Klebsiella pneumoniae in ICU-admitted COVID-19 patients: Keep an eye on the ball. J. Glob. Antimicrob. Resist. 2020, 23, 398–400. [Google Scholar] [CrossRef]
- Liu, P.; Li, X.; Luo, M.; Xu, X.; Su, K.; Chen, S.; Qing, Y.; Li, Y.; Qiu, J. Risk Factors for Carbapenem-Resistant Klebsiella pneumoniae Infection: A Meta-Analysis. Microb. Drug Resist. 2018, 24, 190–198. [Google Scholar] [CrossRef]
- Mędrzycka-Dąbrowska, W.; Lange, S.; Zorena, K.; Dąbrowski, S.; Ozga, D.; Tomaszek, L. Carbapenem-Resistant Klebsiella pneumoniae Infections in ICU COVID-19 Patients-A Scoping Review. J. Clin. Med. 2021, 10, 2067. [Google Scholar] [CrossRef] [PubMed]
- Pintado, V.; Ruiz-Garbajosa, P.; Escudero-Sanchez, R.; Gioia, F.; Herrera, S.; Vizcarra, P.; Fortún, J.; Cobo, J.; Martín-Dávila, P.; Morosini, M.I.; et al. Carbapenemase-producing Enterobacterales infections in COVID-19 patients. Infect. Dis. 2022, 54, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, I.M.; Dumitrascu, M.; Vlad, N.D.; Cernat, R.C.; Ilie-Serban, C.; Hangan, A.; Slujitoru, R.E.; Gherghina, A.; Mitroi-Maxim, C.; Curtali, L.; et al. Carbapenem-Resistant Klebsiella pneumoniae Associated with COVID-19. Antibiotics 2021, 10, 561. [Google Scholar] [CrossRef] [PubMed]
- Gorrie, C.L.; Mirčeta, M.; Wick, R.R.; Edwards, D.J.; Thomson, N.R.; Strugnell, R.A.; Pratt, N.F.; Garlick, J.S.; Watson, K.M.; Pilcher, D.V.; et al. Gastrointestinal Carriage Is a Major Reservoir of Klebsiella pneumoniae Infection in Intensive Care Patients. Clin. Infect. Dis. 2017, 65, 208–215. [Google Scholar] [CrossRef]
- Messika, J.; La Combe, B.; Ricard, J.D. Oropharyngeal colonization: Epidemiology, treatment and ventilator-associated pneumonia prevention. Ann. Transl. Med. 2018, 6, 426. [Google Scholar] [CrossRef]
- Liao, W.; Liu, Y.; Zhang, W. Virulence evolution, molecular mechanisms of resistance and prevalence of ST11 carbapenem-resistant Klebsiella pneumoniae in China: A review over the last 10 years. J. Glob. Antimicrob. Resist. 2020, 23, 174–180. [Google Scholar] [CrossRef]
- Wang, J.; Feng, Y.; Zong, Z. Worldwide transmission of ST11-KL64 carbapenem-resistant Klebsiella pneumoniae: An analysis of publicly available genomes. mSphere 2023, e0017323. [Google Scholar] [CrossRef]
- Xie, M.; Yang, X.; Xu, Q.; Ye, L.; Chen, K.; Zheng, Z.; Dong, N.; Sun, Q.; Shu, L.; Gu, D.; et al. Clinical evolution of ST11 carbapenem resistant and hypervirulent Klebsiella pneumoniae. Commun. Biol. 2021, 4, 650. [Google Scholar] [CrossRef]
- Xu, M.; Qian, C.; Jia, H.; Feng, L.; Shi, S.; Zhang, Y.; Wang, L.; Cao, J.; Zhou, T.; Zhou, C. Emergence of Ceftazidime-Avibactam Resistance and Decreased Virulence in Carbapenem-Resistant ST11 Klebsiella pneumoniae During Antibiotics Treatment. Infect. Drug Resist. 2022, 15, 6881–6891. [Google Scholar] [CrossRef]
- Heiden, S.E.; Hübner, N.-O.; Bohnert, J.A.; Heidecke, C.-D.; Kramer, A.; Balau, V.; Gierer, W.; Schaefer, S.; Eckmanns, T.; Gatermann, S.; et al. A Klebsiella pneumoniae ST307 outbreak clone from Germany demonstrates features of extensive drug resistance, hypermucoviscosity, and enhanced iron acquisition. Genome Med. 2020, 12, 113. [Google Scholar] [CrossRef]
- Fritzenwanker, M.; Imirzalioglu, C.; Herold, S.; Wagenlehner, F.M.; Zimmer, K.P.; Chakraborty, T. Treatment Options for Carbapenem-Resistant Gram-Negative Infections. Dtsch. Arztebl. Int. 2018, 115, 345–352. [Google Scholar] [CrossRef]
- Zhu, J.; Chen, Y.; Yang, X. Antibiotic Resistance, Molecular Characteristics and Risk Factors of Carbapenem-Resistant Klebsiella pneumoniae in Clinical Isolates. Infect. Drug Resist. 2022, 15, 6671–6680. [Google Scholar] [CrossRef]
- Rodríguez-Baño, J.; Gutiérrez-Gutiérrez, B.; Machuca, I.; Pascual, A. Treatment of Infections Caused by Extended-Spectrum-Beta-Lactamase-, AmpC-, and Carbapenemase-Producing Enterobacteriaceae. Clin. Microbiol. Rev. 2018, 31, e00079-17. [Google Scholar] [CrossRef]
- Karampatakis, T.; Tsergouli, K.; Behzadi, P. Carbapenem-Resistant Klebsiella pneumoniae: Virulence Factors, Molecular Epidemiology and Latest Updates in Treatment Options. Antibiotics 2023, 12, 234. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed Ahmed, M.A.E.G.; Zhong, L.-L.; Shen, C.; Yang, Y.; Doi, Y.; Tian, G.-B. Colistin and its role in the Era of antibiotic resistance: An extended review (2000–2019). Emerg. Microbes Infect. 2020, 9, 868–885. [Google Scholar] [CrossRef] [PubMed]
- Torres, D.A.; Seth-Smith, H.M.B.; Joosse, N.; Lang, C.; Dubuis, O.; Nüesch-Inderbinen, M.; Hinic, V.; Egli, A. Colistin resistance in Gram-negative bacteria analysed by five phenotypic assays and inference of the underlying genomic mechanisms. BMC Microbiol. 2021, 21, 321. [Google Scholar] [CrossRef] [PubMed]
- Yu, L.; Zhang, J.; Fu, Y.; Zhao, Y.; Wang, Y.; Zhao, J.; Guo, Y.; Li, C.; Zhang, X. Synergetic Effects of Combined Treatment of Colistin With Meropenem or Amikacin on Carbapenem-Resistant Klebsiella pneumoniae in vitro. Front. Cell. Infect. Microbiol. 2019, 9, 422. [Google Scholar] [CrossRef] [PubMed]
- Paul, M.; Daikos, G.L.; Durante-Mangoni, E.; Yahav, D.; Carmeli, Y.; Benattar, Y.D.; Skiada, A.; Andini, R.; Eliakim-Raz, N.; Nutman, A.; et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: An open-label, randomised controlled trial. Lancet Infect. Dis. 2018, 18, 391–400. [Google Scholar] [CrossRef] [PubMed]
- Geng, T.T.; Xu, X.; Huang, M. High-dose tigecycline for the treatment of nosocomial carbapenem-resistant Klebsiella pneumoniae bloodstream infections: A retrospective cohort study. Medicine 2018, 97, e9961. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Chen, Q.; Shen, F.; Jiang, Y.; Wu, X.; Hua, X.; Fu, Y.; Yu, Y. Resistance evolution of hypervirulent carbapenem-resistant Klebsiella pneumoniae ST11 during treatment with tigecycline and polymyxin. Emerg. Microbes Infect. 2021, 10, 1129–1136. [Google Scholar] [CrossRef]
- Bulik, C.C.; Nicolau, D.P. Double-carbapenem therapy for carbapenemase-producing Klebsiella pneumoniae. Antimicrob. Agents Chemother. 2011, 55, 3002–3004. [Google Scholar] [CrossRef]
- Tan, X.; Kim, H.S.; Baugh, K.; Huang, Y.; Kadiyala, N.; Wences, M.; Singh, N.; Wenzler, E.; Bulman, Z.P. Therapeutic Options for Metallo-beta-Lactamase-Producing Enterobacterales. Infect. Drug Resist. 2021, 14, 125–142. [Google Scholar] [CrossRef]
- Marshall, S.; Hujer, A.M.; Rojas, L.J.; Papp-Wallace, K.M.; Humphries, R.M.; Spellberg, B.; Hujer, K.M.; Marshall, E.K.; Rudin, S.D.; Perez, F.; et al. Can Ceftazidime-Avibactam and Aztreonam Overcome beta-Lactam Resistance Conferred by Metallo-beta-Lactamases in Enterobacteriaceae? Antimicrob. Agents Chemother. 2017, 61, e02243-16. [Google Scholar] [CrossRef]
- Mauri, C.; Maraolo, A.E.; Di Bella, S.; Luzzaro, F.; Principe, L. The Revival of Aztreonam in Combination with Avibactam against Metallo-beta-Lactamase-Producing Gram-Negatives: A Systematic Review of In Vitro Studies and Clinical Cases. Antibiotics 2021, 10, 1012. [Google Scholar] [CrossRef] [PubMed]
- Spaziante, M.; Oliva, A.; Ceccarelli, G.; Venditti, M. What are the treatment options for resistant Klebsiella pneumoniae carbapenemase (KPC)-producing bacteria? Expert Opin. Pharmacother. 2020, 21, 1781–1787. [Google Scholar] [CrossRef]
- Jean, S.S.; Harnod, D.; Hsueh, P.R. Global Threat of Carbapenem-Resistant Gram-Negative Bacteria. Front. Cell. Infect. Microbiol. 2022, 12, 823684. [Google Scholar] [CrossRef] [PubMed]
- Wu, N.; Chen, L.K.; Zhu, T. Phage therapy for secondary bacterial infections with COVID-19. Curr. Opin. Virol. 2022, 52, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Zurabov, F.M.; Chernevskaya, E.A.; Beloborodova, N.V.; Zurabov, A.Y.; Petrova, M.V.; Yadgarov, M.Y.; Popova, V.M.; Fatuev, O.E.; Zakharchenko, V.E.; Gurkova, M.M.; et al. Bacteriophage Cocktails in the Post-COVID Rehabilitation. Viruses 2022, 14, 2614. [Google Scholar] [CrossRef]
- FDA Allows Phage Therapy for COVID19 Patients. Available online: https://www.bacteriophage.news/fda-phage-therapy-for-covid19-patients/ (accessed on 27 June 2023).
- Loc-Carrillo, C.; Abedon, S.T. Pros and cons of phage therapy. Bacteriophage 2011, 1, 111–114. [Google Scholar] [CrossRef]
- Gattringer, R.; Nikš, M.; Ostertág, R.; Schwarz, K.; Medvedovic, H.; Graninger, W.; Georgopoulos, A. Evaluation of MIDITECH automated colorimetric MIC reading for antimicrobial susceptibility testing. J. Antimicrob. Chemother. 2002, 49, 651–659. [Google Scholar] [CrossRef]
- EUCAST Breakpoint Tables for Interpretation oh MICs and Zone Diameters. Version 13.0.2023. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_13.0_Breakpoint_Tables.pdf (accessed on 27 June 2023).
- EUCAST Guidelines for Detection of Resistance Mechanisms and Specific Resistances of Clinical and/or Epidemiological Importance, Version 2.01. 2017. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Resistance_mechanisms/EUCAST_detection_of_resistance_mechanisms_170711.pdf (accessed on 27 June 2023).
- Prjibelski, A.; Antipov, D.; Meleshko, D.; Lapidus, A.; Korobeynikov, A. Using SPAdes De Novo Assembler. Curr. Protoc. Bioinform. 2020, 70, e102. [Google Scholar] [CrossRef] [PubMed]




| Ceftazidime–Avibactam MIC [mg/L] | KPC (n) | Imipenem–Relebactam MIC [mg/L] | KPC (n) | Meropenem–Vaborbaktam MIC [mg/L] | KPC (n) |
|---|---|---|---|---|---|
| 0.032 | 1 | 0.094 | 1 | 0.023 | 3 |
| 0.094 | 1 | 0.125 | 2 | 0.032 | 3 |
| 0.190 | 2 | 0.190 | 1 | 0.047 | 1 |
| 0.380 | 1 | 0.250 | 1 | ||
| 0.750 | 2 | 0.380 | 1 | ||
| 0.5 | 1 |
| Cefiderocol MIC [mg/L] | KPC (n) | NDM (n) |
|---|---|---|
| 0.016 | 1 | - |
| 0.032 | 4 | - |
| 0.064 | 1 | 1 |
| 0.094 | 1 | 1 |
| 0.19 | - | 2 |
| 0.25 | - | 1 |
| Sublineage | ST | Clonal Group | Serotype (wzi) 1 | Carbapenemase Gene | No. of Strains |
|---|---|---|---|---|---|
| SL-258 | 11 | CG340 | K15:O4 (50) | NDM-1 | 4 |
| CG3666 | ? (24) | NDM-1 | 1 | ||
| SL-307 | 307 | CG307 | K2:O1/2 (173) | KPC-2 | 6 |
| SL-10716 | 5889 | CG11340 | K14/15:O3 (new) | KPC-2 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ficik, J.; Andrezál, M.; Drahovská, H.; Böhmer, M.; Szemes, T.; Liptáková, A.; Slobodníková, L. Carbapenem-Resistant Klebsiella pneumoniae in COVID-19 Era—Challenges and Solutions. Antibiotics 2023, 12, 1285. https://doi.org/10.3390/antibiotics12081285
Ficik J, Andrezál M, Drahovská H, Böhmer M, Szemes T, Liptáková A, Slobodníková L. Carbapenem-Resistant Klebsiella pneumoniae in COVID-19 Era—Challenges and Solutions. Antibiotics. 2023; 12(8):1285. https://doi.org/10.3390/antibiotics12081285
Chicago/Turabian StyleFicik, Jozef, Michal Andrezál, Hana Drahovská, Miroslav Böhmer, Tomáš Szemes, Adriána Liptáková, and Lívia Slobodníková. 2023. "Carbapenem-Resistant Klebsiella pneumoniae in COVID-19 Era—Challenges and Solutions" Antibiotics 12, no. 8: 1285. https://doi.org/10.3390/antibiotics12081285
APA StyleFicik, J., Andrezál, M., Drahovská, H., Böhmer, M., Szemes, T., Liptáková, A., & Slobodníková, L. (2023). Carbapenem-Resistant Klebsiella pneumoniae in COVID-19 Era—Challenges and Solutions. Antibiotics, 12(8), 1285. https://doi.org/10.3390/antibiotics12081285







