Evaluating the Translational Potential of Bacteriocins as an Alternative Treatment for Staphylococcus aureus Infections in Animals and Humans
Abstract
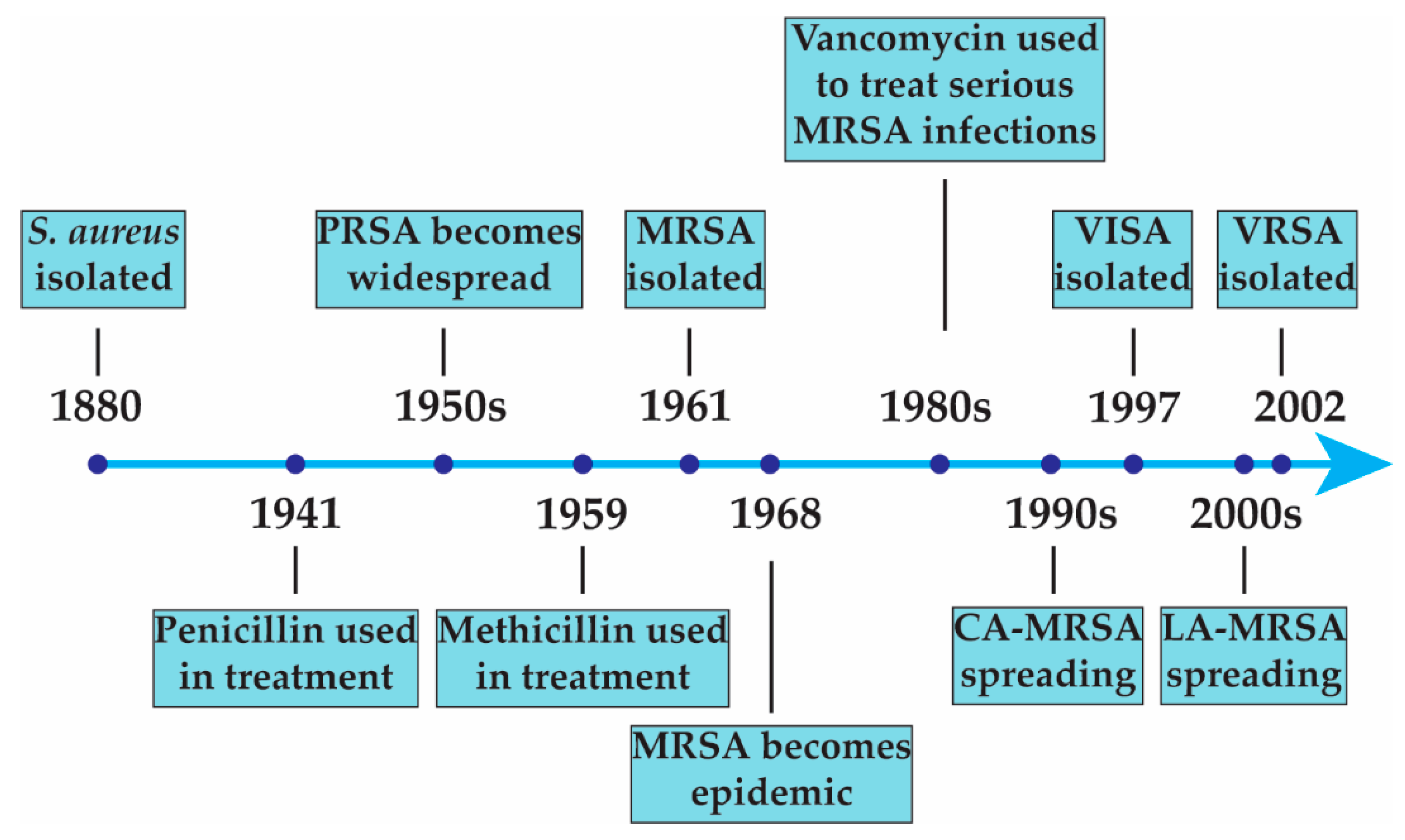
1. Introduction
2. Bacteriocins
2.1. Background
2.2. The Strengths and Limitations of Bacteriocins
3. In Vivo Experiments Evaluating the Efficacy of Bacteriocins against S. aureus Infections
3.1. Skin Infection Models
3.2. Respiratory Infection Models
3.3. Systemic Infection and Other Severe Infection Models
3.4. Nasal, Intestinal, and Skin Carriage
4. Additional Applications of Bacteriocins against S. aureus
4.1. Industrial Applications
4.2. Bacteriocins against S. aureus in Clinical Trials
| Identifier or Citation | Intervention | Proposed Sample Size/Enrollment | Primary Endpoint(s) | Status | Results |
|---|---|---|---|---|---|
| Fernández, et al. [173] | Application of a nisin solution (6 μg/mL) to the nipple and mammary areola | 8 lactating women with clinical signs of staphylococcal mastitis | Evaluate the clinical signs of mastitis and bacterial loads after 2 weeks | Complete | Bacterial load in the nisin group was statistically lower than the control group. No clinical signs of staphylococcal mastitis were observed in the nisin group on day 14 of the trial |
| Clinical Trials.gov NCT02467972 | One of the experimental groups had a dietary supplement of nisin. Nisin was added to ready-to-eat frozen soups (3 times/week with 18 portions in total) | 61 healthy participants | Change in bowel function, colonic bacteria population, and hormonal parameters related to hunger and satiety after six weeks | Complete | Not available |
| Clinical Trials.gov NCT02928042 | Tracheal aspiration-derived pathogens were treated with LAB members and nisin to evaluate their effectiveness at treating ventilator-associated pneumonia | 80 patients who were mechanically ventilated for at least 48 h were recruited and who had their tracheal aspirate cultures used for the study | The antimicrobial properties and effects of nisin and LAB members on P. aeruginosa, A. baumannii, K. pneumonia, and S. aureus growth rate | Complete | Not available |
| EudraCT/CTIS 2011-002703-14 | Part A: a single dose (100 mg) of NVB302 or a placebo Part B: Once daily doses of NVB302 or a placebo for ten days | Part A: Up to five cohorts of 8 healthy subjects Part B: Up to four cohorts of 8 healthy subjects | Assessment of the safety and tolerability of single and multiple oral ascending doses of NVB302 | Complete | Not available |
5. Conclusions
| Bacteriocin | Peptide Sequence | Mechanism of Action | Reference |
|---|---|---|---|
| Mutacin 1140 | 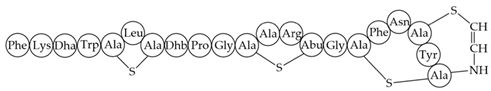 | Inhibition of cell wall synthesis, pore formation | [107,176,177,178] |
| Epidermicin NI01 | MAAFMKLIQFLATLGQKYVSLAWKHKGTILKWINAGQSFEWIYKQIKKLWAR (unmodified) | Multi-mode pore formation induced by four-helices | [127,179] |
| Nisin (Nisin A) |  Nisin F: Nisin A H27N; Nisin Z: Nisin A H27N, I30V | Inhibition of cell wall synthesis, pore formation | [105,180,181,182,183] |
| NAI-107 (Microbisporicin) | 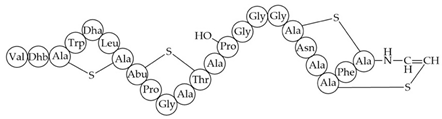 | Inhibition of cell wall synthesis | [118] |
| CMB001 |  | Unknown | [141,184] |
| Garvicin KS | Three-component: GakA, MGAIIKAGAKIVGKGVLGGGASWLGWNVGEKIWK GakB, MGAIIKAGAKIIGKGLLGGAAGGATYGGLKKIFG GakC, MGAIIKAGAKIVGKGALTGGGVWLAEKLFGGK (unmodified) | Unknown | [185] |
| Micrococcin P1 | 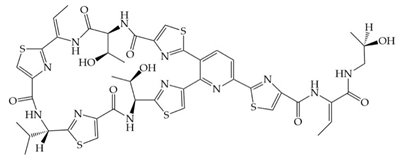 | Inhibition of ribosomal protein synthesis | [186] |
| Lysostaphin | 26.9 kDa protein in mature form | Cleaving of pentaglycine bridges in the cell wall | [187,188] |
| NVB333 |  | Inhibition of cell wall synthesis | [103] |
| Clausin | 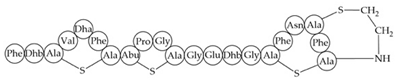 | Inhibition of cell wall synthesis | [47] |
| Amyloliquecidin |
Two-component lantibiotic, exact structure unknown, primary amino acid sequences: CAWYDISCKLGNKGAWCTLTVECQSSCN, TTPSSLPCGVFVTAAFCPSTKCTSSC | Inhibition of cell wall synthesis | [48] |
| Mersacidin |  | Inhibition of cell wall synthesis | [45,189] |
| Lacticin NK34 | 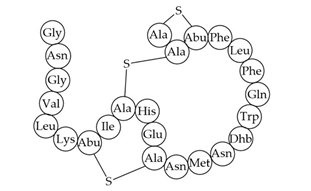 | Inhibition of cell wall synthesis | [112] |
| Lacticin 3147 | 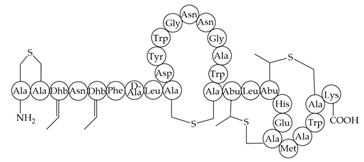 | Inhibition of cell wall synthesis | [46,190] |
| Lugdunin | 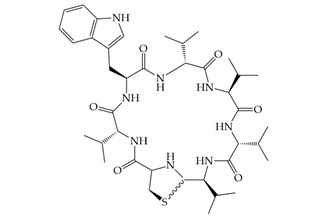 | Disrupts membrane potential | [99] |
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance; World Health Organization: Geneva, Switzerland, 2014; 256p. [Google Scholar]
- Noble, W.C.; Valkenburg, H.A.; Wolters, C.H.L. Carriage of Staphylococcus aureus in random samples of a normal population. Epidemiology Infect. 1967, 65, 567–573. [Google Scholar] [CrossRef] [PubMed]
- Acton, D.S.; Plat-Sinnige, M.J.T.; Van Wamel, W.; De Groot, N.; Van Belkum, A. Intestinal carriage of Staphylococcus aureus: How does its frequency compare with that of nasal carriage and what is its clinical impact? Eur. J. Clin. Microbiol. Infect. Dis. 2009, 28, 115–127. [Google Scholar] [CrossRef]
- Tuazon, C.U.; Perez, A.; Kishaba, T.; Sheagren, J.N. Staphylococcus aureus Among Insulin-Injecting Diabetic Patients. JAMA 1975, 231, 1272. [Google Scholar] [CrossRef] [PubMed]
- Weinke, T.; Schiller, R.; Fehrenbach, F.J.; Pohle, H.D. Association between Staphylococcus aureus nasopharyngeal colonization and septicemia in patients infected with the human immunodeficiency virus. Eur. J. Clin. Microbiol. Infect. Dis. 1992, 11, 985–989. [Google Scholar] [CrossRef]
- Kluytmans, J.A.J.W.; Mouton, J.W.; Ijzerman, E.P.F.; Vandenbroucke-Grauls, C.M.J.E.; Maat, A.W.P.M.; Wagenvoort, J.H.T.; Verbrugh, H.A. Nasal Carriage of Staphylococcus aureus as a Major Risk Factor for Wound Infections after Cardiac Surgery. J. Infect. Dis. 1995, 171, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Yu, V.L.; Goetz, A.; Wagener, M.; Smith, P.B.; Rihs, J.D.; Hanchett, J.; Zuravleff, J.J. Staphylococcus aureus Nasal Carriage and Infection in Patients on Hemodialysis. N. Engl. J. Med. 1986, 315, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.Y.C.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G., Jr. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef]
- Giesbrecht, P.; Kersten, T.; Maidhof, H.; Wecke, J. Staphylococcal Cell Wall: Morphogenesis and Fatal Variations in the Presence of Penicillin. Microbiol. Mol. Biol. Rev. 1998, 62, 1371–1414. [Google Scholar] [CrossRef]
- Chambers, H.F. Methicillin resistance in staphylococci: Molecular and biochemical basis and clinical implications. Clin. Microbiol. Rev. 1997, 10, 781–791. [Google Scholar] [CrossRef]
- Hackbarth, C.J.; Kocagoz, T.; Kocagoz, S.; Chambers, H.F. Point mutations in Staphylococcus aureus PBP 2 gene affect penicillin-binding kinetics and are associated with resistance. Antimicrob. Agents Chemother. 1995, 39, 103–106. [Google Scholar] [CrossRef]
- DeLeo, F.R.; Chambers, H.F. Reemergence of antibiotic-resistant Staphylococcus aureus in the genomics era. J. Clin. Investig. 2009, 119, 2464–2474. [Google Scholar] [CrossRef]
- Otto, M. Understanding the epidemic of community-associated MRSA and finding a cure: Are we asking the right questions? Expert Rev. Anti-Infect. Ther. 2009, 7, 141–143. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fitzgerald, J.R. Livestock-associated Staphylococcus aureus: Origin, evolution and public health threat. Trends Microbiol. 2012, 20, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Barna, J.C.J.; Williams, D.H. The structure and mode of action of glycopeptide antibiotics of the vancomycin group. Annu. Rev. Microbiol. 1984, 38, 339–357. [Google Scholar] [CrossRef]
- Maple, P.; Hamilton-Miller, J.; Brumfitt, W. World-wide antibiotic resistance in methicillin-resistant Staphylococcus aureus. Lancet 1989, 333, 537–540. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.P. Vancomycin: A History. Clin. Infect. Dis. 2006, 42, S5–S12. [Google Scholar] [CrossRef]
- Hiramatsu, K.; Hanaki, H.; Ino, T.; Yabuta, K.; Oguri, T.; Tenover, F.C. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J. Antimicrob. Chemother. 1997, 40, 135–136. [Google Scholar] [CrossRef]
- Jackson, M.A.; Hicks, R.A. Vancomycin failure in staphylococcal endocarditis. Pediatr. Infect. Dis. J. 1987, 6, 750–751. [Google Scholar] [CrossRef]
- Chang, S.; Sievert, D.M.; Hageman, J.C.; Boulton, M.L.; Tenover, F.C.; Downes, F.P.; Shah, S.; Rudrik, J.T.; Pupp, G.R.; Brown, W.J.; et al. Infection with Vancomycin-Resistant Staphylococcus aureus Containing the vanA Resistance Gene. N. Engl. J. Med. 2003, 348, 1342–1347. [Google Scholar] [CrossRef]
- Howden, B.P.; Davies, J.K.; Johnson, P.D.R.; Stinear, T.P.; Grayson, M.L. Reduced Vancomycin Susceptibility in Staphylococcus aureus, Including Vancomycin-Intermediate and Heterogeneous Vancomycin-Intermediate Strains: Resistance Mechanisms, Laboratory Detection, and Clinical Implications. Clin. Microbiol. Rev. 2010, 23, 99–139. [Google Scholar] [CrossRef]
- Arthur, M.; Molinas, C.; Depardieu, F.; Courvalin, P. Characterization of Tn1546, a Tn3-related transposon conferring glycopeptide resistance by synthesis of depsipeptide peptidoglycan precursors in Enterococcus faecium BM4147. J. Bacteriol. 1993, 175, 117–127. [Google Scholar] [CrossRef]
- Foucault, M.-L.; Courvalin, P.; Grillot-Courvalin, C. Fitness Cost of VanA-Type Vancomycin Resistance in Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2009, 53, 2354–2359. [Google Scholar] [CrossRef]
- Weber, S.G.; Gold, H.S.; Hooper, D.C.; Karchmer, A.; Carmeli, Y. Fluoroquinolones and the Risk for Methicillin-resistant Staphylococcus aureus in Hospitalized Patients. Emerg. Infect. Dis. 2003, 9, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Lowy, F.D. Antimicrobial resistance: The example of Staphylococcus aureus. J. Clin. Investig. 2003, 111, 1265–1273. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Onodera, Y.; Lee, J.C.; Hooper, D.C. NorB, an Efflux Pump in Staphylococcus aureus Strain MW2, Contributes to Bacterial Fitness in Abscesses. J. Bacteriol. 2008, 190, 7123–7129. [Google Scholar] [CrossRef]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad Bugs, No Drugs: No ESKAPE! An Update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cotter, P.D.; Ross, R.; Hill, C. Bacteriocins—A viable alternative to antibiotics? Nat. Rev. Genet. 2012, 11, 95–105. [Google Scholar] [CrossRef]
- Piewngam, P.; Otto, M. Probiotics to prevent Staphylococcus aureus disease? Gut Microbes 2019, 11, 94–101. [Google Scholar] [CrossRef]
- Piewngam, P.; Zheng, Y.; Nguyen, T.H.; Dickey, S.W.; Joo, H.-S.; Villaruz, A.E.; Glose, K.A.; Fisher, E.L.; Hunt, R.L.; Li, B.; et al. Pathogen elimination by probiotic Bacillus via signalling interference. Nature 2018, 562, 532–537. [Google Scholar] [CrossRef]
- Pulingam, T.; Parumasivam, T.; Gazzali, A.M.; Sulaiman, A.M.; Chee, J.Y.; Lakshmanan, M.; Chin, C.F.; Sudesh, K. Antimicrobial resistance: Prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur. J. Pharm. Sci. 2021, 170, 106103. [Google Scholar] [CrossRef]
- Ebner, P.; Reichert, S.; Luqman, A.; Krismer, B.; Popella, P.; Götz, F. Lantibiotic production is a burden for the producing staphylococci. Sci. Rep. 2018, 8, 7471. [Google Scholar] [CrossRef] [PubMed]
- Maldonado-Barragán, A.; West, S.A. The cost and benefit of quorum sensing-controlled bacteriocin production in Lactobacillus plantarum. J. Evol. Biol. 2019, 33, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Heilbronner, S.; Krismer, B.; Brötz-Oesterhelt, H.; Peschel, A. The microbiome-shaping roles of bacteriocins. Nat. Rev. Genet. 2021, 19, 726–739. [Google Scholar] [CrossRef] [PubMed]
- Klaenhammer, T.R. Bacteriocins of lactic acid bacteria. Biochimie 1988, 70, 337–349. [Google Scholar] [CrossRef] [PubMed]
- Riley, M.A. Molecular mechanisms of bacteriocin evolution. Annu. Rev. Genet. 1998, 32, 255–278. [Google Scholar] [CrossRef]
- Cotter, P.D.; Hill, C.; Ross, R.P. Bacteriocins: Developing innate immunity for food. Nat. Rev. Genet. 2005, 3, 777–788. [Google Scholar] [CrossRef]
- Jack, R.W.; Tagg, J.R.; Ray, B. Bacteriocins of gram-positive bacteria. Microbiol. Rev. 1995, 59, 171–200. [Google Scholar] [CrossRef]
- Klaenhammer, T.R. Genetics of bacteriocins produced by lactic acid bacteria. FEMS Microbiol. Rev. 1993, 12, 39–85. [Google Scholar] [CrossRef]
- Kumariya, R.; Garsa, A.K.; Rajput, Y.; Sood, S.; Akhtar, N.; Patel, S. Bacteriocins: Classification, synthesis, mechanism of action and resistance development in food spoilage causing bacteria. Microb. Pathog. 2019, 128, 171–177. [Google Scholar] [CrossRef]
- Mathur, H.; Rea, M.; Cotter, P.; Hill, C.; Ross, R. The Sactibiotic Subclass of Bacteriocins: An Update. Curr. Protein Pept. Sci. 2015, 16, 549–558. [Google Scholar] [CrossRef]
- Mokoena, M.P. Lactic Acid Bacteria and Their Bacteriocins: Classification, Biosynthesis and Applications against Uropathogens: A Mini-Review. Molecules 2017, 22, 1255. [Google Scholar] [CrossRef] [PubMed]
- Wiedemann, I.; Breukink, E.; van Kraaij, C.; Kuipers, O.P.; Bierbaum, G.; de Kruijff, B.; Sahl, H.-G. Specific Binding of Nisin to the Peptidoglycan Precursor Lipid II Combines Pore Formation and Inhibition of Cell Wall Biosynthesis for Potent Antibiotic Activity. J. Biol. Chem. 2001, 276, 1772–1779. [Google Scholar] [CrossRef]
- Hsu, S.-T.D.; Breukink, E.; Tischenko, E.; Lutters, M.A.G.; De Kruijff, B.; Kaptein, R.; Bonvin, A.M.; Van Nuland, N.A. The nisin–lipid II complex reveals a pyrophosphate cage that provides a blueprint for novel antibiotics. Nat. Struct. Mol. Biol. 2004, 11, 963–967. [Google Scholar] [CrossRef]
- Brötz, H.; Bierbaum, G.; Leopold, K.; Reynolds, P.E.; Sahl, H.-G. The Lantibiotic Mersacidin Inhibits Peptidoglycan Synthesis by Targeting Lipid II. Antimicrob. Agents Chemother. 1998, 42, 154–160. [Google Scholar] [CrossRef]
- Wiedemann, I.; Bottiger, T.; Bonelli, R.R.; Wiese, A.; Hagge, S.O.; Gutsmann, T.; Seydel, U.; Deegan, L.; Hill, C.; Ross, P.; et al. The mode of action of the lantibiotic lacticin 3147—A complex mechanism involving specific interaction of two peptides and the cell wall precursor lipid II. Mol. Microbiol. 2006, 61, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Bouhss, A.; Al-Dabbagh, B.; Vincent, M.; Odaert, B.; Aumont-Nicaise, M.; Bressolier, P.; Desmadril, M.; Mengin-Lecreulx, D.; Urdaci, M.C.; Gallay, J. Specific Interactions of Clausin, a New Lantibiotic, with Lipid Precursors of the Bacterial Cell Wall. Biophys. J. 2009, 97, 1390–1397. [Google Scholar] [CrossRef]
- Van Staden, A.D.P. In Vitro and In Vivo Characterization of Amyloliquecidin, a Novel Two-Component Lantibiotic Produced by Bacillus Amyloliquefaciens; Stellenbosch University: Stellenbosch, South Africa, 2015. [Google Scholar]
- Cleveland, J.; Montville, T.J.; Nes, I.F.; Chikindas, M.L. Bacteriocins: Safe, natural antimicrobials for food preservation. Int. J. Food Microbiol. 2001, 71, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Perez, R.H.; Zendo, T.; Sonomoto, K. Novel bacteriocins from lactic acid bacteria (LAB): Various structures and applications. Microb. Cell Factories 2014, 13, S3. [Google Scholar] [CrossRef]
- Jiang, H.; Zou, J.; Cheng, H.; Fang, J.; Huang, G. Purification, Characterization, and Mode of Action of Pentocin JL-1, a Novel Bacteriocin Isolated from Lactobacillus pentosus, against Drug-Resistant Staphylococcus aureus. BioMed Res. Int. 2017, 2017, 7657190. [Google Scholar] [CrossRef]
- Soltani, S.; Hammami, R.; Cotter, P.D.; Rebuffat, S.; Said, L.B.; Gaudreau, H.; Bédard, F.; Biron, E.; Drider, D.; Fliss, I. Bacteriocins as a new generation of antimicrobials: Toxicity aspects and regulations. FEMS Microbiol. Rev. 2021, 45, fuaa039. [Google Scholar] [CrossRef]
- Newstead, L.L.; Varjonen, K.; Nuttall, T.; Paterson, G.K. Staphylococcal-Produced Bacteriocins and Antimicrobial Peptides: Their Potential as Alternative Treatments for Staphylococcus aureus Infections. Antibiotics 2020, 9, 40. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.R.; Coburn, P.S.; Gilmore, M.S. Enterococcal Cytolysin: A Novel Two Component Peptide System that Serves as a Bacterial Defense Against Eukaryotic and Prokaryotic Cells. Curr. Protein Pept. Sci. 2005, 6, 77–84. [Google Scholar] [CrossRef] [PubMed]
- Vaucher, R.d.A.; Gewehr, C.d.C.V.; Correa, A.P.F.; Sant‘anna, V.; Ferreira, J.; Brandelli, A. Evaluation of the immunogenicity and in vivo toxicity of the antimicrobial peptide P34. Int. J. Pharm. 2011, 421, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Hols, P.; Ledesma-García, L.; Gabant, P.; Mignolet, J. Mobilization of Microbiota Commensals and Their Bacteriocins for Therapeutics. Trends Microbiol. 2019, 27, 690–702. [Google Scholar] [CrossRef] [PubMed]
- Mesa-Pereira, B.; Rea, M.C.; Cotter, P.D.; Hill, C.; Ross, R.P. Heterologous Expression of Biopreservative Bacteriocins with a View to Low Cost Production. Front. Microbiol. 2018, 9, 1654. [Google Scholar] [CrossRef] [PubMed]
- Field, D.; Gaudin, N.; Lyons, F.; O’Connor, P.M.; Cotter, P.D.; Hill, C.; Ross, R.P. A Bioengineered Nisin Derivative to Control Biofilms of Staphylococcus pseudintermedius. PLoS ONE 2015, 10, e0119684. [Google Scholar] [CrossRef]
- Field, D.; Connor, P.M.O.; Cotter, P.D.; Hill, C.; Ross, R.P. The generation of nisin variants with enhanced activity against specific Gram-positive pathogens. Mol. Microbiol. 2008, 69, 218–230. [Google Scholar] [CrossRef]
- Sabo, S.D.S.; Lopes, A.M.; Santos-Ebinuma, V.D.C.; Rangel-Yagui, C.D.O.; Oliveira, R.P.D.S. Bacteriocin partitioning from a clarified fermentation broth of Lactobacillus plantarum ST16Pa in aqueous two-phase systems with sodium sulfate and choline-based salts as additives. Process. Biochem. 2018, 66, 212–221. [Google Scholar] [CrossRef]
- da Silva Sabo, S.; Vitolo, M.; González, J.M.D.; de Souza Oliveira, R.P. Overview of Lactobacillus plantarum as a promising bacteriocin producer among lactic acid bacteria. Food Res. Int. 2014, 64, 527–536. [Google Scholar] [CrossRef]
- Guyonnet, D.; Fremaux, C.; Cenatiempo, Y.; Berjeaud, J.M. Method for Rapid Purification of Class IIa Bacteriocins and Comparison of Their Activities. Appl. Environ. Microbiol. 2000, 66, 1744–1748. [Google Scholar] [CrossRef]
- Deshpande, A.; Pasupuleti, V.; Thota, P.; Pant, C.; Rolston, D.D.K.; Sferra, T.J.; Hernandez, A.V.; Donskey, C.J. Community-associated Clostridium difficile infection and antibiotics: A meta-analysis. J. Antimicrob. Chemother. 2013, 68, 1951–1961. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, M.H.; Mooney, L.; Bendall, R.; Settle, C.D.; Fawley, W.N. A case-control study of community-associated Clostridium difficile infection. J. Antimicrob. Chemother. 2008, 62, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H. Broad-Spectrum Antimicrobials and the Treatment of Serious Bacterial Infections: Getting It Right up Front. Clin. Infect. Dis. 2008, 47 (Suppl. 1), S3–S13. [Google Scholar] [CrossRef]
- Kollef, M.H.; Sherman, G.; Ward, S.; Fraser, V.J. Inadequate Antimicrobial Treatment of Infections. Chest 1999, 115, 462–474. [Google Scholar] [CrossRef]
- Mitchell, D.H.; Howden, B.P. Diagnosis and management of Staphylococcus aureus bacteraemia. Intern. Med. J. 2005, 35, S17–S24. [Google Scholar] [CrossRef]
- Rhee, C.; Kadri, S.S.; Dekker, J.P.; Danner, R.L.; Chen, H.-C.; Fram, D.; Zhang, F.; Wang, R.; Klompas, M.; For The Cdc Prevention Epicenters Program. Prevalence of Antibiotic-Resistant Pathogens in Culture-Proven Sepsis and Outcomes Associated With Inadequate and Broad-Spectrum Empiric Antibiotic Use. JAMA Netw. Open 2020, 3, e202899. [Google Scholar] [CrossRef]
- Barbosa, A.A.T.; de Melo, M.R.; da Silva, C.M.R.; Jain, S.; Dolabella, S.S. Nisin resistance in Gram-positive bacteria and approaches to circumvent resistance for successful therapeutic use. Crit. Rev. Microbiol. 2021, 47, 376–385. [Google Scholar] [CrossRef]
- Van Schaik, W.; Gahan, C.G.; Hill, C. Acid-adapted Listeria monocytogenes displays enhanced tolerance against the lantibiotics nisin and lacticin 3147. J. Food Prot. 1999, 62, 536–539. [Google Scholar] [CrossRef]
- Mantovani, H.C.; Russell, J.B. Nisin Resistance of Streptococcus bovis. Appl. Environ. Microbiol. 2001, 67, 808–813. [Google Scholar] [CrossRef] [PubMed]
- de Freire Bastos, M.D.C.; Coelho, M.L.V.; Da Silva Santos, O.C. Resistance to bacteriocins produced by Gram-positive bacteria. Microbiology 2015, 161, 683–700. [Google Scholar] [CrossRef]
- Jarvis, B. Resistance to Nisin and Production of Nisin-Inactivating Enzymes by Several Bacillus Species. J. Gen. Microbiol. 1967, 47, 33–48. [Google Scholar] [CrossRef][Green Version]
- Collins, B.; Guinane, C.M.; Cotter, P.D.; Hill, C.; Ross, R.P. Assessing the Contributions of the LiaS Histidine Kinase to the Innate Resistance of Listeria monocytogenes to Nisin, Cephalosporins, and Disinfectants. Appl. Environ. Microbiol. 2012, 78, 2923–2929. [Google Scholar] [CrossRef]
- Dicks, L.M.T.; Dreyer, L.; Smith, C.; Van Staden, A.D. A Review: The Fate of Bacteriocins in the Human Gastro-Intestinal Tract: Do They Cross the Gut–Blood Barrier? Front. Microbiol. 2018, 9, 2297. [Google Scholar] [CrossRef]
- Meade, E.; Slattery, M.A.; Garvey, M. Bacteriocins, Potent Antimicrobial Peptides and the Fight against Multi Drug Resistant Species: Resistance is Futile? Antibiotics 2020, 9, 32. [Google Scholar] [CrossRef] [PubMed]
- Walsh, L.; Johnson, C.N.; Hill, C.; Ross, R.P. Efficacy of Phage- and Bacteriocin-Based Therapies in Combatting Nosocomial MRSA Infections. Front. Mol. Biosci. 2021, 8, 654038. [Google Scholar] [CrossRef] [PubMed]
- Blake, K.L.; Randall, C.P.; O’Neill, A.J. In Vitro Studies Indicate a High Resistance Potential for the Lantibiotic Nisin in Staphylococcus aureus and Define a Genetic Basis for Nisin Resistance. Antimicrob. Agents Chemother. 2011, 55, 2362–2368. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Wang, Y.; He, Y.; Zhang, Y.; She, Q.; Chai, Y.; Li, P.; Shang, Q. Characterization of Subtilin L-Q11, a Novel Class I Bacteriocin Synthesized by Bacillus subtilis L-Q11 Isolated From Orchard Soil. Front. Microbiol. 2019, 10, 484. [Google Scholar] [CrossRef] [PubMed]
- Zhao, R.; Lu, Y.; Ran, J.; Li, G.; Lei, S.; Zhu, Y.; Xu, B. Purification and characterization of bacteriocin produced by Lactobacillus rhamnosus zrx01. Food Biosci. 2020, 38, 100754. [Google Scholar] [CrossRef]
- Ghobrial, O.; Derendorf, H.; Hillman, J.D. Human serum binding and its effect on the pharmacodynamics of the lantibiotic MU1140. Eur. J. Pharm. Sci. 2010, 41, 658–664. [Google Scholar] [CrossRef]
- Ansari, A.; Zohra, R.R.; Tarar, O.M.; Qader, S.A.U.; Aman, A. Screening, purification and characterization of thermostable, protease resistant Bacteriocin active against methicillin resistant Staphylococcus aureus (MRSA). BMC Microbiol. 2018, 18, 192. [Google Scholar] [CrossRef]
- Twomey, D.; Ross, R.P.; Ryan, M.; Meaney, B.; Hill, C. Lantibiotics produced by lactic acid bacteria: Structure, function and applications. Antonie Van Leeuwenhoek 2002, 82, 165–185. [Google Scholar] [CrossRef] [PubMed]
- Sulthana, R.; Archer, A. Bacteriocin nanoconjugates: Boon to medical and food industry. J. Appl. Microbiol. 2020, 131, 1056–1071. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Saeed, K.; Khan, I. Nanoparticles: Properties, applications and toxicities. Arab. J. Chem. 2019, 12, 908–931. [Google Scholar] [CrossRef]
- Tiwari, J.N.; Tiwari, R.N.; Kim, K.S. Zero-dimensional, one-dimensional, two-dimensional and three-dimensional nanostructured materials for advanced electrochemical energy devices. Prog. Mater. Sci. 2012, 57, 724–803. [Google Scholar] [CrossRef]
- Zohri, M.; Alavidjeh, M.S.; Mirdamadi, S.S.; Behmadi, H.; Nasr, S.M.H.; Gonbaki, S.E.; Ardestani, M.S.; Arabzadeh, A.J. Nisin-Loaded Chitosan/Alginate Nanoparticles: A Hopeful Hybrid Biopreservative. J. Food Saf. 2013, 33, 40–49. [Google Scholar] [CrossRef]
- Zohri, M.; Alavidjeh, M.S.; Haririan, I.; Ardestani, M.S.; Ebrahimi, S.E.S.; Sani, H.T.; Sadjadi, S.K. A Comparative Study Between the Antibacterial Effect of Nisin and Nisin-Loaded Chitosan/Alginate Nanoparticles on the Growth of Staphylococcus aureus in Raw and Pasteurized Milk Samples. Probiotics Antimicrob. Proteins 2010, 2, 258–266. [Google Scholar] [CrossRef]
- Wang, H.; She, Y.; Chu, C.; Liu, H.; Jiang, S.; Sun, M.; Jiang, S. Preparation, antimicrobial and release behaviors of nisin-poly (vinyl alcohol)/wheat gluten/ZrO2 nanofibrous membranes. J. Mater. Sci. 2015, 50, 5068–5078. [Google Scholar] [CrossRef]
- Heunis, T.D.J.; Smith, C.; Dicks, L.M.T. Evaluation of a Nisin-Eluting Nanofiber Scaffold To Treat Staphylococcus aureus-Induced Skin Infections in Mice. Antimicrob. Agents Chemother. 2013, 57, 3928–3935. [Google Scholar] [CrossRef]
- Liu, Y.; Liu, Y.; Du, Z.; Zhang, L.; Chen, J.; Shen, Z.; Liu, Q.; Qin, J.; Lv, H.; Wang, H.; et al. Skin microbiota analysis-inspired development of novel anti-infectives. Microbiome 2020, 8, 85. [Google Scholar] [CrossRef]
- Miller, L.G.; Eisenberg, D.F.; Liu, H.; Chang, C.-L.; Wang, Y.; Luthra, R.; Wallace, A.; Fang, C.; Singer, J.; Suaya, J.A. Incidence of skin and soft tissue infections in ambulatory and inpatient settings, 2005–2010. BMC Infect. Dis. 2015, 15, 1–8. [Google Scholar] [CrossRef]
- Esposito, S.; Noviello, S.; Leone, S. Epidemiology and microbiology of skin and soft tissue infections. Curr. Opin. Infect. Dis. 2016, 29, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Stevens, D.L.; Bisno, A.L.; Chambers, H.F.; Dellinger, E.P.; Goldstein, E.J.C.; Gorbach, S.L.; Hirschmann, J.; Kaplan, S.L.; Montoya, J.G.; Wade, J.C.; et al. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2014, 59, e10–e52. [Google Scholar] [CrossRef]
- Esposito, S.; Bassetti, M.; Concia, E.; De Simone, G.; De Rosa, F.G.; Grossi, P.; Novelli, A.; Menichetti, F.; Petrosillo, N.; Tinelli, M.; et al. Diagnosis and management of skin and soft-tissue infections (SSTI). A literature review and consensus statement: An update. J. Chemother. 2017, 29, 197–214. [Google Scholar] [CrossRef] [PubMed]
- Watkins, R.R.; David, M.Z. Approach to the Patient with a Skin and Soft Tissue Infection. Infect. Dis. Clin. North Am. 2021, 35, 1–48. [Google Scholar] [CrossRef] [PubMed]
- Staden, A.D.P.v.; Heunis, T.; Smith, C.; Deane, S.; Dicks, L.M.T. Efficacy of Lantibiotic Treatment of Staphylococcus aureus-Induced Skin Infections, Monitored by In Vivo Bioluminescent Imaging. Antimicrob. Agents Chemother. 2016, 60, 3948–3955. [Google Scholar] [CrossRef] [PubMed]
- Ovchinnikov, K.V.; Kranjec, C.; Thorstensen, T.; Carlsen, H.; Diep, D.B. Successful Development of Bacteriocins into Therapeutic Formulation for Treatment of MRSA Skin Infection in a Murine Model. Antimicrob. Agents Chemother. 2020, 64. [Google Scholar] [CrossRef]
- Zipperer, A.; Konnerth, M.C.; Laux, C.; Berscheid, A.; Janek, D.; Weidenmaier, C.; Burian, M.; Schilling, N.A.; Slavetinsky, C.; Marschal, M.; et al. Human commensals producing a novel antibiotic impair pathogen colonization. Nature 2016, 535, 511–516. [Google Scholar] [CrossRef]
- Francis, J.S.; Doherty, M.C.; Lopatin, U.; Johnston, C.P.; Sinha, G.; Ross, T.; Cai, M.; Hansel, N.N.; Perl, T.; Ticehurst, J.R.; et al. Severe Community-Onset Pneumonia in Healthy Adults Caused by Methicillin-Resistant Staphylococcus aureus Carrying the Panton-Valentine Leukocidin Genes. Clin. Infect. Dis. 2005, 40, 100–107. [Google Scholar] [CrossRef]
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratala, J.; et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111. [Google Scholar] [CrossRef]
- Jiang, H.; Tang, R.-N.; Wang, J. Linezolid versus vancomycin or teicoplanin for nosocomial pneumonia: Meta-analysis of randomised controlled trials. Eur. J. Clin. Microbiol. Infect. Dis. 2013, 32, 1121–1128. [Google Scholar] [CrossRef]
- Boakes, S.; Weiss, W.J.; Vinson, M.; Wadman, S.; Dawson, M.J. Antibacterial activity of the novel semisynthetic lantibiotic NVB333 in vitro and in experimental infection models. J. Antibiot. 2016, 69, 850–857. [Google Scholar] [CrossRef]
- De Kwaadsteniet, M.; Doeschate, K.; Dicks, L. Nisin F in the treatment of respiratory tract infections caused by Staphylococcus aureus. Lett. Appl. Microbiol. 2009, 48, 65–70. [Google Scholar] [CrossRef] [PubMed]
- de Kwaadsteniet, M.; Doeschate, K.T.; Dicks, L.M.T. Characterization of the Structural Gene Encoding Nisin F, a New Lantibiotic Produced by a Lactococcus lactis subsp. lactis Isolate from Freshwater Catfish (Clarias gariepinus). Appl. Environ. Microbiol. 2008, 74, 547–549. [Google Scholar] [CrossRef] [PubMed]
- Ghobrial, O.G.; Derendorf, H.; Hillman, J.D. Pharmacokinetic and pharmacodynamic evaluation of the lantibiotic MU1140. J. Pharm. Sci. 2010, 99, 2521–2528. [Google Scholar] [CrossRef] [PubMed]
- Geng, M.; Ravichandran, A.; Escano, J.; Smith, L. Efficacious Analogs of the Lantibiotic Mutacin 1140 against a Systemic Methicillin-Resistant Staphylococcus aureus Infection. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Bastos, M.D.C.D.F.; Coutinho, B.G.; Coelho, M.L.V. Lysostaphin: A Staphylococcal Bacteriolysin with Potential Clinical Applications. Pharmaceuticals 2010, 3, 1139–1161. [Google Scholar] [CrossRef]
- Oluola, O.; Kong, L.; Fein, M.; Weisman, L.E. Lysostaphin in Treatment of Neonatal Staphylococcus aureus Infection. Antimicrob. Agents Chemother. 2007, 51, 2198–2200. [Google Scholar] [CrossRef]
- Placencia, F.X.; Kong, L.; E Weisman, L. Treatment of Methicillin-Resistant Staphylococcus aureus in Neonatal Mice: Lysostaphin Versus Vancomycin. Pediatr. Res. 2009, 65, 420–424. [Google Scholar] [CrossRef]
- Lee, N.-K.; Park, Y.-L.; Kim, H.-W.; Park, Y.-H.; Rhim, S.-L.; Kim, J.-M.; Kim, J.-M.; Nam, H.-M.; Jung, S.-C.; Paik, H.-D. Purification and Characterization of Lacticin NK34 Produced by Lactococcus lactis NK34 against Bovine Mastitis. Korean J. Food Sci. Anim. Resour. 2008, 28, 457–462. [Google Scholar] [CrossRef]
- Kim, S.; Shin, S.; Koo, H.; Youn, J.-H.; Paik, H.-D.; Park, Y. In vitro antimicrobial effect and in vivo preventive and therapeutic effects of partially purified lantibiotic lacticin NK34 against infection by Staphylococcus species isolated from bovine mastitis. J. Dairy Sci. 2010, 93, 3610–3615. [Google Scholar] [CrossRef]
- Kavanagh, N.; Ryan, E.J.; Widaa, A.; Sexton, G.; Fennell, J.; O’Rourke, S.; Cahill, K.C.; Kearney, C.J.; O’Brien, F.J.; Kerrigan, S.W. Staphylococcal Osteomyelitis: Disease Progression, Treatment Challenges, and Future Directions. Clin. Microbiol. Rev. 2018, 31, e00084-17. [Google Scholar] [CrossRef]
- Van de Belt, H.; Neut, D.; Schenk, W.; van Horn, J.R.; van der Mei, H.C.; Busscher, H.J. Infection of orthopedic implants and the use of antibiotic-loaded bone cements: A review. Acta Orthop. Scand. 2001, 72, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Saleh, K.J.; Ragland, P.S.; Pour, A.E.; Mont, M.A. Efficacy of antibiotic-impregnated cement in total hip replacement. Acta Orthop. 2008, 79, 335–341. [Google Scholar] [CrossRef] [PubMed]
- van Staden, A.; Brand, A.; Dicks, L. Nisin F-loaded brushite bone cement prevented the growth of Staphylococcus aureus in vivo. J. Appl. Microbiol. 2012, 112, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Murray, R.J. Staphylococcus aureus infective endocarditis: Diagnosis and management guidelines. Intern. Med. J. 2005, 35, S25–S44. [Google Scholar] [CrossRef]
- Castiglione, F.; Lazzarini, A.; Carrano, L.; Corti, E.; Ciciliato, I.; Gastaldo, L.; Candiani, P.; Losi, D.; Marinelli, F.; Selva, E.; et al. Determining the Structure and Mode of Action of Microbisporicin, a Potent Lantibiotic Active Against Multiresistant Pathogens. Chem. Biol. 2008, 15, 22–31. [Google Scholar] [CrossRef]
- Jabés, D.; Brunati, C.; Candiani, G.; Riva, S.; Romanó, G.; Donadio, S. Efficacy of the New Lantibiotic NAI-107 in Experimental Infections Induced by Multidrug-Resistant Gram-Positive Pathogens. Antimicrob. Agents Chemother. 2011, 55, 1671–1676. [Google Scholar] [CrossRef]
- Wertheim, H.F.; Melles, D.C.; Vos, M.C.; van Leeuwen, W.; van Belkum, A.; Verbrugh, H.A.; Nouwen, J.L. The role of nasal carriage in Staphylococcus aureus infections. Lancet Infect. Dis. 2005, 5, 751–762. [Google Scholar] [CrossRef]
- Bode, L.G.M.; Kluytmans, J.A.J.W.; Wertheim, H.F.L.; Bogaers, D.; Vandenbroucke-Grauls, C.M.J.E.; Roosendaal, R.; Troelstra, A.; Box, A.T.A.; Voss, A.; van der Tweel, I.; et al. Preventing Surgical-Site Infections in Nasal Carriers of Staphylococcus aureus. N. Engl. J. Med. 2010, 362, 9–17. [Google Scholar] [CrossRef]
- Muñoz, P.; Hortal, J.; Giannella, M.; Barrio, J.; Rodríguez-Créixems, M.; Pérez, M.; Rincón, C.; Bouza, E. Nasal carriage of S. aureus increases the risk of surgical site infection after major heart surgery. J. Hosp. Infect. 2008, 68, 25–31. [Google Scholar] [CrossRef]
- von Eiff, C.; Becker, K.; Machka, K.; Stammer, H.; Peters, G. Nasal Carriage as a Source of Staphylococcus aureus Bacteremia. N. Engl. J. Med. 2001, 344, 11–16. [Google Scholar] [CrossRef]
- Lee, A.S.; Macedo-Vinas, M.; François, P.; Renzi, G.; Schrenzel, J.; Vernaz, N.; Pittet, D.; Harbarth, S. Impact of Combined Low-Level Mupirocin and Genotypic Chlorhexidine Resistance on Persistent Methicillin-Resistant Staphylococcus aureus Carriage After Decolonization Therapy: A Case-control Study. Clin. Infect. Dis. 2011, 52, 1422–1430. [Google Scholar] [CrossRef]
- Hetem, D.; Bonten, M. Clinical relevance of mupirocin resistance in Staphylococcus aureus. J. Hosp. Infect. 2013, 85, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Desroches, M.; Potier, J.; Laurent, F.; Bourrel, A.-S.; Doucet-Populaire, F.; Decousser, J.-W.; Archambaud, M.; Aubert, G.; Biendo, M.; Blanchard-Marche, G.; et al. Prevalence of mupirocin resistance among invasive coagulase-negative staphylococci and methicillin-resistant Staphylococcus aureus (MRSA) in France: Emergence of a mupirocin-resistant MRSA clone harbouring mupA. J. Antimicrob. Chemother. 2013, 68, 1714–1717. [Google Scholar] [CrossRef]
- Sandiford, S.; Upton, M. Identification, Characterization, and Recombinant Expression of Epidermicin NI01, a Novel Unmodified Bacteriocin Produced by Staphylococcus epidermidis That Displays Potent Activity against Staphylococci. Antimicrob. Agents Chemother. 2012, 56, 1539–1547. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, S.; Warn, P.; Sattar, A.; Derrick, J.P.; Upton, M. A single dose of epidermicin NI01 is sufficient to eradicate MRSA from the nares of cotton rats. J. Antimicrob. Chemother. 2016, 72, 778–781. [Google Scholar] [CrossRef]
- Niu, W.W.; Neu, H.C. Activity of mersacidin, a novel peptide, compared with that of vancomycin, teicoplanin, and daptomycin. Antimicrob. Agents Chemother. 1991, 35, 998–1000. [Google Scholar] [CrossRef]
- Kruszewska, D.; Sahl, H.-G.; Bierbaum, G.; Pag, U.; Hynes, S.O.; Ljungh, Å. Mersacidin eradicates methicillin-resistant Staphylococcus aureus (MRSA) in a mouse rhinitis model. J. Antimicrob. Chemother. 2004, 54, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Piewngam, P.; Khongthong, S.; Roekngam, N.; Theapparat, Y.; Sunpaweravong, S.; Faroongsarng, D.; Otto, M. Probiotic for pathogen-specific Staphylococcus aureus decolonisation in Thailand: A phase 2, double-blind, randomised, placebo-controlled trial. Lancet Microbe 2023, 4, e75–e83. [Google Scholar] [CrossRef]
- Sassone-Corsi, M.; Nuccio, S.-P.; Liu, H.; Hernandez, D.; Vu, C.T.; Takahashi, A.A.; Edwards, R.A.; Raffatellu, M. Microcins mediate competition among Enterobacteriaceae in the inflamed gut. Nature 2016, 540, 280–283. [Google Scholar] [CrossRef] [PubMed]
- Kommineni, S.; Bretl, D.J.; Lam, V.; Chakraborty, R.; Hayward, M.; Simpson, P.; Cao, Y.; Bousounis, P.; Kristich, C.J.; Salzman, N.H. Bacteriocin production augments niche competition by enterococci in the mammalian gastrointestinal tract. Nature 2015, 526, 719–722. [Google Scholar] [CrossRef] [PubMed]
- Leyden, J.J.; Marples, R.R.; Kligman, A.M. Staphylococcus aureus in the lesions of atopic dermatitis. Br. J. Dermatol. 1974, 90, 525. [Google Scholar] [CrossRef] [PubMed]
- Valenta, C.; Bernkop-Schnürch, A.; Rigler, H.P. The Antistaphylococcal Effect of Nisin in a Suitable Vehicle: A Potential Therapy for Atopic Dermatitis in Man. J. Pharm. Pharmacol. 1996, 48, 988–991. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.A.; Vocanson, M.; Nicolas, J.-F.; Wolf, P.; Patra, V. Microbial derived antimicrobial peptides as potential therapeutics in atopic dermatitis. Front. Immunol. 2023, 14, 1125635. [Google Scholar] [CrossRef]
- Nakatsuji, T.; Hata, T.R.; Tong, Y.; Cheng, J.Y.; Shafiq, F.; Butcher, A.M.; Salem, S.S.; Brinton, S.L.; Spergel, A.K.R.; Johnson, K.; et al. Development of a human skin commensal microbe for bacteriotherapy of atopic dermatitis and use in a phase 1 randomized clinical trial. Nat. Med. 2021, 27, 700–709. [Google Scholar] [CrossRef]
- Williams, M.R.; Costa, S.K.; Zaramela, L.S.; Khalil, S.; Todd, D.A.; Winter, H.L.; Sanford, J.A.; O’neill, A.M.; Liggins, M.C.; Nakatsuji, T.; et al. Quorum sensing between bacterial species on the skin protects against epidermal injury in atopic dermatitis. Sci. Transl. Med. 2019, 11. [Google Scholar] [CrossRef]
- Cao, L.; Wu, J.; Xie, F.; Hu, S.; Mo, Y. Efficacy of Nisin in Treatment of Clinical Mastitis in Lactating Dairy Cows. J. Dairy Sci. 2007, 90, 3980–3985. [Google Scholar] [CrossRef]
- Lepak, A.J.; Marchillo, K.; Craig, W.A.; Andes, D.R. In Vivo Pharmacokinetics and Pharmacodynamics of the Lantibiotic NAI-107 in a Neutropenic Murine Thigh Infection Model. Antimicrob. Agents Chemother. 2015, 59, 1258–1264. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Karczewski, J.; Brown, C.M.; Maezato, Y.; Krasucki, S.P.; Streatfield, S.J.; Karczewski, J.; Brown, C.M.; Maezato, Y.; Krasucki, S.P.; Streatfield, S.J. Efficacy of a novel lantibiotic, CMB001, against MRSA. J. Antimicrob. Chemother. 2021, 76, 1532–1538. [Google Scholar] [CrossRef]
- Twomey, D.; Wheelock, A.; Flynn, J.; Meaney, W.; Hill, C.; Ross, R. Protection Against Staphylococcus aureus Mastitis in Dairy Cows Using a Bismuth-Based Teat Seal Containing the Bacteriocin, Lacticin 3147. J. Dairy Sci. 2000, 83, 1981–1988. [Google Scholar] [CrossRef]
- Khan, I.; Oh, D.-H. Integration of nisin into nanoparticles for application in foods. Innov. Food Sci. Emerg. Technol. 2016, 34, 376–384. [Google Scholar] [CrossRef]
- Ng, Z.J.; Abu Zarin, M.; Lee, C.K.; Tan, J.S. Application of bacteriocins in food preservation and infectious disease treatment for humans and livestock: A review. RSC Adv. 2020, 10, 38937–38964. [Google Scholar] [CrossRef]
- Verma, D.K.; Thakur, M.; Singh, S.; Tripathy, S.; Gupta, A.K.; Baranwal, D.; Patel, A.R.; Shah, N.; Utama, G.L.; Niamah, A.K.; et al. Bacteriocins as antimicrobial and preservative agents in food: Biosynthesis, separation and application. Food Biosci. 2022, 46, 101594. [Google Scholar] [CrossRef]
- Negash, A.W.; Tsehai, B.A. Current Applications of Bacteriocin. Int. J. Microbiol. 2020, 2020, 1–7. [Google Scholar] [CrossRef]
- Mbandlwa, P.; Doyle, N.; Hill, C.; Stanton, C.; Ross, R.P. Bacteriocins: Novel Applications in Food, and Human and Animal Health, in Encyclopedia of Dairy Sciences, 3rd ed.; McSweeney, P.L.H., McNamara, J.P., Eds.; Academic Press: Oxford, UK, 2022; pp. 46–54. [Google Scholar] [CrossRef]
- Rilla, N.; Martínez, B.; Rodriguez, A. Inhibition of a Methicillin-Resistant Staphylococcus aureus Strain in Afuega’l Pitu Cheese by the Nisin Z–Producing Strain Lactococcus lactis subsp. lactis IPLA 729. J. Food Prot. 2004, 67, 928–933. [Google Scholar] [CrossRef] [PubMed]
- Grande, M.J.; López, R.L.; Abriouel, H.; Valdivia, E.; Ben Omar, N.; Maqueda, M.; Martínez-Cañamero, M.; Gálvez, A. Treatment of Vegetable Sauces with Enterocin AS-48 Alone or in Combination with Phenolic Compounds To Inhibit Proliferation of Staphylococcus aureus. J. Food Prot. 2007, 70, 405–411. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, A.; Ananou, S.; Gálvez, A.; Martínez-Bueno, M.; Rodríguez, A.; Maqueda, M.; Valdivia, E. Inhibition of Staphylococcus aureus in dairy products by enterocin AS-48 produced in situ and ex situ: Bactericidal synergism with heat. Int. Dairy J. 2007, 17, 760–769. [Google Scholar] [CrossRef]
- Burgos, M.J.G.; Pulido, R.P.; Aguayo, M.D.C.L.; Gálvez, A.; Lucas, R. The Cyclic Antibacterial Peptide Enterocin AS-48: Isolation, Mode of Action, and Possible Food Applications. Int. J. Mol. Sci. 2014, 15, 22706–22727. [Google Scholar] [CrossRef]
- Lauková, A.; Czikková, S.; Dobránsky, T.; Burdová, O. Inhibition ofListeria monocytogenesand Staphylococcus aureus by enterocin CCM 4231 in milk products. Food Microbiol. 1999, 16, 93–99. [Google Scholar] [CrossRef]
- An, J.; Zhu, W.; Liu, Y.; Zhang, X.; Sun, L.; Hong, P.; Wang, Y.; Xu, C.; Xu, D.; Liu, H. Purification and characterization of a novel bacteriocin CAMT2 produced by Bacillus amyloliquefaciens isolated from marine fish Epinephelus areolatus. Food Control. 2015, 51, 278–282. [Google Scholar] [CrossRef]
- Wu, Y.; An, J.; Liu, Y.; Wang, Y.; Ren, W.; Fang, Z.; Sun, L.; Gooneratne, R. Mode of action of a novel anti-Listeria bacteriocin (CAMT2) produced by Bacillus amyloliquefaciens ZJHD3-06 from Epinephelus areolatus. Arch. Microbiol. 2018, 201, 61–66. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC); European Food Safety Authority (EFSA); European Medicines Agency (EMA). ECDC/EFSA/EMA second joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals. EFSA J. 2017, 15, 4872–5007. [Google Scholar] [CrossRef]
- Hollis, A.; Ahmed, Z. Preserving Antibiotics, Rationally. N. Engl. J. Med. 2013, 369, 2474–2476. [Google Scholar] [CrossRef]
- Muurinen, J.; Richert, J.; Wickware, C.L.; Richert, B.; Johnson, T.A. Swine growth promotion with antibiotics or alternatives can increase antibiotic resistance gene mobility potential. Sci. Rep. 2021, 11, 1–13. [Google Scholar] [CrossRef]
- Morris, C.; Helliwell, R.; Raman, S. Framing the agricultural use of antibiotics and antimicrobial resistance in UK national newspapers and the farming press. J. Rural. Stud. 2016, 45, 43–53. [Google Scholar] [CrossRef]
- Ben Lagha, A.; Haas, B.; Gottschalk, M.; Grenier, D. Antimicrobial potential of bacteriocins in poultry and swine production. Vet. Res. 2017, 48, 22. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.M.; Riley, M.A.; Crabb, J.H. Treating Bovine Mastitis with Nisin: A Model for the Use of Protein Antimicrobials in Veterinary Medicine. In The Bacteriocins: Current Knowledge and Future Prospects; Caister Academic Press: Poole, UK, 2016; pp. 127–140. [Google Scholar] [CrossRef][Green Version]
- Holmes, A.H.; Moore, L.S.P.; Sundsfjord, A.; Steinbakk, M.; Regmi, S.; Karkey, A.; Guerin, P.J.; Piddock, L.J.V. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet 2016, 387, 176–187. [Google Scholar] [CrossRef]
- Bradley, A. Bovine Mastitis: An Evolving Disease. Vet. J. 2002, 164, 116–128. [Google Scholar] [CrossRef]
- Coelho, M.L.V.; dos Santos Nascimento, J.; Fagundes, P.C.; Madureira, D.J.; de Oliveira, S.S.; de Paiva Brito, M.A.V.; de Freire Bastos, M.D.C. Activity of staphylococcal bacteriocins against Staphylococcus aureus and Streptococcus agalactiae involved in bovine mastitis. Res. Microbiol. 2007, 158, 625–630. [Google Scholar] [CrossRef]
- Barboza-Corona, J.E.; de la Fuente-Salcido, N.; Alva-Murillo, N.; Ochoa-Zarzosa, A.; López-Meza, J.E. Activity of bacteriocins synthesized by Bacillus thuringiensis against Staphylococcus aureus isolates associated to bovine mastitis. Vet. Microbiol. 2009, 138, 179–183. [Google Scholar] [CrossRef]
- Ryan, M.P.; Meaney, W.J.; Ross, R.P.; Hill, C. Evaluation of Lacticin 3147 and a Teat Seal Containing This Bacteriocin for Inhibition of Mastitis Pathogens. Appl. Environ. Microbiol. 1998, 64, 2287–2290. [Google Scholar] [CrossRef]
- Kaur, B.; Balgir, P.P.; Mittu, B.; Kumar, B.; Garg, N. Biomedical Applications of Fermenticin HV6b Isolated from Lactobacillus fermentum HV6b MTCC10770. BioMed Res. Int. 2013, 2013, 1–8. [Google Scholar] [CrossRef]
- Ahmad, V.; Khan, M.S.; Jamal, Q.M.S.; Alzohairy, M.A.; Al Karaawi, M.A.; Siddiqui, M.U. Antimicrobial potential of bacteriocins: In therapy, agriculture and food preservation. Int. J. Antimicrob. Agents 2017, 49, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Angelopoulou, A.; Field, D.; Ryan, C.A.; Stanton, C.; Hill, C.; Ross, R.P. The microbiology and treatment of human mastitis. Med Microbiol. Immunol. 2018, 207, 83–94. [Google Scholar] [CrossRef] [PubMed]
- Jiménez, E.; de Andrés, J.; Manrique, M.; Pareja-Tobes, P.; Tobes, R.; Martínez-Blanch, J.F.; Codoñer, F.M.; Ramón, D.; Fernández, L.; Rodríguez, J.M. Metagenomic Analysis of Milk of Healthy and Mastitis-Suffering Women. J. Hum. Lact. 2015, 31, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Inhibition Effects of Probiotics on Pathogens Associated with VAP. Available online: https://ClinicalTrials.gov/show/NCT02928042 (accessed on 1 June 2023).
- Alexandre, Y.; Le Berre, R.; Barbier, G.; Le Blay, G. Screening of Lactobacillus spp. for the prevention of Pseudomonas aeruginosa pulmonary infections. BMC Microbiol. 2014, 14, 107. [Google Scholar] [CrossRef]
- Functional Ingredients: Effect in Gastrointestinal System. Available online: https://ClinicalTrials.gov/show/NCT02467972 (accessed on 1 June 2023).
- Fernández, L.; Delgado, S.; Herrero, H.; Maldonado, A.; Rodríguez, J.M. The Bacteriocin Nisin, an Effective Agent for the Treatment of Staphylococcal Mastitis during Lactation. J. Hum. Lact. 2008, 24, 311–316. [Google Scholar] [CrossRef]
- Årdal, C.; Balasegaram, M.; Laxminarayan, R.; McAdams, D.; Outterson, K.; Rex, J.H.; Sumpradit, N. Antibiotic development—Economic, regulatory and societal challenges. Nat. Rev. Microbiol. 2020, 18, 267–274. [Google Scholar] [CrossRef]
- Benítez-Chao, D.F.; León-Buitimea, A.; Lerma-Escalera, J.A.; Morones-Ramírez, J.R. Bacteriocins: An Overview of Antimicrobial, Toxicity, and Biosafety Assessment by in vivo Models. Front. Microbiol. 2021, 12. [Google Scholar] [CrossRef]
- Hillman, J.D.; Novák, J.; Sagura, E.; Gutierrez, J.A.; Brooks, T.A.; Crowley, P.J.; Hess, M.; Azizi, A.; Leung, K.-P.; Cvitkovitch, D.; et al. Genetic and Biochemical Analysis of Mutacin 1140, a Lantibiotic from Streptococcus mutans. Infect. Immun. 1998, 66, 2743–2749. [Google Scholar] [CrossRef] [PubMed]
- Ghobrial, O.G.; Derendorf, H.; Hillman, J.D. Pharmacodynamic activity of the lantibiotic MU1140. Int. J. Antimicrob. Agents 2009, 33, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, R.; Bhattarai, N.; Baral, P.; Gerstman, B.S.; Park, J.H.; Handfield, M.; Chapagain, P.P. Molecular mechanisms of pore formation and membrane disruption by the antimicrobial lantibiotic peptide Mutacin 1140. Phys. Chem. Chem. Phys. 2019, 21, 12530–12539. [Google Scholar] [CrossRef] [PubMed]
- Hammond, K.; Lewis, H.; Halliwell, S.; Desriac, F.; Nardone, B.; Ravi, J.; Hoogenboom, B.W.; Upton, M.; Derrick, J.P.; Ryadnov, M.G. Flowering Poration—A Synergistic Multi-Mode Antibacterial Mechanism by a Bacteriocin Fold. iScience 2020, 23, 101423. [Google Scholar] [CrossRef]
- Breukink, E.; Wiedemann, I.; van Kraaij, C.; Kuipers, O.P.; Sahl, H.-G.; de Kruijff, B. Use of the Cell Wall Precursor Lipid II by a Pore-Forming Peptide Antibiotic. Science 1999, 286, 2361–2364. [Google Scholar] [CrossRef]
- Sahl, H.G.; Kordel, M.; Benz, R. Voltage-dependent depolarization of bacterial membranes and artificial lipid bilayers by the peptide antibiotic nisin. Arch. Microbiol. 1987, 149, 120–124. [Google Scholar] [CrossRef]
- Mulders, J.W.M.; Boerrigter, I.J.; Rollema, H.S.; Siezen, R.J.; de Vos, W.M. Identification and characterization of the lantibiotic nisin Z, a natural nisin variant. Eur. J. Biochem. 1991, 201, 581–584. [Google Scholar] [CrossRef]
- Kaletta, C.; Entian, K.D. Nisin, a peptide antibiotic: Cloning and sequencing of the nisA gene and posttranslational processing of its peptide product. J. Bacteriol. 1989, 171, 1597–1601. [Google Scholar] [CrossRef]
- Karczewski, J.; Krasucki, S.P.; Asare-Okai, P.N.; Diehl, C.; Friedman, A.; Brown, C.M.; Maezato, Y.; Streatfield, S.J. Isolation, Characterization and Structure Elucidation of a Novel Lantibiotic from Paenibacillus sp. Front. Microbiol. 2020, 11. [Google Scholar] [CrossRef]
- Ovchinnikov, K.V.; Chi, H.; Mehmeti, I.; Holo, H.; Nes, I.F.; Diep, D.B. Novel Group of Leaderless Multipeptide Bacteriocins from Gram-Positive Bacteria. Appl. Environ. Microbiol. 2016, 82, 5216–5224. [Google Scholar] [CrossRef] [PubMed]
- Ciufolini, M.A.; Lefranc, D. Micrococcin P1: Structure, biology and synthesis. Nat. Prod. Rep. 2010, 27, 330–342. [Google Scholar] [CrossRef]
- Heinrich, P.; Rosenstein, R.; Böhmer, M.; Sonner, P.; Götz, F. The molecular organization of the lysostaphin gene and its sequences repeated in tandem. Mol. Genet. Genom. 1987, 209, 563–569. [Google Scholar] [CrossRef] [PubMed]
- A Recsei, P.; Gruss, A.D.; Novick, R.P. Cloning, sequence, and expression of the lysostaphin gene from Staphylococcus simulans. Proc. Natl. Acad. Sci. 1987, 84, 1127–1131. [Google Scholar] [CrossRef] [PubMed]
- Bierbaum, G.; Brã¶Tz, H.; Koller, K.-P.; Sahl, H.-G. Cloning, sequencing and production of the lantibiotic mersacidin. FEMS Microbiol. Lett. 1995, 127, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Martin, N.I.; Sprules, T.; Carpenter, M.R.; Cotter, P.D.; Hill, C.; Ross, R.P.; Vederas, J.C. Structural Characterization of Lacticin 3147, a Two-Peptide Lantibiotic with Synergistic Activity. Biochemistry 2004, 43, 3049–3056. [Google Scholar] [CrossRef]
| Bacteriocin | Producing Strain | Target Strains | Model Organism | In Vivo Demonstration | Reference |
|---|---|---|---|---|---|
| Mutacin 1140 | Streptococcus mutans | S. aureus (ATCC 25923 and ATCC 33591) | BALB/c mouse | Systemic infection | [107] |
| Epidermicin NI01 | S. epidermidis | MRSA ATCC 43300 | SPF Cotton rat | Nasal carriage | [128] |
| Nisin (Nisin A) | Lactococcus lactis | S. aureus Xen36 | Nude mouse | Skin infection | [97] |
| BALB/c mouse | [90] | ||||
| Nisin F | Lactococcus lactis F10 | S. aureus K S. aureus Xen36 | Wistar rat BALB/c mouse | Respiratory infection Osteomyelitis | [104,116] |
| Nisin Z | Lactococcus lactis | Undetermined S. aureus strains | Cow | Mastitis | [139] |
| NAI-107 | Microbispora ATCC PTA-5024 | S. aureus 1524 S. aureus (ATCC 29213, USA200, 307109, MW2, USA300, ATCC 25923, 6538P, Smith, WIS-1) | SD rat ICR mouse | Endocarditis | [119] |
| Intramuscular infection | [140] | ||||
| CMB001 | Paenibacillus kyungheensis | S. aureus USA300 | ICR mouse | Intramuscular infection | [141] |
| Garvicin KS | Lactococcus garvieae KS1546 | S. aureus Xen31 | BALB/c mouse | Skin infection | [98] |
| Micrococcin P1 | Staphylococcus equorum WS 2733 | S. aureus Xen31 | BALB/c mouse | Skin infection | [98] |
| Lysostaphin | Staphylococcus simulans | S. aureus USA300 | Neonatal Wistar mouse Neonatal FVB mouse | Systemic infection Systemic infection | [109] |
| [110] | |||||
| NVB333 | Actinoplanes liguriae | S. aureus UNT103-3, S. aureus ATCC 33591, MRSA UNT084-3 | SPF CD-1 mouse | Intramuscular infection Respiratory infection | [103] |
| Clausin | Alkalihalobacillus clausii | S. aureus Xen36 | Nude mouse | Skin Infection | [97] |
| Amyloliquecidin | Bacillus velezensis | S. aureus Xen36 | Nude mouse | Skin infection | [97] |
| Mersacidin | Bacillus sp. strain HIL Y-85,54728. | S. aureus 99308 | BALB/c mouse | Nasal carriage | [130] |
| Lacticin NK34 | Lactococcus lactis | S. aureus 69 | ICR mouse | Systemic infection | [112] |
| Lacticin 3147 | Lactococcus lactis subsp. lactis DPC3147 | Undetermined S. aureus strains | Cow | Mastitis | [142] |
| Lugdunin | Staphylococcus lugunensis | S. aureus USA3000 | Cotton rat | Skin infection | [99] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinzinger, L.R.; Pugh, A.R.; Wagner, J.A.; Otto, M. Evaluating the Translational Potential of Bacteriocins as an Alternative Treatment for Staphylococcus aureus Infections in Animals and Humans. Antibiotics 2023, 12, 1256. https://doi.org/10.3390/antibiotics12081256
Heinzinger LR, Pugh AR, Wagner JA, Otto M. Evaluating the Translational Potential of Bacteriocins as an Alternative Treatment for Staphylococcus aureus Infections in Animals and Humans. Antibiotics. 2023; 12(8):1256. https://doi.org/10.3390/antibiotics12081256
Chicago/Turabian StyleHeinzinger, Lauren R., Aaron R. Pugh, Julie A. Wagner, and Michael Otto. 2023. "Evaluating the Translational Potential of Bacteriocins as an Alternative Treatment for Staphylococcus aureus Infections in Animals and Humans" Antibiotics 12, no. 8: 1256. https://doi.org/10.3390/antibiotics12081256
APA StyleHeinzinger, L. R., Pugh, A. R., Wagner, J. A., & Otto, M. (2023). Evaluating the Translational Potential of Bacteriocins as an Alternative Treatment for Staphylococcus aureus Infections in Animals and Humans. Antibiotics, 12(8), 1256. https://doi.org/10.3390/antibiotics12081256





