Multidrug-Resistant (MDR) Urinary Tract Infections Associated with Gut Microbiota in CoV and Non-CoV Patients in a Urological Clinic during the Pandemic: A Single Center Experience
Abstract
1. Introduction
2. Results
3. Materials and Methods
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wagenlehner, F.M.; Naber, K.G. Treatment of bacterial urinary tract infections:presence and future. Eur Urol. 2006, 49, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Bernardo, L.; Teixeira, J.C.; Marques-Pinto, A.; Vila, F.; Lindoro, J.; Fraga, A. How the COV-19 pandemic changed postoperative infections in urology wards: A retrospective cohort study from two urology departments. Can. Urol. Assoc. J. 2022, 16, E267–E273. [Google Scholar]
- Bentivegna, E.; Luciani, M.; Arcari, L.; Santino, I.; Simmaco, M.; Martelleti, P. Reduction of Multidrug-Resistant (MDR) bacterial Infections during the COV-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1003. [Google Scholar] [CrossRef] [PubMed]
- Tham, N.; Fazio, T.; Johnson, D.; Skandarajah, A.; Hayes, I.P. Hospital Aquired Infections in Surgical Patients: Impact of COV-19-Related Infections Prevention Measures. World J. Surg. 2022, 46, 1249–1258. [Google Scholar] [CrossRef]
- Gasperini, B.; Cherubini, A.; Lucarelli, M.; Espinosa, E.; Prospero, E. Multidrug-Resistant Bacterial Infections in Geriatric Hospitalised Patients before and after the COV-19 Outbreak: Results from a Retrospective Observational Study in Two Geriatric Wards. Antibiotics 2021, 10, 95. [Google Scholar] [CrossRef]
- Miftode, I.L.; Leca, D.; Miftode, R.S.; Roşu, F.; Plesca, C.; Loghin, I.; Timpau, A.S.S.; Mitu, I.; Mititiuc, I.; Dorneanu, O.; et al. The Clash of the Titans: COVID-19, Carbapenem-Resistant Enterobacterales, and First mcr-1-Mediated Colistin Resistance in Humans in Romania. Antibiotics 2023, 12, 324. [Google Scholar] [CrossRef]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant extensively drug-resistant and pandrug-resistant bacteria:An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2011, 18, 268–281. [Google Scholar] [CrossRef]
- Mohammadi, A.; Khatami, F.; Azimbeik, Z.; Khajavi, A.; Aloosh, M.; Aghamir, S.M. Hospital-aquired infections in a tertiary hospital in Iran before and during the COV-19 pandemic. Wien Med Wochenschr. 2022, 172, 220–226. [Google Scholar] [CrossRef]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O.; et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016–2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef]
- Tyagi, V.; Sharma, A.K.; Bhandari, M. Urological implications of SARS-CoV-19. Can. J. Urol. 2020, 27, 10205–10212. [Google Scholar]
- Gul, M.; Kaymar, M.; Yildiz, M.; Batur, A.F.; Akrand, M.; Kilic, O.; Goktas, S. The Increased Risk of Complicated Ureteral Stones in the Era of COV-19 Pandemic. J. Endourol. 2020, 34, 882–886. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368, m1091. [Google Scholar] [CrossRef] [PubMed]
- Luciani, M.; Bentivegna, E.; Spuntareli, V.; Lamberti, P.A.; Cacioli, G.; del Potro, F.; Sesti, G.; Martalleti, P.; de Biase, L. Recurrent COV-19 pneumonia in the course of chemotherapy. Consequence of a weakened immune system? J. Med. Virol. 2021, 93, 1882–1884. [Google Scholar] [CrossRef] [PubMed]
- Gaspari, R.; Spinazzola, G.; Teofili, L.; Avolio, A.W.; Fiori, B.; Maresca, G.M.; Spanu, T.; Nicolotti, N.; De Pascuale, G. Protective Effect of SARS-CoV-2 preventive measures against ESKAPE and Escherichia coli infections. Eur. J. Clin. Investig. 2021, 51, e13689. [Google Scholar] [CrossRef]
- Bentivegna, E.; Alessio, G.; Spuntarelli, V.; Luciani, M.; Santino, I.; Simmaco, M.; Martelletti, P. Impact of COV-19 prevention measures on risk of healthcare-associated Clostridium difficile infection. Am. J. Infect. Control. 2021, 49, 640–642. [Google Scholar] [CrossRef]
- Garcia-Vidal, C.; Sanjuan, G.; Moreno-García, E.; Puerta-Alcalde, P.; Garcia-Pouton, N.; Chumbita, M.; Fernandez-Pittol, M.; Pitart, C.; Inciarte, A.; Bodro, M.; et al. Incidence of co-infections and superinfections in hospitalized patients with COV-19: A retrospective cohort study. Clin. Microbiol. Infect. 2021, 27, 83–88. [Google Scholar] [CrossRef]
- Tiri, B.; Sensi, E.; Marsiliani, V.; Cantarini, M.; Priante, G.; Vernelli, C.; Martella, L.A.; Costantini, M.; Mariottini, A.; Andreani, P.; et al. Antimicrobial stewardship program, COV-19, and infection control: Spread of carbapenem-resistant Klebsiella pneumoniae colonization in ICU COV-19 patients. What did not work? J. Clin. Med. 2020, 9, 2744. [Google Scholar] [CrossRef]
- Kampmeier, S.; Tönnies, H.; Correa-Martinez, C.L.; Mellmann, A.; Schwierzeck, V. A nosocomial cluster of vancomycin- resistant Enterococci among COV-19 patients in an intensive care unit. Antimicrob. Resist Infect Control. 2020, 9, 154. [Google Scholar] [CrossRef]
- Medina-Polo, J.; Jimenes-Alcaide, E.; Garcia-Gonzales, L.; Guerrero-Ramos, F.; Perez-Cadavid, S.; Arre’bola-Pajares, A.; Sopena-Sutil, R.; Benites-Salas, R.; Diaz-Gonzales, R.; Tejido-Sanchez, A. Healthcare-associated infections in a department of urology: Incidence and patterns of antibiotic resistance. Scan. J. Urol. 2014, 48, 203–209. [Google Scholar] [CrossRef]
- Liew, Y.; Lee, W.H.L.; Tan, L.; Kwa, A.L.H.; Thien, S.Y.; Cherng, B.P.Z.; Chung, S.J. Antimicrobial stewardship programme: A vital resource for hospitals during the global outbreak of coronavirus disease 2019 (COV-19). Int. J. Antimicrob. Agents 2020, 56, 106145. [Google Scholar] [CrossRef]
- Tenney, J.; Hudson, N.; Alnifaidy, H.; Cheng Li, J.T.; Fung, K.H. Risk factors for aquiring multi-drug resistant organisms in urinary tract infections: A systematic literature review. Saudi Pharm. J. 2018, 26, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Milan, P.B.; Ivan, I.M. Catheter-associated and nosocomial urinary tract infections:antibiotic resistance and influence on commonly used antimicrobial therapy. Int. Urol. Nephrol. 2009, 41, 461–464. [Google Scholar] [CrossRef]
- Miftode, E.; Miftode, L.; Coman, I.; Prepeliuc, C.; Obreja, M.; Stamateanu, O.; Parânga, T.G.; Leca, D.; Plesca, C.E. Diabetes Mellitus—A Risk Factor for Unfavourable Outcome in COVID-19 Patients -The Experience of an Infectious Diseases Regional Hospital. Healthcare 2021, 9, 788. [Google Scholar] [CrossRef]
- Dezza, F.C.; Arcari, G.; Alessi, F.; Valeri, S.; Curtolo, A.; Sacco FCeccarelli, G.; Raponi, G.; Alessandri, F.; Mastroiani, C.M.; Venditti MOliva, A. Clinical Impact of COV-19 on Multi-Drug- Resistant, Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Settings: Two Pandemias Compared. Antibiotics 2022, 11, 926. [Google Scholar] [CrossRef] [PubMed]
- Sobel, J.D. Urinary Tract Infections. In Mandell, Douglas and Bennett’s Principles and Practice of Infectious Disease, 8th ed.; Mandell, G.L., Bennett, J.E., Eds.; Elsevier: Sanders, PA, USA, 2015; Volume 1, pp. 886–913. [Google Scholar]
- Bonkat, G.; Bartoletti, R.; Bruyere, F.; Cai, T.; Geerling, S.E.; Köves, B.; Schubert, S.; Wagenlehner, F. EAU Guidelines on Urological Infections; European Association of Urology: Arnhem, The Netherlands, 2021. [Google Scholar]
- Wagenlehner, F.; Tandogdu, Z.; Bartoletti, R.; Cai, T.; Cek, M.; Kulchavenya, E.; Ko”ves, B.; Naber, K.; Perepanova, T.; Tenke, P.; et al. GPIU Investigators. The Global Prevalence of Infections in Urology(GPIU)Study: A Worldwide Surveillance Study in Urology Patients. Eur. Urol. Focus 2016, 2, 345–347. [Google Scholar] [CrossRef] [PubMed]
- Medina-Polo, J.; Sopena-Sutil, R.; Benitez-Sala, R.; Lara-Isla, A.; Alonso-Isa, M.; Gil-Moradillo, J.; Justo- Quintas, J.; Garcia-Rojo, E.; Gonzales-Padilla, D.A.; Passas-Martinez, J.B.; et al. Prospective study analyzing risk factors and characteristics of healthcare-associated infections in a Urology ward. Investig. Clin. Urol. 2017, 58, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Tandogdu, Z.; Cek, M.; Wagenlehner, F.; Naber, K.; Tenke, P.; van Ostrum, E.; Johansen, T.B. Resistance patterns of nosocomial urinary tract infections in urology departments: 8-year results of the global prevalence of infections in urology study. World J. Urol. 2014, 32, 791–801. [Google Scholar] [CrossRef]
- Miftode, I.L.; Nastase, E.V.; Miftode, R.; Miftode, E.G.; Iancu, L.S.; Luncă, C.; Păduraru, D.A.; Costache, I.; Stafie, C.; Dorneanu, O. Insights into multidrug resistant K. pneumoniae urinary tract infections: From susceptibility to mortality. Exp. Ther. Med. 2021, 22, 1086. [Google Scholar] [CrossRef]
- Miftode, I.L.; Pasare, M.A.; Miftode, R.S.; Nastase, E.; Plesca, C.E.; Lunca, C.; Miftode, E.G.; Timpau, A.S.; Iancu, L.S.; Dorneanu, O.S. What Doesn’t Kill Them Makes Them Stronger: The Impact of the Resistance Patterns of Urinary Enterobacterales Isolates in Patients from a Tertiary Hospital in Eastern Europe. Antibiotics 2022, 11, 548. [Google Scholar] [CrossRef]

| Non-COVID MDR UTI (n = 66) | COVID MDR UTI (n = 22) | p | ||
|---|---|---|---|---|
| Male | 35 (53%) | 12 (54.5%) | 0.902 F | |
| Female | 31 (47%) | 10 (45.5%) | ||
| Age (mean ± SD) | Male | 63.31 ± 13.29 | 67.92 ± 6.99 | 0.136 t |
| Female | 58.13 ± 18.69 | 65.20 ± 11.29 | 0.161 t | |
| Residence area (urban) | 35 (53%) | 10 (45.5%) | 0.538 F | |
| Comorbidities | ||||
| 1. Type 2 diabetes (DM) | 20 (30.3%) | 6 (27.3%) | 0.787 F | |
| 2. Neoplasia | 27 (40.9%) | 8 (36.4%) | 0.706 F | |
| 3. Kidney failure | 26 (39.4%) | 12 (54.5%) | 0.214 F | |
| 4. Heart failure | 17 (25.8%) | 3 (13.6%) | 0.240 F | |
| 5. Anemia | 21 (31.8%) | 7 (31.8%) | 1 F | |
| 6. Stroke sequelae | 10 (15.2%) | 3 (13.6%) | 0.990F | |
| 7. Hypertension | 28 (42.4%) | 9 (40.9%) | 0.901 F | |
| Urosepsis at the moment of admission | 14 (21.2%) | 12 (54.5%) | 0.003 F | |
| Urinary Catheters at the Time of Diagnosis | Non-COVID MDR UTI (n = 66) | COVID MDR UTI (n = 22) | p-Value for Chi-Square Test and Fisher’s Exact Test |
|---|---|---|---|
| Permanent urethral catheter | 15 (22.7%) | 5 (22.73%) | 1 |
| Permanent double-J ureteral catheter | 30 (45.5%) | 4 (18.2%) | 0.023 |
| Permanent nephrostomy catheter | 9 (13.6%) | 6 (27.3%) | 0.190 |
| Cutaneous ureterostomy catheter | 2 (3.0%) | 1 (4.5%) | 0.999 |
| Lumbar drain tube | 1 (1.5%) | 1 (4.5%) | 0.440 |
| Permanent cystostomy catheter | 3 (4.5%) | 0 (0.0%) | 0.507 |
| Total number of permanent urinary catheters | 60 catheters in 56 patients (4 patients had 2 catheter types at the same time) | 17 catheters in 17 patients | |
| Total number of patients with urinary catheters | 56 (84.85%) | 17 (77.27%) | 0.413 |
| Non-COVID MDR UTI (n = 66) | COVID MDR UTI (n = 22) | p-Value for Chi-Square Test and Fisher’s Exact Test | |
|---|---|---|---|
| Hospitalization in the last 180 days | 51 (77.3%) | 16 (72.7%) | 0.665 |
| Antibiotic therapy in the last 180 days | 58 (87.9%) | 17 (77.3%) | 0.297 |
| Hospitalization days (mean ± standard deviation) | 6.09 ± 4.87 | 9.27 ± 4.92 | 0.010 t |
| Types of urological interventions performed before the diagnosis of MDR infections | |||
| 1 TURP (transurethral resection of the prostate) | 1 (1.5%) | 3 (13.6%) | 0.047 |
| 2 TURBT (transurethral resection of bladder tumors) | 2 (3.0%) | 0 (0.0%) | 0.999 |
| 3 Percutaneous nephrostomy tube insertion | 6 (9.1%) | 5 (22.73%) | 0.093 |
| 4 Nephrectomy | 1 (1.5%) | 1 (4.5%) | 0.440 |
| 5 Urethral catheter replacement | 8 (12.1%) | 1 (4.5%) | 0.440 |
| 6 Urethrotomy | 3 (4.5%) | 1 (4.54%) | 0.440 |
| 7 Percutaneous nephrolithotomy (PCNL) | 3 (4.5%) | 0 (0.0%) | 0.570 |
| 8 Percutaneous lumbar drainage | 1(1.5%) | 1 (4.5%) | 0.440 |
| 9 Double-J catheter insertion | 18 (27.3%) | 2 (9.1%) | 0.078 |
| 10 Double-J catheter replacement | 14 (21.2%) | 2 (9.1%) | 0.338 |
| 11 Urethral catheter insertion | 3 (4.5%) | 2(9,1%) | 0.425 |
| 12 Urethral dilatation | 1 (1.5%) | 0 (0.0%) | 0.999 |
| 13 Percutaneous nephrostomy tube replacement | 2 (3.0%) | 2 (9.1%) | 0.259 |
| 14 Ureterostomy double-J catheter replacement | 1 (1.5%) | 1 (4.5%) | 0.440 |
| Total urological maneuvers before the occurrence of MDR | 64 (96.97%) | 21 (95.45%) | 0.734 |
| Types of MDR Bacteria | Non-COVID MDR UTI (n = 66) | COVID MDR UTI (n = 22) | p-Value for Chi-Square Test and Fisher’s Exact Test |
|---|---|---|---|
| Escherichia coli | 28 (42.4%) | 7 (31.8%) | 0.379 |
| Klebsiella spp. | 23 (34.8%) | 5 (22.7%) | 0.290 |
| Pseudomonas aeruginosa | 6 (9.1%) | 6 (27.3%) | 0.066 |
| Proteus mirabilis | 2 (3.0%) | 2 (9.1%) | 0.259 |
| Enterobacter spp. | 0 (0.0%) | 1 (4.5%) | 0.250 |
| Providencia spp. | 1 (1.5%) | 0 (0.0%) | 0.999 |
| Serratia marcescens | 1 (1.5%) | 0 (0.0%) | 0.999 |
| Enterococcus spp. | 5 (7.6%) | 1 (4.5%) | 0.998 |
| Total MDR infections | 66 | 22 |
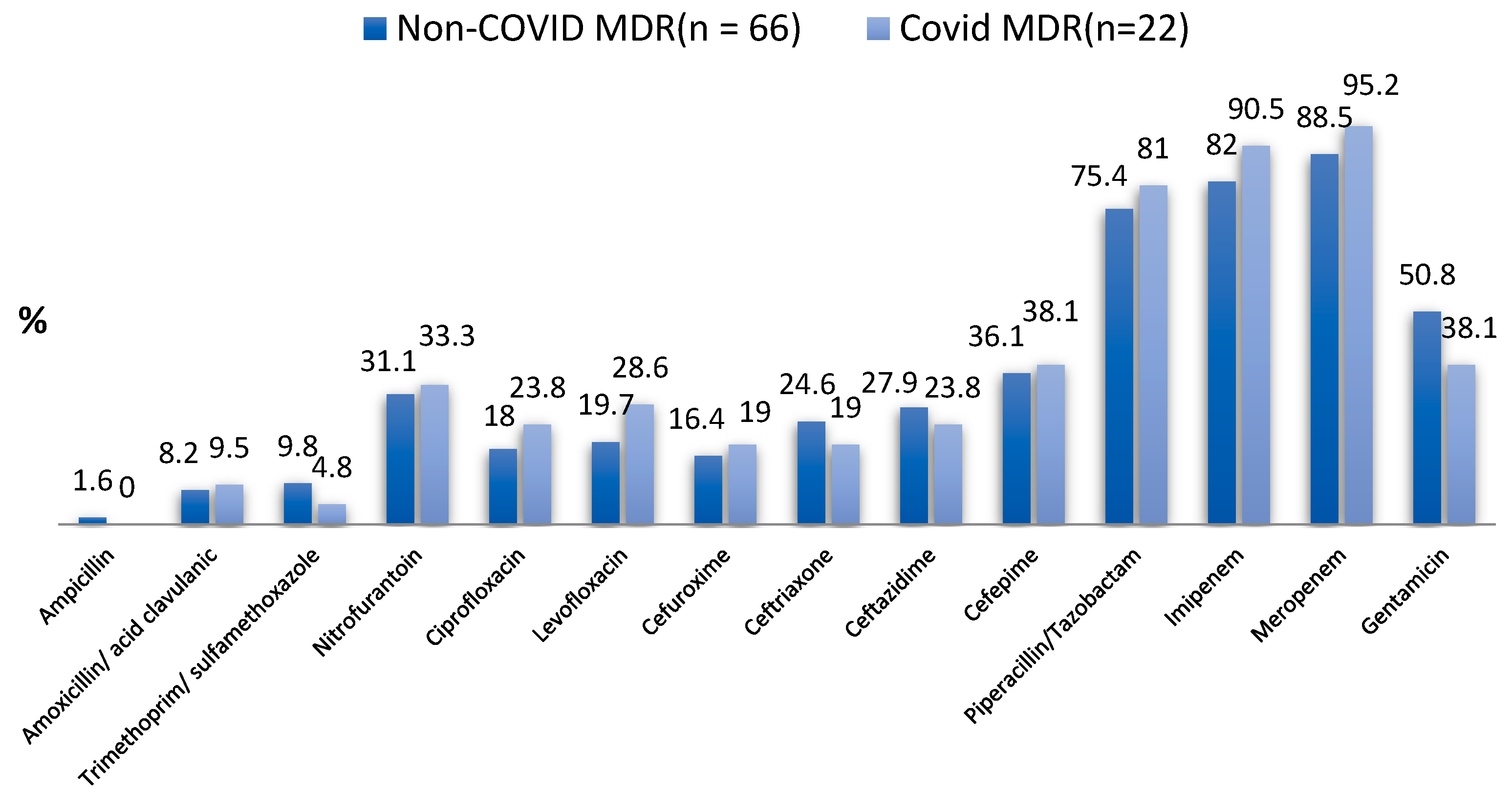
| Type of Tested Antibiotic | Non-COVID MDR UTI (n = 61) | COVID MDR UTI (n = 21) | p-Value for Chi-Square Test and Fisher’s Exact Test |
|---|---|---|---|
| Ampicillin | 1 (1.6%) | 0 (0.0%) | 0.999 |
| Amoxicillin/Acid clavulanic | 5 (8.2%) | 2 (9.5%) | 0.999 |
| Trimethoprim/Sulfamethoxazole | 6 (9.8%) | 1 (4.8%) | 0.671 |
| Nitrofurantoin | 19 (31.1%) | 7 (33.3%) | 0.853 |
| Ciprofloxacin | 11 (18.0%) | 5 (23.8%) | 0.541 |
| Levofloxacin | 12 (19.7%) | 6 (28.6%) | 0.542 |
| Cefuroxime | 10 (16.4%) | 4 (19.0%) | 0.747 |
| Ceftriaxone | 15 (24.6%) | 4 (19.0%) | 0.768 |
| Ceftazidime | 17 (27.9%) | 5 (23.8%) | 0.717 |
| Cefepime | 22 (36.1%) | 8 (38.1%) | 0.868 |
| Piperacillin/Tazobactam | 46 (75.4%) | 17 (81.0%) | 0.768 |
| Imipenem | 50 (82.0%) | 19 (90.5%) | 0.498 |
| Meropenem | 54 (88.5%) | 20 (95.2%) | 0.673 |
| Gentamicin | 31 (50.8%) | 8 (38.1%) | 0.314 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Radu, V.D.; Costache, R.C.; Onofrei, P.; Miftode, E.; Linga, I.; Ouatu, R.M.; Boiculese, L.; Bobeica, R.L.; Tanasa Vasilache, I.; Mititiuc, I.L. Multidrug-Resistant (MDR) Urinary Tract Infections Associated with Gut Microbiota in CoV and Non-CoV Patients in a Urological Clinic during the Pandemic: A Single Center Experience. Antibiotics 2023, 12, 973. https://doi.org/10.3390/antibiotics12060973
Radu VD, Costache RC, Onofrei P, Miftode E, Linga I, Ouatu RM, Boiculese L, Bobeica RL, Tanasa Vasilache I, Mititiuc IL. Multidrug-Resistant (MDR) Urinary Tract Infections Associated with Gut Microbiota in CoV and Non-CoV Patients in a Urological Clinic during the Pandemic: A Single Center Experience. Antibiotics. 2023; 12(6):973. https://doi.org/10.3390/antibiotics12060973
Chicago/Turabian StyleRadu, Viorel Dragos, Radu Cristian Costache, Pavel Onofrei, Egidia Miftode, Iacov Linga, Radu Mihaita Ouatu, Lucian Boiculese, Razvan Lucian Bobeica, Ingrid Tanasa Vasilache, and Irina Luanda Mititiuc. 2023. "Multidrug-Resistant (MDR) Urinary Tract Infections Associated with Gut Microbiota in CoV and Non-CoV Patients in a Urological Clinic during the Pandemic: A Single Center Experience" Antibiotics 12, no. 6: 973. https://doi.org/10.3390/antibiotics12060973
APA StyleRadu, V. D., Costache, R. C., Onofrei, P., Miftode, E., Linga, I., Ouatu, R. M., Boiculese, L., Bobeica, R. L., Tanasa Vasilache, I., & Mititiuc, I. L. (2023). Multidrug-Resistant (MDR) Urinary Tract Infections Associated with Gut Microbiota in CoV and Non-CoV Patients in a Urological Clinic during the Pandemic: A Single Center Experience. Antibiotics, 12(6), 973. https://doi.org/10.3390/antibiotics12060973







