The Prevalence of Carbapenemase-Producing Microorganisms and Use of Novel Cephalosporins for the Treatment of Severe Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria in a Pediatric Cardiac Intensive Care Unit
Abstract
1. Introduction
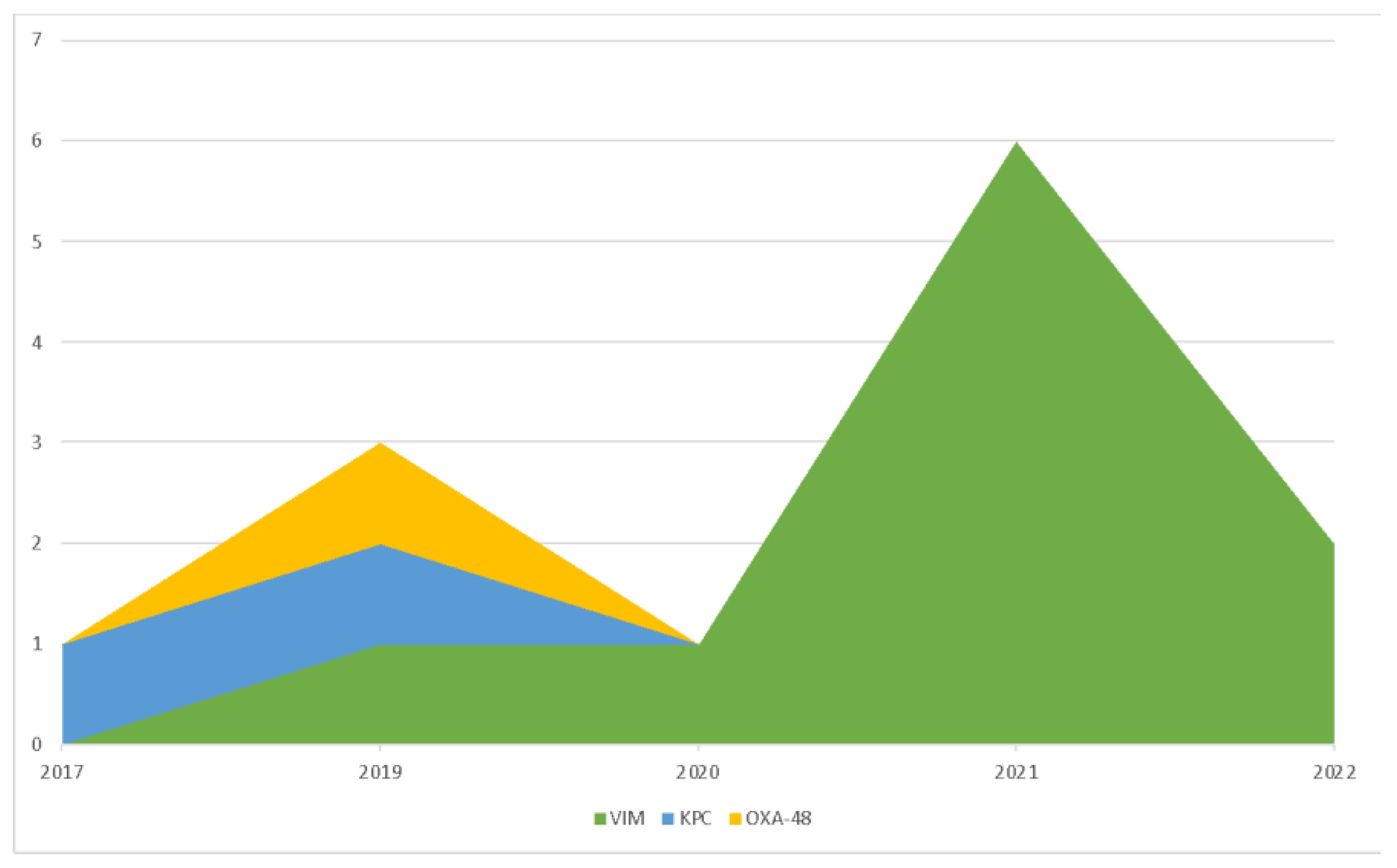
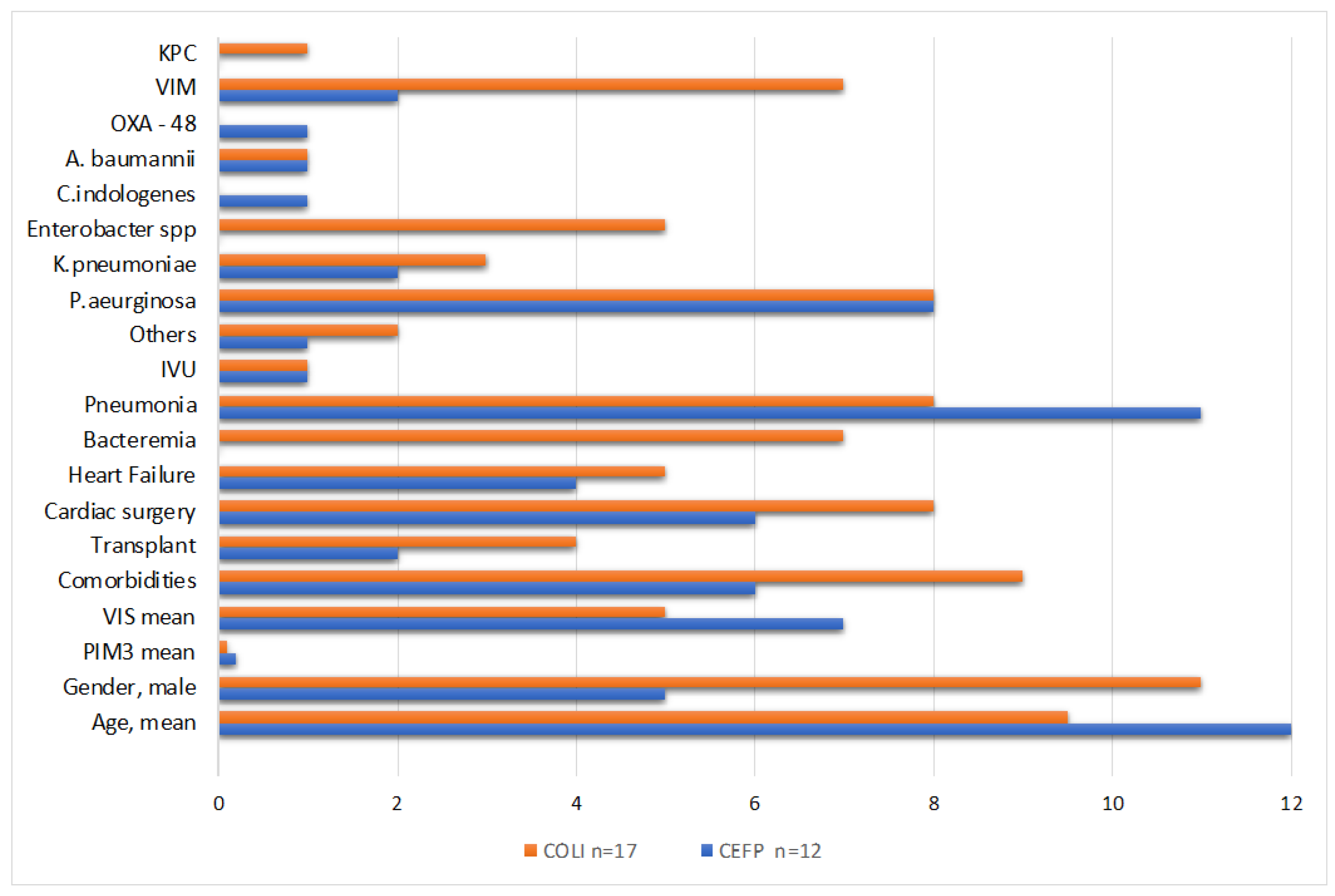
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Definitions
4.2. Statistical Analysis
4.3. Microbiological Cultures and Antibiotic Susceptibility Testing
4.4. PCR-Based Methods for Carbapenemase Genes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. 2014. Available online: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis (accessed on 28 February 2023).
- ISS, the National Institute of Health in Italy. Available online: https://www.iss.it (accessed on 28 February 2023).
- Grundmann, H.; Glasner, C.; Albiger, B.; Aanensen, D.M.; Tomlinson, C.T.; Andrasević, A.T.; Cantón, R.; Carmeli, Y.; Friedrich, A.W.; Giske, C.G.; et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): A prospective, multinational study. Lancet Infect. Dis. 2017, 17, 153–163. [Google Scholar] [CrossRef]
- Lat, I.; Daley, M.J.; Shewale, A.; Pangrazzi, M.H.; Hammond, D.; Olsen, K.M.; DEFINE Study Group and the Discovery Research Network. A multicenter, prospective, observational study to determine predictive factors for multidrug resistant pneumonia in critically ill adults: The DEFINE study. Pharmacotherapy 2018, 39, 253–260. [Google Scholar] [CrossRef]
- McCann, E.; Srinivasan, A.; DeRyke, C.A.; Ye, G.; DePestel, D.D.; Murray, J.; Gupta, V. Carbapenem-Nonsusceptible Gram-Negative Pathogens in ICU and Non-ICU Settings in US Hospitals in 2017: A Multicenter Study. Open Forum. Infect. Dis. 2018, 5, ofy241. [Google Scholar] [CrossRef] [PubMed]
- Shorr, A.F. Review of studies of the impact on Gram-negative bacterial resistance on outcomes in the intensive care unit. Crit. Care Med. 2009, 37, 1463–1469. [Google Scholar] [CrossRef] [PubMed]
- Hall, M.W.; Greathouse, K.C.; Thakkar, R.K.; Sribnick, E.A.; Muszynski, J.A. Immunoparalysis in Pediatric Critical Care. Pediatr. Clin. N. Am. 2017, 64, 1089–1102. [Google Scholar] [CrossRef] [PubMed]
- Au Giacobbe, D.R.; Corcione, S.; Salsano, A.; Del Puente, F.; Mornese Pinna, S.; De Rosa, F.G.; Mikulska, M.; Santini, F.; Viscoli, C. Current and emerging pharmacotherapy for the treatment of infections following open-heart surgery. Expert Opin. Pharm. 2019, 20, 751–772. [Google Scholar] [CrossRef]
- Doi, Y. Treatment Options for Carbapenem-resistant Gram-negative Bacterial Infections. Clin. Infect. Dis. 2019, 69, S565–S575. [Google Scholar] [CrossRef]
- Sheu, C.C.; Chang, Y.T.; Lin, S.Y.; Chen, Y.H.; Hsueh, P.R. Infections Caused by Carbapenem-Resistant Enterobacteriaceae: An Update on Therapeutic Options. Front. Microbiol. 2019, 10, 80. [Google Scholar] [CrossRef] [PubMed]
- CDC’s 2019 Antibiotic Resistance Threats Report. Available online: www.cdc.gov/DrugResistance/Biggest-Threats.html (accessed on 28 February 2023).
- Logan, L.K. Carbapenem-resistant enterobacteriaceae: An emerging problem in children. Clin. Infect. Dis. 2012, 55, 852–859. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Kontopidou, F.; Katerelos, P.; Daikos, G.; Roilides, E.; Theodoridou, M. Infections caused by carbapenem-resistant Gram-negative pathogens in hospitalized children. Pediatr. Infect. Dis. J. 2013, 32, e151–e154. [Google Scholar] [CrossRef]
- Montagnani, C.; Prato, M.; Scolfaro, C.; Colombo, S.; Esposito, S.; Tagliabue, C.; Lo Vecchio, A.; Bruzzese, E.; Loy, A.; Cursi, L.; et al. Italian Society of Pediatric Infectious Diseases. Carbapenem-resistant Enterobacteriaceae Infections in Children: An Italian Retrospective Multicenter Study. Pediatr. Infect. Dis. J. 2016, 61, e01440-17. [Google Scholar]
- Hammoudi Halat, D.; Ayoub Moubareck, C. The Current Burden of Carbapenemases: Review of Significant Properties and Dissemination among Gram-Negative Bacteria. Antibiotics 2020, 9, 186. [Google Scholar] [CrossRef] [PubMed]
- Yin, L.; He, L.; Miao, J.; Yang, W.; Wang, X.; Ma, J.; Wu, N.; Cao, Y.; Wang, C. Carbapenem-resistant Enterobacterales colonization and subsequent infection in a neonatal intensive care unit in Shanghai, China. Infect. Prev. Pract. 2021, 3, 100147. [Google Scholar] [CrossRef]
- Marimuthu, K.; Ng, O.T.; Cherng, B.P.Z.; Fong, R.K.C.; Pada, S.K.; De, P.P.; Ooi, S.T.; Smitasin, N.; Thoon, K.C.; Krishnan, P.U.; et al. Antecedent Carbapenem Exposure as a Risk Factor for Non-Carbapenemase-Producing Carbapenem-Resistant Enterobacteriaceae and Carbapenemase-Producing Enterobacteriaceae. Antimicrob Agents Chemother. 2019, 63, e00845-19. [Google Scholar] [CrossRef]
- Queenan, A.M.; Bush, K. Carbapenemases: The versatile betalactamases. Clin. Microbiol. Rev. 2007, 20, 440–458. [Google Scholar] [CrossRef]
- Chia, J.H.; Siu, L.K.; Su, L.H.; Lin, H.S.; Kuo, A.J.; Lee, M.H.; Wu, T.L. Emergence of carbapenem-resistant Escherichia coli in Taiwan: Resistance due to combined CMY-2 production and porin deficiency. J. Chemother. 2009, 21, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Armand-Lefèvre, L.; Angebault, C.; Barbier, F.; Hamelet, E.; Defrance, G.; Ruppé, E.; Bronchard, R.; Lepeule, R.; Lucet, J.C.; El Mniai, A.; et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013, 57, 1488–1495. [Google Scholar] [CrossRef]
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America 2022 Guidance on the Treatment of Extended-Spectrum β-lactamase Producing Enterobacterales (ESBL-E), Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with Difficult-to-Treat Resistance (DTR-P. aeruginosa). Clin. Infect. Dis. 2022, 75, 187–212. [Google Scholar] [PubMed]
- Gutiérrez-Gutiérrez, B.; Salamanca, E.; de Cueto, M.; Hsueh, P.R.; Viale, P.; Paño-Pardo, J.R.; Venditti, M.; Tumbarello, M.; Daikos, G.; Cantón, R.; et al. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): A retrospective cohort study. Lancet Infect. Dis. 2017, 17, 726–734. [Google Scholar] [CrossRef]
- Ordooei Javan, A.; Shokouhi, S.; Sahraei, Z. A review on colistin nephrotoxicity. Eur. J. Clin. Pharmacol. 2015, 71, 801–810. [Google Scholar] [CrossRef]
- Chen, Y.; Huang, H.B.; Peng, J.M.; Weng, L.; Du, B. Efficacy and Safety of Ceftazidime-Avibactam for the Treatment of Carbapenem-Resistant Enterobacterales Bloodstream Infection: A Systematic Review and Meta-Analysis. Microbiol. Spectr. 2022, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Bassetti, M.; Garau, J. Current and future perspectives in the treatment of multidrug-resistant Gram-negative infections. J. Antimicrob. Chemother. 2021, 76, iv23–iv37. [Google Scholar] [CrossRef] [PubMed]
- Van Duin, D.; Lok, J.J.; Earley, M.; Cober, E.; Richter, S.S.; Perez, F.; Salata, R.A.; Kalayjian, R.C.; Watkins, R.R.; Doi, Y.; et al. Antibacterial Resistance Leadership Group. Colistin Versus Ceftazidime-Avibactam in the Treatment of Infections Due to Carbapenem-Resistant Enterobacteriaceae. Clin. Infect. Dis. 2018, 66, 163–171. [Google Scholar] [CrossRef]
- Shields, R.K.; Nguyen, M.H.; Chen, L.; Press, E.G.; Potoski, B.A.; Marini, R.V.; Doi, Y.; Kreiswirth, B.N.; Clancy, C.J. Ceftazidime-Avibactam Is Superior to Other Treatment Regimens against Carbapenem-Resistant Klebsiella pneumoniae Bacteremia. Antimicrob. Agents Chemother. 2017, 61, e00883-17. [Google Scholar] [CrossRef] [PubMed]
- Castón, J.J.; Lacort-Peralta, I.; Martín-Dávila, P.; Loeches, B.; Tabares, S.; Temkin, L.; Torre-Cisneros, J.; Paño-Pardo, J.R. Clinical efficacy of ceftazidime/avibactam versus other active agents for the treatment of bacteremia due to carbapenemase-producing Enterobacteriaceae in hematologic patients. Int. J. Infect. Dis. 2017, 59, 118–123. [Google Scholar] [CrossRef]
- Alraddadi, B.M.; Saeedi, M.; Qutub, M.; Alshukairi, A.; Hassanien, A.; Wali, G. Efficacy of ceftazidime-avibactam in the treatment of infections due to Carbapenem-resistant Enterobacteriaceae. BMC Infect Dis. 2019, 19, 772. [Google Scholar] [CrossRef]
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters, Version 10.0. 2020. Available online: https://www.eucast.org/ (accessed on 28 February 2023).
| Sepsis/ Septic Shock | Pneumonia | UTI | Others | Total n° (%) | |
|---|---|---|---|---|---|
| P. aeruginosa | 6 | 18 | 2 | 1 | 27 (64) |
| Non-Carbapenemase Producers | 6 | 15 | 2 | 1 | 24 (89) |
| Carbapenemase Producers | 0 | 3 | 0 | 0 | 3 (11) |
| VIM | 0 | 3 | 0 | 0 | 3 (11) |
| K. pneumoniae | 3 | 1 | 1 | 1 | 6 (14) |
| Non-Carbapenemase Producers | 0 | 0 | 1 | 1 | 2 (33) |
| Carbapenemase Producers | 3 | 1 | 0 | 0 | 4 (66) |
| VIM | 1 | 0 | 0 | 0 | 1 (17) |
| KPC | 2 | 0 | 0 | 0 | 2 (33) |
| OXA 48 | 0 | 1 | 0 | 0 | 1 (17) |
| Enterobacter spp. | 4 | 1 | 0 | 1 | 6 (14) |
| Non-Carbapenemase Producers | 1 | 0 | 0 | 0 | 1 (17) |
| Carbapenemase Producers | 3 | 1 | 0 | 1 | 5 (83) |
| VIM | 3 | 1 | 0 | 1 | 5 (83) |
| A. baumannii | 0 | 2 | 0 | 0 | 2 (5) |
| Non-Carbapenemase Producers | 0 | 1 | 0 | 0 | 1 (50) |
| Carbapenemase Producers | 0 | 1 | 0 | 0 | 1 (50) |
| VIM | 0 | 1 | 0 | 0 | 1 (50) |
| C. indologenes | 0 | 1 | 0 | 0 | 1 (2) |
| Non-Carbapenemase Producers | 0 | 1 | 0 | 0 | 1 (100) |
| Characteristics of the Treatment | No. (%) |
|---|---|
| Empiric Therapy | 22 (52) |
| Carbapenems | 10 (45) |
| Piperacillin/Tazobactam | 2 (9) |
| Ceftazidime/Avibactam | 6 (27) |
| Others (e.g., glycopetides, aminoglycosides, fluoroquinolones) | 4 (20) |
| Combined therapy for empiric therapy | 6 (27) |
| Targeted therapy | |
| Monotherapy | 20 (48) |
| Ceftazidime/Avibactam | 10 (50) |
| Colistin | 2 (10) |
| Ceftolozane/Tazobactam | 2 (10) |
| Cefiderocol | 1 (5) |
| Others (e.g., fluoroquinolones, tigecyclin) | 5 (25) |
| Combined therapy | 22 (52) |
| Carbapenems + Colistin | 14 (63.3) |
| Ceftazidime/Avibactam + Colistin | 2 (9) |
| Carbapenems + Aminoglycosides | 1 (4.5) |
| Colistin + Aminoglycosides | 1 (4.5) |
| Others (e.g., cephalosporines + fluoroquinolones, cephalosporines + aminoglycosides) | 4 (18.2) |
| Adverse reactions during treatment | 0 |
| First line therapy failure | 3 (7) |
| Total n = 29 (%) | N-CEFs n = 12 (%) | COLI n = 17 (%) | p-Value | |
|---|---|---|---|---|
| Clinical Cure | 13 (45) | 8 (67) | 5 (29) | 0.04 |
| Attributable mortality to CRO | 1 (3) | 0 | 1 (6) | 1 |
| 30-day relapse by the same isolate | 2 (7) | 1 (8) | 1 (6) | 1 |
| 30-day all-cause mortality | 4 (14) | 1 (8) | 3 (18) | 0.62 |
| Therapy discontinuation due to adverse events | 0 | 0 | 0 | |
| Length of overall hospitalization, median, days | 179.5 | 116 | 0.46 | |
| Length of CICU stay, median, days | 98 | 113 | 0.7 | |
| Overall duration of therapy, median, days | 14 | 14 | 1 | |
| Duration of targeted therapy, median, days | 11.5 | 13 | 0.98 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tripiciano, C.; Romani, L.; Mercadante, S.; Cursi, L.; Di Giuseppe, M.; Calo Carducci, F.I.; Fragasso, T.; Di Chiara, L.; Garisto, C.; Sisto, A.; et al. The Prevalence of Carbapenemase-Producing Microorganisms and Use of Novel Cephalosporins for the Treatment of Severe Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria in a Pediatric Cardiac Intensive Care Unit. Antibiotics 2023, 12, 796. https://doi.org/10.3390/antibiotics12050796
Tripiciano C, Romani L, Mercadante S, Cursi L, Di Giuseppe M, Calo Carducci FI, Fragasso T, Di Chiara L, Garisto C, Sisto A, et al. The Prevalence of Carbapenemase-Producing Microorganisms and Use of Novel Cephalosporins for the Treatment of Severe Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria in a Pediatric Cardiac Intensive Care Unit. Antibiotics. 2023; 12(5):796. https://doi.org/10.3390/antibiotics12050796
Chicago/Turabian StyleTripiciano, Costanza, Lorenza Romani, Stefania Mercadante, Laura Cursi, Martina Di Giuseppe, Francesca Ippolita Calo Carducci, Tiziana Fragasso, Luca Di Chiara, Cristiana Garisto, Annamaria Sisto, and et al. 2023. "The Prevalence of Carbapenemase-Producing Microorganisms and Use of Novel Cephalosporins for the Treatment of Severe Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria in a Pediatric Cardiac Intensive Care Unit" Antibiotics 12, no. 5: 796. https://doi.org/10.3390/antibiotics12050796
APA StyleTripiciano, C., Romani, L., Mercadante, S., Cursi, L., Di Giuseppe, M., Calo Carducci, F. I., Fragasso, T., Di Chiara, L., Garisto, C., Sisto, A., Vallesi, L., Costabile, V., Lancella, L., Bernaschi, P., & De Luca, M. (2023). The Prevalence of Carbapenemase-Producing Microorganisms and Use of Novel Cephalosporins for the Treatment of Severe Infections Caused by Carbapenem-Resistant Gram-Negative Bacteria in a Pediatric Cardiac Intensive Care Unit. Antibiotics, 12(5), 796. https://doi.org/10.3390/antibiotics12050796






