Neonatal Brain Abscess with Serratia marcescens after Intrauterine Infection: A Case Report
Abstract
1. Introduction
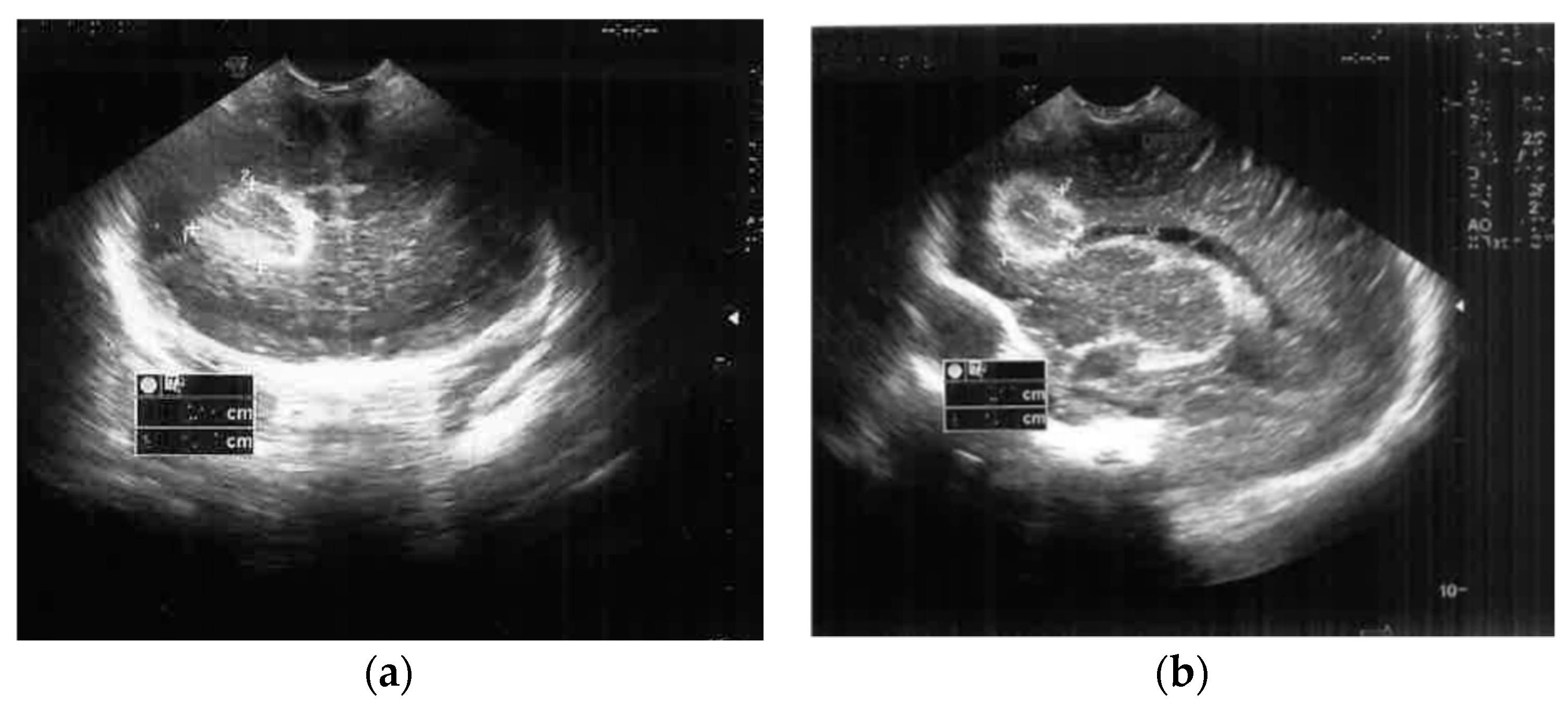
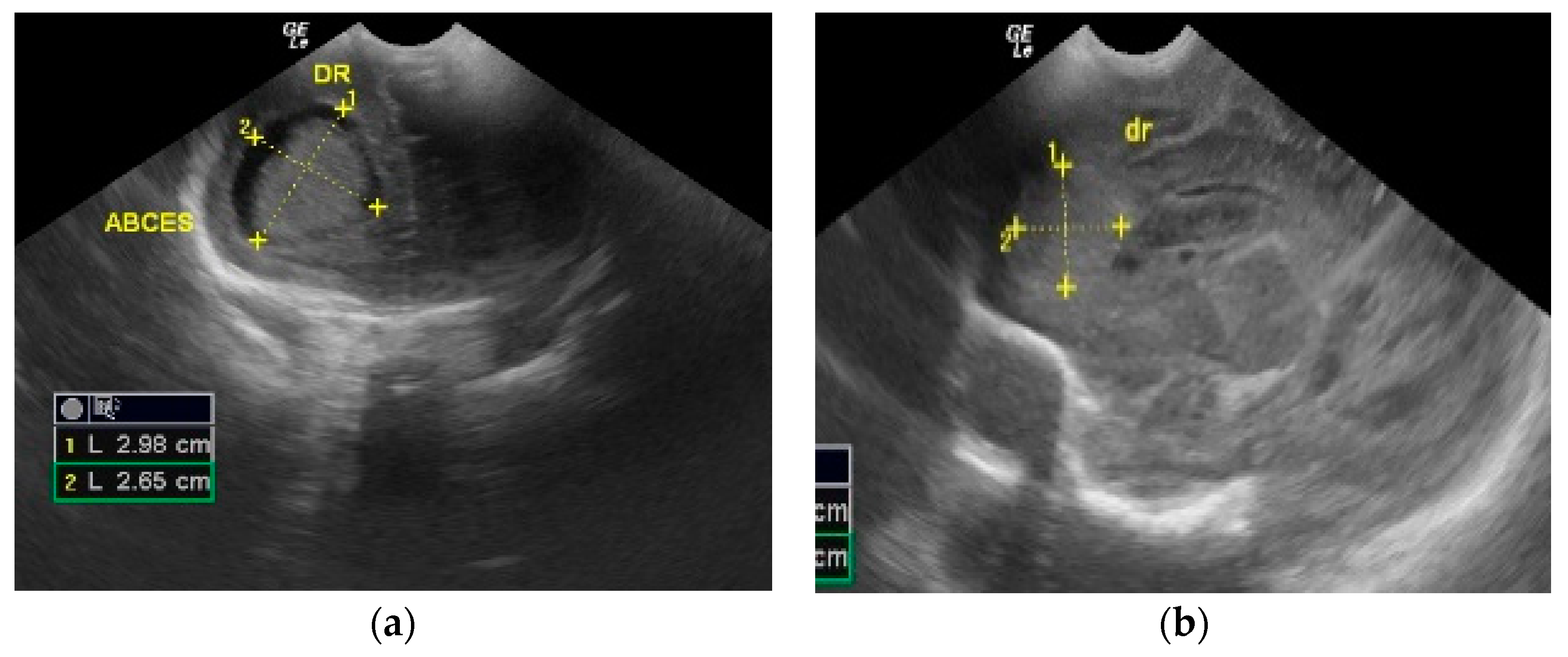
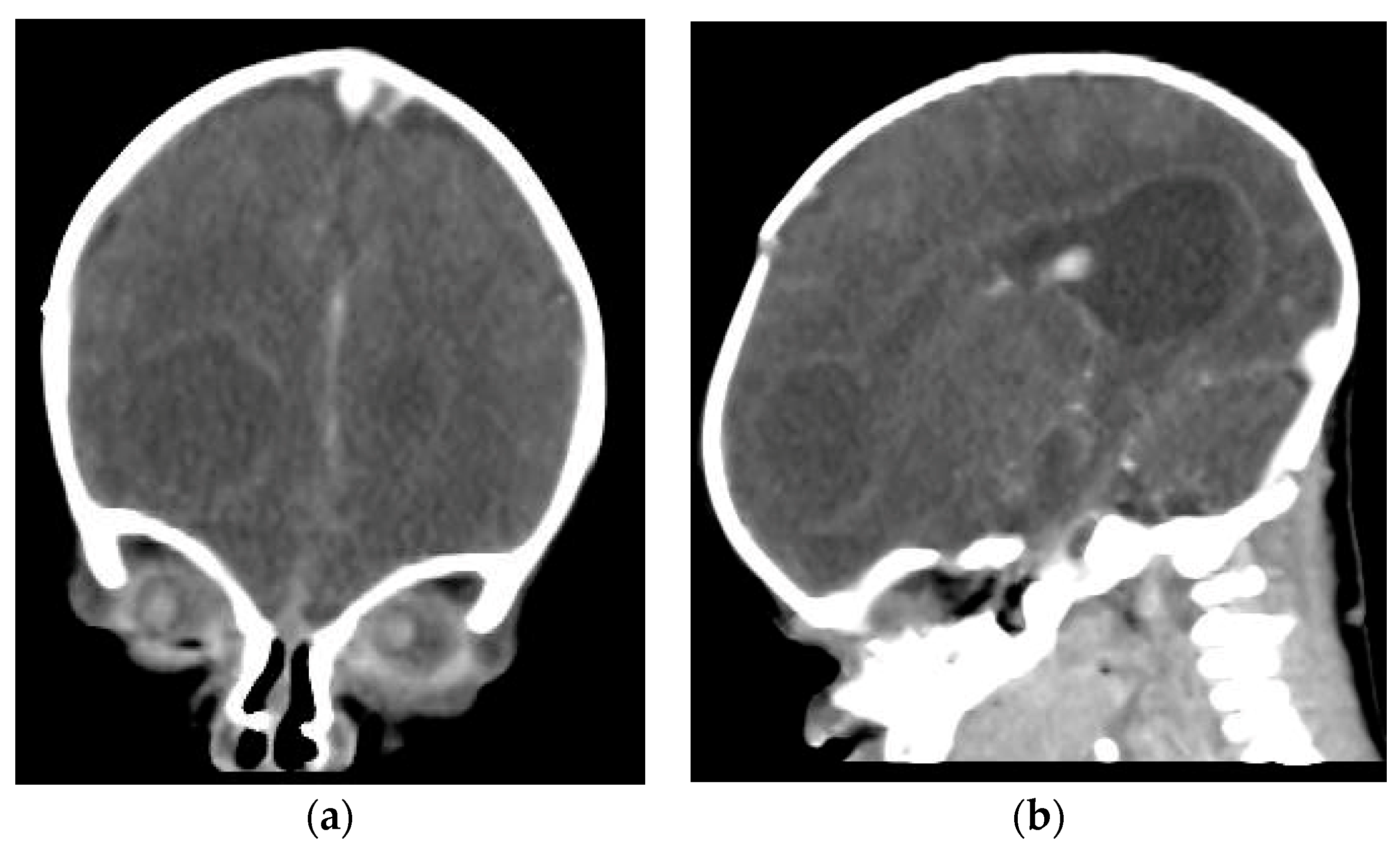
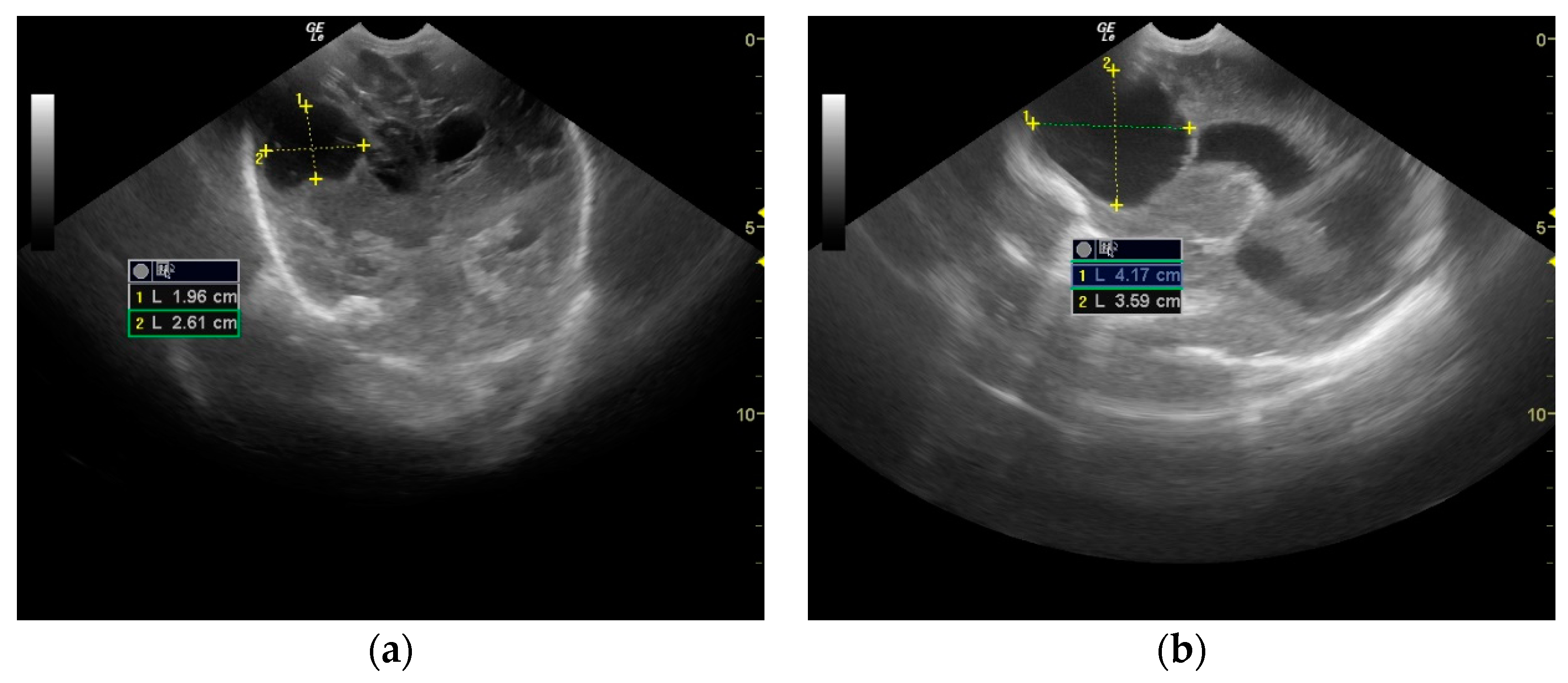
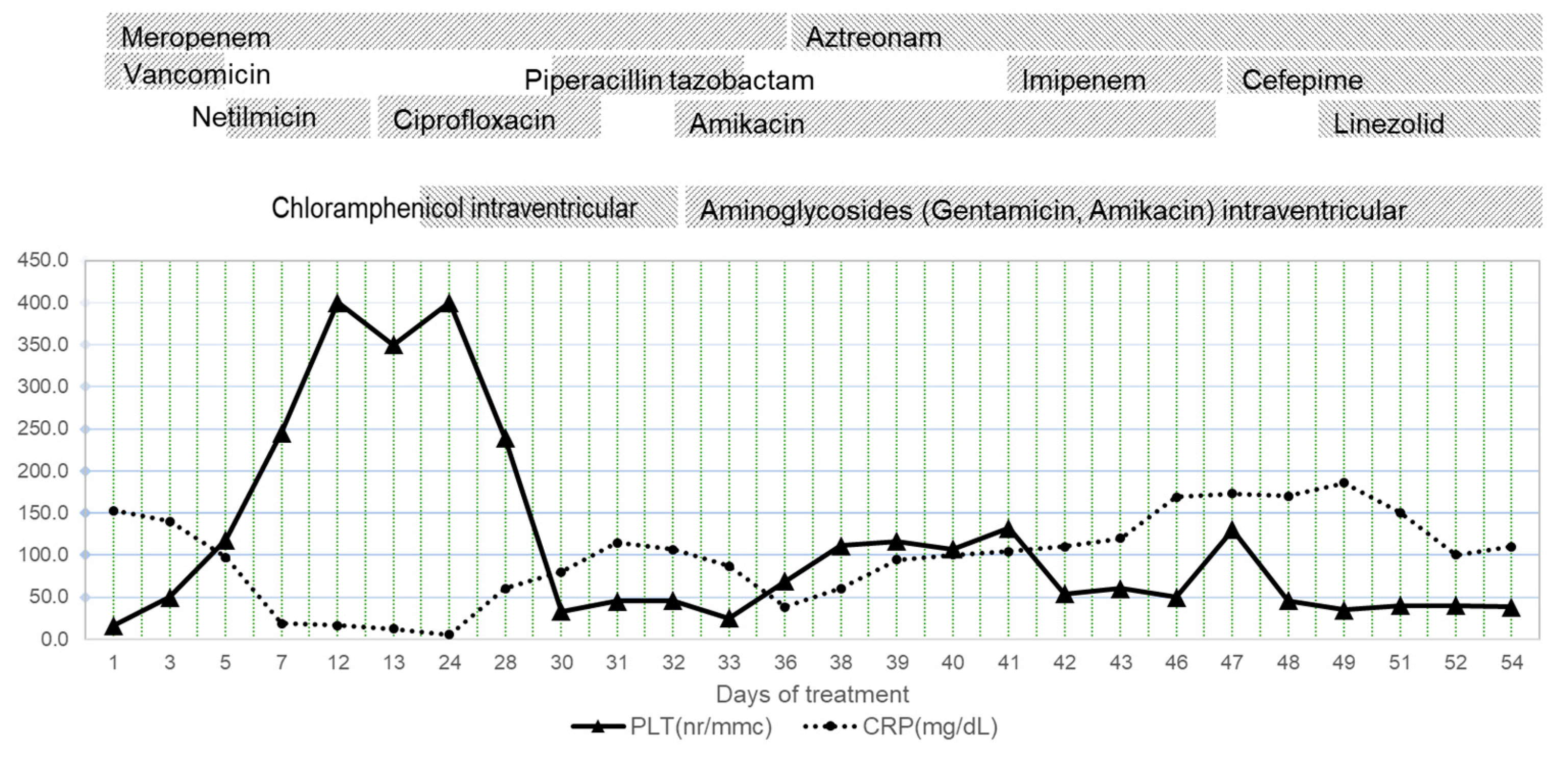
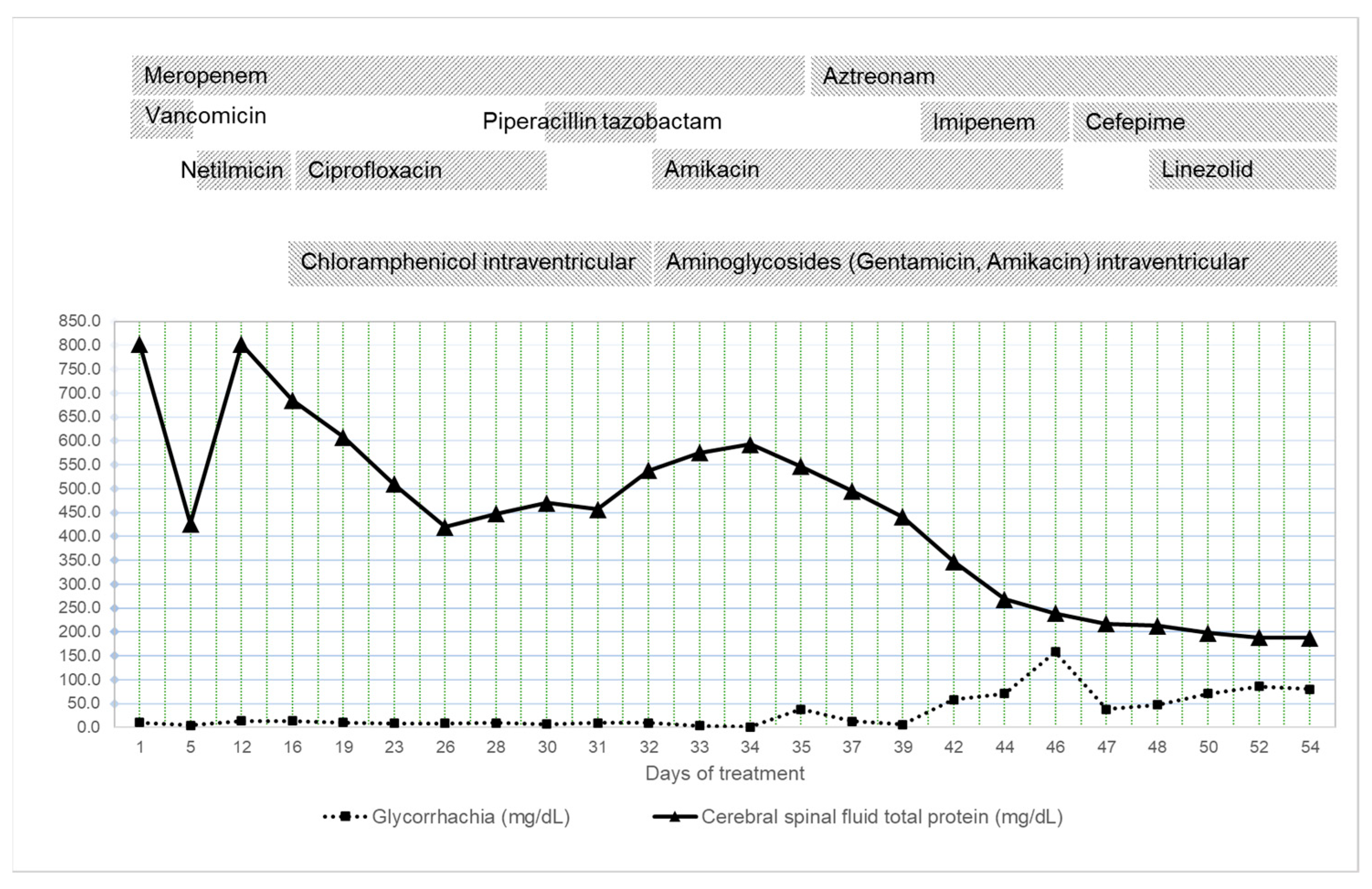
2. Case Presentation
3. Discussion
4. Conclusions
5. Teaching Point
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ottria, G.; Dallera, M.; Aresu, O.; Manniello, M.A.; Parodi, B.; Spagnolo, A.M.; Cristina, M.L. Environmental monitoring programme in the cell therapy facility of a research centre: Preliminary investigation. J. Prev. Med. Hyg. 2010, 51, 133–138. [Google Scholar]
- Al Jarousha, A.M.; El Qouqa, A.; El Jadba, A.H.; Al Afifi, A.S. An outbreak of Serratia marcescens septicaemia in neonatal intensive care unit in Gaza City, Palestine. J. Hosp. Infect. 2008, 70, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Su, L.H.; Ou, J.T.; Leu, H.S.; Chiang, P.C.; Chiu, Y.P.; Chia, J.H.; Kuo, A.J.; Chiu, C.H.; Chu, C.; Wu, T.L.; et al. Extended epidemic of nosocomial urinary tract infections caused by Serratia marcescens. J. Clin. Microbiol. 2003, 41, 4726–4732. [Google Scholar] [CrossRef] [PubMed]
- Tavares-Carreon, F.; De Anda-Mora, K.; Rojas-Barrera, I.C.; Andrade, A. Serratia marcescens antibiotic resistance mechanisms of an opportunistic pathogen: A literature review. PeerJ 2023, 11, e14399. [Google Scholar] [CrossRef]
- Gastmeier, P.; Loui, A.; Stamm-Balderjahn, S.; Hansen, S.; Zuschneid, I.; Sohr, D.; Behnke, M.; Obladen, M.; Vonberg, R.P.; Rüden, H. Outbreaks in neonatal intensive care units—They are not like others. Am. J. Infect. Control. 2007, 35, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Millán-Lou, M.I.; López, C.; Bueno, J.; Pérez-Laguna, V.; Lapresta, C.; Fuertes, M.E.; Rite, S.; Santiago, M.; Romo, M.; Samper, S.; et al. Successful control of Serratia marcescens outbreak in a neonatal unit of a tertiary-care hospital in Spain. Enferm. Infecc. Microbiol. Clin. (Engl. Ed.) 2022, 5, 248–254. [Google Scholar] [CrossRef]
- Casolari, C.; Pecorari, M.; Fabio, G.; Cattani, S.; Venturelli, C.; Piccinini, L.; Tamassia, M.G.; Gennari, W.; Sabbatini, A.M.; Leporati, G.; et al. A simultaneous outbreak of Serratia marcescens and Klebsiella pneumoniae in a neonatal intensive care unit. J. Hosp. Infect. 2005, 61, 312–320. [Google Scholar] [CrossRef]
- Arslan, U.; Erayman, I.; Kirdar, S.; Yuksekkaya, S.; Cimen, O.; Tuncer, I.; Bozdogan, B. Serratia marcescens sepsis outbreak in a neonatal intensive care unit. Pediatr. Int. 2010, 52, 208–212. [Google Scholar] [CrossRef]
- Maragakis, L.L.; Winkler, A.; Tucker, M.G.; Cosgrove, S.E.; Ross, T.; Lawson, E.; Carroll, K.C.; Perl, T.M. Outbreak of multidrug-resistant Serratia marcescens infection in a neonatal intensive care unit. Infect. Control. Hosp. Epidemiol. 2008, 29, 418–423. [Google Scholar] [CrossRef]
- Coggins, S.A.; Edwards, E.M.; Flannery, D.D.; Gerber, J.S.; Horbar, J.D.; Puopolo, K.M. Serratia Infection Epidemiology Among Very Preterm Infants in the Neonatal Intensive Care Unit. Pediatr. Infect. Dis. J. 2023, 42, 152–158. [Google Scholar] [CrossRef]
- Friedman, N.D.; Kotsanas, D.; Brett, J.; Billah, B.; Korman, T.M. Investigation of an outbreak of Serratia marcescens in a neonatal unit via a case-control study and molecular typing. Am. J. Infect. Control. 2008, 36, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Villari, P.; Crispino, M.; Salvadori, A.; Scarcella, A. Molecular epidemiology of an outbreak of Serratia marcescens in a neonatal intensive care unit. Infect. Control. Hosp. Epidemiol. 2001, 22, 630–634. [Google Scholar] [CrossRef]
- Bentlin, M.R.; de Souza Rugolo, L.M.S. Late-onset Sepsis: Epidemiology, Evaluation, and Outcome. NeoReviews 2010, 11, e426–e435. [Google Scholar] [CrossRef]
- Hadžimuratović, E.; Hadžimuratović, A.; Hadžipašić, A. Multiple brain abscesses caused by Serratia marcescens in preterm newborn. Case Rep. Perinat. Med. 2017, 7, 20170020. [Google Scholar] [CrossRef]
- Feferbaum, R.; Diniz, E.M.; Valente, M.; Giolo, C.R.; Vieira, R.A.; Galvani, A.L.; Ceccon, M.E.; Araujo, M.C.; Krebs, V.L.; Vaz, F.A. Brain abscess by citrobacter diversus in infancy: Case report. Arq. Neuropsiquiatr. 2000, 58, 736–740. [Google Scholar] [CrossRef]
- de Oliveira, R.S.; Pinho, V.F.; Madureira, J.F.; Machado, H.R. Brain abscess in a neonate: An unusual presentation. Childs Nerv. Syst. 2007, 23, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Lappay, J.I.; Gaddi, M.J.S.; Calotes-Castillo, L.V. Serratia marcescens Healthcare-Associated Ventriculitis and Cerebral Abscess in a Neonate with Chiari II Malformation: A Case Report and Systematic Review. Acta. Med. Philipp. 2022, 56, 10. Available online: https://actamedicaphilippina.upm.edu.ph/index.php/acta/article/view/82 (accessed on 3 February 2023).
- Hirooka, T.M.; Fontes, R.B.; Diniz, E.M.; Pinto, F.C.; Matushita, H. Cerebral abscess caused by Serratia marcescens in a premature neonate. Arq. Neuropsiquiatr. 2007, 65, 1018–1021. [Google Scholar] [CrossRef]
- de Vries, L.S.; Volpe, J.J. Chapter 35-Bacterial and Fungal Intracranial Infections. In Volpe’s Neurology of the Newborn, 6th ed.; Volpe, J.J., Inder, T.E., Darras, B.T., de Vries, L.S., du Plessis, A.J., Neil, J., Perlman, J., Eds.; Elsevier: Amsterdam, The Netherlands, 2018; pp. 1050–1089. ISBN 9780323428767. [Google Scholar] [CrossRef]
- Renier, D.; Flandin, C.; Hirsch, E.; Hirsch, J.F. Brain abscesses in neonates. A study of 30 cases. J. Neurosurg. 1988, 69, 877–882. [Google Scholar] [CrossRef]
- Zaidi, A.K.; Thaver, D.; Ali, S.A.; Khan, T.A. Pathogens associated with sepsis in newborns and young infants in developing countries. Pediatr. Infect. Dis. J. 2009, 28, S10–S18. [Google Scholar] [CrossRef]
- Cristina, M.L.; Sartini, M.; Spagnolo, A.M. Serratia marcescens Infections in Neonatal Intensive Care Units (NICUs). Int. J. Environ. Res. Public. Health. 2019, 16, 610. [Google Scholar] [CrossRef] [PubMed]
- Mahlen, S.D. Serratia infections: From military experiments to current practice. Clin. Microbiol. Rev. 2011, 24, 755–791. [Google Scholar] [CrossRef] [PubMed]
- Madide, A.; Smith, J. Intracranial complications of Serratia marcescens infection in neonates. S. Afr. Med. J. 2016, 106, 36–38. [Google Scholar] [CrossRef] [PubMed]
- Celik, I.H.; Demirel, G.; Erdeve, O.; Uraş, N.; Dilmen, U. Multiple large brain abscesses in a newborn that may have resulted from intrauterine infection. Turk. J. Pediatr. 2011, 53, 561–566. [Google Scholar] [PubMed]
- Ottolini, K.M.; Litke-Wager, C.A.; Johnson, R.L.; Schulz, E.V. Serratia Chorioamnionitis and Culture Proven Sepsis in a Preterm Neonate: A Case Report and Review of the Literature. Pediatr. Infect. Dis. J. 2021, 40, e62–e65. [Google Scholar] [CrossRef] [PubMed]
- Erenberg, M.; Yagel, Y.; Press, F.; Weintraub, A.Y. Chorioamnionitis caused by Serratia marcescens in a healthy pregnant woman with preterm premature rupture of membranes: A rare case report and review of the literature. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 211, 227–230. [Google Scholar] [CrossRef]
- Shiqiao, H.; Bei, X.; Yudi, G.; Lei, J. Assisted reproductive technology is associated with premature rupture of membranes. J. Matern. Fetal Neonatal Med. 2021, 34, 555–561. [Google Scholar] [CrossRef]
- Lei, L.L.; Lan, Y.L.; Wang, S.Y.; Feng, W.; Zhai, Z.J. Perinatal complications and live-birth outcomes following assisted reproductive technology: A retrospective cohort study. Chin. Med. J. (Engl.) 2019, 132, 2408–2416. [Google Scholar] [CrossRef]
- Barkovich, A.J. The encephalopathic neonate: Choosing the proper imaging technique. AJNR Am. J. Neuroradiol. 1997, 18, 1816–1820. [Google Scholar]
- Messerschmidt, A.; Prayer, D.; Olischar, M.; Pollak, A.; Birnbacher, R. Brain abscesses after Serratia marcescens infection on a neonatal intensive care unit: Differences on serial imaging. Neuroradiology 2004, 46, 148–152. [Google Scholar] [CrossRef]
- Weber, W.; Henkes, H.; Felber, S.; Jänisch, W.; Woitalla, D.; Kühne, D. Septisch-embolischer und septisch-metastatischer Hirnabszess [Septic-embolic and septic metastatic brain abscess]. Radiologe 2000, 40, 1017–1028. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.R.; Diacovo, T.; Baker, C.J. Serratia marcescens meningitis in neonates. Pediatr. Infect. Dis. J. 1992, 11, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Moradigaravand, D.; Boinett, C.J.; Martin, V.; Peacock, S.J.; Parkhill, J. Recent independent emergence of multiple multidrug-resistant Serratia marcescens clones within the United Kingdom and Ireland. Genome Res. 2016, 26, 1101–1109. [Google Scholar] [CrossRef] [PubMed]
- Stock, I.; Grueger, T.; Wiedemann, B. Natural antibiotic susceptibility of strains of Serratia marcescens and the S. liquefaciens complex: S. liquefaciens sensu stricto, S. proteamaculans and S. grimesii. Int. J. Antimicrob. Agents. 2003, 22, 35–47. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.N.; Ferguson, J.K. Antibiotic therapy for inducible AmpC β-lactamase-producing Gram-negative bacilli: What are the alternatives to carbapenems, quinolones and aminoglycosides? Int. J. Antimicrob. Agents. 2012, 40, 297–305. [Google Scholar] [CrossRef]
- Nicasio, A.M.; Quintiliani RJr DeRyke, C.A.; Kuti, J.L.; Nicolau, D.P. Treatment of Serratia marcescens meningitis with prolonged infusion of meropenem. Ann. Pharmacother. 2007, 41, 1077–1081. [Google Scholar] [CrossRef]
- Sharma, B.S.; Gupta, S.K.; Khosla, V.K. Current concepts in the management of pyogenic brain abscess. Neurol. India. 2000, 48, 105–111. [Google Scholar] [PubMed]
- Piccirilli, A.; Cherubini, S.; Brisdelli, F.; Fazii, P.; Stanziale, A.; Di Valerio, S.; Chiavaroli, V.; Principe, L.; Perilli, M. Molecular Characterization by Whole-Genome Sequencing of Clinical and Environmental Serratia marcescens Strains Isolated during an Outbreak in a Neonatal Intensive Care Unit (NICU). Diagnostics 2022, 12, 2180. [Google Scholar] [CrossRef]
- Lu, C.H.; Chang, W.N.; Lui, C.C. Strategies for the management of bacterial brain abscess. J. Clin. Neurosci. 2006, 13, 979–985. [Google Scholar] [CrossRef]
- Spennato, P.; Aliberti, F.; Colaleo, F.; Mirone, G.; Di Martino, G.; Cinalli, G. Endoscopic ultrasonic aspiration of brain abscess. Childs Nerv. Syst. 2018, 34, 1579–1582. [Google Scholar] [CrossRef]
- Yu, X.; Liu, R.; Wang, Y.; Zhao, H.; Chen, J.; Zhang, J.; Hu, C. CONSORT: May stereotactic intracavity administration of antibiotics shorten the course of systemic antibiotic therapy for brain abscesses? Medicine 2017, 96, e6359. [Google Scholar] [CrossRef] [PubMed]
- Gilard, V.; Beccaria, K.; Hartley, J.C.; Blanot, S.; Marqué, S.; Bourgeois, M.; Puget, S.; Thompson, D.; Zerah, M.; Tisdall, M. Brain abscess in children, a two-centre audit: Outcomes and controversies. Arch. Dis. Child. 2020, 105, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.; Kan, J.; Qiu, G.; Zhao, D.; Ren, F.; Luo, Z.; Zhang, Y. Clinical Prognosis in Neonatal Bacterial Meningitis: The Role of Cerebrospinal Fluid Protein. PLoS ONE. 2015, 10, e0141620. [Google Scholar] [CrossRef]
- Pammi, M.; Holland, L.; Butler, G.; Gacser, A.; Bliss, J.M. Candida parapsilosis is a significant neonatal pathogen: A systematic review and meta-analysis. Pediatr. Infect. Dis. J. 2013, 32, e206–e216. [Google Scholar] [CrossRef]
- De Rose, D.U.; Santisi, A.; Ronchetti, M.P.; Martini, L.; Serafini, L.; Betta, P.; Maino, M.; Cavigioli, F.; Cocchi, I.; Pugni, L.; et al. On Behalf Of Study Group Of Neonatal Infectious Diseases. Invasive Candida Infections in Neonates after Major Surgery: Current Evidence and New Directions. Pathogens 2021, 10, 319. [Google Scholar] [CrossRef]
- Juster-Reicher, A.; Flidel-Rimon, O.; Amitay, M.; Even-Tov, S.; Shinwell, E.; Leibovitz, E. High-dose liposomal amphotericin B in the therapy of systemic candidiasis in neonates. Eur. J. Clin. Microbiol. Infect. Dis. 2003, 22, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Moles, L.; Gómez, M.; Moroder, E.; Jiménez, E.; Escuder, D.; Bustos, G.; Melgar, A.; Villa, J.; Del Campo, R.; Chaves, F.; et al. Serratia marcescens colonization in preterm neonates during their neonatal intensive care unit stay. Antimicrob. Resist. Infect. Control. 2019, 8, 135. [Google Scholar] [CrossRef]
| Antimicrobial Agent | Sensitivity |
|---|---|
| Ciprofloxacin | S |
| Trimethoprim-sulfamethoxazole | S |
| Imipenem | S |
| Meropenem | S |
| Amikacin | I |
| Piperacillin-tazobactam | I |
| Amoxicillin | R |
| Ampicillin | R |
| Cefoperazone +/− Sulbactam | R |
| Ceftrixaone | R |
| Cefuroxime | R |
| Gentamicin | R |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bizubac, M.; Balaci-Miroiu, F.; Filip, C.; Vasile, C.M.; Herișeanu, C.; Marcu, V.; Stoica, S.; Cîrstoveanu, C. Neonatal Brain Abscess with Serratia marcescens after Intrauterine Infection: A Case Report. Antibiotics 2023, 12, 722. https://doi.org/10.3390/antibiotics12040722
Bizubac M, Balaci-Miroiu F, Filip C, Vasile CM, Herișeanu C, Marcu V, Stoica S, Cîrstoveanu C. Neonatal Brain Abscess with Serratia marcescens after Intrauterine Infection: A Case Report. Antibiotics. 2023; 12(4):722. https://doi.org/10.3390/antibiotics12040722
Chicago/Turabian StyleBizubac, Mihaela, Francisca Balaci-Miroiu, Cristina Filip, Corina Maria Vasile, Carmen Herișeanu, Veronica Marcu, Sergiu Stoica, and Catalin Cîrstoveanu. 2023. "Neonatal Brain Abscess with Serratia marcescens after Intrauterine Infection: A Case Report" Antibiotics 12, no. 4: 722. https://doi.org/10.3390/antibiotics12040722
APA StyleBizubac, M., Balaci-Miroiu, F., Filip, C., Vasile, C. M., Herișeanu, C., Marcu, V., Stoica, S., & Cîrstoveanu, C. (2023). Neonatal Brain Abscess with Serratia marcescens after Intrauterine Infection: A Case Report. Antibiotics, 12(4), 722. https://doi.org/10.3390/antibiotics12040722






