Impact of COVID-19 Pandemic in Antibiotic Consumption in Navarre (Spain): An Interrupted Time Series Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Data Sources and Outcomes
2.3. Statistical Analysis
2.4. Ethics Statement
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aslam, B.; Khurshid, M.; Arshad, M.I.; Muzammil, S.; Rasool, M.; Yasmeen, N.; Shah, T.; Chaudhry, T.H.; Rasool, M.H.; Shahid, A.; et al. Antibiotic Resistance: One Health One World Outlook. Front. Cell. Infect. Microbiol. 2021, 11, 771510. [Google Scholar] [CrossRef] [PubMed]
- Join Action Antimicrobial Resistance and Healthcare-Associated Infections. (EU JAMRAI). Available online: https://eu-jamrai.eu/ (accessed on 11 November 2022).
- Ministerio de Sanidad Consumo y Bienestar Social. Plan Nacional Frente a las Resistencias Antibióticos (PRAN). Programas de Optimización de Uso de Antibióticos (PROA). 2017. Available online: https://www.resistenciaantibioticos.es (accessed on 11 November 2022).
- Llor, C. Prudent use of antibiotics and suggestions for improvement in the primary health care system. Enferm. Infecc. Microbiol. Clin. 2010, 28 (Suppl. S4), 17–22. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Urrusuno, R.; Flores-Dorado, M.; Vilches-Arenas, A.; Serrano-Martino, C.; Corral-Baena, S.; Montero-Balosa, M.C. Appropriateness of antibiotic prescribing in a primary care area: A cross-sectional study. Enferm. Infecc. Microbiol. Clin. 2014, 32, 285–292. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- Fernández-Urrusuno, R.; Meseguer-Barros, C.M.; Anaya-Ordóñez, S.; Borrego-Izquierdo, Y.; Lallana-Álvarez, M.J.; Madridejos-Mora, M.; Tejón, E.M.; Sánchez, R.P.; Pérez-Rodríguez, O.; García-Gil, M.; et al. Patients receiving a high burden of antibiotics in the community in Spain: A cross-sectional study. Pharmacol. Res. Perspect. 2021, 9, e00692. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Baño, J.; Pérez-Moreno, M.A.; Peñalva, G.; Garnacho-Montero, J.; Pinto, C.; Salcedo, I.; Fernández-Urrusuno, R.; Neth, O.; Gil-Navarro, M.V.; Pérez-Milena, A.; et al. PIRASOA Programme Group Outcomes of the PIRASOA programme, an antimicrobial stewardship programme implemented in hospitals of the Public Health System of Andalusia, Spain: An ecologic study of time-trend analysis. Clin. Microbiol. Infect. 2020, 26, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Urrusuno, R.; Meseguer-Barros, C.M.; Benavente-Cantalejo, R.S.; Hevia, E.; Serrano-Martino, C.; Irastorza-Aldasoro, A.; Limón-Mora, J.; López-Navas, A.; Pascual-Pisa, B. Successful improvement of antibiotic prescribing at Primary Care in Andalusia following the implementation of an antimicrobial guide through multifaceted interventions: An interrupted time-series analysis. PLoS ONE 2020, 15, e0233062. [Google Scholar] [CrossRef] [PubMed]
- Alzueta-Isturiz, N.; Fontela-Bulnes, C.; Echeverría-Gorriti, A.; Gil-Setas, A.; Aldaz-Herce, P.; Garjón Parra, J. Results of implementation of a pilot antimicrobial stewardship program (ASP) in Primary Care. An. Sist. Sanit. Navar. 2020, 43, 373–379. (In Spanish) [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Novel Coronavirus (2019-nCoV). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 11 November 2022).
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Worldometer. Available online: http://www.worldometers.info/coronavirus/ (accessed on 11 November 2022).
- EMCL COVID. Available online: https://covid-statistics.jrc.ec.europa.eu/RMeasures (accessed on 11 November 2022).
- Rodríguez-Baño, J.; Rossolini, G.M.; Schultsz, C.; Tacconelli, E.; Murthy, S.; Ohmagari, N.; Holmes, A.; Bachmann, T.; Goossens, H.; Canton, R.; et al. Key considerations on the potential impacts of the COVID-19 pandemic on antimicrobial resistance research and surveillance. Trans. R. Soc. Trop. Med. Hyg. 2021, 115, 1122–1129. [Google Scholar] [CrossRef] [PubMed]
- Konstantinoudis, G.; Cameletti, M.; Gómez-Rubio, V.; Gómez, I.L.; Pirani, M.; Baio, G.; Larrauri, A.; Riou, J.; Egger, M.; Vineis, P.; et al. Regional excess mortality during the 2020 COVID-19 pandemic in five European countries. Nat. Commun. 2022, 13, 482. [Google Scholar] [CrossRef] [PubMed]
- Equipo COVID-19. RENAVE. CNE. CNM (ISCIII). Situación de COVID-19 en España a 24 de Mayo de 2022. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Paginas/InformesCOVID-19.aspx (accessed on 7 January 2022).
- Peñalva, G.; Benavente, R.S.; Pérez-Moreno, M.A.; Pérez-Pacheco, M.D.; Pérez-Milena, A.; Murcia, J.; Cisneros, J.M. Effect of the coronavirus disease 2019 pandemic on antibiotic use in primary care. Clin. Microbiol. Infect. 2021, 27, 1058–1060. [Google Scholar] [CrossRef] [PubMed]
- WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index. Available online: https://www.whocc.no/atc_ddd_index_and_guidelines/atc_ddd_index/ (accessed on 11 November 2022).
- Cochrane Effective Practice and Organisation of Care (EPOC). Interrupted Time Series (ITS) Analyses. EPOC Resources for Review Authors. 2017. Available online: http://epoc.cochrane.org/epoc-specific-resources-review-authors (accessed on 16 November 2022).
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad Servicios Sociales e Igualdad. Real Decreto Legislativo 1/2015, de 24 de Julio, por el que se Aprueba el Texto Refundido de la Ley de Garantías y uso Racional de los Medicamentos y Productos Sanitarios. 2015. Available online: https://www.boe.es/eli/es/rdlg/2015/07/24/1 (accessed on 16 November 2022).
- Högberg, L.D.; Vlahović-Palčevski, V.; Pereira, C.; Weist, K.; Monnet, D.L. Decrease in community antibiotic consumption during the COVID-19 pandemic, EU/EEA, 2020. Eurosurveillance 2021, 26, 2101020. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Available online: https://www.ecdc.europa.eu/en/news-events/reported-decrease-antibiotic-consumption-across-eueea-during-covid-19-pandemic#:~:text=The%20latest%20data%20from%20the,of%20the%20COVID%2D19%20pandemic (accessed on 16 November 2022).
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef] [PubMed]
- Gautret, P.; Lagier, J.C.; Parola, P.; Hoang, V.T.; Meddeb, L.; Mailhe, M.; Doudier, B.; Courjon, J.; Giordanengo, V.; Vieira, V.E.; et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: Results of an open-label non-randomized clinical trial. Int. J. Antimicrob. Agents 2020, 56, 105949. [Google Scholar] [CrossRef] [PubMed]
- RECOVERY Collaborative Group. Azithromycin in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2021, 397, 605–612. [Google Scholar] [CrossRef] [PubMed]
- Tsay, S.V.; Bartoces, M.; Gouin, K.; Kabbani, S.; Hicks, L.A. Antibiotic Prescriptions Associated With COVID-19 Outpatient Visits Among Medicare Beneficiaries, April 2020 to April 2021. JAMA 2022, 327, 2018–2019. [Google Scholar] [CrossRef] [PubMed]
- Gagliotti, C.; Buttazzi, R.; Ricchizzi, E.; di Mario, S.; Tedeschi, S.; Moro, M.L. Community use of antibiotics during the COVID-19 lockdown. Infect. Dis. 2021, 53, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad Consumo y Bienestar Social. Plan Nacional Frente a la Resistencia a Los Antibióticos 2019–2021. Mapas de Consumo en Salud Humana. Available online: https://www.resistenciaantibioticos.es/es/lineas-de-accion/vigilancia/mapas-de-consumo/consumo-antibioticos-humana/consumos-antibioticos-en-atencion-primaria (accessed on 12 January 2023).
- Audi, A.; AlIbrahim, M.; Kaddoura, M.; Hijazi, G.; Yassine, H.M.; Zaraket, H. Seasonality of Respiratory Viral Infections: Will COVID-19 Follow Suit? Front. Public Health 2020, 8, 567184. [Google Scholar] [CrossRef] [PubMed]


| 1st Quarter | 2nd Quarter | 3rd Quarter | 4th Quarter | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2018 | 2019 | 2020 | 2021 | 2018 | 2019 | 2020 | 2021 | 2018 | 2019 | 2020 | 2021 | 2018 | 2019 | 2020 | 2021 | p * | |
| Defined daily doses per 1000 inhabitants per day (DID) | |||||||||||||||||
| J01A—Tetracyclines | 1.04 | 1.15 | 1.24 | 1.60 | 0.96 | 1.02 | 0.93 | 1.22 | 0.66 | 0.77 | 0.79 | 0.83 | 0.99 | 1.17 | 1.25 | 1.24 | 0.796 |
| J01C—Betalactams. Penicillins | 11.00 | 10.52 | 10.04 | 4.97 | 8.85 | 9.16 | 4.86 | 5.26 | 7.55 | 7.52 | 5.06 | 5.14 | 9.50 | 9.28 | 5.09 | 7.23 | 0.010 |
| J01D—Other betalactam antibacterials | 2.66 | 2.31 | 2.46 | 1.62 | 1.99 | 1.98 | 1.45 | 1.68 | 1.80 | 1.83 | 1.69 | 1.72 | 2.19 | 2.24 | 1.69 | 2.09 | 0.051 |
| J01E—Sulfonamides and trimethoprim | 0.31 | 0.33 | 0.41 | 0.40 | 0.31 | 0.36 | 0.36 | 0.40 | 0.29 | 0.39 | 0.36 | 0.41 | 0.30 | 0.40 | 0.38 | 0.39 | 0.962 |
| J01F—Macrolides. Lincosamides and streptogramins | 2.74 | 2.19 | 2.22 | 0.98 | 1.92 | 1.72 | 0.94 | 1.03 | 1.62 | 1.38 | 0.82 | 0.87 | 2.09 | 1.92 | 0.95 | 1.50 | 0.011 |
| J01M—Quinolones | 2.99 | 2.12 | 1.66 | 0.92 | 1.95 | 1.60 | 0.89 | 0.89 | 1.78 | 1.29 | 0.92 | 0.91 | 1.79 | 1.41 | 1.00 | 1.20 | 0.011 |
| J01X—Other antibacterials | 0.38 | 0.42 | 0.45 | 0.46 | 0.40 | 0.43 | 0.43 | 0.45 | 0.43 | 0.48 | 0.48 | 0.48 | 0.42 | 0.47 | 0.46 | 0.47 | 0.078 |
| TOTAL | 21.13 | 19.05 | 18.48 | 10.95 | 16.37 | 16.27 | 9.85 | 10.93 | 14.13 | 13.65 | 10.11 | 10.35 | 17.29 | 16.90 | 10.83 | 14.12 | 0.007 |
| Number of patients | |||||||||||||||||
| J01A—Tetracyclines | 1325 | 1436 | 1550 | 1878 | 1364 | 1404 | 1277 | 1680 | 975 | 1075 | 1093 | 1151 | 1284 | 1465 | 1573 | 1516 | 0.643 |
| J01C—Betalactams. Penicillins | 45,217 | 43,171 | 42,977 | 19,741 | 37,023 | 38,970 | 19,170 | 21,891 | 30,881 | 30,950 | 20,373 | 21,317 | 41,118 | 41,063 | 20,391 | 31,333 | 0.008 |
| J01D—Other betalactam antibacterials | 11,008 | 9554 | 10,427 | 6839 | 8350 | 8333 | 6112 | 7185 | 7706 | 7738 | 7333 | 7395 | 9424 | 9581 | 7365 | 9025 | 0.056 |
| J01E—Sulfonamides and trimethoprim | 833 | 941 | 1280 | 1167 | 932 | 1087 | 1100 | 1237 | 890 | 1234 | 1109 | 1275 | 910 | 1298 | 1166 | 1243 | 0.817 |
| J01F—Macrolides. Lincosamides and streptogramins | 23,083 | 17,043 | 17,527 | 5602 | 15,184 | 13,231 | 5843 | 6430 | 13,091 | 10,107 | 5042 | 5402 | 17,593 | 15,518 | 5855 | 12,040 | 0.013 |
| J01M—Quinolones | 16,949 | 11,645 | 9241 | 4707 | 11,010 | 8814 | 4737 | 4667 | 10,090 | 7155 | 4865 | 4804 | 10,289 | 7948 | 5258 | 6641 | 0.010 |
| J01X—Other antibacterials | 7940 | 8773 | 9723 | 9888 | 8413 | 9206 | 9196 | 9693 | 9399 | 10,397 | 10,730 | 10,618 | 9256 | 10,298 | 10,287 | 10,131 | 0.019 |
| TOTAL | 92,186 | 80,882 | 79,952 | 43,256 | 71,561 | 71,035 | 40,809 | 46,108 | 63,529 | 60,179 | 43,869 | 45,160 | 77,921 | 75,839 | 44,964 | 62,580 | 0.007 |
| 1st Quarter | 2nd Quarter | 3rd Quarter | 4th Quarter | p * | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2021 | Variation | 2019 | 2021 | Variation | 2019 | 2021 | Variation | 2019 | 2021 | Variation | |||
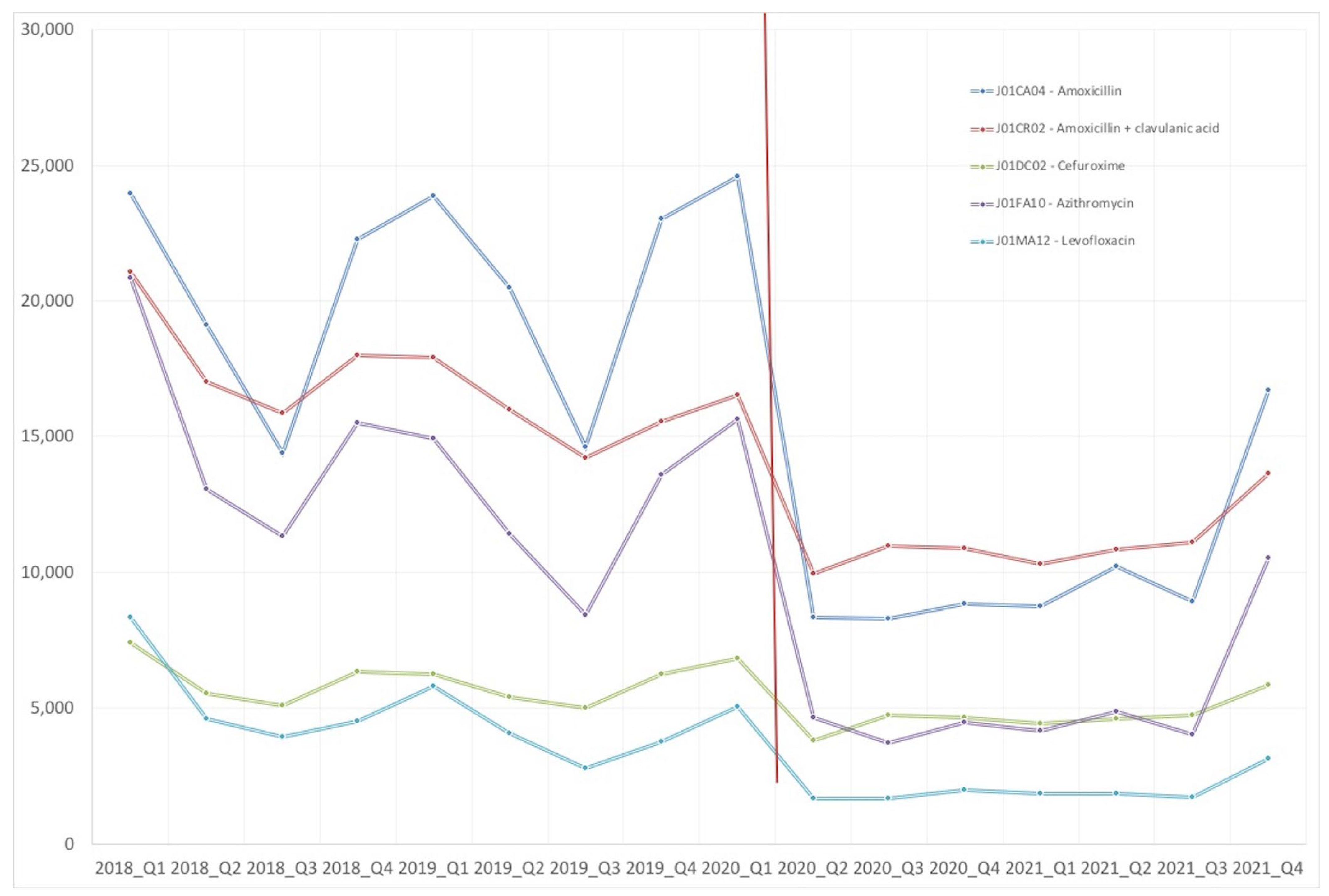
| J01CA04—Amoxicillin | DID | 5.044 | 1.989 | −61% | 4.247 | 2.189 | −48% | 3.220 | 1.947 | −40% | 4.668 | 3.375 | −28% | 0.017 |
| Patients | 23,571 | 8636 | −63% | 20,277 | 10,152 | −50% | 14,637 | 8889 | −39% | 22,833 | 16,544 | −28% | 0.013 | |
| J01CR02—Amoxicillin + clavulanic acid | DID | 4.997 | 2.737 | −45% | 4.377 | 2.826 | −35% | 3.875 | 2.903 | −25% | 4.072 | 3.525 | −13% | 0.003 |
| Patients | 17,761 | 10,264 | −42% | 15,867 | 10,851 | −32% | 14,274 | 11,205 | −22% | 15,520 | 13,678 | −12% | 0.003 | |
| J01DC02—Cefuroxime | DID | 1.556 | 1.117 | −28% | 1.324 | 1.160 | −12% | 1.249 | 1.176 | −6% | 1.522 | 1.434 | −6% | 0.048 |
| Patients | 6093 | 4389 | −28% | 5249 | 4604 | −12% | 4924 | 4732 | −4% | 6111 | 5871 | −4% | 0.042 | |
| J01FA10—Azithromycin | DID | 1.525 | 0.513 | −66% | 1.165 | 0.533 | −54% | 0.894 | 0.474 | −47% | 1.338 | 1.054 | −21% | 0.044 |
| Patients | 14,780 | 4158 | −72% | 11,336 | 4856 | −57% | 8388 | 4041 | −52% | 13,409 | 10,446 | −22% | 0.017 | |
| J01MA12—Levofloxacin | DID | 1.099 | 0.384 | −65% | 0.765 | 0.371 | −52% | 0.550 | 0.367 | −33% | 0.688 | 0.587 | −15% | 0.022 |
| Patients | 5787 | 1864 | −68% | 4068 | 1861 | −54% | 2799 | 1751 | −37% | 3757 | 3130 | −17% | 0.027 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzueta, N.; Echeverría, A.; García, P.; Sanz, L.; Gil-Setas, A.; Beristain, X.; Aldaz, P.; Garjón, J. Impact of COVID-19 Pandemic in Antibiotic Consumption in Navarre (Spain): An Interrupted Time Series Analysis. Antibiotics 2023, 12, 318. https://doi.org/10.3390/antibiotics12020318
Alzueta N, Echeverría A, García P, Sanz L, Gil-Setas A, Beristain X, Aldaz P, Garjón J. Impact of COVID-19 Pandemic in Antibiotic Consumption in Navarre (Spain): An Interrupted Time Series Analysis. Antibiotics. 2023; 12(2):318. https://doi.org/10.3390/antibiotics12020318
Chicago/Turabian StyleAlzueta, Natalia, Amaya Echeverría, Patricia García, Lorea Sanz, Alberto Gil-Setas, Xabier Beristain, Pablo Aldaz, and Javier Garjón. 2023. "Impact of COVID-19 Pandemic in Antibiotic Consumption in Navarre (Spain): An Interrupted Time Series Analysis" Antibiotics 12, no. 2: 318. https://doi.org/10.3390/antibiotics12020318
APA StyleAlzueta, N., Echeverría, A., García, P., Sanz, L., Gil-Setas, A., Beristain, X., Aldaz, P., & Garjón, J. (2023). Impact of COVID-19 Pandemic in Antibiotic Consumption in Navarre (Spain): An Interrupted Time Series Analysis. Antibiotics, 12(2), 318. https://doi.org/10.3390/antibiotics12020318





