Impact of COVID-19 Pandemic on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligibility Criteria
2.2.1. Inclusion Criteria
- Compared the rate of HAIs between the periods before the pandemic and during the pandemic using interrupted time series or before and after study design;
- Published between December 2019 and September 2022;
- Published in English language;
- Available as free full-text article.
2.2.2. Exclusion Criteria
- Described nosocomial transmission of COVID-19 infections;
- Preprints, correspondence, commentary, and letters to the editor;
- Qualitative studies.
2.3. Information Sources
2.4. Search Strategy
2.5. Selection Process
2.6. Data Extraction Process
2.7. Data Items
2.8. Study Risk of Bias Assessment
2.9. Outcome Assessment and Effect Measures
2.10. Data Synthesis
3. Results
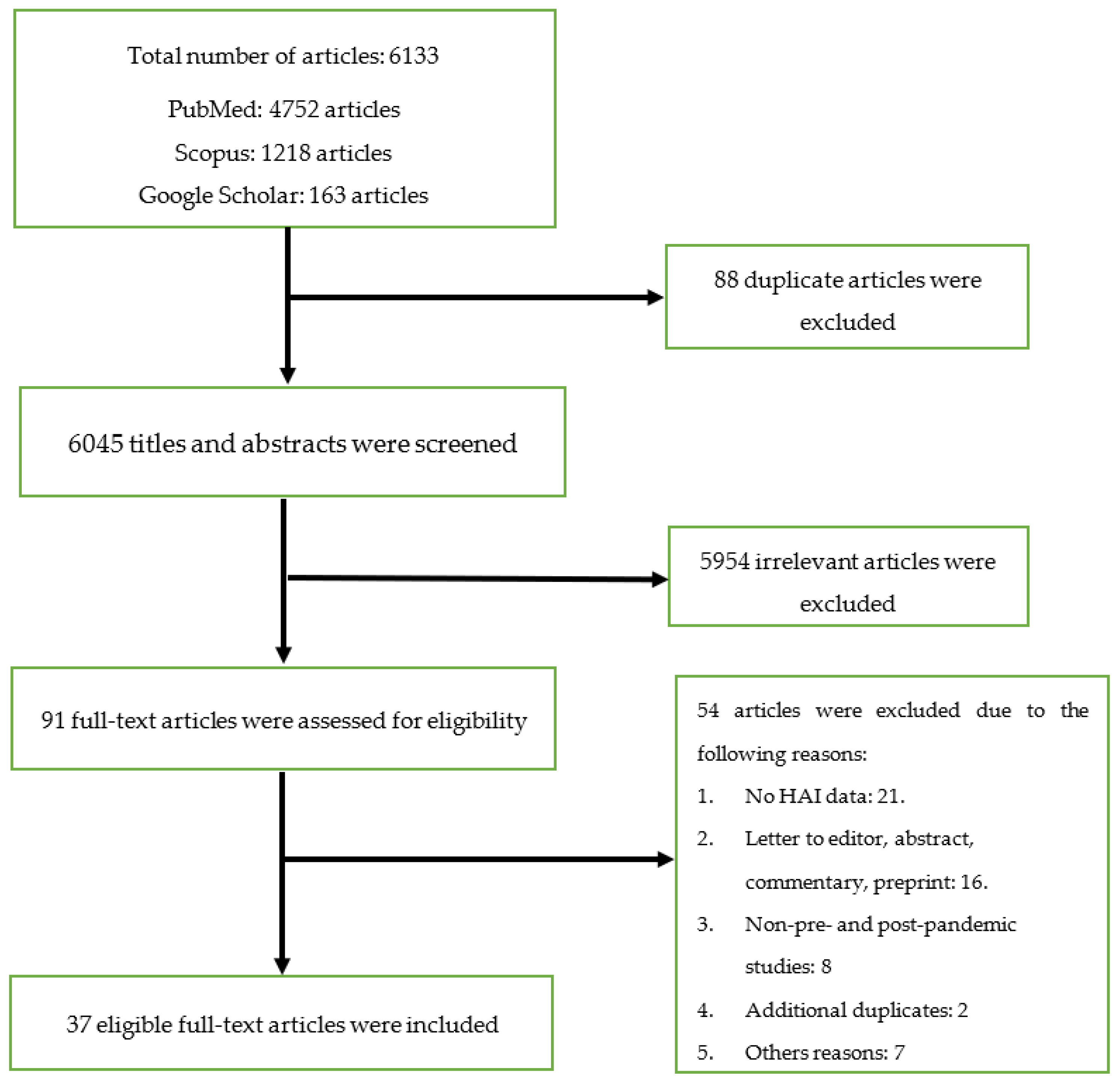
3.1. Study Selection
3.2. Study Characteristics
3.3. Quality Assessment of the Studies
3.4. Qualitative Summary of Results
3.4.1. The Effect of COVID-19 Pandemic on Overall Rate of Healthcare-Associated Infections (HAIs)
3.4.2. The Effect of COVID-19 Pandemic on Central Line-Associated Bloodstream Infections (CLABSIs)
3.4.3. The Effect of COVID-19 Pandemic on Catheter-Associated Urinary Tract Infections (CAUTIs)
3.4.4. The Effect of COVID-19 Pandemic on Healthcare-Associated Clostridium Difficile Infection (CDI)
3.4.5. The Effect of COVID-19 Pandemic on Surgical Site Infections (SSIs)
3.4.6. The Effect of COVID-19 Pandemic on Ventilator-Associated Pneumonia
3.5. Quantitative Summary of Results
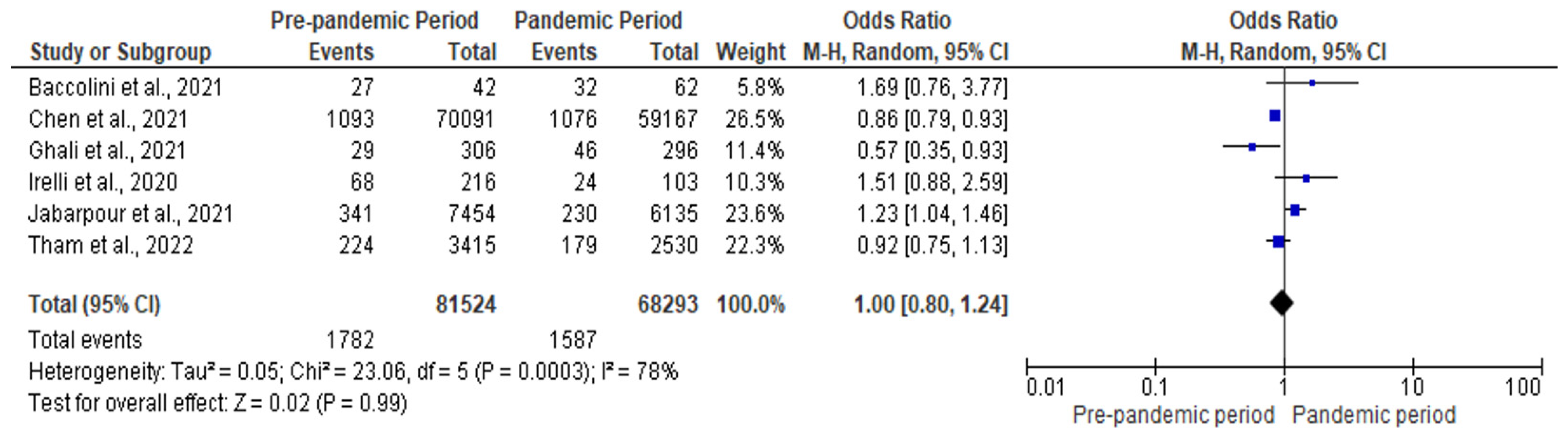
3.5.1. Meta-Analysis for the Effect of COVID-19 Pandemic on Overall HAIs
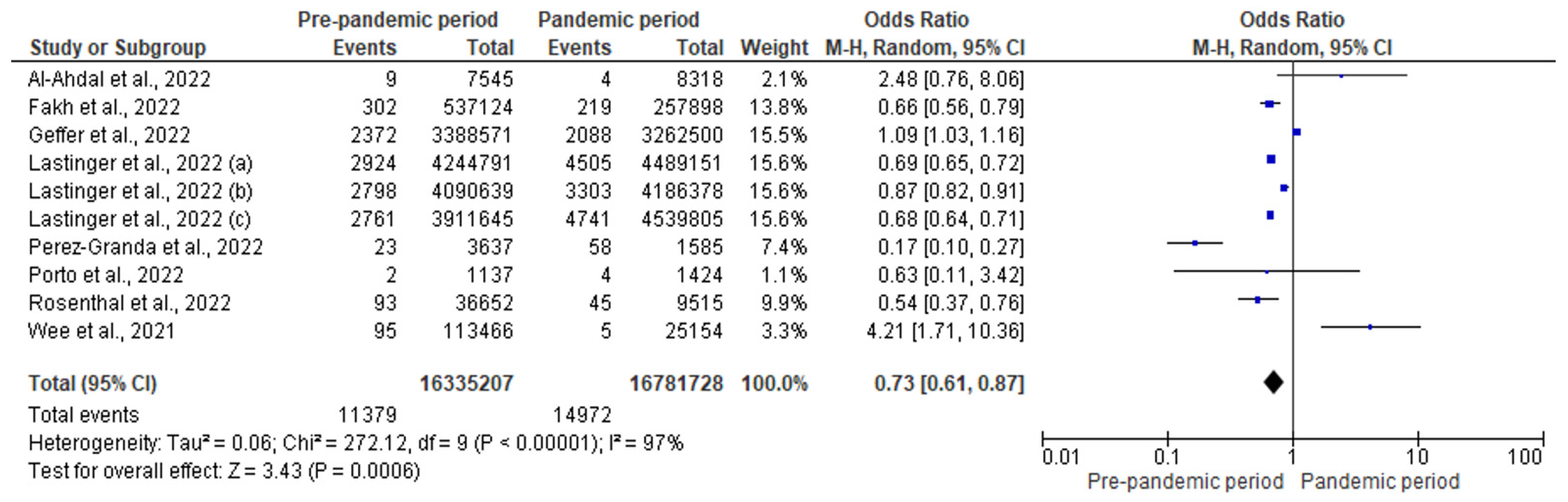
3.5.2. Meta-Analysis for the Effect of COVID-19 Pandemic on CLABSI
3.5.3. Meta-Analysis for the Effect of COVID-19 Pandemic on CDI
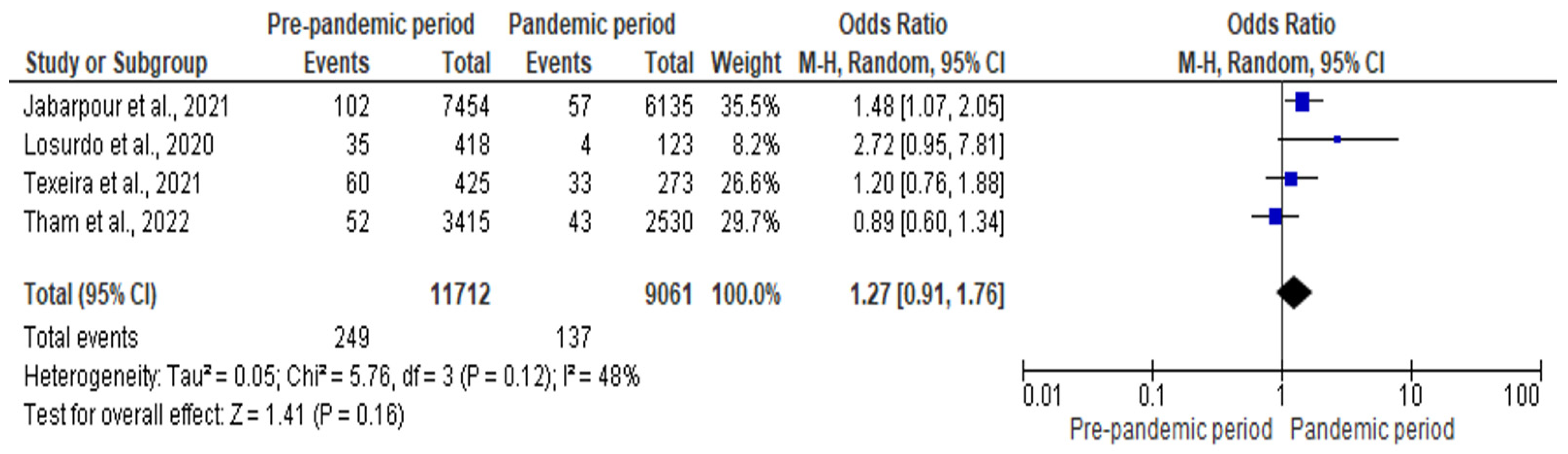
3.5.4. Meta-Analysis for the Effect of COVID-19 Pandemic on CAUTI
3.5.5. Meta-Analysis of the Impact of COVID-19 Pandemic on SSI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Storr, J.; Twyman, A.; Zingg, W.; Damani, N.; Kilpatrick, C.; Reilly, J.; Price, L.; Egger, M.; Grayson, M.L.; Kelley, E.; et al. Core components for effective infection prevention and control programmes: New WHO evidence-based recommendations. Antimicrob. Resist. Infect. Control 2017, 6, 6. [Google Scholar] [CrossRef] [PubMed]
- Magill, S.S.; Edwards, J.R.; Bamberg, W.; Beldavs, Z.G.; Dumyati, G.; Kainer, M.A.; Lynfield, R.; Maloney, M.; McAllister-Hollod, L.; Nadle, J.; et al. Multistate point-prevalence survey of health care–associated infections. N. Engl. J. Med. 2014, 370, 1198–1208. [Google Scholar] [CrossRef] [PubMed]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O.; et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 2018, 23, 1800516. [Google Scholar] [CrossRef] [PubMed]
- Ling, M.L.; Apisarnthanarak, A.; Madriaga, G. The burden of healthcare-associated infections in Southeast Asia: A systematic literature review and meta-analysis. Clin. Infect. Dis. 2015, 60, 1690–1699. [Google Scholar] [CrossRef] [PubMed]
- Allegranzi, B.; Nejad, S.B.; Combescure, C.; Graafmans, W.; Attar, H.; Donaldson, L.; Pittet, D. Burden of endemic health-care-associated infection in developing countries: Systematic review and meta-analysis. Lancet 2011, 377, 228–241. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U.; Amir, O.; Rodríguez-Baño, J. Healthcare-associated infections in Africa: A systematic review and meta-analysis of point prevalence studies. J. Pharm. Policy Pract. 2022, 15, 99. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U. Point-prevalence survey of hospital acquired infections in three acute care hospitals in Northern Nigeria. Antimicrob. Resist. Infect. Control 2020, 9, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Loftus, M.J.; Guitart, C.; Tartari, E.; Stewardson, A.J.; Amer, F.; Bellissimo-Rodrigues, F.; Lee, Y.F.; Mehtar, S.; Sithole, B.L.; Pittet, D. Hand hygiene in low-and middle-income countries. Int. J. Infect. Dis. 2019, 86, 25–30. [Google Scholar] [CrossRef]
- Abubakar, U.; Al-Anazi, M.; Alanazi, Z.; Rodríguez-Baño, J. Impact of COVID-19 pandemic on multidrug resistant gram positive and gram negative pathogens: A systematic review. J. Infect. Public Health 2023, 16, 320–331. [Google Scholar] [CrossRef]
- Ataiyero, Y.; Dyson, J.; Graham, M. Barriers to hand hygiene practices among health care workers in sub-Saharan African countries: A narrative review. Am. J. Infect. Control 2019, 47, 565–573. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, J.; Qiao, F.; Feng, B.; Hu, F.; Xi, Z.A.; Wu, W.; Ni, Z.L.; Liu, L.; Yuan, Y. Compared hand hygiene compliance among healthcare providers before and after the COVID-19 pandemic: A rapid review and meta-analysis. Am. J. Infect. Control 2022, 50, 563–571. [Google Scholar] [CrossRef] [PubMed]
- Stevens, M.P.; Doll, M.; Pryor, R.; Godbout, E.; Cooper, K.; Bearman, G. Impact of COVID-19 on traditional healthcare-associated infection prevention efforts. Infect. Control Hosp. Epidemiol. 2020, 41, 946–947. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Baño, J.; Rossolini, G.M.; Schultsz, C.; Tacconelli, E.; Murthy, S.; Ohmagari, N.; Holmes, A.; Bachmann, T.; Goossens, H.; Canton, R.; et al. Antimicrobial resistance research in a post-pandemic world: Insights on antimicrobial resistance research in the COVID-19 pandemic. J. Glob. Antimicrob. Resist. 2021, 25, 5–7. [Google Scholar] [CrossRef] [PubMed]
- Subramanya, S.H.; Czyż, D.M.; Acharya, K.P.; Humphreys, H. The potential impact of the COVID-19 pandemic on antimicrobial resistance and antibiotic stewardship. Virus Dis. 2021, 32, 330–337. [Google Scholar] [CrossRef] [PubMed]
- McBride, D.L. The impact of visiting restrictions during the COVID-19 pandemic on pediatric patients. J. Pediatr. Nurs. 2021, 61, 436–438. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U.; Usman, M.N.; Baba, M.; Sulaiman, A.; Kolo, M.; Adamu, F.; Jaber, A.A. Practices and perception of healthcare workers towards infection control measures during the COVID-19 pandemic: A cross-sectional online survey from Nigeria. J. Infect. Dev. Ctries. 2022, 16, 1398–1405. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 3 September 2023).
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC definitions for nosocomial infections, 1988. Am. J. Infect. Control 1988, 16, 128–140. [Google Scholar] [CrossRef]
- European Center for Disease Prevention and Control. Point Prevalence Survey of Healthcare Associated Infections and Antimicrobial Use in European Acute Care Hospitals—Protocol Version 5.3; ECDC: Stockholm, Sweden, 2016.
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Baccolini, V.; Migliara, G.; Isonne, C.; Dorelli, B.; Barone, L.C.; Giannini, D.; Marotta, D.; Marte, M.; Mazzalai, E.; Alessandri, F.; et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: A retrospective cohort study. Antimicrob. Resist. Infect. Control 2021, 10, 87. [Google Scholar] [CrossRef]
- Jabarpour, M.; Dehghan, M.; Afsharipour, G.; Hajipour Abaee, E.; Mangolian Shahrbabaki, P.; Ahmadinejad, M.; Maazallahi, M. The impact of COVID-19 outbreak on nosocomial infection rate: A case of Iran. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 6650920. [Google Scholar] [CrossRef] [PubMed]
- Ghali, H.; Ben Cheikh, A.; Bhiri, S.; Khefacha, S.; Latiri, H.S.; Ben Rejeb, M. Trends of Healthcare-associated Infections in a Tuinisian University Hospital and Impact of COVID-19 Pandemic. INQUIRY J. Health Care Organ. Provis. Financ. 2021, 58, 00469580211067930. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhu, P.; Zhang, Y.; Liu, B. Effect of the “Normalized Epidemic Prevention and Control Requirements” on hospital-acquired and community-acquired infections in China. BMC Infect. Dis. 2021, 21, 1178. [Google Scholar] [CrossRef] [PubMed]
- Irelli, E.C.; Orlando, B.; Cocchi, E.; Morano, A.; Fattapposta, F.; Di Piero, V.; Toni, D.; Ciardi, M.R.; Giallonardo, A.T.; Fabbrini, G.; et al. The potential impact of enhanced hygienic measures during the COVID-19 outbreak on hospital-acquired infections: A pragmatic study in neurological units. J. Neurol. Sci. 2020, 418, 117111. [Google Scholar] [CrossRef] [PubMed]
- Tham, N.; Fazio, T.; Johnson, D.; Skandarajah, A.; Hayes, I.P. Hospital Acquired Infections in Surgical Patients: Impact of COVID-19-Related Infection Prevention Measures. World J. Surg. 2022, 46, 1249–1258. [Google Scholar] [CrossRef]
- Alsuhaibani, M.; Kobayashi, T.; McPherson, C.; Holley, S.; Marra, A.R.; Trannel, A.; Dains, A.; Abosi, O.J.; Jenn, K.E.; Meacham, H.; et al. Impact of COVID-19 on an infection prevention and control program, Iowa 2020–2021. Am. J. Infect. Control 2022, 50, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Granda, M.J.; Carrillo, C.S.; Rabadán, P.M.; Valerio, M.; Olmedo, M.; Muñoz, P.; Bouza, E. Increase in the frequency of catheter-related bloodstream infections during the COVID-19 pandemic: A plea for Control. J. Hosp. Infect. 2022, 119, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Conceicao, E.P.; Tan, J.Y.; Magesparan, K.D.; Amin, I.B.; Ismail, B.B.; Toh, H.X.; Jin, P.; Zhang, J.; Wee, E.G.; et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am. J. Infect. Control 2021, 49, 469–477. [Google Scholar] [CrossRef]
- Halverson, T.; Mikolajczak, A.; Mora, N.; Silkaitis, C.; Stout, S. Impact of COVID-19 on hospital acquired infections. Am. J. Infect. Control 2022, 50, 831–833. [Google Scholar] [CrossRef]
- Advani, S.D.; Sickbert-Bennett, E.; Moehring, R.; Cromer, A.; Lokhnygina, Y.; Dodds-Ashley, E.; Kalu, I.C.; DiBiase, L.; Weber, D.J.; Anderson, D.J.; et al. The Disproportionate Impact of COVID-19 Pandemic on Healthcare-Associated Infections in Community Hospitals: Need for Expanding the Infectious Disease Workforce. Clin. Infect. Dis. 2022, 76, e34–e41. [Google Scholar] [CrossRef]
- Fakih, M.G.; Bufalino, A.; Sturm, L.; Huang, R.H.; Ottenbacher, A.; Saake, K.; Winegar, A.; Fogel, R.; Cacchione, J. Coronavirus disease 2019 (COVID-19) pandemic, central-line–associated bloodstream infection (CLABSI), and catheter-associated urinary tract infection (CAUTI): The urgent need to refocus on hardwiring prevention efforts. Infect. Control Hosp. Epidemiol. 2022, 43, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Bobbitt, L.J.; Satyanarayana, G.; Baum, L.V.; Nebhan, C.A.; Kassim, A.A.; Gatwood, K.S. Evaluation of healthcare-associated infection rates in patients with hematologic malignancies and stem cell transplantation during the coronavirus disease 2019 (COVID-19) pandemic. Antimicrob. Steward. Healthc. Epidemiol. 2022, 2, e11. [Google Scholar] [CrossRef] [PubMed]
- Geffers, C.; Schwab, F.; Behnke, M.; Gastmeier, P. No increase of device associated infections in German intensive care units during the start of the COVID-19 pandemic in 2020. Antimicrob. Resist. Infect. Control 2022, 11, 67. [Google Scholar] [CrossRef] [PubMed]
- Kong, A.; Botero Suarez, C.S.; Rahamatalli, B.; Shankweiler, J.; Karasik, O. Hand Hygiene and Hospital-Acquired Infections During COVID-19 Increased Vigilance: One Hospital’s Experience. HCA Healthc. J. Med. 2021, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Porto, A.P.; Borges, I.C.; Buss, L.; Machado, A.; Bassetti, B.R.; Cocentino, B.; Bicalho, C.S.; Carrilho, C.M.; Rodrigues, C.; Neto, E.A.; et al. Healthcare-associated infections on the intensive care unit in 21 Brazilian hospitals during the early months of the coronavirus disease 2019 (COVID-19) pandemic: An ecological study. Infect. Control Hosp. Epidemiol. 2022, 44, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.R.; Weiner-Lastinger, L.M.; Dudeck, M.A.; Fike, L.V.; Kuhar, D.T.; Edwards, J.R.; Pollock, D.; Benin, A. Impact of COVID-19 pandemic on central-line–associated bloodstream infections during the early months of 2020, National Healthcare Safety Network. Infect. Control Hosp. Epidemiol. 2022, 43, 790–793. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, V.D.; Myatra, S.N.; Divatia, J.V.; Biswas, S.; Shrivastava, A.; Al-Ruzzieh, M.A.; Ayaad, O.; Bat-Erdene, A.; Bat-Erdene, I.; Narankhuu, B.; et al. The impact of COVID-19 on health care–associated infections in intensive care units in low-and middle-income countries: International Nosocomial Infection Control Consortium (INICC) findings. Int. J. Infect. Dis. 2022, 118, 83–88. [Google Scholar] [CrossRef]
- Lastinger, L.M.; Alvarez, C.R.; Kofman, A.; Konnor, R.Y.; Kuhar, D.T.; Nkwata, A.; Patel, P.R.; Pattabiraman, V.; Xu, S.Y.; Dudeck, M.A. Continued Increases in HAI Incidence During the Second Year of the COVID-19 Pandemic. Infect. Control Hosp. Epidemiol. 2023, 44, 997–1001. [Google Scholar] [CrossRef]
- Samaroo-Campbell, J.; Qiu, W.; Asrat, H.; Abdallah, M.; Fornek, M.; Episcopia, B.; Quale, J. The initial and lingering impact of coronavirus disease 2019 (COVID-19) on catheter-associated infections in a large healthcare system in New York City. Antimicrob. Steward. Healthc. Epidemiol. 2022, 2, e77. [Google Scholar] [CrossRef]
- AlAhdal, A.M.; Alsada, S.A.; Alrashed, H.A.; Al Bazroun, L.I.; Alshoaibi, A. Impact of the COVID-19 Pandemic on Levels of Device-Associated Infections and Hand Hygiene Compliance. Cureus 2022, 14, e24254. [Google Scholar] [CrossRef]
- Ochoa-Hein, E.; González-Lara, M.F.; Huertas-Jiménez, M.A.; Chávez-Ríos, A.R.; de-Paz-García, R.; Haro-Osnaya, A.; González-González, R.; Cruz-Juárez, B.S.; Hernández-Gilsoul, T.; Rivero-Sigarroa, E.; et al. Surge in Ventilator-Associated Pneumonias and Bloodstream Infections in An Academic Referral Center Converted to Treat COVID-19 Patients. Rev. Investig. Clínica 2021, 73, 210–215. [Google Scholar] [CrossRef] [PubMed]
- Whitaker, A.; Colgrove, G.; Scheutzow, M.; Ramic, M.; Monaco, K.; Hill, J.L., Jr. Decreasing Catheter-Associated Urinary Tract Infection (CAUTI) at a community academic medical center using a multidisciplinary team employing a multi-pronged approach during the COVID-19 pandemic. Am. J. Infect. Control 2023, 51, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Alessio, G.; Spuntarelli, V.; Luciani, M.; Santino, I.; Simmaco, M.; Martelletti, P. Impact of COVID-19 prevention measures on risk of health care-associated Clostridium difficile infection. Am. J. Infect. Control 2021, 49, 640–642. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.B.; Du, T.; Silva, A.; Golding, G.R.; Pelude, L.; Mitchell, R.; Rudnick, W.; Hizon, R.; Al-Rawahi, G.N.; Chow, B.; et al. Trends in Clostridioides difficile infection rates in Canadian hospitals during the coronavirus disease 2019 (COVID-19) pandemic. Infect. Control Hosp. Epidemiol. 2022, 44, 1180–1183. [Google Scholar] [CrossRef] [PubMed]
- Ochoa-Hein, E.; Rajme-López, S.; Rodríguez-Aldama, J.C.; Huertas-Jiménez, M.A.; Chávez-Ríos, A.R.; de Paz-García, R.; Haro-Osnaya, A.; González-Colín, K.K.; González-González, R.; González-Lara, M.F.; et al. Substantial reduction of healthcare facility-onset Clostridioides difficile infection (HO-CDI) rates after conversion of a hospital for exclusive treatment of COVID-19 patients. Am. J. Infect. Control 2021, 49, 966–968. [Google Scholar] [CrossRef] [PubMed]
- Manea, E.; Jipa, R.; Milea, A.; Roman, A.; Neagu, G.; Hristea, A. Healthcare-associated infection during the COVID-19 pandemic in a tertiary care hospital in Romania. Rom. J. Intern. Med. 2021, 59, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Ponce-Alonso, M.; De La Fuente, J.S.; Rincón-Carlavilla, A.; Moreno-Nunez, P.; Martínez-García, L.; Escudero-Sánchez, R.; Pintor, R.; García-Fernández, S.; Cobo, J. Impact of the coronavirus disease 2019 (COVID-19) pandemic on nosocomial Clostridioides difficile infection. Infect. Control Hosp. Epidemiol. 2021, 42, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Sipos, S.; Vlad, C.; Prejbeanu, R.; Haragus, H.; Vlad, D.; Cristian, H.; Dumitrascu, C.; Popescu, R.; Dumitrascu, V.; Predescu, V. Impact of COVID-19 prevention measures on Clostridioides difficile infections in a regional acute care hospital. Exp. Ther. Med. 2021, 22, 1215. [Google Scholar] [CrossRef]
- Sturm, L.K.; Saake, K.; Roberts, P.B.; Masoudi, F.A.; Fakih, M.G. Impact of COVID-19 pandemic on hospital onset bloodstream infections (HOBSI) at a large health system. Am. J. Infect. Control 2022, 50, 245–249. [Google Scholar] [CrossRef]
- Polly, M.; de Almeida, B.L.; Lennon, R.P.; Cortês, M.F.; Costa, S.F.; Guimarães, T. Impact of the COVID-19 pandemic on the incidence of multidrug-resistant bacterial infections in an acute care hospital in Brazil. Am. J. Infect. Control 2022, 50, 32–38. [Google Scholar] [CrossRef]
- Kitt, E.; Brennan, L.; Harrison, C.; Hei, H.; Paul, E.; Satchell, L.; Wilson, K.B.; Smathers, S.; Handy, L.; Coffin, S.E. Dodging the bundle—Persistent healthcare-associated rhinovirus infection throughout the pandemic. Am. J. Infect. Control 2022, 50, 1140–1144. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, B.L.; Cabral, J.; Marques-Pinto, A.; Vila, F.; Lindoro, J.; Fraga, A. How the COVID-19 pandemic changed postoperative infections in urology wards: A retrospective cohort study from two urology departments. Can. Urol. Assoc. J. 2022, 16, E267. [Google Scholar] [CrossRef] [PubMed]
- Mohammadi, A.; Khatami, F.; Azimbeik, Z.; Khajavi, A.; Aloosh, M.; Aghamir, S.M. Hospital-acquired infections in a tertiary hospital in Iran before and during the COVID-19 pandemic. Wien. Med. Wochenschr. 2022, 172, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Losurdo, P.; Paiano, L.; Samardzic, N.; Germani, P.; Bernardi, L.; Borelli, M.; Pozzetto, B.; de Manzini, N.; Bortul, M. Impact of lockdown for SARS-CoV-2 (COVID-19) on surgical site infection rates: A monocentric observational cohort study. Updates Surg. 2020, 72, 1263–1271. [Google Scholar] [CrossRef] [PubMed]
- Ereth, M.H.; Fine, J.; Stamatatos, F.; Mathew, B.; Hess, D.; Simpser, E. Healthcare-associated infection impact with bioaerosol treatment and COVID-19 mitigation measures. J. Hosp. Infect. 2021, 116, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Martínez, A.; Fernández-Cruz, A.; Domínguez, F.; Forteza, A.; Cobo, M.; Sánchez-Romero, I.; Asensio, A. Hospital-acquired infective endocarditis during Covid-19 pandemic. Infect. Prev. Pract. 2020, 2, 100080. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U.; Tangiisuran, B.; Elnaem, M.H.; Sulaiman, S.A.; Khan, F.U. Mortality and its predictors among hospitalized patients with infections due to extended spectrum beta-lactamase (ESBL) Enterobacteriaceae in Malaysia: A retrospective observational study. Future J. Pharm. Sci. 2022, 8, 17. [Google Scholar] [CrossRef]
- Abubakar, U.; Zulkarnain, A.I.; Rodríguez-Baño, J.; Kamarudin, N.; Elrggal, M.E.; Elnaem, M.H.; Harun, S.N. Treatments and Predictors of Mortality for Carbapenem-Resistant Gram-Negative Bacilli Infections in Malaysia: A Retrospective Cohort Study. Trop. Med. Infect. Dis. 2022, 7, 415. [Google Scholar] [CrossRef]
- Elliott, T.M.; Hurst, C.; Doidge, M.; Hurst, T.; Harris, P.N.; Gordon, L.G. Unexpected benefit of COVID-19 hospital restrictions: Reduction in patients isolating with multidrug resistant organisms after restrictions were lifted. Infect. Dis. Health 2022, 27, 10–14. [Google Scholar] [CrossRef]
- Ippolito, M.; Simone, B.; Filisina, C.; Catalanotto, F.R.; Catalisano, G.; Marino, C.; Misseri, G.; Giarratano, A.; Cortegiani, A. Bloodstream infections in hospitalized patients with COVID-19: A systematic review and meta-analysis. Microorganisms 2021, 9, 2016. [Google Scholar] [CrossRef]
- Giacobbe, D.R.; Battaglini, D.; Ball, L.; Brunetti, I.; Bruzzone, B.; Codda, G.; Crea, F.; De Maria, A.; Dentone, C.; Di Biagio, A.; et al. Bloodstream infections in critically ill patients with COVID-19. Eur. J. Clin. Investig. 2020, 50, e13319. [Google Scholar] [CrossRef]
- Balla, K.C.; Rao, S.P.; Arul, C.; Shashidhar, A.; Prashantha, Y.N.; Nagaraj, S.; Suresh, G. Decreasing central line-associated bloodstream infections through quality improvement initiative. Indian Pediatr. 2018, 55, 753–756. [Google Scholar] [CrossRef] [PubMed]
- Eze, P.; Balsells, E.; Kyaw, M.H.; Nair, H. Risk factors for Clostridium difficile infections–an overview of the evidence base and challenges in data synthesis. J. Glob. Health 2017, 7, 010417. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, J.D.; Akram, A.R.; Singanayagam, A.; Wilcox, M.H.; Hill, A.T. Risk factors for Clostridium difficile infection in hospitalized patients with community-acquired pneumonia. J. Infect. 2016, 73, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Loo, V.G.; Bourgault, A.M.; Poirier, L.; Lamothe, F.; Michaud, S.; Turgeon, N.; Toye, B.; Beaudoin, A.; Frost, E.H.; Gilca, R.; et al. Host and pathogen factors for Clostridium difficile infection and colonization. N. Engl. J. Med. 2011, 365, 1693–1703. [Google Scholar] [CrossRef] [PubMed]
- Dieringer, T.D.; Furukawa, D.; Graber, C.J.; Stevens, V.W.; Jones, M.M.; Rubin, M.A.; Goetz, M.B. Inpatient antibiotic utilization in the Veterans’ Health Administration during the coronavirus disease 2019 (COVID-19) pandemic. Infect. Control Hosp. Epidemiol. 2021, 42, 751–753. [Google Scholar] [CrossRef] [PubMed]
- Elligsen, M.; Wan, M.; Lam, P.W.; Lo, J.; Taggart, L.R.; Chan, A.J.; Downing, M.; Gough, K.; Seah, J.; Leung, E. Trends in hospital antibiotic utilization during the coronavirus disease 2019 (COVID-19) pandemic: A multicenter interrupted time-series analysis. Antimicrob. Steward. Healthc. Epidemiol. 2022, 2, e128. [Google Scholar] [CrossRef] [PubMed]
- Castro-Lopes, A.; Correia, S.; Leal, C.; Resende, I.; Soares, P.; Azevedo, A.; Paiva, J.A. Increase of antimicrobial consumption in a tertiary care hospital during the first phase of the COVID-19 pandemic. Antibiotics 2021, 10, 778. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Westwood, D.; MacFadden, D.R.; Soucy, J.P.; Daneman, N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020, 26, 1622–1629. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Soucy, J.P.; Westwood, D.; Daneman, N.; MacFadden, D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 520–531. [Google Scholar] [CrossRef]
- Patton, A.; Davey, P.; Harbarth, S.; Nathwani, D.; Sneddon, J.; Marwick, C.A. Impact of antimicrobial stewardship interventions on Clostridium difficile infection and clinical outcomes: Segmented regression analyses. J. Antimicrob. Chemother. 2018, 73, 517–526. [Google Scholar] [CrossRef] [PubMed]
- Ananthakrishnan, A.N. Clostridium difficile infection: Epidemiology, risk factors and management. Nat. Rev. Gastroenterol. Hepatol. 2011, 8, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U. Antibiotic use among hospitalized patients in northern Nigeria: A multicenter point-prevalence survey. BMC Infect. Dis. 2020, 20, 86. [Google Scholar] [CrossRef]
- Abubakar, U.; Syed Sulaiman, S.A.; Adesiyun, A.G. Utilization of surgical antibiotic prophylaxis for obstetrics and gynaecology surgeries in Northern Nigeria. Int. J. Clin. Pharm. 2018, 40, 1037–1043. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, U.; Syed Sulaiman, S.A.; Adesiyun, A.G. Impact of pharmacist-led antibiotic stewardship interventions on compliance with surgical antibiotic prophylaxis in obstetric and gynecologic surgeries in Nigeria. PLoS ONE 2019, 14, e0213395. [Google Scholar] [CrossRef] [PubMed]
- Mukai, S.; Nomi, M.; Kozawa, S.; Yanagiuchi, A.; Shigemura, K.; Sengoku, A. The impact of the coronavirus disease 2019 pandemic on changes in antimicrobial prophylaxis and development of genito-urinary tract infections after urodynamic study: A retrospective comparative study of a single rehabilitation hospital in Japan. Neurourol. Urodyn. 2022, 41, 1440–1450. [Google Scholar] [CrossRef]
- AlGamdi, S.S.; Alawi, M.; Bokhari, R.; Bajunaid, K.; Mukhtar, A.; Baeesa, S.S. Risk factors for surgical site infection following spinal surgery in Saudi Arabia: A retrospective case–control study. Medicine 2021, 100, e25567. [Google Scholar] [CrossRef]
- Patel, S.; Thompson, D.; Innocent, S.; Narbad, V.; Selway, R.; Barkas, K. Risk factors for surgical site infections in neurosurgery. Ann. R. Coll. Surg. Engl. 2019, 101, 220–225. [Google Scholar] [CrossRef]
- Xue, D.Q.; Qian, C.; Yang, L.; Wang, X.F. Risk factors for surgical site infections after breast surgery: A systematic review and meta-analysis. Eur. J. Surg. Oncol. (EJSO) 2012, 38, 375–381. [Google Scholar] [CrossRef]
- Jain, R.K.; Shukla, R.; Singh, P.; Kumar, R. Epidemiology and risk factors for surgical site infections in patients requiring orthopedic surgery. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 251–254. [Google Scholar] [CrossRef]
| S/No. | Author and Year | Country and Continent | Study Setting/No of Centers | Study Design | Period of the Study | Number of Participants | Types of HAIs Included | Prevalence/Incidence of HAIs before Pandemic | Prevalence/Incidence of HAIs during Pandemic | p Value |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Irelli et al., 2020 [26] | Italy/Europe | Neurology and stroke unit/single center | Retrospective case–control study | 8 March 2020 to 31 May 2020 versus same period in 2019 | 216 (2019) 103 (2020) | Overall HAI | 31.5% | 23.3% | 0.120 |
| 2 | Alsuhaibani et al., 2022 [28] | USA/North America | Hospital-wide/single center | NA | 2018–2019 versus January–December 2020 | NA | CLABSI | 0.7–1.4 per 1000 central line days | 1.8 per 1000 central line days | 0.04 |
| CAUTI | 0.8–1.7 per 1000 catheter days | 0.6–1.6 per 1000 catheter days | 0.54 | |||||||
| CDI | 0.6–1.0 per 10,000 patient days | 0.4–0.6 per 10,000 patient days | 0.11 | |||||||
| 3 | Sturm et al., 2022 [51] | USA/North America | Hospital-wide/multicenter (69 hospitals) | Before and after | Pre-COVID-19 (1 January 2019 to 28 February 2020), and COVID-19 pandemic period (1 March 2020 to 30 April 2021). | NA | Bloodstream infection | 2.78 per 10,000 patient days | 3.56 per 10,000 patient days | <0.001 |
| 4 | Perez-Granda et al., 2022 [29] | Spain/Europe | Hospital-wide/single center | Retrospective before and during the COVID-19 pandemic | March to May 2019 March to May 2020 | 12,111 versus 10,479 patients. | Catheter-related BSI | 1.89 per 1000 admission | 5.53 per 1000 admission | <0.001 |
| 5 | Wee et al., 2021 [30] | Singapore/Asia | Hospital-wide/multicenter | Retrospective before and after | January 2018–January 2020 versus February–August 2020 | NA | RVI | 9.69 per 10,000 patient days | 0.83 per 10,000 patient days | <0.05 |
| CLABSI | 0.83 per 1000 device days | 0.20 per 1000 device days | <0.05 | |||||||
| CAUTI | 1.8 per 1000 device days | 1.8 per 1000 device days | NA | |||||||
| CDI | 3.65 per 10,000 patient days | 3.47 per 10,000 patient days | 0.66 | |||||||
| 6 | Ochoa-Hein et al., 2021 [47] | Mexico/South America | Hospital-wide/single center | Before–after observational study | January 2019–February 2020 versus April–July 2020 | NA | CDI | 9.3 per 10,000 patient days | 1.4 per 10,000 patient days | NA |
| 7 | Polly et al., 2022 [52] | Brazil/South America | Hospital-wide/single center | Retrospective before–after observational study | 2017–2019 versus 2020 | NA | HCAIs due to MDR bacteria | 3.14 per 1000 patient days | 3.89 per 1000 patient days | <0.005 |
| 8 | Halverson et al., 2022 [31] | USA/North America | Hospital-wide/multicenter | Retrospective cohort study | September 2017 to December 2020 | NA | CLABSI | 0.13 per 1000 patient days | 0.24 | 0.0082 |
| CAUTI | 0.13 per 1000 patient days | 0.17 | 0.052 | |||||||
| CDI | 0.52 per 1000 patient days | 0.55 | 0.670 | |||||||
| Overall HAIs | 0.80 per 1000 patient days | 1.06 | 0.017 | |||||||
| 9 | Kitt et al., 2022 [53] | USA/North America | Hospital-wide/single center | Retrospective cohort study | July 2017–June 2021 | NA | HAVI | 0.19 per 1000 patient days | 0.06 per 1000 patient days | <0.01 |
| 10 | Advan et al., 2022 [32] | USA/North America | Hospital-wide/multicenter | Retrospective longitudinal | January 2018–February 2020 versus March 2020–March 2021 | NA | CLABSI | 0.6 per 1000 catheter days | 0.9 | 0.0023 |
| CAUTI | 0.7 per 1000 catheter days | 0.7 | 0.810 | |||||||
| CDI | 3.6 per 10,000 patient days | 2.6 | <0.001 | |||||||
| 11 | Fakih et al., 2022 [33] | USA/North America | Hospital-wide/multicenter | Retrospective | March 2019–February 2020 versus March–August 2020 | NA | CLABSI | 0.56 per 1000 line days | 0.85 | <0.001 |
| CAUTI | 0.86 per 1000 catheter days | 0.77 | 0.190 | |||||||
| 12 | Teixeira et al., 2022 [54] | Portugal/Europe | Urology ward/multicenter | Retrospective observational | April–June 2018 versus April–June 2020 | 425 patients versus 273 patients | SSI | 14.1% | 12.1% | 0.494 |
| 13 | Ponce-Alonso et al., 2021 [49] | Spain/Europe | Hospital-wide/single center | Retrospective | Mar–May 2019 versus March–May 2020 | 39,795 hospital stay (pre) versus 44,831 (pandemic era) hospital stays | CDI | 8.54 per 10,000 patient days | 2.68 per 10,000 patient days | 0.0002 |
| 14 | Bobbitt et al., 2022 [34] | USA/North America | Hematology and stem cell transplant patients/single center | Retrospective observational | March–July 2019 versus March–July 2020 | 295 patients versus 259 patients | CDI | 2.61 per 1000 patient days | 1.58 | 0.512 |
| CLABSI | 0.44 per 1000 patient days | 1.064 | 0.516 | |||||||
| CAUTI | 0.44 per 1000 patient days | 0.53 | 0.899 | |||||||
| 15 | Kong et al., 2021 [36] | USA/North America | Hospital-wide/single center | Retrospective observational | January 2019–February 2020 versus March 2020–June 2020 | NA | CDI | 0.48 ± 0.12 | 0.26 ± 0.25 | 0.200 |
| CLABSI | 1.47 ± 1.63 | 0.37 ± 0.73 | 0.210 | |||||||
| CAUTI | 1.10 ± 1.18 | 0.87 ± 0.58 | 0.720 | |||||||
| 16 | Tham et al., 2022 [27] | Australia | Hospital-wide/single center | Retrospective cohort study | April–June 2019 versus April–June 2020 | 3415 admission (pre-COVID-19) versus 2530 (COVID-19 era) | Overall HAIs | 6.6% | 7.1% | NA |
| UTI | 1.3% | 1.6% | NA | |||||||
| SSI | 1.5% | 1.7% | NA | |||||||
| HAP | 2.5% | 2.3% | NA | |||||||
| BSI | 0.4% | 0.4% | NA | |||||||
| GI | 0.4% | 0.2% | NA | |||||||
| 17 | Mohammadi et al., 2022 [55] | Iran/Asia | Hospital-wide/single center | Retrospective study | April–November 2019 versus April–December 2020 | 16,687 admission (pre pandemic) versus 10,553 admission (pandemic era) | Overall HAIs | 4.73% | 4.78% | NA |
| 18 | Chen et al., 2021 [25] | China/Asia | Hospital-wide/single center | Retrospective before and after | 2018–2019 versus 2020 | 62,625 patients (2018) 70,091 (2019) 59,167 (2020) | Overall HAIs | 1.64% (2018) 1.56% (2019) | 1.82% | 0.001 |
| LRI | 39.5% | 39.7% | 0.971 | |||||||
| UTI | 14.8% | 10.5% | 0.002 | |||||||
| BSI | 11.28% | 12.91% | 0.079 | |||||||
| SSI | 11.83% | 14.84% | 0.084 | |||||||
| GTI | 7.49% | 9.62% | 0.068 | |||||||
| 19 | Losurdo et al., 2020 [56] | Italy/Europe | Surgery department/single center | Retrospective | 2018–2019 versus 2020 | 418 patients (pre-COVID era) versus 123 (COVID-19 era) | SSI | 8.4% | 3.3% | 0.035 |
| Superficial SSI | 5.3% | 0.8% | 0.018 | |||||||
| Deep SSI | 3.4% | 0.0% | 0.025 | |||||||
| Organ-space SSI | 3.6% | 1.6% | 0.209 | |||||||
| 20 | Geffer et al., 2022 [35] | Germany/Europe | ICU/multicenter | NA | 2019 versus 2020 | 863,999 patients (2019) and 696,085 patients (2020) | CLABSI | 0.7 per 1000 central line days | 0.64 | 0.263 |
| VALRTI | 2.95 per ventilator days | 2.02 | <0.001 | |||||||
| CAUTI | 0.61 per 1000 catheter days | 0.49 | 0.008 | |||||||
| 21 | Porto et al., 2022 [37] | Brazil /South America | ICU/multicenter | NA | April–June 2019 versus April–June 2020 | 531 (2019) versus 357 (2020) | CLABSI | 1.60 per 1000 central line days | 2.81 | 0.002 |
| VAP | 2.99 per 1000 ventilator days | 3.65 | 0.167 | |||||||
| 22 | Samaroo-Campbell et al., 2022 [41] | USA/North America | Hospital-wide/multicenter | Retrospective | 15 months before and 15 months after the onset of the pandemic | NA | CLABSI | 1.09 ± 0.43 per 1000 catheter days | 1.76 | NA |
| CAUTI | 1.03 ± 0.18 per 1000-catheter days | 1.80 ± 0.21 | 0.0003 | |||||||
| 23 | Ochoa-Hein et al., 2021 [43] | Mexico/South America | Hospital-wide/single center | Before–after observational study | January 2019–February 2020 versus Apr–Jul 2020 | NA | Overall HAIs | 6.2 per 1000 patient days | 11.8 | 0.023 |
| VAP | 10% | 54.7% | <0.001 | |||||||
| HAP | 26.9% | 18.2% | 0.025 | |||||||
| BSI | 1.3% | 20.6% | <0.001 | |||||||
| CAUTI | 8.3% | 3.5% | 0.039 | |||||||
| SSI | 25.2% | 0.0% | NA | |||||||
| CDI | 15.2% | 1.8% | <0.001 | |||||||
| Candidemia | 0.0% | 8.2% | <0.001 | |||||||
| 24 | Ghali et al., 2021 [24] | Tunisia/Africa | Hospital-wide/single center | Repeated point-prevalence | 2019 versus 2020 | 306 patients versus 296 patients | Overall HAIs | 9.5% | 15.5% | 0.01 |
| 25 | AlAhdal et al., 2022 [42] | Saudi Arabia/Asia | Hospital-wide/single center | Retrospective observational | January–December 2019 versus January–December 2020 | NA | CLABSI | 1.2 per 1000 device days | 0.5 | NA |
| CAUTI | 0.94 per 1000 device days | 0.5 | NA | |||||||
| VAP | 1.3 per 1000 device days | 0.9 | NA | |||||||
| 26 | Ereth et al., 2021 [57] | USA/North America | Hospital-wide/single center | NA | March–December 2019 versus March–December 2020 | NA | NA | 6.71 per 1000 patient days | 1.03 per 1000 patient days | NA |
| 27 | Bentivegna et al., 2021 [45] | Italy/Europe | Medical ward/single center | Retrospective study | 2017–2019 versus March–June 2020 | NA | CDI | 0.066 | 0.037 | NA |
| 28 | Choi et al., 2022 [46] | Canada/North America | Hospital-wide/multicenter | Interrupted time series analysis | January 2015–Febr 2020 versus March 2020–June 2021 | 8,475,872 patient days versus 8,694,620 patient days | CDI | 3.4 | 3.5 | 0.0896 |
| 29 | Rosenthal et al., 2022 [39] | Multinational study/Asia and Europe | ICU/multicenter | Pre and post | January–December 2019 versus January–May 2020 | 7775 patients (pre) versus 1778 patients (pandemic) | CLABSI | 2.54 per 1000 line days | 4.73 per 1000 line days | 0.0006 |
| CAUTI | 1.64 per 1000 catheter days | 1.43 per 1000 catheter days | 0.690 | |||||||
| 30 | Manea et al., 2021 [48] | Romania/Europe | Hospital-wide/single center | Retrospective cohort | March 2017–February 2018 versus 2020–2021 | NA | CDI | 6.1 per 1000 adult discharge | 5.6 per 1000 discharge | 0.600 |
| 31 | Jabarpour et al., 2021 [23] | Iran/Asia | Hospital-wide/single center | Cross-sectional design | March–July 2019 versus March–July 2020 | 7454 patients (pre) versus 6135 patients (pandemic era) | Overall HAIs | 4.6% | 3.7% | 0.020 |
| UTI | 0.8% | 0.5% | 0.040 | |||||||
| BSI | 0.8% | 0.9% | 0.460 | |||||||
| SSI | 1.4% | 0.9% | 0.020 | |||||||
| 32 | Baccolini et al., 2021 [22] | Italy/Europe | ICU/single center | NA | March–April 2019 versus March–April 2020 | 42 patients (pre) and 62 patients (pandemic era) | Overall HAIs | 26.2% | 43.6% | NA |
| 33 | Whitaker et al., 2022 [44] | USA/North America | Hospital-wide/single center | NA | 2019 versus 2020 | NA | CAUTI | 0.37 per 1000 catheter days | 0.23 | NA |
| 34 | Ramos-Matinez et al., 2020 [58] | Spain/Europe | Hospital-wide/single center | NA | 2015–2019 versus March–April 2020 | NA | HAI endocarditis | 0.119 per 1000 days | 0.0194 per 1000 days | <0.001 |
| 35 | Sipos et al., 2021 [50] | Romania/Europe | Hospital-wide/single center | Retrospective | March–November 2018 & 2019 versus March–November 2020 | 43,126 patients (pre) versus 25,124 (pandemic era) | CDI | 151/43126 (0.36%) | 65/25124 (0.26%) | 0.0484 |
| 80.8 per 100,000 bed days | 70.5 per 100,000 bed days | |||||||||
| 36 | Lastinger et al., 2022 [40] | USA/North America | Hospital-wide/single center | NA | First, second and third quarters 2019 versus 1st–3rd quarter 2021 | 1st quarter | CLABSI | 0.687 | 0.998 | <0.05 |
| CAUTI | 0.748 | 0.834 | <0.05 | |||||||
| VAE | 0.948 | 1.431 | <0.05 | |||||||
| SSI colon surgery | 0.866 | 0.820 | >0.05 | |||||||
| SSI abdominal hysterectomy | 0.926 | 0.976 | >0.05 | |||||||
| Lab ID CDI | 0.628 | 0.530 | <0.05 | |||||||
| 2nd quarter | CLABSI | 0.697 | 0.778 | <0.05 | ||||||
| CAUTI | 0.709 | 0.706 | >0.05 | |||||||
| VAE | 0.957 | 1.209 | <0.05 | |||||||
| SSI colon surgery | 0.870 | 0.848 | >0.05 | |||||||
| SSI abdominal hysterectomy | 0.980 | 0.988 | >0.05 | |||||||
| Lab ID CDI | 0.582 | 0.500 | <0.05 | |||||||
| 3rd quarter | CLABSI | 0.699 | 1.037 | <0.05 | ||||||
| CAUTI | 0.705 | 0.801 | <0.05 | |||||||
| VAE | 0.999 | 1.600 | <0.05 | |||||||
| SSI colon surgery | 0.877 | 0.796 | <0.05 | |||||||
| SSI abdominal hysterectomy | 1.087 | 1.042 | >0.05 | |||||||
| Lab ID CDI | 0.564 | 0.482 | <0.05 | |||||||
| 37 | Patel et al., 2022 [38] | USA/North America | Hospital-wide/single center | NA | 2nd quarter 2019 versus 2nd quarter 2020 | NA | CLABSI | 0.68 | 0.87 | <0.05 |
| S/No | Author Name and Year | Selection | Comparability | Outcomes | Quality Score | Quality Scale | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representatives of Sample | Sample Size | Non-Respondents | Ascertainment of Exposure | Based on Design and Analysis | Assessment of Outcomes | Statistical Test | ||||
| 1. | Irelli et al., 2020 [26] | * | * | NA | * | * | ** | * | 7 | Good |
| 2. | Alsuhaibani et al., 2022 [28] | * | * | NA | * | * | ** | * | 7 | Good |
| 3. | Sturm et al., 2022 [51] | * | * | NA | * | * | ** | * | 7 | Good |
| 4. | Perez-Granda et al., 2022 [29] | * | * | NA | * | * | ** | * | 7 | Good |
| 5. | Wee et al., 2021 [30] | * | * | NA | * | * | ** | * | 7 | Good |
| 6. | Ochoa-Hein et al., 2021 [47] | * | * | NA | * | * | * | * | 6 | Fair |
| 7. | Polly et al., 2022 [52] | * | * | NA | * | * | ** | * | 7 | Good |
| 8. | Halverson et al., 2022 [31] | * | * | NA | * | * | ** | * | 7 | Good |
| 9. | Kitt et al., 2022 [53] | * | * | NA | * | * | ** | * | 7 | Good |
| 10. | Advani et al., 2022 [32] | * | * | NA | * | * | ** | * | 7 | Good |
| 11. | Fakih et al., 2022 [33] | * | * | NA | * | * | ** | * | 7 | Good |
| 12. | Teixeira et al., 2022 [54] | * | * | NA | * | * | ** | * | 7 | Good |
| 13. | Ponce-Alonso et al., 2021 [49] | * | * | NA | * | * | ** | * | 7 | Good |
| 14. | Bobbitt et al., 2022 [34] | * | * | NA | * | * | ** | * | 7 | Good |
| 15. | Kong et al., 2021 [36] | * | * | NA | * | * | ** | * | 7 | Good |
| 16. | Tham et al., 2022 [27] | * | * | NA | * | * | ** | * | 7 | Good |
| 17. | Mohammadi et al., 2022 [55] | * | * | NA | * | * | ** | * | 7 | Good |
| 18. | Chen et al., 2021 [25] | * | * | NA | * | * | ** | * | 7 | Good |
| 19. | Losurdo et al., 2020 [56] | * | * | NA | * | * | ** | * | 7 | Good |
| 20. | Geffer et al., 2022 [35] | * | * | NA | * | * | ** | * | 7 | Good |
| 21. | Porto et al., 2022 [37] | * | * | NA | * | * | ** | * | 7 | Good |
| 22. | Samaroo-Campbell et al., 2022 [41] | * | * | NA | * | * | ** | * | 7 | Good |
| 23. | Ochoa-Hein et al., 2021 [43] | * | * | NA | * | * | ** | * | 7 | Good |
| 24. | Ghali et al., 2021 [24] | * | * | NA | * | * | ** | * | 7 | Good |
| 25. | AlAhdal et al., 2022 [42] | * | * | NA | * | * | ** | * | 7 | Good |
| 26. | Ereth et al., 2021 [57] | * | * | NA | * | * | ** | * | 7 | Good |
| 27. | Bentivegna et al., 2021 [45] | * | * | NA | * | * | ** | * | 7 | Good |
| 28. | Choi et al., 2022 [46] | * | * | NA | * | * | * | * | 6 | Fair |
| 29. | Rosenthal et al., 2022 [39] | * | * | NA | * | * | ** | * | 7 | Good |
| 30. | Manea et al., 2021 [48] | * | * | NA | * | * | * | * | 6 | Fair |
| 31. | Jabarpour et al., 2021 [23] | * | * | NA | * | * | ** | * | 7 | Good |
| 32. | Baccolini et al., 2021 [22] | * | * | NA | * | * | ** | * | 7 | Good |
| 33. | Whitaker et al., 2022 [44] | * | * | NA | * | * | ** | * | 7 | Good |
| 34. | Ramos-Matinez et al., 2020 [58] | * | * | NA | * | * | * | * | 6 | Fair |
| 35. | Sipos et al., 2021 [50] | * | * | NA | * | * | ** | * | 7 | Good |
| 36. | Lastinger et al., 2022 [40] | * | * | NA | * | * | ** | * | 7 | Good |
| 37. | Patel et al., 2022 [38] | * | * | NA | * | * | ** | * | 7 | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abubakar, U.; Awaisu, A.; Khan, A.H.; Alam, K. Impact of COVID-19 Pandemic on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. Antibiotics 2023, 12, 1600. https://doi.org/10.3390/antibiotics12111600
Abubakar U, Awaisu A, Khan AH, Alam K. Impact of COVID-19 Pandemic on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. Antibiotics. 2023; 12(11):1600. https://doi.org/10.3390/antibiotics12111600
Chicago/Turabian StyleAbubakar, Usman, Ahmed Awaisu, Amer Hayat Khan, and Khurshid Alam. 2023. "Impact of COVID-19 Pandemic on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis" Antibiotics 12, no. 11: 1600. https://doi.org/10.3390/antibiotics12111600
APA StyleAbubakar, U., Awaisu, A., Khan, A. H., & Alam, K. (2023). Impact of COVID-19 Pandemic on Healthcare-Associated Infections: A Systematic Review and Meta-Analysis. Antibiotics, 12(11), 1600. https://doi.org/10.3390/antibiotics12111600