In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae
Abstract
1. Introduction
2. Results
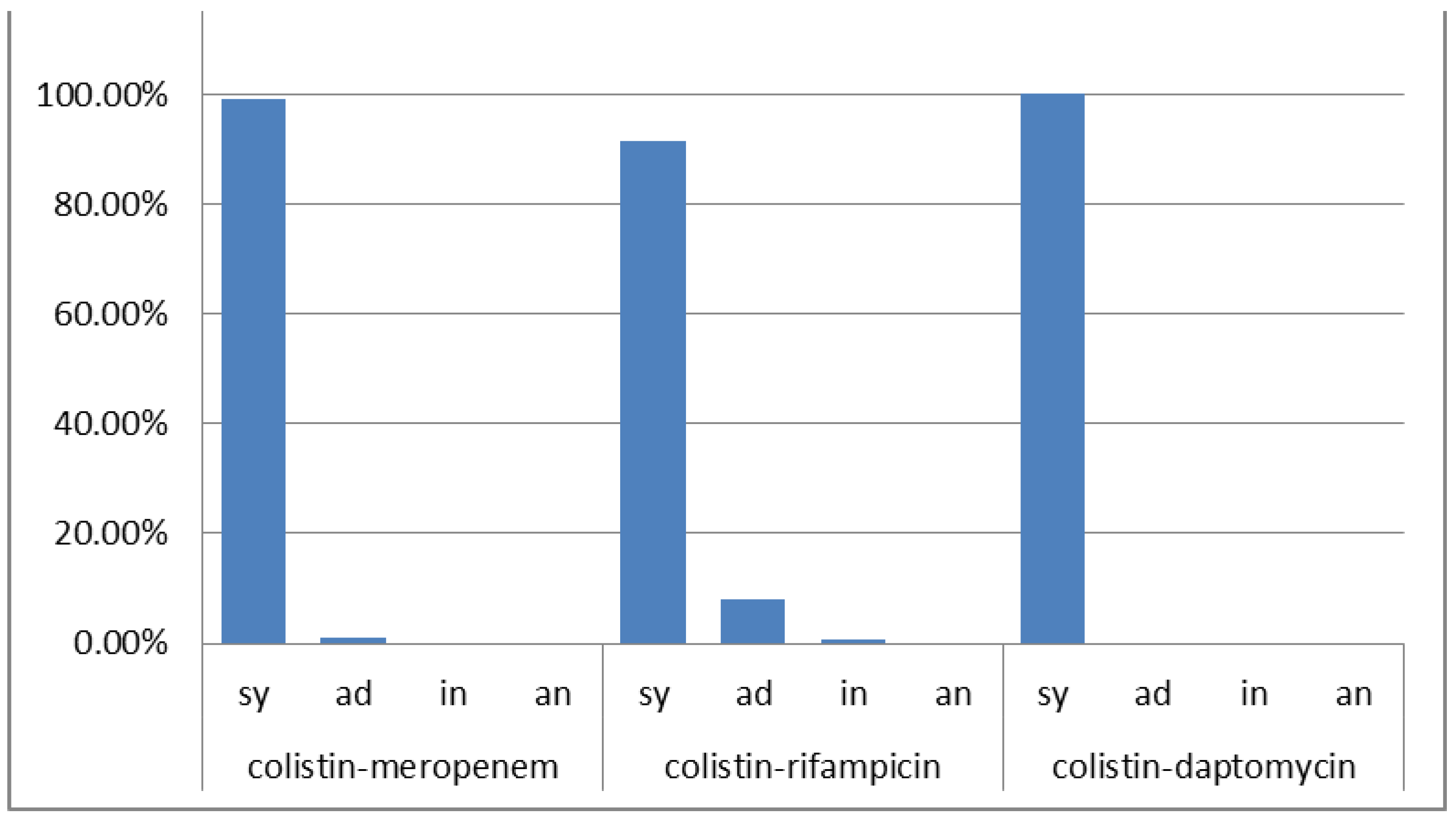
2.1. Acinetobacter baumannii
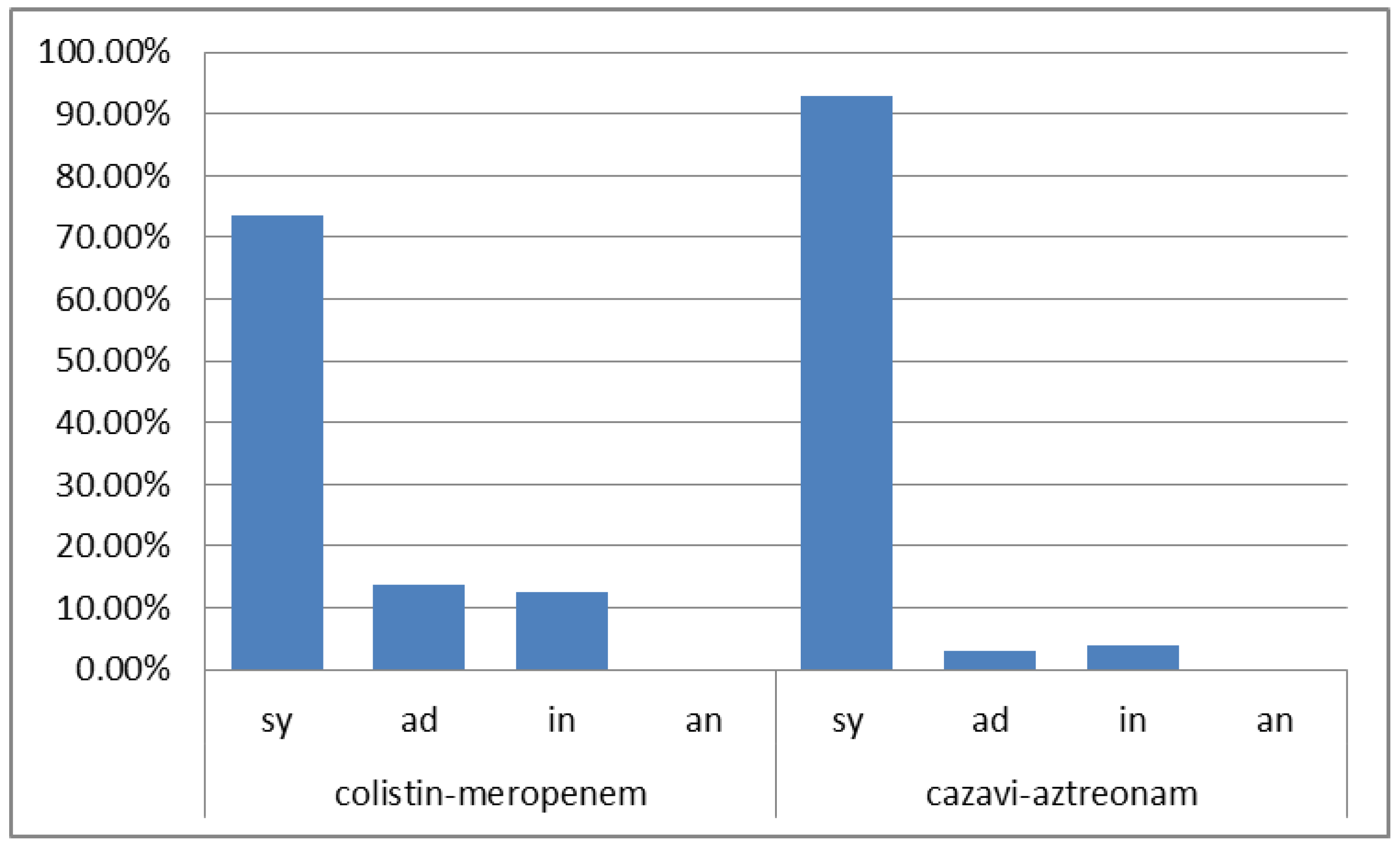
2.2. Klebsiella pneumoniae
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. MIC Test Strip Fixed-Ratio Method
4.3. Phenotypic Detection of K. pneumoniae Carbapenem Resistance Mechanisms
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vardakas, K.Z.; Rafailidis, P.I.; Konstantelias, A.A.; Falagas, M.E. Predictors of mortality in patients with infections due to multi-drug resistant Gram negative bacteria: The study, the patient, the bug or the drug? J. Infect. 2013, 66, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Lemos, E.V.; de la Hoz, F.P.; Alvis, N.; Einarson, T.R.; Quevedo, E.; Castañeda, C.; Leon, Y.; Amado, C.; Cañon, O.; Kawai, K. Impact of carbapenem resistance on clinical and economic outcomes among patients with Acinetobacter baumannii infection in Colombia. Clin. Microbiol. Infect. 2014, 20, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Meletis, G. Carbapenem resistance: Overview of the problem and future perspectives. Ther. Adv. Infect. Dis. 2016, 3, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- Seifert, H.; Blondeau, J.; Lucaßen, K.; Utt, E.A. Global update on the in vitro activity of tigecycline and comparators against isolates of Acinetobacter baumannii and rates of resistant phenotypes (2016–2018). J. Glob. Antimicrob. Resist. 2022, 31, 82–89. [Google Scholar] [CrossRef]
- Meletis, G.; Protonotariou, E.; Gkeka, I.; Kassomenaki, A.; Mantzana, P.; Tychala, A.; Vlachodimou, N.; Kourti, A.; Skoura, L. In vitro activity of eravacycline and cefoperazone/sulbactam against extensively-drug resistant and pan-drug resistant Acinetobacter baumannii isolates from a tertiary hospital in Greece. New Microbiol. 2022, 45, 210–212. [Google Scholar]
- Smoke, S.M.; Brophy, A.; Reveron, S.; Iovleva, A.; Kline, E.G.; Marano, M.; Miller, L.P.; Shields, R.K. Evolution and transmission of cefiderocol-resistant Acinetobacter baumannii during an outbreak in the burn intensive care unit. Clin. Infect. Dis. 2022, ciac647. [Google Scholar] [CrossRef]
- Zhen, S.; Wang, H.; Feng, S. Update of clinical application in ceftazidime-avibactam for multidrug-resistant Gram-negative bacteria infections. Infection 2022, 50, 1409–1423. [Google Scholar] [CrossRef]
- Xiong, L.; Wang, X.; Wang, Y.; Yu, W.; Zhou, Y.; Chi, X.; Xiao, T.; Xiao, Y. Molecular mechanisms underlying bacterial resistance to ceftazidime/avibactam. WIREs Mech. Dis. 2022, 14, e1571. [Google Scholar] [CrossRef]
- Jiang, M.; Sun, B.; Huang, Y.; Liu, C.; Wang, Y.; Ren, Y.; Zhang, Y.; Wang, Y.; Mu, D. Diversity of ceftazidime-avibactam resistance mechanism in KPC2-producing Klebsiella pneumoniae under antimicrobial selection pressure. Infect. Drug Resist. 2022, 15, 4627–4636. [Google Scholar] [CrossRef]
- Williams, P.C. Potential of fosfomycin in treating multidrug-resistant infections in children. J. Paediatr. Child Health 2020, 56, 864–872. [Google Scholar] [CrossRef] [PubMed]
- Jafari, F.; Elyasi, S. Prevention of colistin induced nephrotoxicity: A review of preclinical and clinical data. Expert Rev. Clin. Pharmacol. 2021, 14, 1113–1131. [Google Scholar] [CrossRef] [PubMed]
- Ríos, E.; Del Carmen López Diaz, M.; Culebras, E.; Rodríguez-Avial, I.; Rodríguez-Avial, C. Resistance to fosfomycin is increasing and is significantly associated with extended-spectrum β-lactamase-production in urinary isolates of Escherichia coli. Med. Microbiol. Immunol. 2022, 211, 269–272. [Google Scholar] [CrossRef]
- Meletis, G.; Skoura, L. Polymyxin resistance mechanisms: From intrinsic resistance to mcr genes. Recent Pat. Antiinfect. Drug Discov. 2018, 13, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Bergen, P.J.; Smith, N.M.; Bedard, T.B.; Bulman, Z.P.; Cha, R.; Tsuji, B.T. Rational combinations of polymyxins with other antibiotics. Adv. Exp. Med. Biol. 2019, 1145, 251–288. [Google Scholar] [PubMed]
- Papst, L.; Beović, B.; Pulcini, C.; Durante-Mangoni, E.; Rodríguez-Baño, J.; Kaye, K.S.; Daikos, G.L.; Raka, L.; Paul, M.; ESGAP, ESGBIS, ESGIE and the CRGNB treatment survey study group. Antibiotic treatment of infections caused by carbapenem-resistant Gram-negative bacilli: An international ESCMID cross-sectional survey among infectious diseases specialists practicing in large hospitals. Clin. Microbiol. Infect. 2018, 24, 1070–1076. [Google Scholar] [CrossRef]
- Vardakas, K.Z.; Athanassaki, F.; Pitiriga, V.; Falagas, M.E. Clinical relevance of in vitro synergistic activity of antibiotics for multidrug-resistant Gram-negative infections: A systematic review. J. Glob. Antimicrob. Resist. 2019, 17, 250–259. [Google Scholar] [CrossRef]
- Mancuso, G.; Midiri, A.; Gerace, E.; Biondo, C. Bacterial antimicrobial resistance: The most critical pathogens. Pathogens 2021, 10, 1310. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef]
- Piperaki, E.T.; Tzouvelekis, L.S.; Miriagou, V.; Daikos, G.L. Carbapenem-resistant Acinetobacter baumannii: In pursuit of an effective treatment. Clin. Microbiol. Infect. 2019, 25, 951–957. [Google Scholar] [CrossRef]
- Meletis, G.; Tzampaz, E.; Sianou, E.; Tzavaras, I.; Sofianou, D. Colistin heteroresistance in carbapenemase-producing Klebsiella pneumoniae. J. Antimicrob. Chemotherap. 2011, 66, 946–947. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed Ahmed, M.A.E.; Zhong, L.L.; Shen, C.; Yang, Y.; Doi, Y.; Tian, G.B. Colistin and its role in the Era of antibiotic resistance: An extended review (2000–2019). Emerg. Microbes Infect. 2020, 9, 868–885. [Google Scholar] [CrossRef] [PubMed]
- Karakonstantis, S.; Kritsotakis, E.I.; Gikas, A. Pandrug-resistant Gram-negative bacteria: A systematic review of current epidemiology, prognosis and treatment options. J. Antimicrob. Chemother. 2020, 75, 271–282. [Google Scholar] [CrossRef]
- Karakonstantis, S.; Saridakis, I. Colistin heteroresistance in Acinetobacter spp.: Systematic review and meta-analysis of the prevalence and discussion of the mechanisms and potential therapeutic implications. Int. J. Antimicrob. Agents 2020, 56, 106065. [Google Scholar] [CrossRef] [PubMed]
- Pormohammad, A.; Mehdinejadiani, K.; Gholizadeh, P.; Nasiri, M.J.; Mohtavinejad, N.; Dadashi, M.; Karimaei, S.; Safari, H.; Azimi, T. Global prevalence of colistin resistance in clinical isolates of Acinetobacter baumannii: A systematic review and meta-analysis. Microb. Pathog. 2020, 139, 103887. [Google Scholar] [CrossRef] [PubMed]
- Nowak, J.; Zander, E.; Stefanik, D.; Higgins, P.G.; Roca, I.; Vila, J.; McConnell, M.J.; Cisneros, J.M.; Seifert, H.; MagicBullet Working Group WP4. High incidence of pandrug-resistant Acinetobacter baumannii isolates collected from patients with ventilator-associated pneumonia in Greece, Italy and Spain as part of the MagicBullet clinical trial. J. Antimicrob. Chemother. 2017, 72, 3277–3282. [Google Scholar] [CrossRef]
- Uzairue, L.I.; Rabaan, A.A.; Adewumi, F.A.; Okolie, O.J.; Folorunso, J.B.; Bakhrebah, M.A.; Garout, M.; Alfouzan, W.A.; Halwani, M.A.; Alamri, A.A.; et al. Global prevalence of colistin resistance in Klebsiella pneumoniae from bloodstream infection: A systematic review and meta-analysis. Pathogens 2022, 11, 1092. [Google Scholar] [CrossRef]
- March, G.A.; Bratos, M.A. A meta-analysis of in vitro antibiotic synergy against Acinetobacter baumannii. J. Microbiol. Methods 2015, 119, 31–36. [Google Scholar] [CrossRef]
- Isenberg. Synergism Testing: Broth Microdilution Checkerboard and Broth Macrodilution Methods. In Clinical Microbiology Procedures Handbook, 4th ed.; Wiley: Hoboken, NJ, USA, 2016; Volume 1–3, pp. 5.16.1–5.16.23. [Google Scholar]
- Lenhard, J.R.; Nation, R.L.; Tsuji, B.T. Synergistic combinations of polymyxins. Int. J. Antimicrob. Agents 2016, 48, 607–613. [Google Scholar] [CrossRef]
- Cheng, A.; Chuang, Y.C.; Sun, H.Y.; Sheng, W.H.; Yang, C.J.; Liao, C.H.; Hsueh, P.R.; Yang, J.L.; Shen, N.J.; Wang, J.T.; et al. Excess mortality associated with colistin-tigecycline compared with colistin-carbapenem combination therapy for extensively drug-resistant Acinetobacter baumannii bacteremia: A multicenter prospective observational study. Crit. Care Med. 2015, 43, 1194–1204. [Google Scholar] [CrossRef]
- Kengkla, K.; Kongpakwattana, K.; Saokaew, S.; Apisarnthanarak, A.; Chaiyakunapruk, N. Comparative efficacy and safety of treatment options for MDR and XDR Acinetobacter baumannii infections: A systematic review and network meta-analysis. J. Antimicrob. Chemother. 2018, 73, 22–32. [Google Scholar] [CrossRef] [PubMed]
- Scudeller, L.; Righi, E.; Chiamenti, M.; Bragantini, D.; Menchinelli, G.; Cattaneo, P.; Giske, C.G.; Lodise, T.; Sanguinetti, M.; Piddock, L.J.V.; et al. Systematic review and meta-analysis of in vitro efficacy of antibiotic combination therapy against carbapenem-resistant Gram-negative bacilli. Int. J. Antimicrob. Agents 2021, 57, 106344. [Google Scholar] [CrossRef] [PubMed]
- Ni, W.; Shao, X.; Di, X.; Cui, J.; Wang, R.; Liu, Y. In vitro synergy of polymyxins with other antibiotics for Acinetobacter baumannii: A systematic review and meta-analysis. Int. J. Antimicrob. Agents 2015, 45, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; He, X.; Li, J. Synergy effect of meropenem-based combinations against Acinetobacter baumannii: A systematic review and meta-analysis. Infect. Drug Resist. 2018, 11, 1083–1095. [Google Scholar] [CrossRef]
- Zusman, O.; Avni, T.; Leibovici, L.; Adler, A.; Friberg, L.; Stergiopoulou, T.; Carmeli, Y.; Paul, M. Systematic review and meta-analysis of in vitro synergy of polymyxins and carbapenems. Antimicrob. Agents Chemother. 2013, 57, 5104–5111. [Google Scholar] [CrossRef] [PubMed]
- Laishram, S.; Pragasam, A.K.; Bakthavatchalam, Y.D.; Veeraraghavan, B. An update on technical, interpretative and clinical relevance of antimicrobial synergy testing methodologies. Indian J. Med. Microbiol. 2017, 35, 445–468. [Google Scholar] [CrossRef]
- Abdul-Mutakabbir, J.C.; Yim, J.; Nguyen, L.; Maassen, P.T.; Stamper, K.; Shiekh, Z.; Kebriaei, R.; Shields, R.K.; Castanheira, M.; Kaye, K.S.; et al. In vitro synergy of colistin in combination with meropenem or tigecycline against carbapenem-resistant Acinetobacter baumannii. Antibiotics 2021, 10, 880. [Google Scholar] [CrossRef]
- Hong, D.J.; Kim, J.O.; Lee, H.; Yoon, E.J.; Jeong, S.H.; Yong, D.; Lee, K. In vitro antimicrobial synergy of colistin with rifampicin and carbapenems against colistin-resistant Acinetobacter baumannii clinical isolates. Diagn. Microbiol. Infect. Dis. 2016, 86, 184–189. [Google Scholar] [CrossRef]
- Durante-Mangoni, E.; Signoriello, G.; Andini, R.; Mattei, A.; De Cristoforo, M.; Murino, P.; Bassetti, M.; Malacarne, P.; Petrosillo, N.; Galdieri, N.; et al. Colistin and rifampicin compared with colistin alone for the treatment of serious infections due to extensively drug-resistant Acinetobacter baumannii: A multicenter, randomized clinical trial. Clin. Infect. Dis. 2013, 57, 349–358. [Google Scholar] [CrossRef]
- Aydemir, H.; Akduman, D.; Piskin, N.; Comert, F.; Horuz, E.; Terzi, A.; Kokturk, F.; Ornek, T.; Celebi, G. Colistin vs. the combination of colistin and rifampicin for the treatment of carbapenem-resistant Acinetobacter baumannii ventilator-associated pneumonia. Epidemiol. Infect. 2013, 141, 1214–11222. [Google Scholar] [CrossRef]
- Park, G.C.; Choi, J.A.; Jang, S.J.; Jeong, S.H.; Kim, C.M.; Choi, I.S.; Kang, S.H.; Park, G.; Moon, D.S. In vitro interactions of antibiotic combinations of colistin, tigecycline, and doripenem against extensively drug-resistant and multidrug-resistant Acinetobacter baumannii. Ann. Lab. Med. 2016, 36, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Yang, X.; Chen, L.; Duan, X.; Jiang, Z. In vitro activity of various antibiotics in combination with tigecycline against Acinetobacter baumannii: A systematic review and meta-analysis. Microb. Drug Resist. 2017, 23, 982–993. [Google Scholar] [CrossRef] [PubMed]
- Galani, I.; Orlandou, K.; Moraitou, H.; Petrikkos, G.; Souli, M. Colistin/daptomycin: An unconventional antimicrobial combination synergistic in vitro against multidrug-resistant Acinetobacter baumannii. Int. J. Antimicrob. Agents 2014, 43, 370–374. [Google Scholar] [CrossRef]
- Córdoba, J.; Coronado-Álvarez, N.M.; Parra, D.; Parra-Ruiz, J. In vitro activities of novel antimicrobial combinations against extensively drug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2015, 59, 7316–7319. [Google Scholar] [CrossRef]
- Körber-Irrgang, B.; Kresken, M. In vitro activity of daptomycin combined with other antimicrobial agents against Gram-negative bacteria. Clin. Microbiol. Infect. 2010, 16, S156–S157. [Google Scholar]
- Grundmann, H.; Glasner, C.; Albiger, B.; Aanensen, D.M.; Tomlinson, C.T.; Andrasević, A.T.; Cantón, R.; Carmeli, Y.; Friedrich, A.W.; Giske, C.G.; et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): A prospective, multinational study. Lancet Infect. Dis. 2017, 17, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Maraki, S.; Mavromanolaki, V.E.; Moraitis, P.; Stafylaki, D.; Kasimati, A.; Magkafouraki, E.; Scoulica, E. Ceftazidime-avibactam, meropenen-vaborbactam, and imipenem-relebactam in combination with aztreonam against multidrug-resistant, metallo-β-lactamase-producing Klebsiella pneumoniae. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1755–1759. [Google Scholar] [CrossRef]
- Emeraud, C.; Escaut, L.; Boucly, A.; Fortineau, N.; Bonnin, R.A.; Naas, T.; Dortet, L. Aztreonam plus clavulanate, tazobactam, or avibactam for treatment of infections caused by metallo-β-lactamase-producing Gram-negative bacteria. Antimicrob. Agents Chemother. 2019, 63, e00010-19. [Google Scholar] [CrossRef]
- Wenzler, E.; Deraedt, M.F.; Harrington, A.T.; Danizger, L.H. Synergistic activity of ceftazidime-avibactam and aztreonam against serine and metallo-β-lactamase-producing gram-negative pathogens. Diagn. Microbiol. Infect. Dis. 2017, 88, 352–354. [Google Scholar] [CrossRef]
- Davido, B.; Fellous, L.; Lawrence, C.; Maxime, V.; Rottman, M.; Dinh, A. Ceftazidime-avibactam and aztreonam, an interesting strategy to overcome β-lactam resistance conferred by metallo-β-lactamases in Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2017, 61, e01008-17. [Google Scholar] [CrossRef]
- Marshall, S.; Hujer, A.M.; Rojas, L.J.; Papp-Wallace, K.M.; Humphries, R.M.; Spellberg, B.; Hujer, K.M.; Marshall, E.K.; Rudin, S.D.; Perez, F.; et al. Can ceftazidime-avibactam and aztreonam overcome β-lactam resistance conferred by metallo-β-lactamases in Enterobacteriaceae? Antimicrob. Agents Chemother. 2017, 61, e02243-16. [Google Scholar] [CrossRef] [PubMed]
- Biagi, M.; Wu, T.; Lee, M.; Patel, S.; Butler, D.; Wenzler, E. Searching for the optimal treatment for metallo- and serine-β-Lactamase producing Enterobacteriaceae: Aztreonam in combination with ceftazidime-avibactam or meropenem-vaborbactam. Antimicrob. Agents Chemother. 2019, 63, e01426-19. [Google Scholar] [CrossRef]
- Karakonstantis, S.; Kritsotakis, E.I.; Gikas, A. Treatment options for K. pneumoniae, P. aeruginosa and A. baumannii co-resistant to carbapenems, aminoglycosides, polymyxins and tigecycline: An approach based on the mechanisms of resistance to carbapenems. Infection 2020, 48, 835–851. [Google Scholar] [CrossRef]
- Jayol, A.; Nordmann, P.; Poirel, L.; Dubois, V. Ceftazidime/avibactam alone or in combination with aztreonam against colistin-resistant and carbapenemase-producing Klebsiella pneumoniae. J. Antimicrob. Chemother. 2018, 73, 542–544. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Daikos, G.L.; Tiseo, G.; Bassoulis, D.; Giordano, C.; Galfo, V.; Leonildi, A.; Tagliaferri, E.; Barnini, S.; Sani, S.; et al. Efficacy of ceftazidime-avibactam plus aztreonam in patients with bloodstream infections caused by metallo-β-lactamase-producing Enterobacterales. Clin. Infect. Dis. 2021, 72, 1871–1878. [Google Scholar] [CrossRef] [PubMed]
- Mauri, C.; Maraolo, A.E.; Di Bella, S.; Luzzaro, F.; Principe, L. The revival of aztreonam in combination with avibactam against metallo-β-lactamase-producing Gram-negatives: A systematic review of in vitro studies and clinical cases. Antibiotics 2021, 10, 1012. [Google Scholar] [CrossRef] [PubMed]
- Sader, H.S.; Carvalhaes, C.G.; Arends, S.J.R.; Castanheira, M.; Mendes, R.E. Aztreonam/avibactam activity against clinical isolates of Enterobacterales collected in Europe, Asia and Latin America in 2019. J. Antimicrob. Chemother. 2021, 76, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Rossolini, G.M.; Stone, G.; Kantecki, M.; Arhin, F.F. In vitro activity of aztreonam/avibactam against isolates of Enterobacterales collected globally from ATLAS in 2019. J. Glob. Antimicrob. Resist. 2022, 30, 214–221. [Google Scholar] [CrossRef]
- Paul, M.; Daikos, G.L.; Durante-Mangoni, E.; Yahav, D.; Carmeli, Y.; Benattar, Y.D.; Skiada, A.; Andini, R.; Eliakim-Raz, N.; Nutman, A.; et al. Colistin alone versus colistin plus meropenem for treatment of severe infections caused by carbapenem-resistant Gram-negative bacteria: An open-label, randomised controlled trial. Lancet Infect. Dis. 2018, 18, 391–400. [Google Scholar] [CrossRef]
- Gutiérrez-Gutiérrez, B.; Salamanca, E.; de Cueto, M.; Hsueh, P.R.; Viale, P.; Paño-Pardo, J.R.; Venditti, M.; Tumbarello, M.; Daikos, G.; Cantón, R.; et al. Effect of appropriate combination therapy on mortality of patients with bloodstream infections due to carbapenemase-producing Enterobacteriaceae (INCREMENT): A retrospective cohort study. Lancet Infect. Dis. 2017, 17, 726–734. [Google Scholar] [CrossRef]
- Liu, Q.; Li, W.; Feng, Y.; Tao, C. Efficacy and safety of polymyxins for the treatment of Acinectobacter baumannii infection: A systematic review and meta-analysis. PLoS ONE 2014, 9, e98091. [Google Scholar] [CrossRef] [PubMed]
- Dickstein, Y.; Lellouche, J.; Ben Dalak Amar, M.; Schwartz, D.; Nutman, A.; Daitch, V.; Yahav, D.; Leibovici, L.; Skiada, A.; Antoniadou, A.; et al. Treatment outcomes of colistin- and carbapenem-resistant Acinetobacter baumannii infections: An exploratory subgroup analysis of a randomized clinical trial. Clin. Infect. Dis. 2019, 69, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Karakonstantis, S.; Ioannou, P.; Samonis, G.; Kofteridis, D.P. Systematic review of antimicrobial combination options for pandrug-resistant Acinetobacter baumannii. Antibiotics 2021, 10, 1344. [Google Scholar] [CrossRef] [PubMed]
- Perez, F.; El Chakhtoura, N.G.; Yasmin, M.; Bonomo, R.A. Polymyxins: To combine or not to combine? Antibiotics 2019, 8, 38. [Google Scholar] [CrossRef] [PubMed]
- Pillai, S.K.; Moellering, R.C.; Eliopoulos, G.M. Antimicrobial combinations. In Antimicrobials in Laboratory Medicine, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 365–435. [Google Scholar]
| Antimicrobial | Number of Isolates Tested | MIC Range (mg/L) | MIC50 (mg/L) | MIC90 (mg/L) | Resistance (%) |
|---|---|---|---|---|---|
| Meropenem | 200 | 8–≥16 | ≥16 | ≥16 | 100 |
| Imipenem | 200 | ≥16 | ≥16 | ≥16 | 100 |
| Colistin | 200 | 4–≥16 | ≥16 | ≥16 | 100 |
| Ciprofloxacin | 200 | ≥4 | ≥4 | ≥4 | 100 |
| Amikacin | 136 | 4–≥64 | ≥64 | ≥64 | 97.79 |
| Gentamicin | 133 | 1–≥16 | ≥16 | ≥16 | 98.49 |
| Ampicillin/Sulbactam | 158 | 16–≥32 | ≥32 | ≥32 | NA |
| Tigecycline | 192 | 0.047–12 | 3 | 6 | NA |
| Rifampicin | 178 | 1–≥256 | 6 | 32 | NA |
| Daptomycin | 128 | ≥256 | ≥256 | ≥256 | NA |
| Antimicrobial | Number of Isolates Tested | MIC Range (mg/L) | MIC50 (mg/L) | MIC90 (mg/L) | Resistance (%) |
|---|---|---|---|---|---|
| Meropenem | 106 | ≥16 | ≥16 | ≥16 | 100 |
| Imipenem | 106 | ≥16 | ≥16 | ≥16 | 100 |
| Colistin | 106 | 4–≥16 | ≥16 | ≥16 | 100 |
| Ceftazidime/Avibactam | 104 | 1–≥16 | ≥16 | ≥16 | 87.50 |
| Ceftazidime | 103 | 16–≥64 | ≥64 | ≥64 | 100 |
| Ceftolozane/Tazobactam | 83 | ≥32 | ≥32 | ≥32 | 100 |
| Cefotaxime | 81 | 2–≥64 | ≥64 | ≥64 | 96.29 |
| Aztreonam | 104 | 16–≥64 | ≥64 | ≥64 | 100 |
| Ciprofloxacin | 102 | 0.25–≥4 | ≥4 | ≥4 | 99.01 |
| Amikacin | 104 | 2–≥64 | 32 | ≥64 | 97.11 |
| Gentamicin | 101 | 1–≥16 | ≥16 | ≥16 | 93.06 |
| Piperacillin/Tazobactam | 102 | ≥128 | ≥128 | ≥128 | 100 |
| Fosfomycin | 102 | 16–≥256 | 256 | ≥256 | 90.19 |
| Tigecycline | 92 | 0.25–8 | 2 | 8 | NA |
| Chloramphenicol | 91 | 2–≥64 | 32 | ≥64 | 87.91 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mantzana, P.; Protonotariou, E.; Kassomenaki, A.; Meletis, G.; Tychala, A.; Keskilidou, E.; Arhonti, M.; Katsanou, C.; Daviti, A.; Vasilaki, O.; et al. In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae. Antibiotics 2023, 12, 93. https://doi.org/10.3390/antibiotics12010093
Mantzana P, Protonotariou E, Kassomenaki A, Meletis G, Tychala A, Keskilidou E, Arhonti M, Katsanou C, Daviti A, Vasilaki O, et al. In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae. Antibiotics. 2023; 12(1):93. https://doi.org/10.3390/antibiotics12010093
Chicago/Turabian StyleMantzana, Paraskevi, Efthymia Protonotariou, Angeliki Kassomenaki, Georgios Meletis, Areti Tychala, Eirini Keskilidou, Maria Arhonti, Charikleia Katsanou, Aikaterini Daviti, Olga Vasilaki, and et al. 2023. "In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae" Antibiotics 12, no. 1: 93. https://doi.org/10.3390/antibiotics12010093
APA StyleMantzana, P., Protonotariou, E., Kassomenaki, A., Meletis, G., Tychala, A., Keskilidou, E., Arhonti, M., Katsanou, C., Daviti, A., Vasilaki, O., Kagkalou, G., & Skoura, L. (2023). In Vitro Synergistic Activity of Antimicrobial Combinations against Carbapenem- and Colistin-Resistant Acinetobacter baumannii and Klebsiella pneumoniae. Antibiotics, 12(1), 93. https://doi.org/10.3390/antibiotics12010093







