A Novel Single-Tube Eicosaplex/Octaplex PCR System for the Detection of Extended-Spectrum β-Lactamases, Plasmid-Mediated AmpC β-Lactamases, and Integrons in Gram-Negative Bacteria
Abstract
1. Introduction
2. Materials and Methods
2.1. Bacterial Isolates
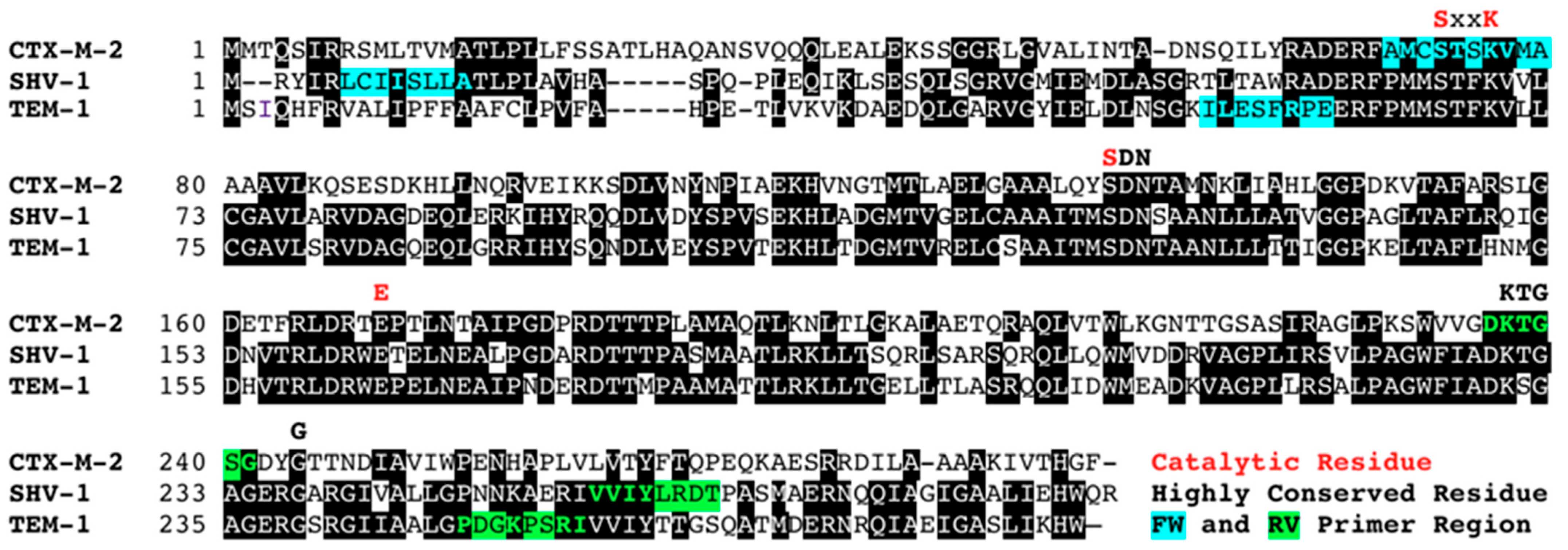
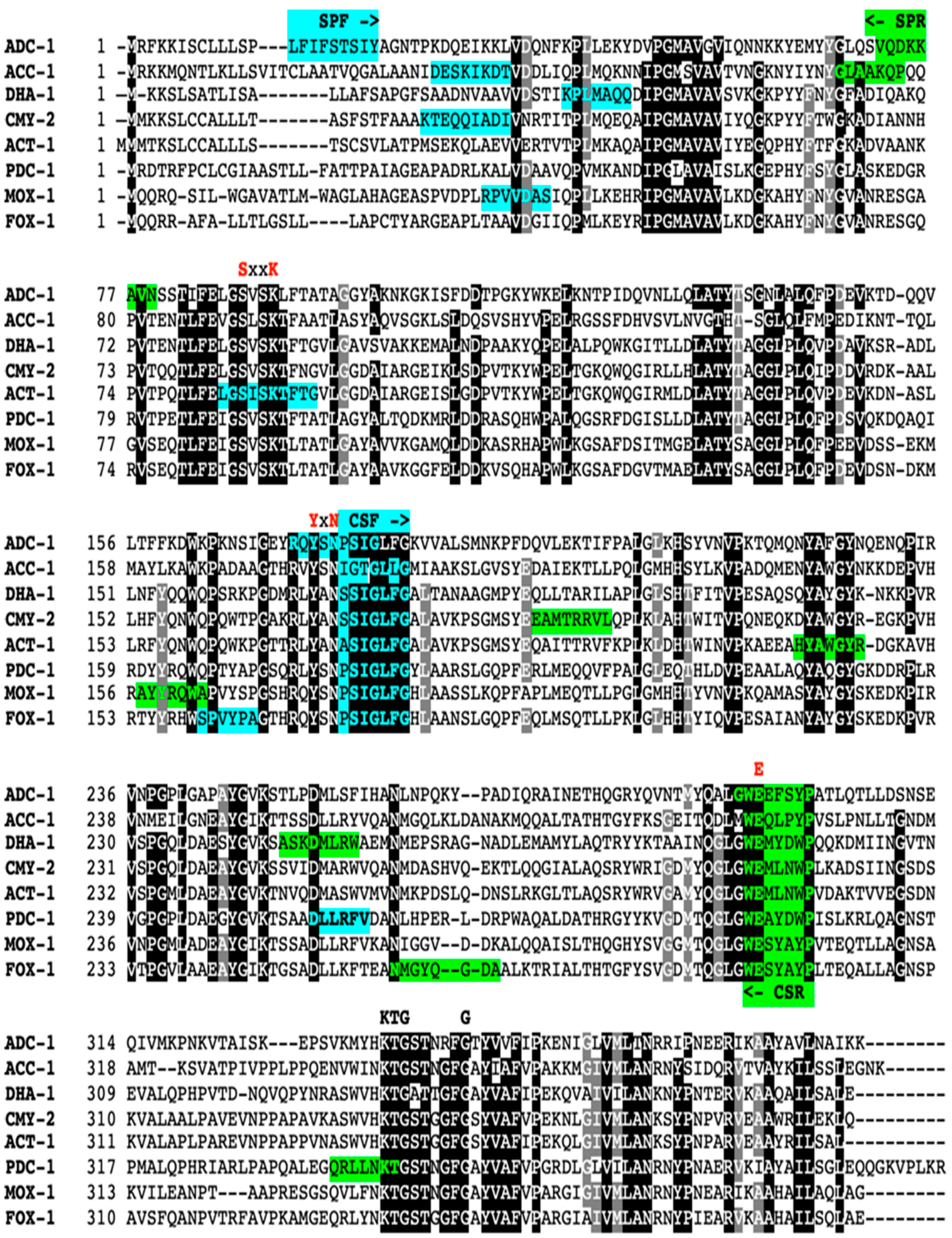
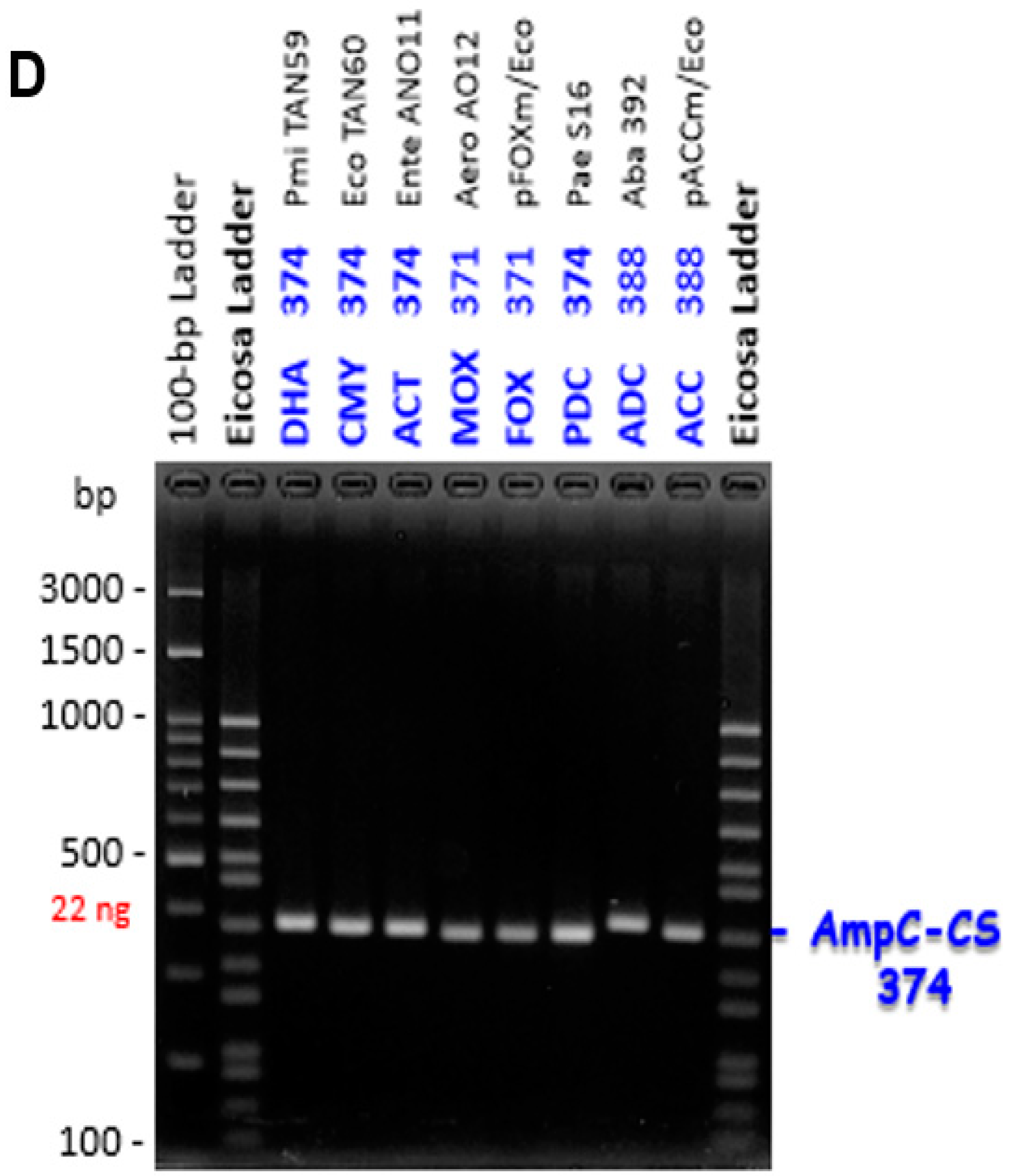
2.2. Design of Specific Primers for Eicosaplex and Octaplex PCRs
2.3. Eicosaplex and Octaplex PCR Technique
2.4. DNA Sequencing and Analysis
2.5. Whole Genome Sequencing and Analysis
3. Results and Discussion
3.1. MER, CTX, CAZ-Resistant Strains from the ANO and AO Substances
3.2. Design of Specific Primers for Eicosaplex and Octaplex PCRs
3.3. Evaluation of the Eicosaplex and Octaplex PCRs with Gram-Negative Strains Isolated from Vegetables and Fruits in Japan
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Centres for Disease Control and Prevention (US). Antibiotic Resistance Threats in the United States; Centres for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2019. Available online: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf (accessed on 5 November 2022).
- O’Neill, J. (Chairman) the review on antimicrobial resistance. Tackling a globalhealth crisis: Initial steps. AMR Rev. Lond. 1–20. Available online: https://amr-review.org/sites/default/files/Report-52.15.pdf (accessed on 5 November 2022).
- Bush, K.; Bradford, P.A. β-Lactams and β-lactamase inhibitors: An overview. In Antibiotics and Antibiotic Resistance; Silver, L.L., Bush, K., Eds.; Cold Spring Harbor Laboratory Press: Cold Spring Harbor, NY, USA, 2016; pp. 23–44. [Google Scholar]
- Bush, K. Past and present perspectives on β-lactamases. Antimicrob. Agents Chemother. 2018, 62, e01076-18. [Google Scholar] [CrossRef]
- Jacoby, G.A. AmpC β-lactamases. Clin. Microbiol. Rev. 2009, 22, 161–182. [Google Scholar] [CrossRef]
- Brolund, A.; Sandegren, L. Characterization of ESBL disseminating plasmids. J. Infect. Dis. 2016, 48, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Dhillon, R.H.; Clark, J. ESBLs: A clear and present danger? Crit. Care Res. Pract. 2012, 2012, 625170. [Google Scholar] [CrossRef] [PubMed]
- Hall, R.M. Integrons and gene cassettes: Hotspots of diversity in bacterial genomes. Ann. N. Y. Acad. Sci. 2012, 1267, 71–78. [Google Scholar] [CrossRef]
- Hall, R.M.; Collis, C.M. Antibiotic resistance in gram-negative bacteria: The role of gene cassettes and integrons. Drug Resist. Updates 1998, 1, 109–119. [Google Scholar] [CrossRef] [PubMed]
- Zankari, E.; Hasman, H.; Cosentino, S.; Vestergaard, M.; Rasmussen, S.; Lund, O.; Aarestrup, F.M.; Larsen, M.V. Identification of acquired antimicrobial resistance genes. J. Antimicrob. Chemother. 2012, 67, 2640–2644. [Google Scholar] [CrossRef]
- Dallenne, C.; Da Costa, A.; Decré, D.; Favier, C.; Arlet, G. Development of a set of multiplex PCR assays for the detection of genes encoding important β-lactamases in Enterobacteriaceae. J. Antimicrob. Chemother. 2010, 65, 490–495. [Google Scholar] [CrossRef]
- Trung, N.T.; Hien, T.T.T.; Huyen, T.T.T.; Quyen, D.T.; Binh, M.T.; Hoan, P.Q.; Meyer, C.G.; Velavan, T.P. Simple multiplex PCR assays to detect common pathogens and associated genes encoding for acquired extended spectrum betalactamases (ESBL) or carbapenemases from surgical site specimens in Vietnam. Ann. Clin. Microbiol. Antimicrob. 2015, 14, 23. [Google Scholar] [CrossRef]
- Kazi, M.; Ajbani, K.; Tornheim, J.A.; Shetty, A.; Rodrigues, C. Multiplex PCR to detect pAmpC β-lactamases among enterobacteriaceae at a tertiary care laboratory in Mumbai, India. Microbiology (Read. Engl.) 2019, 165, 246–250. [Google Scholar] [CrossRef]
- Kao, C.C.; Liu, M.F.; Lin, C.F.; Huang, Y.C.; Liu, P.Y.; Chang, C.W.; Shi, Z.Y. Antimicrobial susceptibility and multiplex PCR screening of AmpC genes from isolates of Enterobacter cloacae, Citrobacter freundii, and Serratia marcescens. J. Microbiol. Immunol. Infect. 2010, 43, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.M.; Ahmed, A.M.; Shimamoto, T.; El-Domany, R.A.; Nariya, H.; Shimamoto, T. First report in Africa of two clinical isolates of Proteus mirabilis carrying Salmonella genomic island (SGI1) variants, SGI1-PmABB and SGI1-W. Infect. Genet. Evol. 2017, 51, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Hussein, A.I.; Ahmed, A.M.; Sato, M.; Shimamoto, T. Characterization of integrons and antimicrobial resistance genes in clinical isolates of Gram-negative bacteria from Palestinian hospitals. Microbiol. Immunol. 2009, 53, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.M.; Shimamoto, T.; Nariya, H.; Shimamoto, T. Emergence of Salmonella genomic island 1 variant SGI1-W in a clinical isolate of Providencia stuartii from Egypt. Antimicrob. Agents Chemother. 2018, 63, e01793-18. [Google Scholar] [CrossRef]
- Khalifa, H.O.; Soliman, A.M.; Saito, T.; Kayama, S.; Yu, L.; Hisatsune, J.; Sugai, M.; Nariya, H.; Ahmed, A.M.; Shimamoto, T.; et al. First report of foodborne Klebsiella pneumoniae coharboring blaVIM-1, blaNDM-1, and mcr-9. Antimicrob. Agents Chemother. 2020, 64, e00882-20. [Google Scholar] [CrossRef] [PubMed]
- Soliman, A.M.; Zarad, H.O.; Nariya, H.; Shimamoto, T.; Shimamoto, T. Genetic analysis of carbapenemase-producing Gram-negative bacteria isolated from a university teaching hospital in Egypt. Infect. Genet. Evol. 2020, 77, 104065. [Google Scholar] [CrossRef]
- Soliman, A.M.; Nariya, H.; Tanaka, D.; Yu, L.; Hisatsune, J.; Kayama, S.; Kondo, K.; Sugai, M.; Shimamoto, T.; Shimamoto, T. Vegetable-derived carbapenemase-producing high-risk Klebsiella pneumoniae ST15 and Acinetobacter baumannii ST2 clones in Japan: Coexistence of blaNDM-1, blaOXA-66, blaOXA-72, and an AbaR4-Like resistance island in the same sample. Appl. Environ. Microbiol. 2021, 87, e02166-20. [Google Scholar] [CrossRef]
- Park, C.; Kim, S.B.; Choi, S.H.; Kim, S. Comparison of 16S rRNA gene based microbial profiling using five next-generation sequencers and various primers. Front. Microbiol. 2021, 12, 715500. [Google Scholar] [CrossRef]
- Wick, R.R.; Judd, L.M.; Gorrie, C.L.; Holt, K.E. Unicycler: Resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 2017, 13, e1005595. [Google Scholar] [CrossRef]
- Yeni, F.; Yavaş, S.; Alpas, H.; Soyer, Y. Most common foodborne pathogens and mycotoxins on fresh produce: A review of recent outbreaks. Crit. Rev. Food Sci. Nutr. 2016, 56, 1532–1544. [Google Scholar] [CrossRef]
- Pletz, M.W.; Wollny, A.; Dobermann, U.-H.; Rödel, J.; Neubauer, S.; Stein, C.; Brandt, C.; Hartung, A.; Mellmann, A.; Trommer, S.; et al. A nosocomial foodborne outbreak of a VIM carbapenemase-expressing Citrobacter freundii. Clin. Infect. Dis. 2018, 67, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Poirel, L.; Walsh, T.R.; Cuvillier, V.; Nordmann, P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn. Microbiol. Infect. Dis. 2011, 70, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Sapkota, S.; Adhikari, S.; Pandey, A.; Khadka, S.; Adhikari, M.; Kandel, H.; Pathak, S.; Pandey, A. Multi-drug resistant extended-spectrum beta-lactamase producing E. coli and Salmonella on raw vegetable salads served at hotels and restaurants in Bharatpur, Nepal. BMC Res. Notes 2019, 12, 516. [Google Scholar] [CrossRef] [PubMed]
- Colosi, I.A.; Baciu, A.M.; Opriș, R.V.; Peca, L.; Gudat, T.; Simon, L.M.; Colosi, H.A.; Costache, C. Prevalence of ESBL, AmpC and carbapenemase-producing Enterobacterales isolated from raw vegetables retailed in Romania. Foods 2020, 9, 1726. [Google Scholar] [CrossRef]

| Strain Name | Bacterial spp. | Source | Country | Isolation Year | Resistance Genes | Reference |
|---|---|---|---|---|---|---|
| Eco TAN60 | E. coli | Clinical | Egypt | 2014 | blaNDM-1, blaSHV-12, blaCTX-M-15, blaTEM-1, blaCMY-2, class 1 integron (aac(6’)-Ib), qnrS, rmtC | [19] |
| Eco TAN92 | E. coli | Clinical | Egypt | 2014 | blaNDM-1, blaCTX-M-15, blaCMY-2, rmtC, class 1 integron carrying (aac(6´)-Ib) | [19] |
| Eco PL65 | E. coli | Clinical | Palestine | 2006 | blaTEM-1, blaOXA-1, blaCTX-M-15, aac(6´)-Ib-cr | [16] |
| Pmi TAN59 | P. mirabilis | Clinical | Egypt | 2014 | class 1 integron (aacA5-aadA7-qacE1- sul1), blaTEM-1, blaDHA, blaOXA-5, qnrA1, class 2 integron (intI2) | [15] |
| Kpn D6 | K. pneumoniae | Water | Japan | 2016 | blaTEM-1, blaSHV-12, blaOXA-1, blaCTX-M-15, aac(6´)-Ib-cr5, oqxAB, class 1 integron | This study |
| Kpn LM22-1 | K. pneumoniae | Chicken | Japan | 2016 | blaSHV-71, oqxAB, fosA, blaVIM-1, mcr-9, blaTEM-1B, blaCTX-M-9, aadA24, ant(2´´)-Ia, aadA2, aph(3´)-Ia, sul1, dfrA1, blaNDM-1, aac(6´)-Ib, aadA1, blaCTX-M-15, blaOXA-9, blaTEM-1A, qnrS1, aac(6´)-Ib-cr | [18] |
| Kpn AO15/22 | K. pneumoniae | Vegetable | Japan | 2015 | blaSHV-28, fosA, oqxAB, blaSHV-1, blaTEM-1A, tet(D), aac(6’)-Ib, aadA1, aph(3’)-VI, blaCTXM-15, blaNDM-1, blaOXA-9, aac(6’)-Ib-cr, qnrS1, aph(6)-Id, aph(3’)-VIb, aph(3’’)-Ib, blaCTXM-14b | [20] |
| Pst TAN3 | P. stuartii | Clinical | Egypt | 2014 | class 1 integron (aadA2-lnuF), blaTEM-1, blaDHA-1, qnrD, floR, class 2 integron (intI2) | [17] |
| Pst TAN14 | P. stuartii | Clinical | Egypt | 2014 | blaNDM-1, blaCMY-2, blaDHA-1, rmtC, qnrA, qnrD, class 1 integron carrying (aac(6’)-Ib) | [19] |
| Pae S16 | P. aeruginosa | Clinical | Egypt | 2014 | class 1 integron (blaVIM-24-aadB-blaOXA-10), blaPDC | [19] |
| Aba 392 | A. baumannii | Clinical | Egypt | 2015 | blaOXA-23-like,blaOXA-51-like, class 1 integron, blaADC,aac(6’)-Ib | This study |
| Aba AO22 | A. baumannii | Vegetable | Japan | 2015 | class 1 integron, blaADC-25, blaOXA-66, sul2, tet(B), aac(3)-Ia, aac(6’)-Ip, aph(3’’)-Ib, aph(6)-Id | [20] |
| Aero AO12 | Aeromonas spp. | Vegetable | Japan | 2014-2015 | blaMOX-12 | This study |
| Aero 19-2B | Aeromonas spp. | Vegetable | Japan | 2019 | blaFOX | This study |
| Ente ANO11 | Enterobacter spp. | Vegetable | Japan | 2014-2015 | blaACT-64 | This study |
| Plasmid Name | Vector | Resistance Genes | Reference |
|---|---|---|---|
| pOXA-2m | pEX-K4J2 (KmR) | blaOXA-2 | This study |
| pIntI3m | pEX-K4J2 (KmR) | Integrase gene of class 3 integron (intI3) | This study |
| pFOXm | pEX-K4J2 (KmR) | blaFOX | This study |
| pACCm | pEX-K4J2 (KmR) | blaACC | This study |
| Primer | Sequence (5’–3’) 1 | Targeted Gene or Targeted β-Lactamase(s) 2 | Amplicon Size (bp) | Primer Concentration (pmol/μL) | Reference |
|---|---|---|---|---|---|
| 515F 1492R | GTGCCAGCMGCCGCGGTAA CGGYTACCTTGTTACGACTT | 16S rRNA | 1001 | 0.2 0.2 | This study |
| OXA1-WGF OXA1-WGR | ATGAAAAACACAATACATATCAACTTC TTATAAATTTAGTGTGTTTAGAATGGTG | OXA-1, OXA-4, OXA-30, OXA-31, OXA-47, OXA-224, OXA-320, OXA-392, OXA-543 | 831 | 0.4 0.4 | This study |
| SHV-FW SHV-RV | GTGTATTATCTCCCTGTTAGCC GGCCAAGCAGGGCGACAAT | SHV-1 to SHV-203 | 722 | 0.2 0.2 | This study |
| TEM-FW TEM-RV | TTGAGAGTTTTCGCCCCGAA ACGGGAGGGCTTACCATCTG | TEM-1 to TEM-232 | 602 | 0.1 0.1 | This study |
| CTXM-FW CTXM-RV | TGCAGYACCAGTAARGTKATGGC CCGCTGCCGGTYTTATC | CTX-M-1 to CTX-M-214, KLUA, KLUC, KLUG, and TOHO-1 to TOHO-3 | 509 | 0.3 0.3 | This study |
| OXA2-FW OXA2-RV | ATAGTTGTGGCAGACGAACG TTGACCAAGCGCTGATGTTC | OXA-2, OXA-3, OXA-15, OXA-20, OXA-21, OXA-32, OXA-37, OXA-46, OXA-53, OXA-118, OXA-119, OXA-141, OXA-161, OXA-210, OXA-226, OXA-415, OXA-539, OXA-540, OXA-541, OXA-543, OXA-544 | 452 | 0.2 0.2 | This study |
| CMY/LAT-CSFCMY/LAT-CSR | TCCAGCATTGGTCTGTTTGG GGCCAGTTCAGCATCTCCCA | CMY-2 to CMY-157, BIL-1, LAT-1 to LAT-4, CFE-1 | 374 | 0.1 0.1 | This study |
| MIR/ACT-CSFMIR/ACT-CSR1 MIR/ACT-CSR2 | GCCAGCATCGGTCTTTTTGG GGCCAGTTGAGCATCTCCCA GGCCAGTTTAGCATTTCCCA | ACT-1 to ACT-54, MIR-1 to MIR-22 | 374 | 0.1 0.1 0.1 | This study |
| DHA-CSF DHA-CSR | AGCAGTATCGGCCTGTTTGG GGCCAGTCATACATTTCCCA | DHA-1 to DHA-25 | 374 | 0.1 0.1 | This study |
| MOX-CSF1 MOX-CSF2 MOX-CSR | CCCAGCATAGGGCTGTTCGG CCCAGCATCGGGCTCTTTGG GGATAGGCGTAACKCTCCCA | MOX-1 to MOX-13, CMY-1, CMY-8, CMY-8b, CMY-9, CMY-10, CMY-11, CMY-19 | 371 | 0.1 0.1 0.1 | This study |
| FOX-CSF FOX-CSR | CCCAGCATMGGCCTGTTTGG GGATAGGCGTARCTCTCCCA | FOX-1 to FOX-16 | 371 | 0.1 0.1 | This study |
| PDC-CSF PDC-CSR | CCGAGCATCGGYCTGTTCGG GGCCAGTCGTAGGCTTCCCA | PDC-1 to PDC-249 | 374 | 0.1 0.1 | This study |
| ACC-CSF ACC-CSR | ATCGGTACYGGTTTGCTAGG GGATATGGCARCTGCTCCCA | ACC-1 to ACC-7 | 380 | 0.1 0.1 | This study |
| ADC-CSF ADC-CSR | GACAATATTCAAAYCCAAGYATTGG GGATAAGAAAAYTCTTCCCAACC | ADC-1 to ADC-107 | 388 | 0.4 0.4 | This study |
| OXA5-FW OXA5-RV | GTATTTCAACAAATYGCCAGAGA CCACCAWGCGACACCAGGA | OXA-5, OXA-7, OXA-10, OXA-11, OXA-13, OXA-14, OXA-17, OXA-19, OXA-28, OXA-35, OXA-56, OXA-74, OXA-101, OXA-129, OXA-142, OXA-145, OXA-147, OXA-183, OXA-233, OXA-240, OXA-246, OXA-251, OXA-256, OXA-368, OXA-454, OXA-520 | 312 | 0.4 0.4 | This study |
| AAC6-FW AAC6-RV | TTGCGATGCTCTATGAGTGGCTA AGTTGTGATGCATTCGCCAG | aac(6′)-Ib | 274 | 0.1 0.1 | This study |
| OXA9-FW OXA9-RV | CAGTTCCGTGGCTTCTGATG GTTGTATTCCGGCTTCAATTCC | OXA-9a, OXA-9b | 211 | 0.1 0.1 | This study |
| IntI1-FW IntI1-RV | AGCTTGGCACCCAGCCTG GACACCGCTCCGTGGATC | intI1 of class 1 integron | 192 | 0.15 0.15 | This study |
| IntI2-FW IntI2-RV | AAGGTTATGCGCTGAAAACTGAA TCTGCGTGTTTATGGCTACATG | intI2 of class 2 integron | 159 | 0.1 0.1 | This study |
| IntI3-FW IntI3-RV | CACCGAGAAGCAAGTGG AATCCGCTTGCGTTCTG | intI3 of class 3 integron | 133 | 0.2 0.2 | This study |
| Primer | Sequence (5’–3’) 1 | Targeted Gene or Targeted β-Lactamase(s) | Amplicon Size (bp) | Primer Concentration (pmol/μL) | Reference |
|---|---|---|---|---|---|
| DHA-SPF DHA-SPR | ACCGCTGATGGCACAGCAG CAGCGCAGCATATCTTTTGAG | DHA-1 to DHA-25 | 648 | 0.2 0.2 | This study |
| CMY/LAT-SPFCMY/LAT-SPR1 CMY/LAT-SPR2 | AAAACAGAACAACARATTGCCGATA GGACGCGTCTGGTCATTGCC GGACGCGGGTGGTCATCGCC | CMY-2 to CMY-157, BIL-1, LAT-1 to LAT-4, CFE-1 | 529 | 0.2 0.2 0.2 | This study |
| MIR/ACT-SPF1MIR/ACT-SPF2MIR/ACT-SPR1MIR/ACT-SPR2 | CTGGGYTCTATAAGTAAAACCTTCACCG CTGGGCTCAATCAGCAAAACCTTCACCG CGGTATCCCCAGGCGTAATG CGATAGCCCCAGGCGTAATG | ACT-1 to ACT-54, MIR-1 to MIR-22 | 428 | 0.3 0.3 0.3 0.3 | This study |
| MOX-SPF MOX-SPR | GCCCCGTGGTGGATGCCAG GYCCACTGGCGGTAGTAGGC | MOX-1 to MOX-13, CMY-1, CMY-8, CMY-8b, CMY-9, CMY-10, CMY-11, CMY-19 | 391 | 0.2 0.2 | This study |
| FOX-SPF FOX-SPR | TGGTCACCGGTTTATCCGGC GCATCTCCCTGATACCCCATGTT | FOX-1 to FOX-16 | 323 | 0.2 0.2 | This study |
| PDC-SPF PDC-SPR | GACCTGCTGCGCTTCGTC GGTCTTGTTCAGCAGGCGCT | PDC-1 to PDC-249 | 263 | 0.2 0.2 | This study |
| ADC-SPF ADC-SPR | CTTTTTATTTTTAGTACCTCAATTTATGC TGCTATTTACGGCTTTTTTATCTTGAAC | ADC-1 to ADC-107 | 202 | 0.4 0.4 | This study |
| ACC-SPF ACC-SPR | GATGAGAGCAAAATTAAAGACACCG AGGCTGTTTTGCCGCTAACC | ACC-1 to ACC-7 | 143 | 0.2 0.2 | This study |
| 54 ANO | Number of Isolates | CTX-M | OXA-1 | OXA-2 | OXA-5 | OXA-9 | SHV | TEM | aac(6’) | intI1 | intI2 | intI3 | AmpC | DHA | CMY/LAT | ACT/MIR | MOX | FOX | PDC | ADC | ACC | ND |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Enterobacter | 16 | - | - | - | - | - | 1 | 2 | - | - | - | - | 16 | - | - | 15 | - | - | - | - | - | 1 |
| Klebsiella | 6 | - | - | - | - | - | 5 | - | - | - | - | - | 1 | - | - | 1 | - | - | - | - | - | - |
| Citrobacter | 2 | - | - | - | - | - | - | - | - | - | - | - | 2 | - | - | - | - | - | - | - | - | 2 |
| Pseudomonas | 1 | - | - | - | - | - | - | - | - | - | - | - | 1 | - | - | - | - | - | - | - | - | 1 |
| Rhanella | 1 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Total | 26 | 1 | - | - | - | - | 6 | 2 | - | - | - | - | 20 | - | - | 16 | - | - | - | - | - | 4 |
| 55 AO | Number of Isolates | CTX-M | OXA-1 | OXA-2 | OXA-5 | OXA-9 | SHV | TEM | aac(6’) | intI1 | intI2 | intI3 | AmpC | DHA | CMY/LAT | ACT/MIR | MOX | FOX | PDC | ADC | ACC | ND |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Klebsiella | 18 | 8 | - | - | - | 2 | 11 | 2 | 2 | - | - | - | 1 | - | - | - | - | - | - | - | - | 1 |
| Enterobacter | 7 | - | - | - | - | - | - | - | - | - | - | - | 7 | - | - | 7 | - | - | - | - | - | - |
| Acinetobacter | 4 | - | - | - | - | - | - | - | - | 1 | - | - | 4 | - | - | - | - | - | - | 4 | - | - |
| Aeromonas | 1 | - | - | - | - | - | - | - | - | - | - | - | 1 | - | - | - | 1 | - | - | - | - | - |
| Proteus | 1 | 1 | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| Total | 31 | 9 | - | - | - | 2 | 11 | 2 | 2 | 1 | - | - | 13 | - | - | 7 | 1 | - | - | 4 | - | 1 |
| No. | Strain AO | Source (# Imported) | Identification by 16S rRNA Sequencing 2 | Growing on LB Agar Medium Supplemented with 3 | Genotype Eicosa (Octa) Plex PCR 4 | ||||
|---|---|---|---|---|---|---|---|---|---|
| AMP 100 24 h | MER 4 24 h | MER 1 24 h | CTX 4 24 h | CAZ 16 24 h | |||||
| 1 | 1-1 | Green onion | ND | + | ND | ||||
| 2 | 1-2 | ND | + | ND | |||||
| 3 | 2-1 | Hakusai | Klebsiella oxytoca | + | OXY-2 | ||||
| 4 | 2-3 | Pseudomonas spp. | + | + | + | ND | |||
| 5 | 2-5 | Klebsiella oxytoca | + | OXY-2 | |||||
| 6 | 2-6 | Pseudomonas spp. | + | + | + | ND | |||
| 7 | 3-1 | Carrot | Aeromonas spp. | + | ND | ||||
| 8 | 3-2 | ND | + | ND | |||||
| 9 | 3-3 | Enterobacter spp. | + | AmpC (ACT) ACT-51v | |||||
| 10 | 4-1 | Leaf lettuce | ND | + | ND | ||||
| 11 | 4-2 | Enterobacter spp. | + | AmpC (ACT) ACT-2v | |||||
| 12 | 4-3 | Aeromonas spp. | + | AmpC (MOX) MOX-12v | |||||
| 13 | 4-4 | ND | + | ND | |||||
| 14 | 5-1 | Italian parsley | ND | + | ND | ||||
| 15 1 | 5-4 | Klebsiella pneumoniae | + | + | + | + | + | SHV, TEM, CTXM, aac(6’)-Ib, OXA-9 (NDM-1) | |
| 16 | 6-1 | Oka hijiki | Pseudomonas spp. | + | + | ND | |||
| 17 | 6-2 | ND | + | ND | |||||
| 18 | 6-3 | Pseudomonas spp. | + | + | ND | ||||
| 19 | 7-1 | # Banana 1 | Klebsiella pneumoniae | + | SHV (SHV-27) | ||||
| 20 | 7-2 | Klebsiella variicola | + | SHV (LEN-19v) | |||||
| 21 | 7-4 | Klebsiella variicola | + | SHV (LEN-19v) | |||||
| 221 | 8-1 | Baby leaf mix | Klebsiella pneumoniae | + | + | + | + | + | SHV, TEM, CTX-M, aac(6’)-Ib,OXA-9 (NDM-1) |
| 231 | 8-2 | Acinetobacter baumannii | + | + | + | + | + | AmpC (ADC) ADC-25, intI1 | |
| 24 | 8-3 | Pseudomonas spp. | + | + | ND | ||||
| 25 | 9-1 | Salad mix | ND | + | ND | ||||
| 26 | 9-2 | Kosakonia spp. | + | + | + | ND | |||
| 27 | 9-3 | Enterobacter spp. | + | AmpC (ACT) CMAEv | |||||
| 28 | 9-5 | ND | + | ND | |||||
| 29 | 9-6 | Enterobacter spp. | + | AmpC (ACT) CMAEv | |||||
| 30 | 10-1 | Red spinach | Enterobacter spp. | + | AmpC (ACT) CMAEv | ||||
| 31 | 11-1 | Radish | Klebsiella oxytoca | + | OXY-1nv | ||||
| 32 | 11-2 | Enterobacter spp. | + | + | + | AmpC (ACT) CMAEnv | |||
| 33 | 12-1 | Mizuna | ND | + | ND | ||||
| 34 | 12-2 | ND | + | ND | |||||
| 35 | 13-1 | # Banana 2 | Acinetobacter spp. | + | + | AmpC (ADC) ADCnv | |||
| 36 | 13-2 | Enterobacter spp. | + | + | + | AmpC (ACT) ACT-9 | |||
| 37 | 14-1 | Tomato | ND | + | ND | ||||
| 38 | 14-2 | ND | + | ND | |||||
| 39 | 14-3 | ND | + | ND | |||||
| 40 | 15-1 | Green paprika | Klebsiella variicola | + | SHV (LEN-27v) | ||||
| 41 | 15-2 | Proteus vulgaris | + | + | CTX-Mw HugA | ||||
| 42 | 15-3 | Acinetobacter pittii | + | + | AmpC (ADC) ADCnv | ||||
| 43 | 16-1 | Eggplant | Klebsiella variicola | + | SHV (LEN-25) | ||||
| 44 | 16-2 | Acinetobacter baumannii | + | + | AmpC (ADC) ADCnv | ||||
| 45 | 16-3 | Klebsiella pneumoniae | + | SHV (SHV-11v, BSBL) | |||||
| 46 | 17-1 | Cucumber | Klebsiella variicola | + | SHV (LEN-16) | ||||
| 47 | 17-2 | Klebsiella oxytoca | + | CTX-M (OXY-2) | |||||
| 48 | 18-1 | Onion | Kosakonia spp. | + | ND | ||||
| 49 | 18-2 | ND | + | ND | |||||
| 50 | 19-1 | Potato | Klebsiella spp. | + | OXY-1-2 | ||||
| 51 | 19-2 | Klebsiella variicola | + | SHV (LEN-13) | |||||
| 52 | 19-3 | Klebsiella aerogenes | + | AmpC (ND) CMAEv | |||||
| 53 | 20-1 | Sweet green pepper | Klebsiella pneumoniae | + | SHV (SHV-11) | ||||
| 54 | 21-1 | Purple pepper | Klebsiella spp. | + | OXY-6nv | ||||
| 55 | 21-2 | Serratia marcescens | + | + | ND | ||||
| No. | Strain ANO | Source (# Imported) | Identification by 16S rRNA Sequencing 1 | Growing on LB Agar Medium Supplemented with 2 | Genotype Eicosa (Octa) Plex PCR 3 | ||||
|---|---|---|---|---|---|---|---|---|---|
| AMP 100 24 h | MER 4 24 h | MER 1 24 h | CTX 4 24 h | CAZ 16 24 h | |||||
| 1 | 1-1 | Apple 1 | Enterobacter spp. | + | + | AmpC-CS (ACT) ACT-16 | |||
| 2 | 1-2 | Enterobacter spp. | + | + | AmpC-CS (ACT) ACT-16 | ||||
| 3 | 2-1 | Persimmon 1 | Pseudomonas spp. | + | + | + | + | ND | |
| 4 | 3-1 | Tomato1 | Pseudomonas Spp. | + | + | + | ND | ||
| 5 | 4-1 | Cucumber 1 | Klebsiella pneumoniae | + | + | SHV-41v | |||
| 6 | 4-2 | ND | + | ND | |||||
| 7 | 5-1 | Grape | Enterobacter spp. | + | AmpC-CS (ACTw) ACT-61v | ||||
| 8 | 5-2 | Enterobacter spp. | + | AmpC-CS (ACTw) ACT-61v | |||||
| 9 | 6-1 | Shimeji | Klebsiella michiganensis | + | + | AmpC-CS (ACT) CMAEv | |||
| 10 | 6-2 | Enterobacter spp. | + | AmpC-CS (ND) CMAEnv | |||||
| 11 | 7-1 | Hakusai | Enterobacter spp. | + | + | + | + | AmpC-CS (ACT) ACT-64, intI1 | |
| 12 | 7-2 | Pseudomonas alcaligenes | + | + | + | + | + | ND | |
| 13 | 8-2 | Apple 2 | Citrobacter freundii | + | + | + | AmpC-CS (ND) CMAEnv | ||
| 14 | 9-1 | Pear 1 | Pseudomonas putida | + | + | ND | |||
| 15 | 9-2 | ND | + | + | ND | ||||
| 16 | 9-4 | ND | + | + | ND | ||||
| 17 | 9-5 | ND | + | + | ND | ||||
| 18 | 10-2 | Persimmon 2 | Enterobacter spp. | + | + | + | AmpC-CS (ACT) CMAE | ||
| 19 | 10-3 | Citrobacter spp. | + | + | + | AmpC-CS (ND) CMAEnv | |||
| 20 | 11-1 | # Kiwi | Pseudomonas spp. | + | + | + | AmpC-CS (ND) AmpCnv | ||
| 21 | 11-3 | Rahnella aquatilis | + | + | CTX-M (RANH-2, ESBL) | ||||
| 22 | 12-1 | Pear 2 | Kosakonia spp. | + | ND | ||||
| 23 | 12-2 | Kosakonia spp. | + | ND | |||||
| 24 | 12-3 | ND | + | ND | |||||
| 25 | 14-1 | Tomato 2 | Pseudomonas spp. | + | + | + | ND | ||
| 26 | 14-2 | Pantoea ananatis | + | + | ND | ||||
| 27 | 14-3 | Pantoea ananatis | + | + | ND | ||||
| 28 | 17-1 | Potato 1 | Klebsiella pneumoniae | + | SHV-1v | ||||
| 29 | 18-1 | Cucumber 2 | Enterobacter cloacae | + | + | + | AmpC-CS (ACT) CMAE | ||
| 30 | 18-2 | Enterobacter spp. | + | + | TEM-1, AmpC-CS (ACT) ACT-32, intI1 | ||||
| 31 | 18-3 | Klebsiella pneumoniae | + | SHV-1v | |||||
| 32 | Single | Enterobacter spp. | + | AmpC-CS (ACT) AZECL-32 | |||||
| 33 | 19-1 | Tomato 3 | ND | + | ND | ||||
| 34 | 19-2 | ND | + | ND | |||||
| 35 | 19-3 | Enterobacter spp. | + | AmpC-CS (ACT) ACT-32 | |||||
| 36 | 20-2 | Potato 2 | Pseudomonas spp. | + | + | ND | |||
| 37 | 20-3 | Pseudomonas spp. | + | + | ND | ||||
| 38 | 21-1 | Green paprika 1 | ND | + | ND | ||||
| 39 | 21-2 | ND | + | ND | |||||
| 40 | 21-3 | Pseudomonas fulva | + | + | + | ND | |||
| 41 | 21-4 | Pseudomonas fulva | + | + | + | ND | |||
| 42 | 22-1 | Korean lettuce | Enterobacter spp. | + | + | + | + | AmpC-CS (ACT) ACT-51v | |
| 43 | 22-3 | Pseudomonas spp. | + | + | + | ND | |||
| 44 | 23-1 | Lettuce | Klebsiella pneumoniae | + | + | SHV-1 | |||
| 45 | 24-1 | # Gold kiwi | Enterobacter cloacae | + | + | + | AmpC-CS (ACT) CMAE | ||
| 46 | 24-2 | Enterobacter cloacae | + | + | + | AmpC-CS (ACT) CMAE | |||
| 47 | 24-3 | Enterobacter cloacae | + | AmpC-CS (ACT) CMAE | |||||
| 48 | 25-1 | Persimmon 3 | ND | + | ND | ||||
| 49 | 25-2 | Klebsiella pneumoniae | + | SHV-1v | |||||
| 50 | 25-3 | ND | + | ND | |||||
| 51 | 26-2 | Green paprika 2 | Pseudomonas spp. | + | + | + | + | ND | |
| 52 | 26-3 | Pseudomonas spp. | + | + | + | + | ND | ||
| 53 | 27-1 | Paprika | Enterobacter cloacae | + | + | + | AmpC-CS (ACT) CMAE | ||
| 54 | 27-2 | Pseudomonas putida | + | + | + | + | ND | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soliman, A.M.; Nariya, H.; Tanaka, D.; Shimamoto, T.; Shimamoto, T. A Novel Single-Tube Eicosaplex/Octaplex PCR System for the Detection of Extended-Spectrum β-Lactamases, Plasmid-Mediated AmpC β-Lactamases, and Integrons in Gram-Negative Bacteria. Antibiotics 2023, 12, 90. https://doi.org/10.3390/antibiotics12010090
Soliman AM, Nariya H, Tanaka D, Shimamoto T, Shimamoto T. A Novel Single-Tube Eicosaplex/Octaplex PCR System for the Detection of Extended-Spectrum β-Lactamases, Plasmid-Mediated AmpC β-Lactamases, and Integrons in Gram-Negative Bacteria. Antibiotics. 2023; 12(1):90. https://doi.org/10.3390/antibiotics12010090
Chicago/Turabian StyleSoliman, Ahmed M., Hirofumi Nariya, Daiki Tanaka, Toshi Shimamoto, and Tadashi Shimamoto. 2023. "A Novel Single-Tube Eicosaplex/Octaplex PCR System for the Detection of Extended-Spectrum β-Lactamases, Plasmid-Mediated AmpC β-Lactamases, and Integrons in Gram-Negative Bacteria" Antibiotics 12, no. 1: 90. https://doi.org/10.3390/antibiotics12010090
APA StyleSoliman, A. M., Nariya, H., Tanaka, D., Shimamoto, T., & Shimamoto, T. (2023). A Novel Single-Tube Eicosaplex/Octaplex PCR System for the Detection of Extended-Spectrum β-Lactamases, Plasmid-Mediated AmpC β-Lactamases, and Integrons in Gram-Negative Bacteria. Antibiotics, 12(1), 90. https://doi.org/10.3390/antibiotics12010090







