The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults
Abstract
1. Introduction
2. Prevalence and Mode of Transmission
3. Pathogenesis
4. Clinical Manifestations and Diagnosis
5. Diagnostic Methods in H. pylori Infection
5.1. Noninvasive Diagnostic Tests
5.1.1. Urea Breath Test
5.1.2. Stool Antigen Test
5.1.3. Serological Tests
5.1.4. Polymerase Chain Reaction
5.2. Invasive Tests
5.2.1. Endoscopy
5.2.2. Histological Examination
5.2.3. The Rapid Test with Urease
5.2.4. Microbiological Culture
5.2.5. Polymerase Chain Reaction
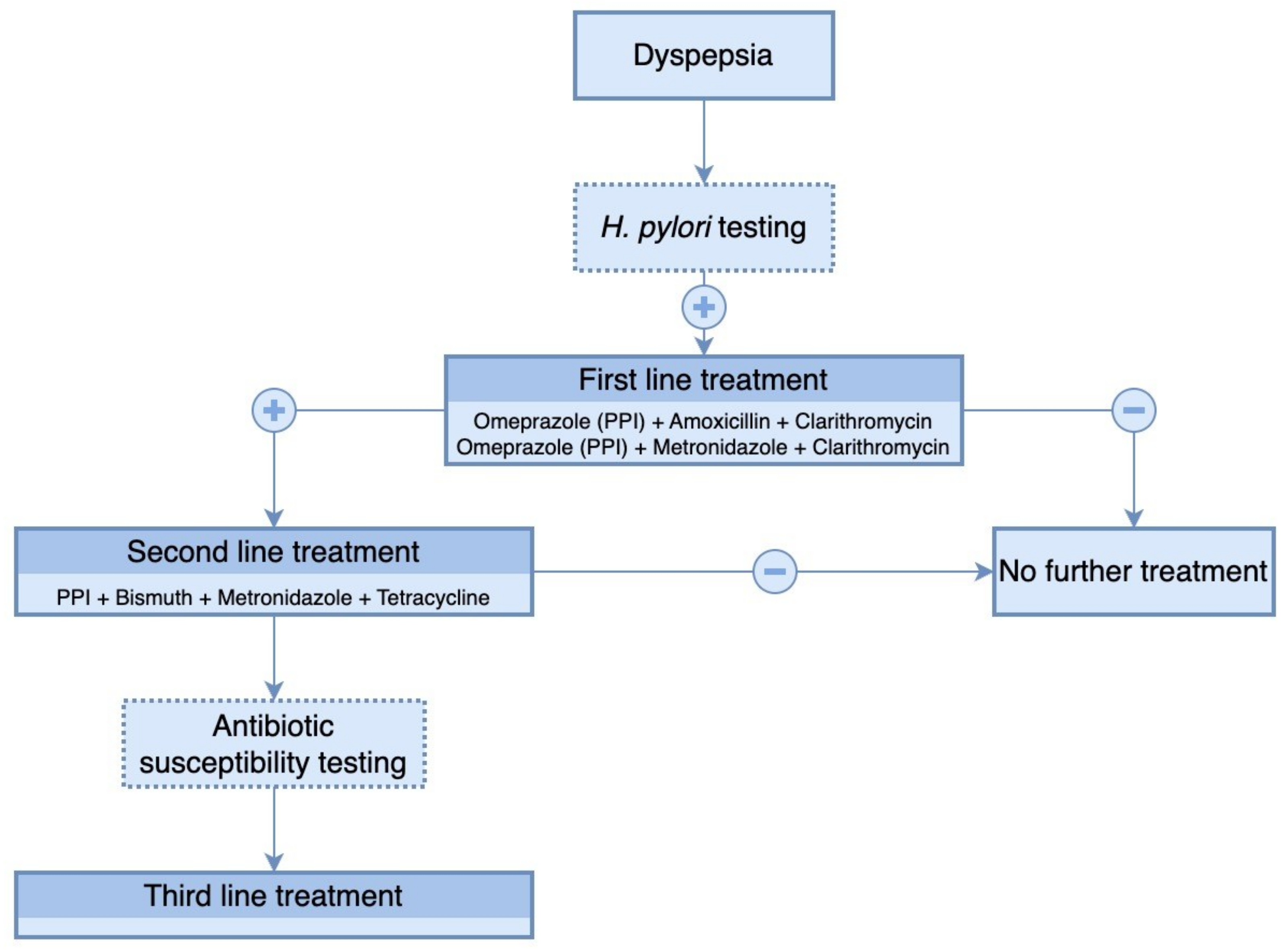
6. Therapeutic Management
6.1. Antibiotic Resistance of H. pylori
6.2. Probiotics
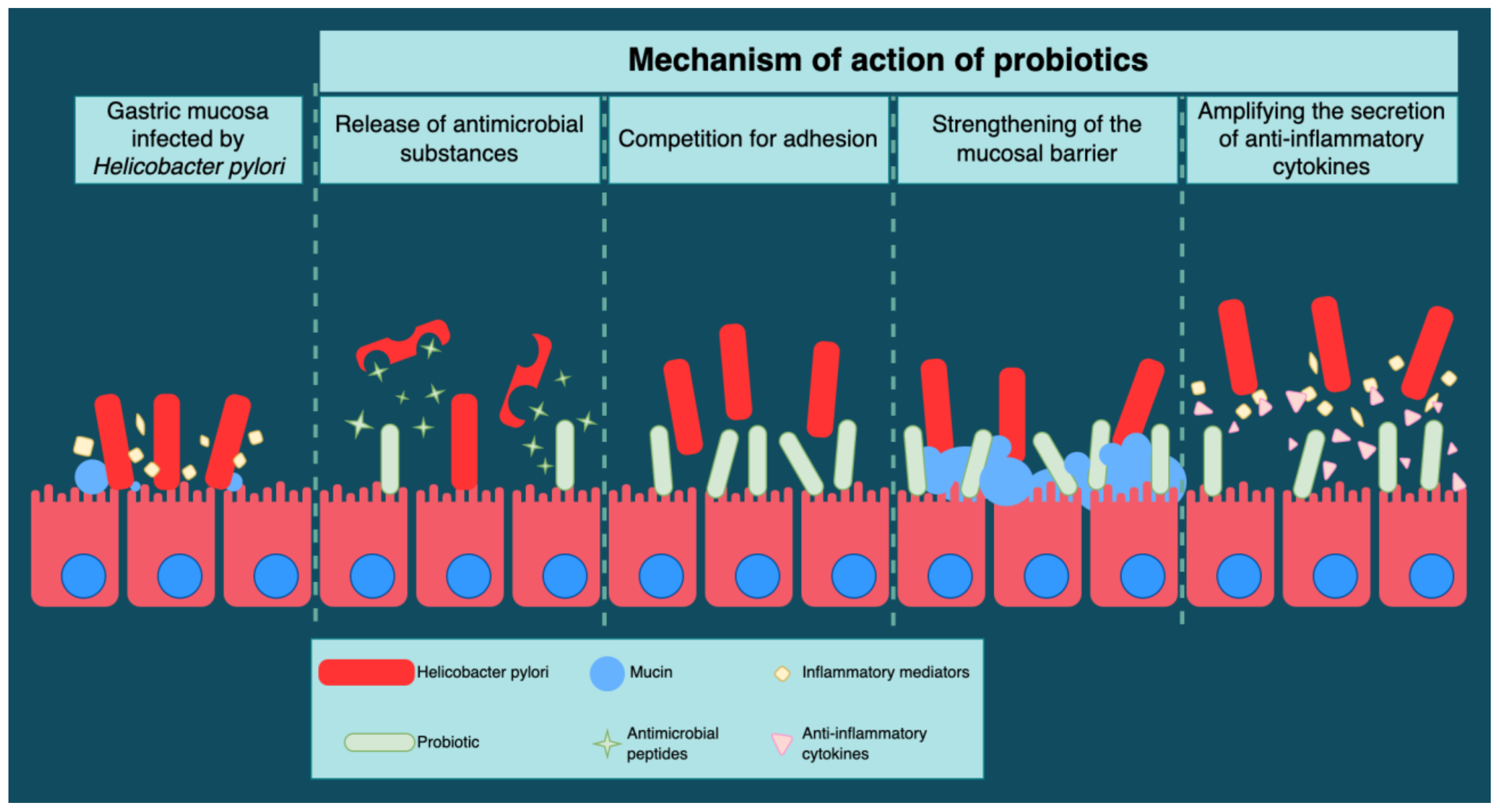
6.3. Mechanism of Action of Probiotics
6.3.1. Non-Immunological Mechanism
Antimicrobial Substances
Competition for Adhesion
The Mucosal Barrier
6.3.2. Immunological Mechanisms
6.4. Efficacity of Different Probiotics
7. Particular Aspects of H. pylori Infection in Pediatric Patients
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moodley, Y.; Linz, B.; Bond, R.P.; Nieuwoudt, M.; Soodyall, H.; Schlebusch, C.M.; Bernhöft, S.; Hale, J.; Suerbaum, S.; Mugisha, L.; et al. Age of the Association between Helicobacter pylori and Man. PLoS Pathog. 2012, 8, e1002693. [Google Scholar] [CrossRef] [PubMed]
- Marshall, B.J.; Warren, J.R. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet 1984, 1, 1311–1315. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Zhu, Y.; Lu, N.-H. Novel and Effective Therapeutic Regimens for Helicobacter pylori in an Era of Increasing Antibiotic Resistance. Front. Cell. Infect. Microbiol. 2017, 7, 168. [Google Scholar] [CrossRef] [PubMed]
- Peleteiro, B.; Bastos, A.; Ferro, A.; Lunet, N. Prevalence of Helicobacter pylori Infection Worldwide: A Systematic Review of Studies with National Coverage. Dig. Dis. Sci. 2014, 59, 1698–1709. [Google Scholar] [CrossRef]
- Urita, Y.; Watanabe, T.; Kawagoe, N.; Takemoto, I.; Tanaka, H.; Kijima, S.; Kido, H.; Maeda, T.; Sugasawa, Y.; Miyazaki, T.; et al. Role of infected grandmothers in transmission of Helicobacter pylori to children in a Japanese rural town. J. Paediatr. Child Health 2013, 49, 394–398. [Google Scholar] [CrossRef]
- Goh, K.-L.; Chan, W.-K.; Shiota, S.; Yamaoka, Y. Epidemiology of Helicobacter pylori Infection and Public Health Implications. Helicobacter 2011, 16 (Suppl. S1), 1–9. [Google Scholar] [CrossRef]
- Łaszewicz, W.; Iwańczak, F.; Iwańczak, B.; Annabhani, A.; Bała, G.; Bąk-Romaniszyn, L.; Budzyńska, A.; Cader, J.; Celiński, K.; Cichy, W.; et al. Seroprevalence of Helicobacter pylori infection in Polish children and adults depending on socioeconomic status and living conditions. Adv. Med. Sci. 2014, 59, 147–150. [Google Scholar] [CrossRef]
- Backert, S.; Clyne, M. Pathogenesis of Helicobacter pylori Infection. Helicobacter 2011, 16 (Suppl. S1), 19–25. [Google Scholar] [CrossRef]
- Abadi, A.T.B.; Ierardi, E.; Lee, Y.Y. Why do we still have Helicobacter Pylori in our Stomachs. Malays. J. Med. Sci. 2015, 22, 70–75. [Google Scholar]
- Yamaoka, Y. How to eliminate gastric cancer-related death worldwide? Nat. Rev. Clin. Oncol. 2018, 15, 407–408. [Google Scholar] [CrossRef]
- Plummer, M.; Franceschi, S.; Vignat, J.; Forman, D.; De Martel, C. Global burden of gastric cancer attributable to Helicobacter pylori. Int. J. Cancer 2015, 136, 487–490. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Chiang, T.-H.; Chou, C.-K.; Tu, Y.-K.; Liao, W.-C.; Wu, M.-S.; Graham, D.Y. Association Between Helicobacter pylori Eradication and Gastric Cancer Incidence: A Systematic Review and Meta-analysis. Gastroenterology 2016, 150, 1113–1124.e5. [Google Scholar] [CrossRef] [PubMed]
- Choi, I.J.; Kook, M.-C.; Kim, Y.-I.; Cho, S.-J.; Lee, J.Y.; Kim, C.G.; Park, B.; Nam, B.-H. Helicobacter pylori Therapy for the Prevention of Metachronous Gastric Cancer. N. Engl. J. Med. 2018, 378, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Pimentel-Nunes, P.; Libânio, D.; Marcos-Pinto, R.; Areia, M.; Leja, M.; Esposito, G.; Garrido, M.; Kikuste, I.; Megraud, F.; Matysiak-Budnik, T.; et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy 2019, 51, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Venerito, M.; Schulz, C. Helicobacter pylori Infection: New Facts in Clinical Management. Curr. Treat. Options Gastroenterol. 2018, 16, 605–615. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori infection—The Maastricht IV/Florence Consensus Report. Gut 2012, 61, 646–664. [Google Scholar] [CrossRef]
- Liu, L.; Gao, H.; Wang, H.; Zhu, K.; Yu, W.; Zhang, Y.; Guo, J. Comparison of Esophageal Function Tests to Investigate the Effect of Helicobacter Pylori Infection on Gastroesophageal Reflux Disease (GERD). J. Pharmacol. Exp. Ther. 2018, 24, 4791–4797. [Google Scholar] [CrossRef]
- Gravina, A.G.; Zagari, R.M.; De Musis, C.; Romano, L.; Loguercio, C.; Romano, M. Helicobacter pylori and extragastric diseases: A review. World J. Gastroenterol. 2018, 24, 3204–3221. [Google Scholar] [CrossRef]
- Wang, Y.K.; Kuo, F.C.; Liu, C.J.; Wu, M.C.; Shih, H.Y.; Wang, S.S.; Wu, J.Y.; Kuo, C.H.; Huang, Y.K.; Wu, D.C. Diagnosis of Helicobacter pylori infection: Current options and developments. World J. Gastroenterol. 2015, 21, 11221–11235. [Google Scholar] [CrossRef]
- Guarner, J.; Kalach, N.; Elitsur, Y.; Koletzko, S. Helicobacter pylori diagnostic tests in children: Review of the literature from 1999 to 2009. Eur. J. Pediatr. 2010, 169, 15–25. [Google Scholar] [CrossRef]
- Ferwana, M.; Abdulmajeed, I.; Alhajiahmed, A.; Madani, W.; Firwana, B.; Hasan, R.; Altayar, O.; Limburg, P.J.; Murad, M.H.; Knawy, B. Accuracy of urea breath test in Helicobacter pylori infection: Meta-analysis. World J. Gastroenterol. 2015, 21, 1305–1314. [Google Scholar] [CrossRef] [PubMed]
- Gisbert, J.P.; De La Morena, F.; Abraira, V. Accuracy of monoclonal stool antigen test for the diagnosis of H. pylori infection: A systematic review and meta-analysis. Am. J. Gastroenterol. 2006, 101, 1921–1930. [Google Scholar] [CrossRef] [PubMed]
- Demirtürk, L.; Yazgan, Y.; Tarçın, O.; Özel, M.; Diler, M.; Öncül, O.; Yıldırım, Ş. Does N-acetyl cystein affect the sensitivity and specificity of Helicobacter pylori stool antigen test? Helicobacter 2003, 8, 120–123. [Google Scholar] [CrossRef]
- Shimoyama, T. Stool antigen tests for the management of Helicobacter pylori infection. World J. Gastroenterol. 2013, 19, 8188–8191. [Google Scholar] [CrossRef] [PubMed]
- Pan, K.F.; Formichella, L.; Zhang, L.; Zhang, Y.; Ma, J.L.; Li, Z.X.; Liu, C.; Wang, Y.M.; Goettner, G.; Ulm, K.; et al. Helicobacter pylori antibody responses and evolution of precancerous gastric lesions in a Chinese population. Int. J. Cancer 2014, 134, 2118–2125. [Google Scholar] [CrossRef] [PubMed]
- Karami, N.; Talebkhan, Y.; Saberi, S.; Esmaeili, M.; Oghalaie, A.; Abdirad, A.; Mostafavi, E.; Hosseini, M.E.; Mohagheghi, M.A.; Mohammadi, M. Seroreactivity to Helicobacter pylori Antigens as a Risk Indicator of Gastric Cancer. Asian Pac. J. Cancer Prev. 2013, 14, 1813–1817. [Google Scholar] [CrossRef] [PubMed]
- Sicinschi, L.A.; Correa, P.; Bravo, L.E.; Peek, R.M.; Wilson, K.T.; Loh, J.T.; Yepez, M.C.; Gold, B.D.; Thompson, D.T.; Cover, T.L.; et al. Non-invasive Genotyping of Helicobacter pylori cagA, vacA, and hopQ from Asymptomatic Children. Helicobacter 2012, 17, 96–106. [Google Scholar] [CrossRef]
- Xiong, L.J.; Tong, Y.; Wang, Z.; Mao, M. Detection of clarithromycin-resistant Helicobacter pylori by stool PCR in children: A comprehensive review of literature. Helicobacter 2013, 18, 89–101. [Google Scholar] [CrossRef]
- Ogaya, Y.; Nomura, R.; Watanabe, Y.; Nakano, K. Detection of Helicobacter pylori DNA in inflamed dental pulp specimens from Japanese children and adolescents. J. Med. Microbiol. 2015, 64, 117–123. [Google Scholar] [CrossRef]
- Cho, Y.-S.; Chae, H.-S.; Na Jang, S.; Kim, J.-S.; Son, H.S.; Kim, H.-K.; Kim, B.-W.; Han, S.-W.; Choi, K.-Y.; Lee, H.K.; et al. Comparison of the 13C-urea breath test and the endoscopic phenol red mucosal pH test in the quantification of Helicobacter pylori infection loading. Korean J. Intern. Med. 2008, 23, 134–139. [Google Scholar] [CrossRef]
- Hernández-Garcés, H.R.; Castellanos-González, V.V.; González-Fabián, L.; Infante-Velázquez, M.; Peña, K.; Andrain-Sierra, Y. Chromoendoscopy with red phenol in the diagnosis of Helicobacter pylori infection. Rev. Esp. Enferm. Dig. 2012, 104, 4–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ji, R.; Li, Y.Q.; Gu, X.M.; Yu, T.; Zuo, X.L.; Zhou, C.J. Confocal laser endomicroscopy for diagnosis of Helicobacter pylori infection: A prospective study. J. Gastroenterol. Hepatol. 2010, 25, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Vaira, D.; Vakil, N.; Gatta, L.; Ricci, C.; Perna, F.; Saracino, I.; Fiorini, G.; Holton, J. Accuracy of a new ultrafast rapid urease test to diagnose Helicobacter pylori infection in 1000 consecutive dyspeptic patients. Aliment. Pharm. 2010, 31, 331–338. [Google Scholar]
- Momtaz, H.; Souod, N.; Dabiri, H.; Sarshar, M. Study of Helicobacter pylori genotype status in saliva, dental plaques, stool and gastric biopsy samples. World J. Gastroenterol. 2012, 18, 2105–2111. [Google Scholar] [CrossRef] [PubMed]
- Lehours, P.; Mégraud, F. Helicobacter pylori molecular diagnosis. Expert Rev. Mol. Diagn. 2011, 11, 351–355. [Google Scholar] [CrossRef]
- Graham, D.Y.; Lee, Y.; Wu, M. Rational Helicobacter pylori Therapy: Evidence-Based Medicine Rather Than Medicine-Based Evidence. Clin. Gastroenterol. Hepatol. 2014, 12, 177–186.e3, Discussion e12–13. [Google Scholar] [CrossRef] [PubMed]
- Safavi, M.; Sabourian, R.; Foroumadi, A. Treatment of Helicobacter pylori infection: Current and future insights. World J. Clin. Cases 2016, 4, 5–19. [Google Scholar] [CrossRef]
- Pohl, D.; Keller, P.M.; Bordier, V.; Wagner, K. Review of current diagnostic methods and advances in Helicobacter pylori diagnostics in the era of next generation sequencing. World J. Gastroenterol. 2019, 25, 4629–4660. [Google Scholar] [CrossRef]
- Lai, Y.; Wei, W.; Du, Y.; Gao, J.; Li, Z. Biomaterials for Helicobacter pylori therapy: Therapeutic potential and future perspectives. Gut Microbes 2022, 14, 2120747. [Google Scholar] [CrossRef]
- Flores-Treviño, S.; Mendoza-Olazarán, S.; Bocanegra-Ibarias, P.; Maldonado-Garza, H.J.; Garza-González, E. Helicobacter pylori drug resistance: Therapy changes and challenges. Expert Rev. Gastroenterol. Hepatol. 2018, 12, 819–827. [Google Scholar] [CrossRef]
- Nguyen, C.T.; Davis, K.A.; Nisly, S.A.; Li, J. Treatment of Helicobacter pylori in Special Patient Populations. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2019, 39, 1012–1022. [Google Scholar] [CrossRef]
- Schubert, J.P.; Warner, M.S.; Rayner, C.K.; Roberts-Thomson, I.C.; Mangoni, A.A.; Costello, S.; Bryant, R.V. Increasing Helicobacter pylori clarithromycin resistance in Australia over 20 years. Intern. Med. J. 2022, 52, 1554–1560. [Google Scholar] [CrossRef] [PubMed]
- Federico, A.; Gravina, A.G.; Miranda, A.; Loguercio, C.; Romano, M. Eradication of Helicobacter pylori infection: Which regimen first? World J. Gastroenterol. 2014, 20, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Chey, W.D.; Leontiadis, G.I.; Howden, C.W.; Moss, S.F. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2017, 112, 212–239. [Google Scholar] [CrossRef] [PubMed]
- De Brito, B.B.; Da Silva, F.A.F.; Soares, A.S.; Pereira, V.A.; Santos, M.L.C.; Sampaio, M.M.; Neves, P.H.M.; De Melo, F.F. Pathogenesis and clinical management of Helicobacter pylori gastric infection. World J. Gastroenterol. 2019, 25, 5578–5589. [Google Scholar] [CrossRef] [PubMed]
- Testerman, T.L.; Morris, J. Beyond the stomach: An updated view of Helicobacter pylori pathogenesis, diagnosis, and treatment. World J. Gastroenterol. 2014, 20, 12781–12808. [Google Scholar] [CrossRef]
- Lü, M.; Yu, S.; Deng, J.; Yan, Q.; Yang, C.; Xia, G.; Zhou, X. Efficacy of Probiotic Supplementation Therapy for Helicobacter pylori Eradication: A Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2016, 11, e0163743. [Google Scholar] [CrossRef]
- Ruggiero, P. Use of probiotics in the fight against Helicobacter pylori. World J. Gastrointest. Pathophysiol. 2014, 5, 384–391. [Google Scholar] [CrossRef]
- Na Kim, M.; Kim, N.; Lee, S.H.; Park, Y.S.; Hwang, J.-H.; Kim, J.-W.; Jeong, S.-H.; Lee, D.H.; Kim, J.S.; Jung, H.C.; et al. The Effects of Probiotics on PPI-Triple Therapy for Helicobacter pylori Eradication. Helicobacter 2008, 13, 261–268. [Google Scholar] [CrossRef]
- Nista, E.C.; Candelli, M.; Cremonini, F.; Cazzato, I.A.; Zocco, M.A.; Franceschi, F.; Cammarota, G.; Gasbarrini, G.; Gasbarrini, A. Bacillus clausii therapy to reduce side-effects of anti-Helicobacter pylori treatment: Randomized, double-blind, placebo controlled trial. Aliment. Pharmacol. Ther. 2004, 20, 1181–1188. [Google Scholar] [CrossRef]
- Tong, J.L.; Ran, Z.H.; Shen, J.; Zhang, C.X.; Xiao, S.D. Meta-analysis: The effect of supplementation with probiotics on eradication rates and adverse events during Helicobacter pylori eradication therapy. Aliment. Pharmacol. Ther. 2007, 25, 155–168. [Google Scholar] [CrossRef] [PubMed]
- Zou, J.; Dong, J.; Yu, X. Meta-Analysis: Lactobacillus Containing Quadruple Therapy Versus Standard Triple First-Line Therapy for Helicobacter pylori Eradication. Helicobacter 2009, 14, 449–459. [Google Scholar] [CrossRef]
- Szajewska, H.; Horvath, A.; Piwowarczyk, A. Meta-analysis: The effects of Saccharomyces boulardii supplementation on Helicobacter pylori eradication rates and side effects during treatment. Aliment. Pharmacol. Ther. 2010, 32, 1069–1079. [Google Scholar] [CrossRef]
- Wang, Z.-H.; Gao, Q.-Y.; Fang, J.-Y. Meta-Analysis of the Efficacy and Safety of Lactobacillus-containing and Bifidobacterium-containing Probiotic Compound Preparation in Helicobacter pylori Eradication Therapy. J. Clin. Gastroenterol. 2013, 47, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Dang, Y.; Reinhardt, J.D.; Zhou, X.; Zhang, G. The Effect of Probiotics Supplementation on Helicobacter pylori Eradication Rates and Side Effects during Eradication Therapy: A Meta-Analysis. PLoS ONE 2014, 9, e111030. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.M.; Qian, W.; Qin, Y.Y.; He, J.; Zhou, Y.H. Probiotics in Helicobacter pylori eradication therapy: A systematic review and meta-analysis. World J. Gastroenterol. 2015, 21, 4345–4357. [Google Scholar] [CrossRef]
- Szajewska, H.; Horvath, A.; Kołodziej, M. Systematic review with meta-analysis: Saccharomyces boulardii supplementation and eradication of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2015, 41, 1237–1245. [Google Scholar] [CrossRef]
- McFarland, L.V.; Huang, Y.; Wang, L.; Malfertheiner, P. Systematic review and meta-analysis: Multi-strain probiotics as adjunct therapy for Helicobacter pylori eradication and prevention of adverse events. United Eur. Gastroenterol. J. 2016, 4, 546–561. [Google Scholar] [CrossRef]
- Yang, J.-C.; Lu, C.-W.; Lin, C.-J. Treatment of Helicobacter pylori infection: Current status and future concepts. World J. Gastroenterol. 2014, 20, 5283–5293. [Google Scholar] [CrossRef]
- Feng, J.-R.; Wang, F.; Qiu, X.; McFarland, L.V.; Chen, P.-F.; Zhou, R.; Liu, J.; Zhao, Q.; Li, J. Efficacy and safety of probiotic-supplemented triple therapy for eradication of Helicobacter pylori in children: A systematic review and network meta-analysis. Eur. J. Clin. Pharmacol. 2017, 73, 1199–1208. [Google Scholar] [CrossRef]
- Bhatia, S.J.; Kochar, N.; Abraham, P.; Nair, N.G.; Mehta, A.P. Lactobacillus acidophilus inhibits growth of Campylobacter pylori in vitro. J. Clin. Microbiol. 1989, 27, 2328–2330. [Google Scholar] [CrossRef] [PubMed]
- Aiba, Y.; Nakano, Y.; Koga, Y.; Takahashi, K.; Komatsu, Y. A highly acid-resistant novel strain of Lactobacillus johnsonii No. 1088 has antibacterial activity, including that against Helicobacter pylori, and inhibits gastrin-mediated acid production in mice. Microbiologyopen 2015, 4, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Mack, D.R.; Ahrne, S.; Hyde, L.; Wei, S.; Hollingsworth, M.A. Extracellular MUC3 mucin secretion follows adherence of Lactobacillus strains to intestinal epithelial cells in vitro. Gut 2003, 52, 827–833. [Google Scholar] [CrossRef]
- Hanisch, F.G.; Bonar, D.; Schloerer, N.; Schroten, H. Human Trefoil Factor 2 Is a Lectin That Binds α-GlcNAc-capped Mucin Glycans with Antibiotic Activity against Helicobacter pylori. J. Biol. Chem. 2014, 289, 27363–27375. [Google Scholar] [CrossRef]
- Wiese, M.; Eljaszewicz, A.; Andryszczyk, M.; Gronek, S.; Gackowska, L.; Kubiszewska, I.; Kaszewski, W.; Helmin-Basa, A.; Januszewska, M.; Motyl, I.; et al. Immunomodulatory effects of Lactobacillous plantarum and Helicobacter pylori CagA? on the expression of selected superficial molecules on monocyte and lymphocyte and the synthesis of cytokines in whole blood culture. J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2012, 63, 217–224. [Google Scholar]
- Emara, M.H.; Elhawari, S.A.; Yousef, S.; Radwan, M.I.; Abdel-Aziz, H.R. Emerging Role of Probiotics in the Management of Helicobacter Pylori Infection: Histopathologic Perspectives. Helicobacter 2016, 21, 3–10. [Google Scholar] [CrossRef]
- Jakobsson, H.E.; Jernberg, C.; Andersson, A.F.; Sjölund-Karlsson, M.; Jansson, J.K.; Engstrand, L. Short-Term Antibiotic Treatment Has Differing Long-Term Impacts on the Human Throat and Gut Microbiome. PLoS ONE 2010, 5, e9836. [Google Scholar] [CrossRef]
- Oh, B.; Kim, B.S.; Kim, J.W.; Kim, J.S.; Koh, S.J.; Kim, B.G.; Lee, K.L.; Chun, J. The Effect of Probiotics on Gut Microbiota during the Helicobacter pylori Eradication: Randomized Controlled Trial. Helicobacter 2016, 21, 165–174. [Google Scholar] [CrossRef]
- Guillemard, E.; Poirel, M.; Schäfer, F.; Quinquis, L.; Rossoni, C.; Keicher, C.; Wagner, F.; Szajewska, H.; Barbut, F.; Derrien, M.; et al. A Randomised, Controlled Trial: Effect of a Multi-Strain Fermented Milk on the Gut Microbiota Recovery after Helicobacter pylori Therapy. Nutrients 2021, 13, 3171. [Google Scholar] [CrossRef]
- Viazis, N.; Argyriou, K.; Kotzampassi, K.; Christodoulou, D.K.; Apostolopoulos, P.; Georgopoulos, S.D.; Liatsos, C.; Giouleme, O.; Koustenis, K.; Veretanos, C.; et al. A Four-Probiotics Regimen Combined with A Standard Helicobacter pylori-Eradication Treatment Reduces Side Effects and Increases Eradication Rates. Nutrients 2022, 14, 632. [Google Scholar] [CrossRef]
- Chen, M.J.; Chen, C.C.; Huang, Y.C.; Tseng, C.C.; Hsu, J.T.; Lin, Y.F.; Fang, Y.J.; Wu, M.S.; Liou, J.M.; Taiwan Gastrointestinal Disease; et al. The efficacy of Lactobacillus acidophilus and rhamnosus in the reduction of bacterial load of Helicobacter pylori and modification of gut microbiota-a double-blind, placebo-controlled, randomized trial. Helicobacter 2021, 26, e12857. [Google Scholar] [CrossRef] [PubMed]
- Helaly, G.H.; El-Afandy, N.M.; Hassan, A.A.; Dowidar, N.L.; Sharaf, S.M. Diagnostic Value of Housekeeping [glmM] Gene Expression in Antral Biopsies in Comparison to Rapid Urease Test and Histological Detection of Helicobacter Pylori Infection. Egypt. J. Med. Microbiol. 2009, 18, 119–130. [Google Scholar]
- Xu, C.; Wu, Y.; Xu, S. Association between Helicobacter pylori infection and growth outcomes in children: A meta-analysis. Helicobacter 2022, 27, e12861. [Google Scholar] [CrossRef]
- Mehdipour, A.; Chaboki, P.; Rasouli Asl, F.; Aghaali, M.; Sharifinejad, N.; Shams, S. Comparing the prevalence of Helicobacter pylori and virulence factors cagA, vacA, and dupA in supra-gingival dental plaques of children with and without dental caries: A case-control study. BMC Oral Health 2022, 22, 170. [Google Scholar] [CrossRef] [PubMed]
- Sruthi, M.A.; Mani, G.; Ramakrishnan, M.; Selvaraj, J. Dental caries as a source of Helicobacter pylori infection in children: An RT-PCR study. Int. J. Paediatr. Dent. 2023, 33, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Spee, L.A.A.; Madderom, M.B.; Pijpers, M.; Van Leeuwen, Y.; Berger, M.Y. Association Between Helicobacter pylori and Gastrointestinal Symptoms in Children. Pediatrics 2010, 125, e651–e669. [Google Scholar] [CrossRef] [PubMed]
- Kolasa-Kicińska, M.; Stawerska, R.; Stawerski, P.; Kałużyński, A.; Czkwianianc, E.; Lewiński, A. Effects of Helicobacter pylori Infection on Ghrelin and Insulin-like Growth Factor 1 Secretion in Children with Idiopathic Short Stature. J. Clin. Med. 2022, 11, 5868. [Google Scholar] [CrossRef]
- Lupu, A.; Miron, I.C.; Cianga, A.L.; Cernomaz, A.T.; Lupu, V.V.; Munteanu, D.; Ghica, D.C.; Fotea, S. The Relationship between Anemia and Helicobacter Pylori Infection in Children. Children 2022, 9, 1324. [Google Scholar] [CrossRef]
- Wu, X.; Wang, W.; Fang, L.; Shi, L.; Rao, X. Is Helicobacter pylori colonization associated with chronic tonsillitis?—A meta-analysis and systematic review. Am. J. Otolaryngol. 2022, 43, 103515. [Google Scholar] [CrossRef]
- Yue, M.; Chen, Q.; Zhou, X.; Li, L.; Lu, C. Is Helicobacter pylori Infection Associated with Celiac Disease? A Meta-analysis. Turk. J. Gastroenterol. 2022, 33, 205–212. [Google Scholar] [CrossRef]
- Wang, D.; Chen, Y.; Ding, Y.; Tu, J. Inverse association between Helicobacter pylori infection and childhood asthma in a physical examination population: A cross-sectional study in Chongqing, China. BMC Pediatr. 2022, 22, 615. [Google Scholar] [CrossRef] [PubMed]
- Jones, N.L.; Koletzko, S.; Goodman, K.; Bontems, P.; Cadranel, S.; Casswall, T.; Czinn, S.; Gold, B.D.; Guarner, J.; Elitsur, Y.; et al. Joint ESPGHAN/NASPGHAN Guidelines for the Management of Helicobacter pylori in Children and Adolescents (Update 2016). J. Craniofacial Surg. 2017, 64, 991–1003. [Google Scholar] [CrossRef] [PubMed]
- Dimitrov, G.; Gottrand, F. Does gastric atrophy exist in children? World J. Gastroenterol. 2006, 12, 6274–6279. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, P.; Mohammadnia-Afrouzi, M.; Javanian, M.; Babazadeh, A.; Koppolu, V.; Vasigala, V.R.; Nouri, H.R.; Ebrahimpour, S. Diagnostic methods for Helicobacter pylori infection: Ideals, options, and limitations. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Kayali, S.; Manfredi, M.; Gaiani, F.; Bianchi, L.; Bizzarri, B.; Leandro, G.; Di Mario, F.; Angelis, G.L.D. Helicobacter pylori, transmission routes and recurrence of infection: State of the art. Acta Biomed. 2018, 89, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Leal, Y.A.; Flores, L.L.; Fuentes-Pananá, E.M.; Cedillo-Rivera, R.; Torres, J. 13C-Urea Breath Test for the Diagnosis of Helicobacter pylori Infection in Children: A Systematic Review and Meta-Analysis. Helicobacter 2011, 16, 327–337. [Google Scholar] [CrossRef]
- Leal, Y.A.; Cedillo-Rivera, R.; Simón, J.A.; Velazquez, J.; Flores, L.L.; Torres, J. Utility of Stool Sample–based Tests for the Diagnosis of Helicobacter pylori Infection in Children. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 718–728. [Google Scholar] [CrossRef]
- Zhang, S.; Zhang, Y.; Chen, S.; Teng, Y.; Li, C. Effects of inflammatory cytokines on eradication and recurrence of Helicobacter pylori infection in children. Pak. J. Med. Sci. 2022, 38, 1883–1887. [Google Scholar] [CrossRef]
- O’Ryan, M.L.; Lucero, Y.; Rabello, M.; Mamani, N.; Salinas, A.M.; Peña, A.; Torres-Torreti, J.P.; Mejías, A.; Ramilo, O.; Suarez, N.; et al. Persistent and TransientHelicobacter pyloriInfections in Early Childhood. Clin. Infect. Dis. 2015, 61, 211–218. [Google Scholar] [CrossRef]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Megraud, F.; Coenen, S.; Versporten, A.; Kist, M.; Lopez-Brea, M.; Hirschl, A.M.; Andersen, L.P.; Goossens, H.; Glupczynski, Y.; Study Group participants. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut 2013, 62, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Fang, H.-R.; Zhang, G.-Q.; Cheng, J.-Y.; Li, Z.-Y. Efficacy of Lactobacillus-supplemented triple therapy for Helicobacter pylori infection in children: A meta-analysis of randomized controlled trials. Eur. J. Pediatr. 2019, 178, 7–16. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marginean, C.M.; Cioboata, R.; Olteanu, M.; Vasile, C.M.; Popescu, M.; Popescu, A.I.S.; Bondari, S.; Pirscoveanu, D.; Marginean, I.C.; Iacob, G.A.; et al. The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults. Antibiotics 2023, 12, 60. https://doi.org/10.3390/antibiotics12010060
Marginean CM, Cioboata R, Olteanu M, Vasile CM, Popescu M, Popescu AIS, Bondari S, Pirscoveanu D, Marginean IC, Iacob GA, et al. The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults. Antibiotics. 2023; 12(1):60. https://doi.org/10.3390/antibiotics12010060
Chicago/Turabian StyleMarginean, Cristina Maria, Ramona Cioboata, Mihai Olteanu, Corina Maria Vasile, Mihaela Popescu, Alin Iulian Silviu Popescu, Simona Bondari, Denisa Pirscoveanu, Iulia Cristina Marginean, George Alexandru Iacob, and et al. 2023. "The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults" Antibiotics 12, no. 1: 60. https://doi.org/10.3390/antibiotics12010060
APA StyleMarginean, C. M., Cioboata, R., Olteanu, M., Vasile, C. M., Popescu, M., Popescu, A. I. S., Bondari, S., Pirscoveanu, D., Marginean, I. C., Iacob, G. A., Popescu, M. D., Stanciu, M., & Mitrut, P. (2023). The Importance of Accurate Early Diagnosis and Eradication in Helicobacter pylori Infection: Pictorial Summary Review in Children and Adults. Antibiotics, 12(1), 60. https://doi.org/10.3390/antibiotics12010060







