Antibiotic Resistance and Therapeutic Efficacy of Helicobacter pylori Infection in Pediatric Patients—A Tertiary Center Experience
Abstract
1. Introduction
2. Material and Methods
2.1. Patients Selection
2.2. Upper Gastrointestinal Endoscopy
2.3. Helicobacter pylori Cultures and Antibiotic Susceptibility Testing
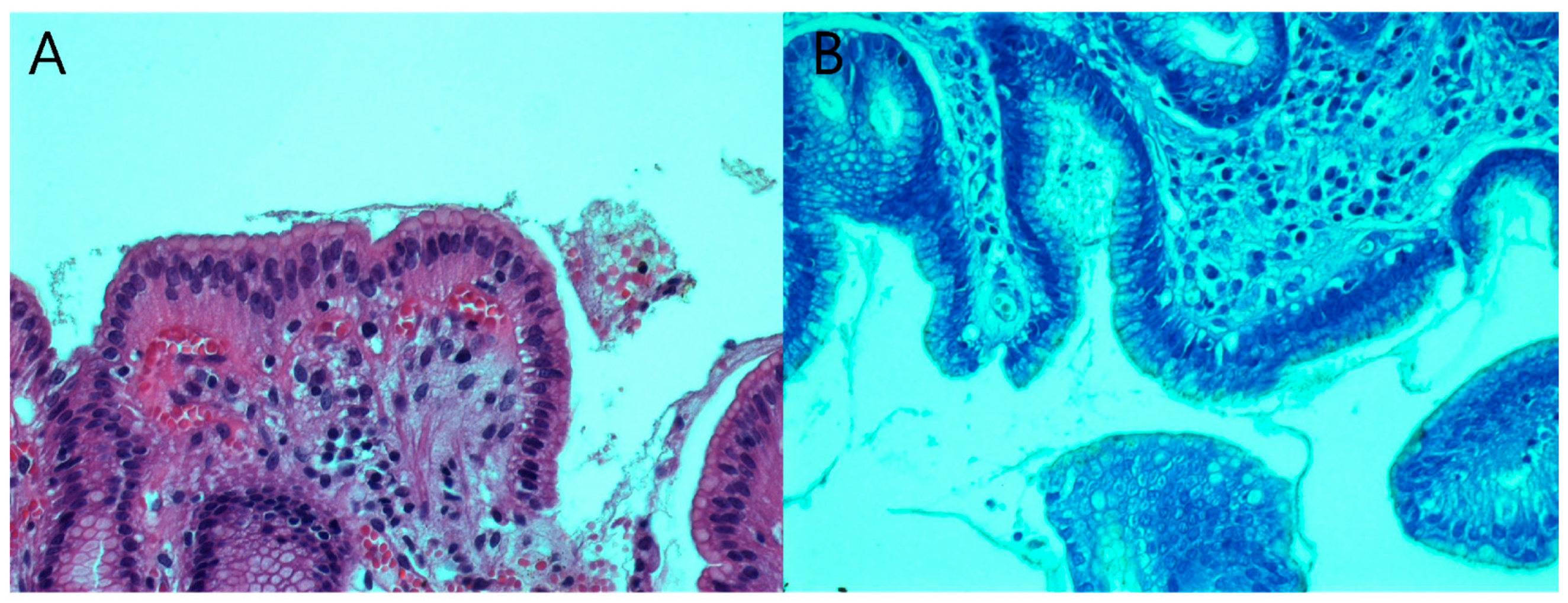
2.4. Histopathological Examination
2.5. Therapeutic Regimens
2.6. Data Analysis
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Marshall, B.J.; Armstrong, J.A.; McGechie, D.B.; Clancy, R.J. Attempt to Fulfil Koch’s Postulates for Pyloric Campylobacter. Med. J. Aust. 1985, 142, 436–439. [Google Scholar] [CrossRef] [PubMed]
- Parkin, D.M.; Bray, F.; Ferlay, J.; Pisani, P. Global Cancer Statistics, 2002. CA Cancer J. Clin. 2005, 55, 74–108. [Google Scholar] [CrossRef] [PubMed]
- IARC. Schistosomes, Liver Flukes and Helicobacter pylori. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; IARC Working Group on the Evaluation of Carcinogenic Risks to Humans; IARC: Lyon, France, 1994; Volume 61, pp. 1–241. [Google Scholar]
- WHO. Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 12 August 2022).
- Suerbaum, S.; Michetti, P. Helicobacter pylori Infection. N. Engl. J. Med. 2002, 347, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Drumm, B.; Day, A.S.; Gold, B.; Gottrand, F.; Kato, S.; Kawakami, E.; Madrazo, A.; Snyder, J.; Thomas, J. Helicobacter pylori and Peptic Ulcer: Working Group Report of the Second World Congress of Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2004, 39 (Suppl. 2), S626–S631. [Google Scholar] [CrossRef] [PubMed]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef]
- Olar, L.; MitruŢ, P.; Florou, C.; Mălăescu, G.D.; Predescu, O.I.; Rogozea, L.M.; Mogoantă, L.; Ionovici, N.; Pirici, I. Evaluation of Helicobacter pylori Infection in Patients with Eso-Gastro-Duodenal Pathology. Rom. J. Morphol. Embryol. 2017, 58, 809–815. [Google Scholar]
- Corojan, A.L.; Dumitrașcu, D.-L.; Ciobanca, P.; Leucuta, D.-C. Prevalence of Helicobacter Pylori Infection among Dyspeptic Patients in Northwestern Romania: A Decreasing Epidemiological Trend in the Last 30 Years. Exp. Ther. Med. 2020, 20, 3488–3492. [Google Scholar] [CrossRef]
- Mărginean, C.O.; Cotoi, O.S.; Pitea, A.M.; Mocanu, S.; Mărginean, C. Assessment of the Relationship between Helicobacter Pylori Infection, Endoscopic Appearance and Histological Changes of the Gastric Mucosa in Children with Gastritis (a Single Center Experience). Rom. J. Morphol. Embryol. 2013, 54, 709–715. [Google Scholar]
- Domșa, A.-M.T.; Lupușoru, R.; Gheban, D.; Șerban, R.; Borzan, C.M. Helicobacter Pylori Gastritis in Children—The Link between Endoscopy and Histology. J. Clin. Med. 2020, 9, 784. [Google Scholar] [CrossRef]
- Pacifico, L.; Anania, C.; Osborn, J.F.; Ferraro, F.; Chiesa, C. Consequences of Helicobacter pylori Infection in Children. World J. Gastroenterol. 2010, 16, 5181–5194. [Google Scholar] [CrossRef]
- Cho, J.; Prashar, A.; Jones, N.L.; Moss, S.F. Helicobacter pylori Infection. Gastroenterol. Clin. N. Am. 2021, 50, 261–282. [Google Scholar] [CrossRef]
- Ertem, D. Clinical Practice: Helicobacter pylori Infection in Childhood. Eur. J. Pediatr. 2013, 172, 1427–1434. [Google Scholar] [CrossRef]
- Jones, N.L.; Koletzko, S.; Goodman, K.; Bontems, P.; Cadranel, S.; Casswall, T.; Czinn, S.; Gold, B.D.; Guarner, J.; Elitsur, Y.; et al. Joint ESPGHAN/NASPGHAN Guidelines for the Management of Helicobacter pylori in Children and Adolescents (Update 2016). J. Pediatr. Gastroenterol. Nutr. 2017, 64, 991–1003. [Google Scholar] [CrossRef]
- Dixon, M.F.; Genta, R.M.; Yardley, J.H.; Correa, P. Classification and Grading of Gastritis. The Updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am. J. Surg. Pathol. 1996, 20, 1161–1181. [Google Scholar] [CrossRef]
- Sipponen, P.; Price, A.B. The Sydney System for Classification of Gastritis 20 Years Ago. J. Gastroenterol. Hepatol. 2011, 26 (Suppl. 1), 31–34. [Google Scholar] [CrossRef]
- Kalach, N.; Bontems, P.; Cadranel, S. Advances in the Treatment of Helicobacter Pylori Infection in Children. Ann. Gastroenterol. 2015, 28, 10–18. [Google Scholar]
- Mégraud, F.; Lehours, P. Helicobacter Pylori Detection and Antimicrobial Susceptibility Testing. Clin. Microbiol. Rev. 2007, 20, 280–322. [Google Scholar] [CrossRef]
- Mégraud, F. H Pylori Antibiotic Resistance: Prevalence, Importance, and Advances in Testing. Gut 2004, 53, 1374–1384. [Google Scholar] [CrossRef]
- Botija, G.; García Rodríguez, C.; Recio Linares, A.; Campelo Gutiérrez, C.; Pérez-Fernández, E.; Barrio Merino, A. Antibiotic Resistances and Eradication Rates in Helicobacter pylori Infection. An. Pediatr. 2021, 95, 431–437. [Google Scholar] [CrossRef]
- Gong, E.J.; Kim, D.H.; Ahn, J.Y.; Na, H.K.; Jung, K.W.; Lee, J.H.; Choi, K.D.; Song, H.J.; Lee, G.H.; Jung, H.-Y.; et al. Effects of Proton Pump Inhibitor on the Distribution of Helicobacter pylori and Associated Gastritis in Patients with Gastric Atrophy. Digestion 2020, 101, 279–286. [Google Scholar] [CrossRef]
- Megraud, F.; Boyanova, L.; Lamouliatte, H. Activity of Lansoprazole against Helicobacter Pylori. Lancet 1991, 337, 1486. [Google Scholar] [CrossRef] [PubMed]
- Fallone, C.A.; Loo, V.G.; Lough, J.; Barkun, A.N. Hematoxylin and Eosin Staining of Gastric Tissue for the Detection of Helicobacter pylori. Helicobacter 1997, 2, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Alkhamiss, A.S. Evaluation of Better Staining Method among Hematoxylin and Eosin, Giemsa and Periodic Acid Schiff-Alcian Blue for the Detection of Helicobacter pylori in Gastric Biopsies. Malays. J. Med. Sci. 2020, 27, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Galoș, F.; Năstase, G.; Boboc, C.; Coldea, C.; Anghel, M.; Orzan, A.; Bălgrădean, M. A Study of the Correlation between Bacterial Culture and Histological Examination in Children with Helicobacter Pylori Gastritis; IntechOpen: London, UK, 2018; ISBN 978-1-78984-971-4. [Google Scholar]
- Sonnenberg, A.; Lash, R.H.; Genta, R.M. A National Study of Helicobactor Pylori Infection in Gastric Biopsy Specimens. Gastroenterology 2010, 139, 1894–1901.e2. [Google Scholar] [CrossRef] [PubMed]
- Zabala Torrres, B.; Lucero, Y.; Lagomarcino, A.J.; Orellana-Manzano, A.; George, S.; Torres, J.P.; O’Ryan, M. Review: Prevalence and Dynamics of Helicobacter pylori Infection during Childhood. Helicobacter 2017, 22, e12399. [Google Scholar] [CrossRef] [PubMed]
- Dong, B.N.; Graham, D.Y. Helicobacter pylori Infection and Antibiotic Resistance: A WHO High Priority? Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 383–384. [Google Scholar] [CrossRef]
- Megraud, F.; Bruyndonckx, R.; Coenen, S.; Wittkop, L.; Huang, T.-D.; Hoebeke, M.; Bénéjat, L.; Lehours, P.; Goossens, H.; Glupczynski, Y. Helicobacter pylori Resistance to Antibiotics in Europe in 2018 and Its Relationship to Antibiotic Consumption in the Community. Gut 2021, 70, 1815–1822. [Google Scholar] [CrossRef]
- Choi, I.J.; Kim, C.G.; Lee, J.Y.; Kim, Y.-I.; Kook, M.-C.; Park, B.; Joo, J. Family History of Gastric Cancer and Helicobacter pylori Treatment. N. Engl. J. Med. 2020, 382, 427–436. [Google Scholar] [CrossRef]
- Nishizawa, T.; Suzuki, H.; Sakitani, K.; Yamashita, H.; Yoshida, S.; Hata, K.; Kanazawa, T.; Fujiwara, N.; Kanai, T.; Yahagi, N.; et al. Family History Is an Independent Risk Factor for the Progression of Gastric Atrophy among Patients with Helicobacter pylori Infection. United Eur. Gastroenterol. J. 2017, 5, 32–36. [Google Scholar] [CrossRef]
- Yatsuya, H.; Toyoshima, H.; Tamakoshi, A.; Kikuchi, S.; Tamakoshi, K.; Kondo, T.; Mizoue, T.; Tokui, N.; Hoshiyama, Y.; Sakata, K.; et al. Individual and Joint Impact of Family History and Helicobacter pylori Infection on the Risk of Stomach Cancer: A Nested Case-Control Study. Br. J. Cancer 2004, 91, 929–934. [Google Scholar] [CrossRef]
- Galoș, F.; Boboc, C.; Năstase, G.; Orzan, A.; Coldea, C.; Anghel, M.; Bălgrădean, M. Endoscopical Aspects of Helicobacter Pylori Gastritis in Children; IntechOpen: London, UK, 2018; ISBN 978-1-83881-147-1. [Google Scholar]
- Ricci, C.; Holton, J.; Vaira, D. Diagnosis of Helicobacter Pylori: Invasive and Non-Invasive Tests. Best Pract. Res. Clin. Gastroenterol. 2007, 21, 299–313. [Google Scholar] [CrossRef]
- Genta, R.M.; Graham, D.Y. Comparison of Biopsy Sites for the Histopathologic Diagnosis of Helicobacter pylori: A Topographic Study of H. Pylori Density and Distribution. Gastrointest. Endosc. 1994, 40, 342–345. [Google Scholar] [CrossRef]
- Whitney, A.E.; Guarner, J.; Hutwagner, L.; Gold, B.D. Helicobacter pylori Gastritis in Children and Adults: Comparative Histopathologic Study. Ann. Diagn. Pathol. 2000, 4, 279–285. [Google Scholar] [CrossRef]
- Serrano, C.; Wright, S.W.; Bimczok, D.; Shaffer, C.L.; Cover, T.L.; Venegas, A.; Salazar, M.G.; Smythies, L.E.; Harris, P.R.; Smith, P.D. Down-Regulated Th17 Responses Are Associated with Reduced Gastritis in Helicobacter pylori-Infected Children. Mucosal Immunol. 2013, 6, 950–959. [Google Scholar] [CrossRef]
- Nardone, G.; Staibano, S.; Rocco, A.; Mezza, E.; Balzano, T.; Salvatore, G.; Staiano, A.; Donofrio, V.; Grazioli, B.; de Rosa, G.; et al. Effect of Helicobacter pylori Infection on Gastric Cell Proliferation and Genomic Instablity in a Paediatric Population of Southern Italy. Dig. Liver Dis. 2001, 33, 743–749. [Google Scholar] [CrossRef]
- Yang, H.R. Updates on the Diagnosis of Helicobacter pylori Infection in Children: What Are the Differences between Adults and Children? Pediatr. Gastroenterol. Hepatol. Nutr. 2016, 19, 96–103. [Google Scholar] [CrossRef]
- Mitchell, H.M.; Bohane, T.D.; Tobias, V.; Bullpitt, P.; Daskalopoulos, G.; Carrick, J.; Mitchell, J.D.; Lee, A. Helicobacter pylori Infection in Children: Potential Clues to Pathogenesis. J. Pediatr. Gastroenterol. Nutr. 1993, 16, 120–125. [Google Scholar] [CrossRef]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori Infection—The Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef]
- Kaya, A.D.; Oztürk, C.E.; Akcan, Y.; Behçet, M.; Karakoç, A.E.; Yücel, M.; Mısırlıoglu, M.; Tuncer, S. Prevalence of Helicobacter pylori in Symptomatic Patients and Detection of Clarithromycin Resistance Using Melting Curve Analysis. Curr. Ther. Res. 2007, 68, 151–160. [Google Scholar] [CrossRef]
- Ogata, S.K.; Kawakami, E.; Patrício, F.R.; Pedroso, M.Z.; Santos, A.M. Evaluation of Invasive and Non-Invasive Methods for the Diagnosis of Helicobacter pylori Infection in Symptomatic Children and Adolescents. Sao Paulo Med. J. 2001, 119, 67–71. [Google Scholar] [CrossRef]
- Cosgun, Y.; Yildirim, A.; Yucel, M.; Karakoc, A.E.; Koca, G.; Gonultas, A.; Gursoy, G.; Ustun, H.; Korkmaz, M. Evaluation of Invasive and Noninvasive Methods for the Diagnosis of Helicobacter pylori Infection. Asian Pac. J. Cancer Prev. 2016, 17, 5265–5272. [Google Scholar] [CrossRef] [PubMed]
- Saracino, I.M.; Zullo, A.; Holton, J.; Castelli, V.; Fiorini, G.; Zaccaro, C.; Ridola, L.; Ricci, C.; Gatta, L.; Vaira, D. High Prevalence of Primary Antibiotic Resistance in Helicobacter pylori Isolates in Italy. J. Gastrointest. Liver Dis. 2012, 21, 363–365. [Google Scholar]
- Patel, S.K.; Pratap, C.B.; Jain, A.K.; Gulati, A.K.; Nath, G. Diagnosis of Helicobacter pylori: What Should Be the Gold Standard? World J. Gastroenterol. 2014, 20, 12847–12859. [Google Scholar] [CrossRef] [PubMed]
- Kohli, Y.; Tanaka, Y.; Kato, T.; Ito, S. Endoscopic diagnosis of Helicobacter pylori distribution in human gastric mucosa by phenol red dye spraying method. Nihon Rinsho Jpn. J. Clin. Med. 1993, 51, 3182–3186. [Google Scholar]
- Bujanda, L.; Nyssen, O.P.; Vaira, D.; Saracino, I.M.; Fiorini, G.; Lerang, F.; Georgopoulos, S.; Tepes, B.; Heluwaert, F.; Gasbarrini, A.; et al. Antibiotic Resistance Prevalence and Trends in Patients Infected with Helicobacter pylori in the Period 2013–2020: Results of the European Registry on H. Pylori Management (Hp-EuReg). Antibiotics 2021, 10, 1058. [Google Scholar] [CrossRef]
- Saracino, I.M.; Pavoni, M.; Zullo, A.; Fiorini, G.; Saccomanno, L.; Lazzarotto, T.; Cavallo, R.; Antonelli, G.; Vaira, D. Antibiotic Resistance and Therapy Outcome in H. Pylori Eradication Failure Patients. Antibiotics 2020, 9, 121. [Google Scholar] [CrossRef]
- Pastukh, N.; Peretz, A.; Brodsky, D.; Isakovich, N.; Azrad, M.; On, A. Antimicrobial Susceptibility of Helicobacter pylori Strains Isolated from Children in Israel. J. Glob. Antimicrob. Resist. 2018, 12, 175–178. [Google Scholar] [CrossRef]
- Schwarzer, A.; Bontems, P.; Urruzuno, P.; Kalach, N.; Iwanczak, B.; Roma-Giannikou, E.; Sykora, J.; Kindermann, A.; Casswall, T.; Cadranel, S.; et al. Sequential Therapy for Helicobacter pylori Infection in Treatment-Naïve Children. Helicobacter 2016, 21, 106–113. [Google Scholar] [CrossRef]
- Matos, I.A.; Oliva, S.E.D.; Escobedo, A.A.; Jiménez, O.M.V.; Villaurrutia, Y.D.C.V. Helicobacter pylori Infection in Children. BMJ Paediatr. Open 2020, 4, e000679. [Google Scholar] [CrossRef]
- Bontems, P.; Kalach, N.; Oderda, G.; Salame, A.; Muyshont, L.; Miendje, D.Y.; Raymond, J.; Cadranel, S.; Scaillon, M. Sequential Therapy versus Tailored Triple Therapies for Helicobacter pylori Infection in Children. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 646–650. [Google Scholar] [CrossRef]
- Zullo, A.; Rinaldi, V.; Winn, S.; Meddi, P.; Lionetti, R.; Hassan, C.; Ripani, C.; Tomaselli, G.; Attili, A.F. A New Highly Effective Short-Term Therapy Schedule for Helicobacter pylori Eradication. Aliment. Pharmacol. Ther. 2000, 14, 715–718. [Google Scholar] [CrossRef]
- Su, D.-J.; Chang, M.-H.; Yang, J.-C.; Ni, Y.-H.; Hsu, H.-Y.; Wu, J.-F. Fourteen-Day Sequential Therapy Is Superior to 7-Day Triple Therapy as First-Line Regimen for Helicobacter pylori Infected Children. J. Formos. Med. Assoc. 2022, 121, 202–209. [Google Scholar] [CrossRef]

| Mean age ± SD, years | 11 years 7 months ± 4 years 5 months |
| Male/female | 24 (40.67%)/35 (59.32%) |
| Family history for H. pylori infection | 10/59 (16.94%) |
| Symptoms > 6 months | 26/59 (44.06%) |
| Previous therapy | 22/59 (37.28%) |
| Parameter | Normal Endoscopic Aspect | Pathological Endoscopic Aspect | p Value |
|---|---|---|---|
| Patients without previous therapies (37 patients) | 1/37 (2.70%) | 36/37 (97.29%) | 0.002 |
| Patients with previous therapies (22 patients) | 7/22 (31.81%) | 15/22 (68.18%) |
| Parameter | Low H. pylori Density | Moderate H. pylori Density | Marked H. pylori Density | p Value | |
|---|---|---|---|---|---|
| Positive H. pylori cultures (%) | 5/28 (17.85%) | 4/21 (19.04%) | 1/7 (14.28%) | 0.01 | |
| Activity of H. pylori gastritis | Without activity (%) | 7/28 (25%) | 1/21 (4.76%) | 1/7 (14.28%) | 0.03 |
| Mild activity (%) | 11/28 (39.2%) | 6/21 (28.57%) | 4/7 (57.14%) | ||
| Moderate activity (%) | 10/28 (35.7%) | 13/21 (61.9%) | 2/7 (28.57%) | ||
| Severe activity (%) | 0 | 1/21 (4.76%) | 0 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galoș, F.; Boboc, C.; Ieșanu, M.-I.; Anghel, M.; Ioan, A.; Iana, E.; Coșoreanu, M.T.; Boboc, A.A. Antibiotic Resistance and Therapeutic Efficacy of Helicobacter pylori Infection in Pediatric Patients—A Tertiary Center Experience. Antibiotics 2023, 12, 146. https://doi.org/10.3390/antibiotics12010146
Galoș F, Boboc C, Ieșanu M-I, Anghel M, Ioan A, Iana E, Coșoreanu MT, Boboc AA. Antibiotic Resistance and Therapeutic Efficacy of Helicobacter pylori Infection in Pediatric Patients—A Tertiary Center Experience. Antibiotics. 2023; 12(1):146. https://doi.org/10.3390/antibiotics12010146
Chicago/Turabian StyleGaloș, Felicia, Cătălin Boboc, Mara-Ioana Ieșanu, Mălina Anghel, Andreea Ioan, Elena Iana, Maria Teodora Coșoreanu, and Anca Andreea Boboc. 2023. "Antibiotic Resistance and Therapeutic Efficacy of Helicobacter pylori Infection in Pediatric Patients—A Tertiary Center Experience" Antibiotics 12, no. 1: 146. https://doi.org/10.3390/antibiotics12010146
APA StyleGaloș, F., Boboc, C., Ieșanu, M.-I., Anghel, M., Ioan, A., Iana, E., Coșoreanu, M. T., & Boboc, A. A. (2023). Antibiotic Resistance and Therapeutic Efficacy of Helicobacter pylori Infection in Pediatric Patients—A Tertiary Center Experience. Antibiotics, 12(1), 146. https://doi.org/10.3390/antibiotics12010146







