Genetic Polymorphisms Associated with Perioperative Joint Infection following Total Joint Arthroplasty: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Literature Search
2.3. Eligibility Criteria
2.4. Study Selection
2.5. Characteristics of Included Studies
2.6. Strengthening the Reporting of Genetic Association Studies (STREGA)
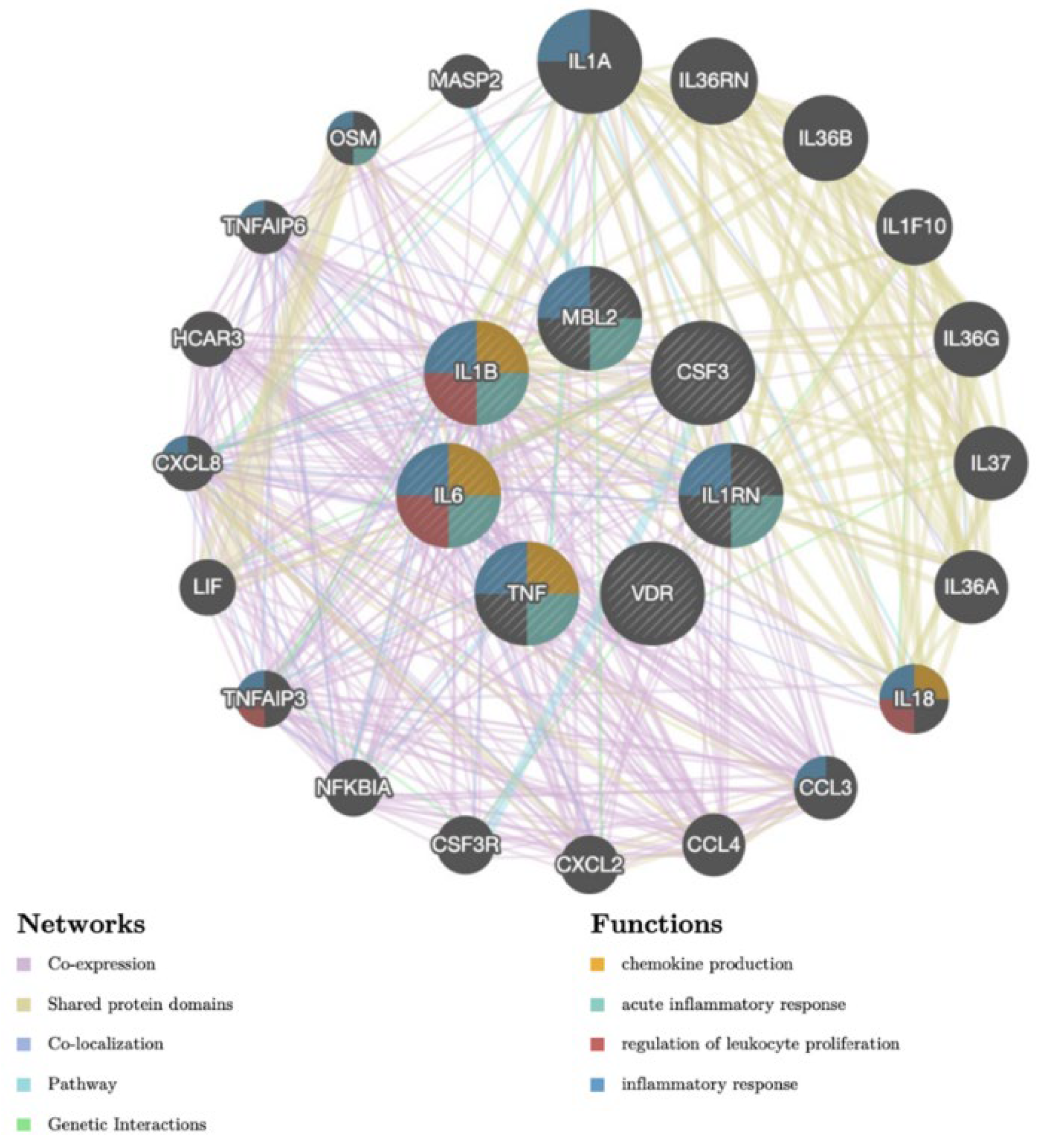
2.7. GeneMANIA: Genetic Pathways and Interactions of PJI
2.8. Meta-Analysis
3. Results
3.1. Literature Search
3.2. Study Characteristics
3.3. Quality Assessment of Studies
3.4. Interaction and Genetic Pathways of Prosthetic Joint Infection (GeneMANIA)
3.5. Systematic Review
3.5.1. Cytokines
3.5.2. Proteins and Enzymes
3.5.3. Receptors
3.5.4. RANK/RANKL/OPG Pathway
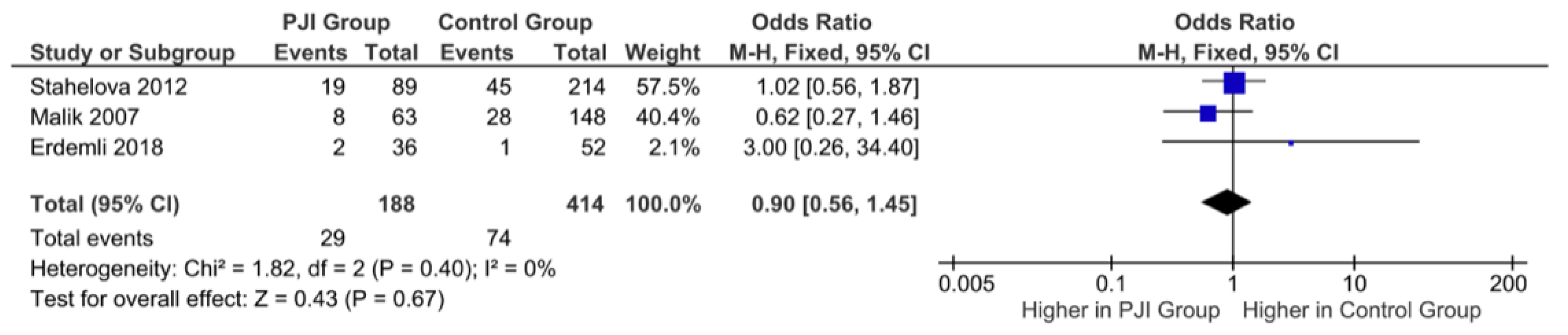
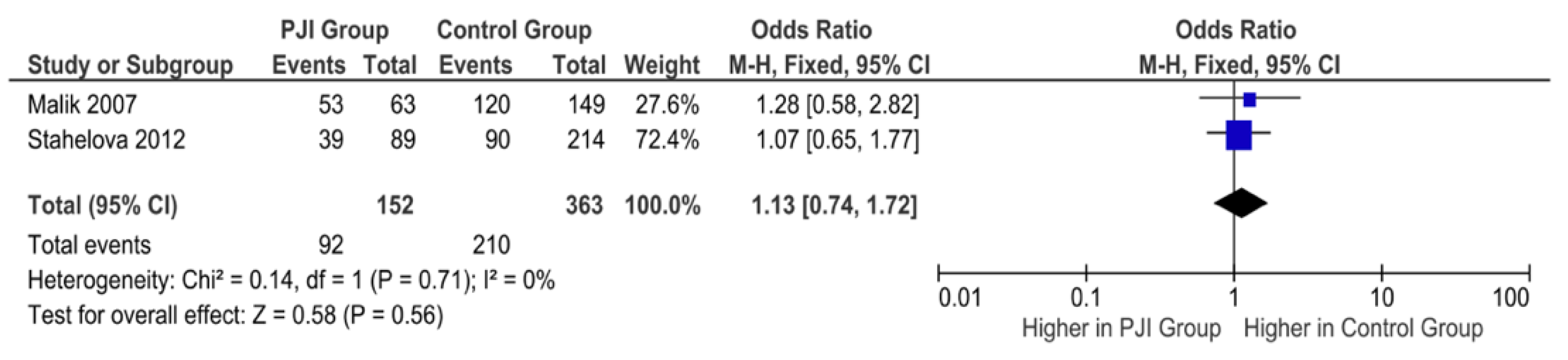
3.6. Meta-Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Mall, N.A.; Chalmers, P.N.; Moric, M.; Tanaka, M.J.; Cole, B.J.; Bach, B.R.; Paletta, G.A. Incidence and Trends of Anterior Cruciate Ligament Reconstruction in the United States. Am. J. Sports Med. 2014, 42, 2363–2370. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. Am. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Padegimas, E.M.; Maltenfort, M.; Lazarus, M.D.; Ramsey, M.L.; Williams, G.R.; Namdari, S. Future Patient Demand for Shoulder Arthroplasty by Younger Patients: National Projections. Clin. Orthop. Relat. Res. 2015, 473, 1860–1867. [Google Scholar] [CrossRef] [PubMed]
- Nichols, C.I.; Vose, J.G. Clinical Outcomes and Costs Within 90 Days of Primary or Revision Total Joint Arthroplasty. J. Arthroplast. 2016, 31, 1400–1406.e3. [Google Scholar] [CrossRef] [PubMed]
- Birkmeyer, J.D.; Gust, C.; Dimick, J.B.; Birkmeyer, N.J.O.; Skinner, J.S. Hospital Quality and the Cost of Inpatient Surgery in the United States. Ann. Surg. 2012, 255, 1–5. [Google Scholar] [CrossRef]
- Alp, E.; Cevahir, F.; Ersoy, S.; Guney, A. Incidence and economic burden of prosthetic joint infections in a university hospital: A report from a middle-income country. J. Infect. Public Health 2016, 9, 494–498. [Google Scholar] [CrossRef]
- Li, C.; Renz, N.; Trampuz, A. Management of Periprosthetic Joint Infection. Hip Pelvis 2018, 30, 138–146. [Google Scholar] [CrossRef]
- Bohl, D.D.; Samuel, A.M.; Basques, B.A.; Della Valle, C.J.; Levine, B.R.; Grauer, J.N. How Much Do Adverse Event Rates Differ Between Primary and Revision Total Joint Arthroplasty? J. Arthroplast. 2016, 31, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Bunn, K.J.; Isaacson, M.J.; Ismaily, S.K.; Noble, P.C.; Incavo, S.J. Quantifying and Predicting Surgeon Work Effort for Primary and Revision Total Knee Arthroplasty. J. Arthroplast. 2016, 31 (Suppl. 9), 59–62. [Google Scholar] [CrossRef]
- Isaacson, M.J.; Bunn, K.J.; Noble, P.C.; Ismaily, S.K.; Incavo, S.J. Quantifying and Predicting Surgeon Work Input in Primary vs Revision Total Hip Arthroplasty. J. Arthroplast. 2016, 31, 1188–1193. [Google Scholar] [CrossRef]
- Haenle, M.; Skripitz, C.; Mittelmeier, W.; Skripitz, R. Economic Impact of Infected Total Knee Arthroplasty. Sci. World J. 2012, 2012, 196515. [Google Scholar] [CrossRef] [PubMed]
- Medzhitov, R. Recognition of microorganisms and activation of the immune response. Nature 2007, 449, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.H.; Bayat, A.; Jury, F.; Kay, P.R.; Ollier, W.E. Genetic Susceptibility to Total Hip Arthroplasty Failure—Positive Association With Mannose-Binding Lectin. J. Arthroplast. 2007, 22, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.H.A.; Jury, F.; Bayat, A.; Ollier, W.E.R.; Kay, P.R. Genetic susceptibility to total hip arthroplasty failure: A preliminary study on the influence of matrix metalloproteinase 1, interleukin 6 polymorphisms and vitamin D receptor. Ann. Rheum. Dis. 2007, 66, 1116–1120. [Google Scholar] [CrossRef] [PubMed]
- Navratilova, Z.; Gallo, J.; Mrazek, F.; Lostak, J.; Petrek, M. MBL2gene variation affecting serum MBL is associated with prosthetic joint infection in Czech patients after total joint arthroplasty. Tissue Antigens 2012, 80, 444–451. [Google Scholar] [CrossRef]
- Turner, M.W. Mannose-binding lectin: The pluripotent molecule of the innate immune system. Immunol. Today 1996, 17, 532–540. [Google Scholar] [CrossRef]
- McCawley, L.J.; Matrisian, L.M. Matrix metalloproteinases: They’re not just for matrix anymore! Curr. Opin. Cell Biol. 2001, 13, 534–540. [Google Scholar] [CrossRef]
- Kawai, T.; Akira, S. Toll-like Receptors and Their Crosstalk with Other Innate Receptors in Infection and Immunity. Immunity 2011, 34, 637–650. [Google Scholar] [CrossRef]
- Walsh, M.C.; Choi, Y. Biology of the RANKL–RANK–OPG System in Immunity, Bone, and Beyond. Front. Immunol. 2014, 5, 511. [Google Scholar] [CrossRef]
- Erdemli, B.; Özbek, E.A.; Ba¸sarir, K.; Karahan, Z.C.; Öcal, D.; Biriken, D. Proinflammatory biomarkers’ level and functional genetic polymorphisms in periprosthetic joint infection. Acta Orthop. Traumatol. Turc. 2018, 52, 143–147. [Google Scholar] [CrossRef]
- Malik, M.H.A.; Bayat, A.; Jury, F.; Ollier, W.E.R.; Kay, P.R. Genetic susceptibility to hip arthroplasty failure—association with the RANK/OPG pathway. Int. Orthop. 2006, 30, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Stahelova, A.; Mrazek, F.; Smizansky, M.; Petrek, M.; Gallo, J. Variation in the IL1B, TNF and IL6 genes and individual susceptibility to prosthetic joint infection. BMC Immunol. 2012, 13, 25. [Google Scholar] [CrossRef] [PubMed]
- Mrazek, F.; Gallo, J.; Stahelova, A.; Petrek, M. Coding variants of TLR2 and TLR4 genes do not substantially contribute to prosthetic joint infection. Agents Actions 2013, 62, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Navratilova, Z.; Gallo, J.; Smizansky, M.; Mrazek, F.; Petrek, M. Osteoprotegerin gene polymorphism is not associated with prosthetic joint infection after total joint arthroplasty in the Czech population. Biomed. Pap. 2014, 158, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Sirajudeen, S.; Shah, I.; Al Menhali, A. A Narrative Role of Vitamin D and Its Receptor: With Current Evidence on the Gastric Tissues. Int. J. Mol. Sci. 2019, 20, 3832. [Google Scholar] [CrossRef]
- Shao, J.; Zhang, H.; Yin, B.; Li, J.; Zhu, Y.; Zhang, Y. Risk factors for surgical site infection following operative treatment of ankle fractures: A systematic review and meta-analysis. Int. J. Surg. 2018, 56, 124–132. [Google Scholar] [CrossRef]
- Milunsky, A. The “New Genetics” in Clinical Practice: A Brief Primary. J. Am. Board Fam. Med. 2017, 30, 377–379. [Google Scholar] [CrossRef]
- Khorsand, P.; Hormozdiari, F. Nebula: Ultra-efficient mapping-free structural variant genotyper. Nucleic Acids Res. 2021, 49, 47. [Google Scholar] [CrossRef]
- Khoury, M.J. Human Genome Epidemiology: Translating advances in human genetics into population-based data for medicine and public health. Genet. Med. 1999, 1, 71–73. [Google Scholar] [CrossRef] [Green Version]

| Author (Year) | Genetic Polymorphism Studied | Study Type | Study Country | Sample Ethnicity | Sample Size | Mean Age at Surgery (All Groups) | Operation |
|---|---|---|---|---|---|---|---|
| Erdemli et al. (2018) [20] | TNFα-238 (A) IL6-174 (C) GCSF3R (T) IL1 RN-VNTR (1/2 and 2/2) IL1B-511 (T) | Prospective | Turkey | Turkish | 88 (36 septic, 52 aseptic) | 68 | Revision arthroplasty |
| Malik et al. (2007) [13] | MBL-221 (promoter) MBL-550 (C) MBL Codon 54 (G) MBL Codon 52 | Case-control | United Kingdom | White patients from Northwest England | 312 (71 septic, 91 aseptic, 150 controls) | 68.6 | THA |
| Malik et al. (2006) [21] | OPG-163 OPG-245 OPG + 1181 RANK + 575 | Case-control | United Kingdom | White patients from Northwest England | 312 (71 septic, 91 aseptic, 150 non-TJA controls) | 68.6 | THA |
| Malik et al. (2007) b [14] | IL6-174 (C) MMP1-1 (C) MMP1-3 MMP1-4 MMP2 MMP4 VDR (T) VDR (L) | Case-control | United Kingdom | White patients from Northwest England | 312 (71 septic, 91 aseptic, 150 non-TJA controls) | 68.6 | THA |
| Mrazek et al. (2013) [23] | TLR2 R753Q TLR4 D299G TLR4 T399I | Case-control | Czech Republic | Czech | 350 (98 septic, 252 aseptic, 189 non-TJA controls) | 64 (septic), 49 (aseptic) | TJA |
| Navratilova et al. (2012) [15] | MBL2-550 (L) MBL2-221 (X) MBL2+54 (A) | Case-control | Czech Republic | Czech | 553 (112 septic, 245 aseptic, 196 non-TJA controls) | 63 (septic), 50 (Aseptic), 29 (Control) | TJA |
| Navratilova et al. (2014) [24] | OPG-163 (C) | Case-control | Czech Republic | Czech | 534 (98 septic, 251 aseptic, 185 non-TJA controls) | 67 (PJI), 49 (Aseptic TJA), 28 (Control group) | TJA |
| Stahelova et al. (2012) [22] | IL1B-511 (T) IL1B+3962 TNF-308 TNF-238 IL6-174 IL6nt565 | Case-control | Czech Republic | Czech | 471 89 (PJI), 214 (no PJI), 168 non-TJA controls | 63 (PJI) 47 (Aseptic TJA) not reported for control group | TJA |
| Study | Introduction | Methods | Results | Discussion | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Objectives and hypothesis clearly stated | 2. Clear eligibility criteria for participants/studies | 3. Clear definition of all variables | 4. Statistical methods replicable | 5. Assessment of HWE | 6. Assessment of ethnicity | 7. Mixed ethnicities addressed statistically | 8. Sufficient descriptive data (age, gender) | 9. Genotype frequencies stated | 10. Sample in HWE | 11. Consideration of population | |
| Erdemli et al. (2018) [20] | + | + | + | + | + | - | - | + | - | + | - |
| Malik et al. (2007)—MMP1 [14] | + | + | + | + | + | + | + | + | + | + | + |
| Malik et al. (2006)—RANK [21] | + | + | + | + | + | + | + | + | + | + | + |
| Malik et al. (2007)—MBL [13] | + | + | + | + | + | + | + | + | + | + | + |
| Mraszek et al. (2013) [23] | + | + | + | + | + | + | + | + | + | + | + |
| Navratilova et al. (2012) [15] | + | + | + | + | + | + | + | + | + | + | + |
| Navratilova et al. (2014) [24] | + | - | + | + | + | + | + | + | + | + | + |
| Stahelova et al. (2012) [22] | + | + | + | + | + | + | + | + | + | + | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hijazi, A.; Hasan, A.; Pearl, A.; Memon, R.; Debeau, M.; Roldan, M.; Awad, M.E.; Abdul-Kabir, E.; Saleh, K.J. Genetic Polymorphisms Associated with Perioperative Joint Infection following Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. Antibiotics 2022, 11, 1187. https://doi.org/10.3390/antibiotics11091187
Hijazi A, Hasan A, Pearl A, Memon R, Debeau M, Roldan M, Awad ME, Abdul-Kabir E, Saleh KJ. Genetic Polymorphisms Associated with Perioperative Joint Infection following Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. Antibiotics. 2022; 11(9):1187. https://doi.org/10.3390/antibiotics11091187
Chicago/Turabian StyleHijazi, Adel, Ahmad Hasan, Adam Pearl, Ramiz Memon, Michael Debeau, Mariana Roldan, Mohamed E. Awad, Ehsen Abdul-Kabir, and Khaled J. Saleh. 2022. "Genetic Polymorphisms Associated with Perioperative Joint Infection following Total Joint Arthroplasty: A Systematic Review and Meta-Analysis" Antibiotics 11, no. 9: 1187. https://doi.org/10.3390/antibiotics11091187
APA StyleHijazi, A., Hasan, A., Pearl, A., Memon, R., Debeau, M., Roldan, M., Awad, M. E., Abdul-Kabir, E., & Saleh, K. J. (2022). Genetic Polymorphisms Associated with Perioperative Joint Infection following Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. Antibiotics, 11(9), 1187. https://doi.org/10.3390/antibiotics11091187





