Actinomyces sp. Presence in the Bone Specimens of Patients with Osteonecrosis of the Jaw: The Histopathological Analysis and Clinical Implication
Abstract
:1. Introduction
2. Methodology
- (i)
- MRONJ: (1) Current or previous treatment with antiresorptive therapy alone or in combination with immune modulators or antiangiogenic medications; (2) Exposed bone or bone that can be probed through an intraoral or extraoral fistula(e) in the maxillofacial region that has persisted for more than eight weeks; (3) No history of radiation therapy to the jaws or metastatic disease to the jaws. MRONJ has stage 0–3 based on patient’s symptoms, clinical and radiological findings [6].
- (ii)
- ORN: irradiated bone becomes devitalized and exposed through the overlying skin or mucosa without healing for three months, without recurrence of the tumour [7].
The Specimen
3. Results
3.1. Brief Description of the Clinical Cases
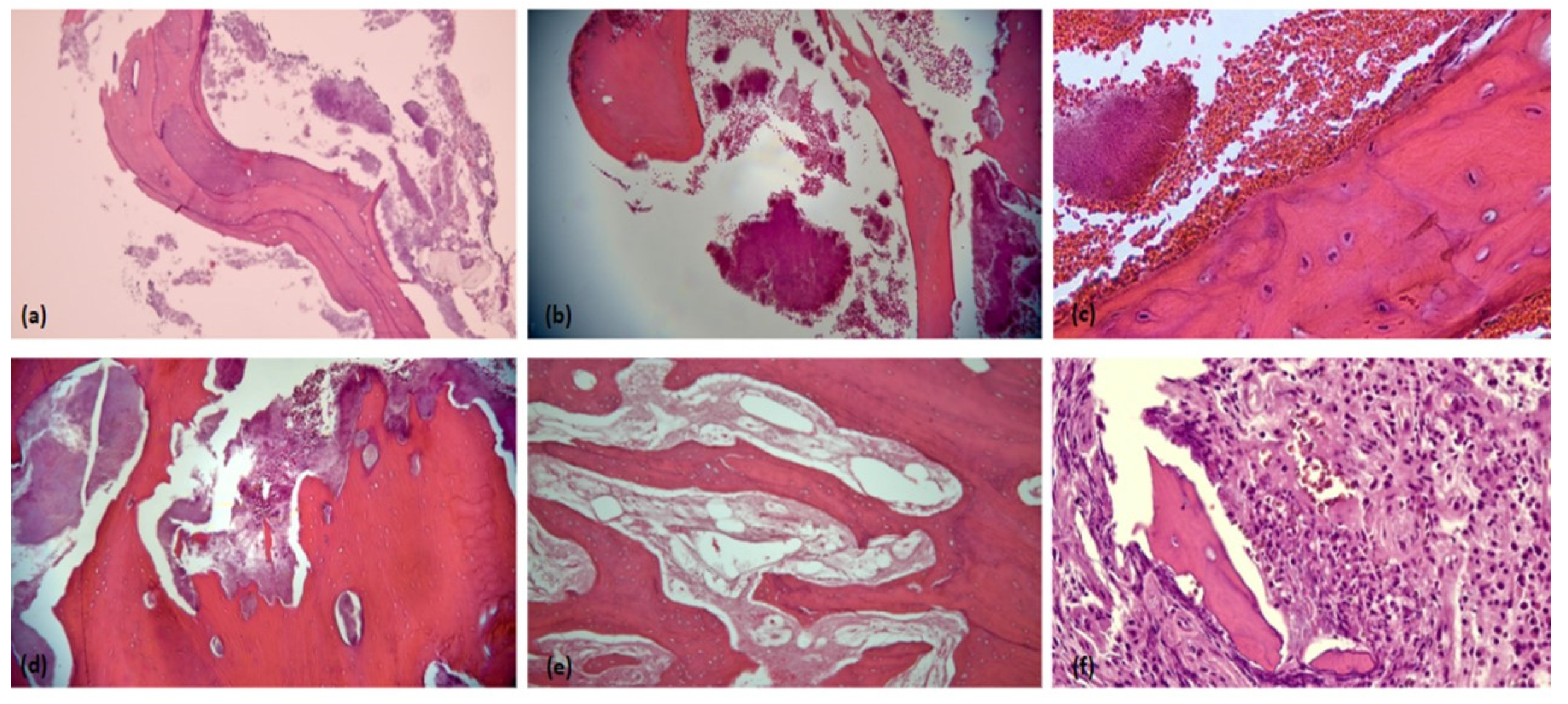
3.2. Histopathological Examination
3.3. Presence of Actinomyces sp.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gajdács, M.; Urbán, E.; Terhes, G. Microbiological and Clinical Aspects of Cervicofacial Actinomyces Infections: An Overview. Dent. J. 2019, 7, 85. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gadiwalla, Y.; Patel, V. Osteonecrosis of the jaw unrelated to medication or radiotherapy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, 446–453. [Google Scholar] [CrossRef] [PubMed]
- Muniz, L.V.; Lacerda, R.P.; Chaves, A.L.F.; Soares, J.M.A.; Leitão, T.J.; Barbosa, L.A.; dos Santos, H.B.; Ribeiro, R.I. Osteoradionecrosis of the jaw infected with Actinomyces sp: A challenge for clinical practice. Biosci. J. 2015, 31, 296–302. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.-G.; Lee, E.-Y.; Lee, O.-J.; Kim, S.; Kang, J.-Y.; Lim, J.S. Prediction models for early diagnosis of actinomycotic osteomyelitis of the jaw using machine learning techniques: A preliminary study. BMC Oral Health 2022, 22, 164. [Google Scholar] [CrossRef] [PubMed]
- Aghahosseini, F.; Hoseini, E.G.; Mahdavi, N. Actinomycotic Osteomyelitis of the Maxilla in a Patient on Phenytoin. Front. Dent. 2022, 19, 3. [Google Scholar] [CrossRef]
- Ruggiero, S.L.; Dodson, T.B.; Aghaloo, T.; Carlson, E.R.; Ward, B.B.; Kademani, D. American Association of Oral and Maxillofacial Surgeons’ Position Paper on Medication-Related Osteonecrosis of the Jaws—2022 Update. J. Oral Maxillofac. Surg. 2022, 80, 920–943. [Google Scholar] [CrossRef] [PubMed]
- Nadella, K.R.; Kodali, R.M.; Guttikonda, L.K.; Jonnalagadda, A. Osteoradionecrosis of the Jaws: Clinico-Therapeutic Management: A Literature Review and Update. J. Maxillofac. Oral Surg. 2015, 14, 891–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omar, N.I.; Baharin, B.; Lau, S.F.; Ibrahim, N.; Mohd, N.; Fauzi, A.A.; Muhammad, N.; Fernandez, N.M. The Influence of Ficus deltoidea in Preserving Alveolar Bone in Ovariectomized Rats. Vet. Med. Int. 2020, 2020, 8862489. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, S.; Yoshida, H.; Yoshimura, H. Orofacial soft tissues actinomycosis: A retrospective, 10-year single-institution experience. J. Dent. Sci. 2021, 16, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Lyons, A.; Osher, J.; Warner, E.; Kumar, R.; Brennan, P.A. Osteoradionecrosis—A review of current concepts in defining the extent of the disease and a new classification proposal. Br. J. Oral Maxillofac. Surg. 2014, 52, 392–395. [Google Scholar] [CrossRef] [PubMed]
- Valour, F.; Sénéchal, A.; Dupieux, C.; Karsenty, J.; Lustig, S.; Breton, P.; Gleizal, A.; Boussel, L.; Laurent, F.; Braun, E.; et al. Actinomycosis: Etiology, clinical features, diagnosis, treatment, and management. Infect. Drug Resist. 2014, 7, 183–197. [Google Scholar] [PubMed] [Green Version]
- De Antoni, C.C.; Matsumoto, M.A.; Da Silva, A.A.; Curi, M.M.; Júnior, J.F.S.; Sassi, L.M.; Cardoso, C.L. Medication-related osteonecrosis of the jaw, osteoradionecrosis, and osteomyelitis: A comparative histopathological study. Braz. Oral Res. 2018, 32, e23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Ceulaer, J.; Tacconelli, E.; Vandecasteele, S.J. Actinomyces osteomyelitis in bisphosphonate-related osteonecrosis of the jaw (BRONJ): The missing link? Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 1873–1880. [Google Scholar] [CrossRef] [PubMed]
- Aftimos, V.; Zeinoun, T.; Tayeh, R.B.; Aftimos, G. Bisphosphonate Related Osteonecrosis of the Jaw: A Study of 18 Cases Associated with Fungal Infection. Int. J. Dent. 2014, 2014, 869067. [Google Scholar] [CrossRef] [PubMed]
- Boff, R.C.; Salum, F.G.; Figueiredo, M.A.; Cherubini, K. Important aspects regarding the role of microorganisms in bisphosphonate-related osteonecrosis of the jaws. Arch. Oral Biol. 2014, 59, 790–799. [Google Scholar] [CrossRef] [PubMed]
- Curi, M.; Dib, L.; Kowalski, L.; Landman, G.; Mangini, C. Opportunistic actinomycosis in osteoradionecrosis of the jaws in patients affected by head and neck cancer: Incidence and clinical significance. Oral Oncol. 2000, 36, 294–299. [Google Scholar] [CrossRef]
- Bhagawati, B.T.; Solanki, M.; Solanki, H.; Sharma, M. Actinomycotic osteomyelitis of maxilla in a diabetic patient—“A rare case report & review of literature”. J. Indian Acad. Oral Med. Radiol. 2021, 33, 487–489. [Google Scholar]
- Mawardi, H.; Giro, G.; Kajiya, M.; Ohta, K.; Almazrooa, S.; AlShwaimi, E.; Woo, S.-B.; Nishimura, I.; Kawai, T. A Role of Oral Bacteria in Bisphosphonate-induced Osteonecrosis of the Jaw. J. Dent. Res. 2011, 90, 1339–1345. [Google Scholar] [CrossRef] [PubMed]
- Gross, C.; Weber, M.; Creutzburg, K.; Möbius, P.; Preidl, R.; Amann, K.; Wehrhan, F. Osteoclast profile of medication-related osteonecrosis of the jaw secondary to bisphosphonate therapy: A comparison with osteoradionecrosis and osteomyelitis. J. Transl. Med. 2017, 15, 128. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 |
|---|---|---|---|---|---|---|---|---|
| Race | Malay | Malay | Chinese | Chinese | Malay | Chinese | Chinese | Chinese |
| Gender | Male | Male | Female | Female | Female | Male | Male | Male |
| Age | 55 | 64 | 72 | 66 | 53 | 66 | 47 | 69 |
| Comorbidities | GCT metastasis | Multiple myeloma, hypertension, dyslipidaemia | NPC, 8hypertension | Osteoporosis, SLE, diabetes, 8hypertension | NPC | Tongue OSCC | Lacrimal SCC | Tongue OSCC |
| Affected site | Mandible | Maxilla | Maxilla | Mandible | Mandible | Mandible | Maxilla | Mandible |
| Staging | Stage 2 * | Stage 3 * | Stage 3# | Stage 2 * | Stage 3# | Stage 1# | Stage 3# | Stage 3# |
|
|
|
| |||||
| Radiotherapy doses | 70 Gy | Data not available | 66 Gy | Data not available | 70 Gy | |||
| ORN onset post-radiotherapy | 14 years | 8 years | 7 years | 3 years | 3 years | |||
| Radiographic findings | Mixed osteolytic and sclerosis at the lower left mandible edentulous alveolar ridge. Cortical bone margin intact. | Bone surrounding teeth 14-16 and 26 were severely resorbed. Alveolar ridge margin appeared shaggy with multiple radiolucencies. | No abnormality detected on the maxilla and mandibular ridges. | Sequestrum-like radiopacity seen on left mandible with a focal region of tooth 34 appeared radiolucent. | Mixed osteolytic and sclerosis at the angle of mandible. Cortical bone margin still intact. Bone supporting around teeth 46-47 are sufficient. | Mixed osteolytic and sclerosis at the lower edentulous ridges. | Unknown | Lower edentulous ridge showed general horizontal resorption. |
| Organisms isolated from culture & sensitivity | Mixed growth | No culture & sensitivity performed | No culture & sensitivity performed | No culture & sensitivity performed | Data not available | No culture & sensitivity performed | Data not available | No culture & sensitivity performed |
| Brief microscopic findings | Areas of acute inflammatory infiltrates with granulation tissue formation. Necrotic bone with sulphur granule-like material observed. | Necrotic bone with collection of bluish material resembling sulfur granules of actinomyces. | Fragments of non-vital mature bone surrounded by a focus of basophilic microorganisms with a mixed inflammatory infiltrate. Scalloping resorbed bone margin was also seen. | Presence of trabeculae of non-vital bones surrounded by bacterial colonies and mixed inflammatory cells was evident. | Non-vital bony fragments were surrounded by colonies of microorganisms and mixed inflammatory cells. Also observed were foci of necrosis with some areas exhibiting ingrowth of epithelium towards the non-vital bones. | Fragments of non-vital bone with peripheral resorption and numerous basophilic bacterial colonization. | Non-vital bones were observed to be attached to the non-inflamed fibrous tissue and there was presence of microorganism colonies. | Non-vital bones with attached intensely inflamed fibrous tissue and presence of microorganism colonies were present. |
| Final diagnosis | MRONJ | MRONJ | ORN | MRONJ | ORN | ORN | ORN | ORN |
| Histological Findings | ORN | MRONJ |
|---|---|---|
| Necrotic bone | ✓ | ✓ |
| Osteoclast | ✓ | ✓ |
| Osteoblastic rimming | ✓ | |
| Reactive bone | ✓ | ✓ |
| Empty osteocytes lacunae | ✓ | ✓ |
| Inflammation | ✓ | ✓ |
| Blood vessels | ✓ | |
| Hyperaemia and thrombosis | ✓ | ✓ |
| Microorganism (Actinomyces sp.) | ✓ | ✓ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, N.; Apandi, N.I.M.; Shuhardi, S.A.; Ramli, R. Actinomyces sp. Presence in the Bone Specimens of Patients with Osteonecrosis of the Jaw: The Histopathological Analysis and Clinical Implication. Antibiotics 2022, 11, 1067. https://doi.org/10.3390/antibiotics11081067
Ibrahim N, Apandi NIM, Shuhardi SA, Ramli R. Actinomyces sp. Presence in the Bone Specimens of Patients with Osteonecrosis of the Jaw: The Histopathological Analysis and Clinical Implication. Antibiotics. 2022; 11(8):1067. https://doi.org/10.3390/antibiotics11081067
Chicago/Turabian StyleIbrahim, Norliwati, Nurul Inaas Mahamad Apandi, Syafiqah Aina Shuhardi, and Roszalina Ramli. 2022. "Actinomyces sp. Presence in the Bone Specimens of Patients with Osteonecrosis of the Jaw: The Histopathological Analysis and Clinical Implication" Antibiotics 11, no. 8: 1067. https://doi.org/10.3390/antibiotics11081067
APA StyleIbrahim, N., Apandi, N. I. M., Shuhardi, S. A., & Ramli, R. (2022). Actinomyces sp. Presence in the Bone Specimens of Patients with Osteonecrosis of the Jaw: The Histopathological Analysis and Clinical Implication. Antibiotics, 11(8), 1067. https://doi.org/10.3390/antibiotics11081067






