Abstract
Few articles have reported drug concentrations of different ophthalmic dosage forms in the ocular tissues. This study aimed to determine the ocular pharmacokinetics of gatifloxacin 0.3% eye gel (GTX-Gel) and gatifloxacin 0.3% eye solution (GTX-Sol) at different time intervals after topical instillation in rabbits. A total of 126 healthy New Zealand rabbits were included, of which six rabbits did not receive antibiotics (control group). The remaining rabbits were randomly divided into four groups. GTX-Gel and GTX-Sol (50 μL) were topically instilled every hour in groups A1 and B1, respectively, and every two hours in groups A2 and B2, respectively, for 12 h. Ocular tissues were collected 2, 4, 8, 12, and 24 h after administration. Gatifloxacin concentration was measured using high-performance liquid chromatography coupled with tandem mass spectrometry. The drug reached peak concentrations (Cmax) in all tissues at 8–12 h. With the same administration frequency, the Cmax was higher with GTX-Gel than with GTX-Sol (p < 0.05). Except for the iris-ciliary body, other ocular tissues did not show significant difference (p > 0.05) in gatifloxacin concentration between either pair of groups. Gatifloxacin ophthalmic gel was found to attain significantly higher concentrations than the ophthalmic solution in ocular tissues.
1. Introduction
Ophthalmic drug forms have been one of the most important and widely developed pharmaceuticals for several years [1,2,3]. Bacterial keratitis and endophthalmitis are severe forms of ocular infections that can lead to irreversible visual loss if not treated properly and timely [4,5,6]. To prevent or treat ocular infections, topical antibiotics must penetrate the relevant tissues at concentrations sufficient to eradicate the causative organisms [7].
Topical fluoroquinolone antibiotics are widely used in clinical practice. Gatifloxacin is a fourth-generation topical fluoroquinolone. Studies have shown that gatifloxacin is more potent than second- and third-generation fluoroquinolones, suggesting that it is superior to these in treating and preventing ocular infections caused by gram-positive organisms and atypical mycobacteria [8]. Low bioavailability of drugs after optical instillation is observed because of the complicated anatomy of the eye, the small absorptive surface, lipophilicity of corneal epithelium, binding of the drug with the proteins in tear fluid, and defense mechanisms of the eye, such as tear formation, blinking, and flow of substances through the nasolacrimal duct [9,10,11]. Previous studies have demonstrated that prolonged precorneal residence and delay the elimination of the drug from the precorneal area can effectively increase the bioavailability of drugs [12]. To achieve the required drug concentration in the target tissue and sustain it for an appropriate period of time, polymers, such as carbomers, hyaluronic acid and hypromellose among others were introduced into formulations of conventional ophthalmic dosage forms. Carbomer as bioadhesive polymers can prolong the retention time of the drug on the surface of the eye and drug release to increase the ocular absorption [13]. The main advantages of carbomer include its excellent biocompatibility and mucoadhesiveness, which increased both the rate and extent of drug transfer from oil to the aqueous phase. Its use as a vehicle in ocular drug delivery has been reviewed previously [14].
Studies have revealed that carbomers were used in timolol liquid formulations to form gels to increase the viscosity of the formulation, which would, in turn, reduce the frequency of drug application [15]. In patients with keratitis and endophthalmitis, the antibiotics need to penetrate relevant tissues at sufficient concentrations. Thus, carbomers are added to gatifloxacin eye drops to increase its tissue permeability, and lower its dosing frequency for the patients’ convenience [16]. The purpose of this study was to compare the pharmacokinetic and distribution of gatifloxacin 0.3% ophthalmic gel (GTX-Gel) and gatifloxacin 0.3% ophthalmic solution (GTX-Sol) in the ocular tissues after topical application once every hour and every 2 h.
2. Results
2.1. Method Development
The study method was validated for selectivity, linearity, accuracy, precision, matrix effect, recovery, and stability according to the US Food and Drug Administration bioanalytical method validation guidelines. In the chromatograms of plasma and ocular tissue homogenates from untreated rabbits, no endogenous interfering peaks were found at the retention times of gatifloxacin and Internal Standard (IS). Corneal homogenate was used as an example to show specificity, as shown in Figure 1.
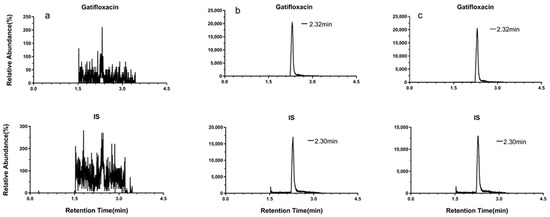
Figure 1.
Representative multiple reaction monitoring (MRM) chromatograms of (a) a blank corneal homogenate; (b) a corneal homogenate spiked with 0.4 μg/mL gatifloxacin and the IS; and (c) a corneal sample from the rabbit in group A1.
The linearity of the method was studied by analyzing the calibration standards in duplicate at each concentration level in different biological specimens. All calibration curves showed good linearity and all correlation coefficients (r) were >0.99 (Table 1).

Table 1.
Calibration curves for the determination of gatifloxacin concentration in different biological specimens.
The results mentioned above and in Table 2 and Table 3 show that this method was successfully validated and could be applied to studies of ocular pharmacokinetics of gatifloxacin in rabbits.

Table 2.
Precision, accuracy, recovery, and matrix effect of gatifloxacin in the cornea (n = 6).

Table 3.
Stability of gatifloxacin in the cornea (n = 3).
2.2. Pharmacokinetic and Ocular Tissue Distribution Study
The concentration-time values of gatifloxacin in ocular tissues and plasma are presented in Figure 2, and the estimated pharmacokinetic values are summarized in Table 4.
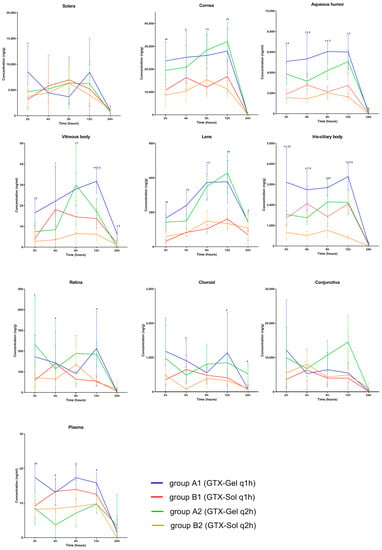
Figure 2.
Concentration-time values of gatifloxacin in ocular tissues and plasma. Each point represents the mean concentration (n = 5–6). ±: the standard error of the mean. *: The difference was statistically significant between groups A1 and B1; #: The difference was statistically significant between groups A2 and B2; $: The difference was statistically significant between groups A1 and A2; &: The difference was statistically significant between groups B1 and B2 (p < 0.05).

Table 4.
AUC0–24 values of gatifloxacin in ocular tissues and plasma.
The drug concentration in the sclera and conjunctiva fluctuated at 4–10 μg/g in each period in the 4 gourps. No significant difference in the drug concentration was found between groups (p > 0.05). The drug concentration in the posterior segment of the eyeball was low, such as in the vitreous body, retina, and choroid. The value fluctuated between 0.01–1 μg/g. For the iris-ciliary body, gatifloxacin concentration was significantly higher in group A1 than other groups (p < 0.05).
After the administration of GTX-Gel or GTX-Sol every hour or every two hours for 12 h, the drug distribution in ocular tissues was ranked in the following order from highest to lowest: cornea > sclera > conjunctiva > aqueous humor > iris-ciliary body > choroid > lens > retina > vitreous body > plasma. The drug reached peak concentrations (Cmax) in the corneal tissue, aqueous humor, vitreous body, lens, iris-ciliary body, retina, and choroid at 8–12 h. Cmax values of gatifloxacin in ocular tissues are summarized in Table 5.

Table 5.
Cmax values of gatifloxacin in ocular tissues.
With the same administration frequency, the between-group differences in Cmax in the cornea, aqueous humor, vitreous body, lens, and iris-ciliary body were significant (p < 0.05). After the final dose, the gatifloxacin concentration in the cornea and aqueous humor was lower than the lower limit of quantification (20 mg/mL) in all groups. With the same administration frequency, between-group differences in the gatifloxacin concentration in the sclera, retina, choroid, conjunctiva, and plasma were not statistically significant (p > 0.05).
The mean area under curve during the 24 h period (AUC0–24) was significantly higher for GTX-Gel than for GTX-Sol in the ocular tissues (p < 0.05). In all groups, the lowest AUC0–24 was found in the plasma, which indicated that the drug was minimally absorbed into the systemic circulation. The mean plasma AUC0–24 was higher in the GTX-Gel groups than in the GTX-Sol groups, but the difference was not statistically significant (p > 0.05).
Except for the iris-ciliary body, no other tissues showed significant differences in gatifloxacin concentration between the groups A1 and A2, or between B1 and B2 (p > 0.05). These results indicate that when the administration frequency decreased from hourly to two-hourly, the concentration of gatifloxacin in the ocular tissues did not effectively decrease. It may be clinically significant to increase the administration frequency of 0.3% GTX-Gel or GTX-Sol to once every hour for the treatment of iris-ciliary body infections.
3. Discussion
The most important finding of this study was that 0.3% GTX-Gel has greater penetration of ocular tissues than GTX-Sol. When the administration frequency of either formulation decreased from once every hour to once every 2 h, the drug concentration in the ocular tissues did not effectively decrease.
Previous studies have shown that gatifloxacin is more potent than second- and third-generation fluoroquinolones [17]. Compared with older fluoroquinolones, gatifloxacin is characterized by higher in vitro activity against gram-positive bacteria, most notably Streptococcus pneumoniae. It also exhibits enhanced activity against atypical pathogens (Chlamydia and Mycoplasma species) and some anaerobic bacterial pathogens [8,18].
Perioperative antibiotic prophylaxis for endophthalmitis following eye surgery is the most effective form of prophylaxis [7]. Fluoroquinolones possess the advantages of broad antibiotic spectra, high efficiency, low toxicity, and high corneal penetration, and they exert antimicrobial effects by affecting the activities of DNA gyrase and topoisomerase IV [19,20]. Therefore, fluoroquinolone drops are one of the most common perioperative agents used in clinics [21]. That was the main reason we chose to study the pharmacokinetic and distribution of gatifloxacin. A previous study investigated the penetration of 0.3% gatifloxacin ophthalmic gel and 0.3% gatifloxacin ophthalmic solution into the aqueous humor after topical application in patients undergoing phacoemulsification procedures. They found that the bioavailability of ophthalmic gel was approximately 2-fold greater than that of the solution, which indicated that the gel maintained the longest time and had the best penetration and bioavailability [22].
The continuing escalation of antimicrobial-resistance indicates that slowing the rate at which resistance develops in pathogens is of paramount importance. The concept of mutant prevention concentration (MPC) represents a novel in vitro measurement of fluoroquinolone potency [23,24]. Tissue penetration by a topical antibiotic is important for attaining MPCs, as it affects the ability of the drug to achieve a concentration well above the minimum inhibitory concentrations (MIC) for a given microorganism. In essence, MPC defines the antimicrobial drug concentration threshold. Generally, a Cmax/MIC ratio of 8 to 10 has been associated with effective treatment. When comparing the gatifloxacin ocular tissue concentrations achieved in this study with MPCs derived from the MICs in the study conducted by Hosaka et al. [25], we found that GTX-Gel achieved MPCs of 8.92 for Staphylococcus haemolyticus (SH) and Pseudomonas aeruginosa (PA)in the cornea. This indicated that GTX-Gel would useful for PA keratitis in rabbit eye, which was confirmed by Mah F S et al. [26] in the previous study. Table 6 lists the in vitro data on MIC90 of gatifloxacin for these bacterial isolates.

Table 6.
In vitro activity of gatifloxacin against clinical isolates [16].
However, GTX-Sol could not achieve MPCs for S. haemolyticus and P. aeruginosa in the cornea. Neither GTX-Gel nor GTX-Sol could achieve MPCs for these pathogens in the aqueous humor or iris-ciliary body. However, GTX-Gel could achieve the MPC for S. pneumoniae in the aqueous humor and iris-ciliary body. All MPC values were higher in the GTX-Gel groups than in the GTX-Sol groups. Notably, neither GTX-Gel nor GTX-Sol could achieve MPC or MIC in the vitreous body. This is consistent with other studies investigating topically administered drug penetration, which show that negligible concentrations were detected in the vitreous body [27,28]. This could be a major obstacle in the treatment of endophthalmitis.
Another important finding of the current study is that even with an hourly dosing for 12 h, the concentration of gatifloxacin in the ocular tissues was undetectable 12 h after the application of the last dose. This indicates that maintaining the drug concentration at required levels at night is difficult, which is a major problem in clinical practice.
Our results confirmed that, compared to GTX-Sol, GTX-Gel exhibited better penetration into the cornea, aqueous humor, and iris-ciliary body, and this indicates that patients treated with this formulation could demonstrate a lower tendency to develop resistant organisms.
GTX-Gel contains gatifloxacin (0.3%), carbomer, hyaluronic acid and other excipients. These substances increase viscosity of GTX-Gel to 2 Pa s. The value of viscosity around 5–6 Pa s was reported to obtain the highest mucoadhesiveness of the polymeric dispersions [29]. Although CTX-Gel does not achieve the best viscosity, but it provides optimal comfort and does not blur the vision. The increased viscosity makes the drug enable longer contact with the eye surface, and thus improve the bioavailability of the formulation [30]. These ingredients have protective effects on the cornea [1,31,32]. These findings suggest that 0.3% GTX-Gel could promote corneal wound healing and that it requires a low frequency of drug application. In addition, they exhibit better physicochemical characteristics, such as bioadhesion and ocular tolerance, compared to conventional ophthalmic preparations, as a consequence of prolonged pre-corneal residence time. Furthermore, as ophthalmic gels do not cause “blurred vision”, they can be comfortably applied and, thus, are more acceptable for patients [22]. The formula has been granted an invention patent of China National Intellectual Property Administration (CNIPA) (Patent Number: CN102078284B) and a United States Patent (Patent Number: US8901131B2) [33].
The strength of this study includes the demonstration of differences in drug concentrations in all ocular tissues. The limitations of this study include the small sample size and the short duration of the experiment. We did not detect the duration of the peak concentration of either of the dosage forms.
In conclusion, this study demonstrated that, compared with topically administered 0.3% GTX-Sol, 0.3% GTX-Gel showed greater penetration into the cornea, aqueous humor, vitreous body, lens, and iris-ciliary body after administration every hour or two hours for 12 h. Thus, 0.3% GTX-Gel exhibited an advantage over 0.3% GTX-Sol, as it requires a lower application frequency because of better penetration into the ocular tissues. In addition, when the frequency of GTX-Gel or GTX-Sol decreased from once every hour to once every 2 h, the drug concentration in the ocular tissues did not effectively decrease. We believe that our results will provide guidance for the clinical use of these medications. GTX-Gel offers a more effective ophthalmic therapy for ocular infections than conventional eye drops.
4. Materials and Methods
4.1. Materials
One hundred and twenty-six healthy New Zealand white rabbits (63 males and 63 females), ranging from 2.0 to 2.5 kg in weight were raised for at least 1 week under standardized temperature, humidity, and lighting conditions before the experiment. All animals were treated in accordance with the guidelines of the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research. Ethics approval for the study protocol was obtained from the appropriate institutional review board.
4.2. Preparation of Calibration Standards and Quality Control Samples
Standard stock solutions of gatifloxacin and the IS were prepared separately in methanol at a concentration of 1.0 μg/μL. Stock gatifloxacin solutions were diluted with methanol to obtain a series of working solutions (0.4–4 μg/mL). The concentration of the IS working solution was 0.4 μg/mL. Quality control working solutions at concentrations of 0.8, 1, and 3.2 μg/mL were prepared from a separately prepared 1000 μg/mL stock solution of gatifloxacin. All the solutions were stored at 4 °C until further analysis.
Calibration standards were freshly prepared by placing 25 μL of each gatifloxacin working solution into 50 μL of blank rabbit plasma or ocular tissue homogenates, added with 25 μL of the IS working solution and 175 μL of methanol. The mixture was vortex-mixed for 1 min and centrifuged at 14,500 rpm for 10 min. Then, 40 μL of the supernatant, containing 16 × 10−5 L of methanol, was vortex-mixed at 14,500 rpm for 5 min. An aliquot of 7 × 10−6 L of the supernatant was injected into a liquid chromatography with tandem mass spectrometry (LC/MS/MS) system. Quality control samples were also prepared using the method described above with final concentrations of 40,500, and 1600 ng/mL.
4.3. Sample Processing Methods
The animals were randomly divided into five groups. Six rabbits in the control group did not receive any antibiotics, and the remaining 120 rabbits were randomly divided into four groups; 5 × 10−5 L of GTX-Gel (group A1) or GTX-Sol (group B1) was instilled in the conjunctival sac of the left eye every hour min for 12 h. Similarly, 50 μL of GTX-Gel (group A2) or GTX-Sol (group B2) was instilled every 2 h for 12 h. GTX-Gel and GTX-Sol (0.3%, for research only) were obtained from Shenyang Xingqi Pharmaceutical Co., Ltd. (Shenyang, China). Approximately 2 mL of blood was collected from the heart of each rabbit at 2, 4, 8, 12, and 24 h after topical instillation. The blood samples were poured into a tube containing heparin and mixed thoroughly. The rabbits were euthanized by an overdose of anesthesia, and the aqueous humor, conjunctiva, cornea, iris-ciliary body, lens, vitreous body, retina, choroid, and sclera were collected from the left eye. The aqueous humor and vitreous body were collected by aspiration with syringes. The solid tissues, except for the retina and choroid, were procured and rinsed briefly with physiological saline solution to remove blood, blotted on filter paper, and then weighed. All specimens were stored at −80 °C until analysis. Samples at each time interval were collected half an hour after the dose was administered. The sampling times were within a window of ±5 min from the assigned time.
Solid ocular tissues were individually homogenized in double-distilled water at 1:10 (w/v), except for the retina, choroid, and lens (for which 1:3 w/v was used). The plasma, aqueous humor, and vitreous humor previously collected from the treated rabbit eye were used as samples directly. Next, 50 μL of the diluted solution was transferred to an Eppendorf tube®, and 25 μL of the IS working solution and 175 μL of methanol were added. The mixture was then treated using the same procedure followed for previous samples. The gatifloxacin concentrations in the solid ocular tissues were calculated by dividing the total amount of extracted drug in each specimen by the tissue weight.
4.4. Pharmacokinetic and Statistical Analysis
Drug concentrations in the corneal tissues and aqueous humor were determined using the previously described HPLC-MS/MS method. The Cmax was obtained from visual inspection of the data, and the AUC was calculated using the linear trapezoidal rule, as described by Nedelman et al. [34] Statistical analysis was performed using Student’s two-tailed t test, and by analysis of variance and Scheffe’s test.
5. Conclusions
This study demonstrated that, compared with topically administered 0.3% GTX-Sol, 0.3% GTX-Gel showed greater penetration into the ocular tissues after administration. When the frequency of GTX-Gel or GTX-Sol decreased from once every hour to once every 2 h, an equivalent gatifloxacin concentration could be achieved in the ocular tissues. The use of topically administered GTX-Gel or GTX-Sol could not achieve an effective antimicrobial drug concentration in the vitreous body, furthermore, the concentration of gatifloxacin in the ocular tissues was undetectable when the medication was stopped at night for 12 h.
Author Contributions
M.L. and X.Z. contributed equally to this work. Conceptualization, M.L., X.L. and F.D.; methodology, X.Z. and Y.Y.; software, Q.Y. and J.Z.; validation, M.L. and Y.L.; formal analysis, M.L. and X.Z.; investigation, X.L. and F.D.; resources, Y.L.; data curation, X.Z.; writing—original draft preparation, M.L.; writing—review and editing, M.L. and F.D.; visualization, Q.Y.; supervision, X.L. and F.D.; project administration, X.L. and F.D.; funding acquisition, X.L. and F.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by funds from the National Natural Science Foundation of China (grant number 81974135), Fundamental Research Funds of The State Key Laboratory of Ophthalmology (grant numbers 30306020240020130 and 3030902113030), and High-Level Hospital Construction Project (grant number 303010401).
Institutional Review Board Statement
The animal study protocol was approved by the Medical Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Baranowski, P.; Karolewicz, B.; Gajda, M.; Pluta, J. Ophthalmic drug dosage forms: Characterisation and research methods. Sci. World J. 2014, 2014, 861904. [Google Scholar] [CrossRef] [PubMed]
- Pawar, P.; Katara, R.; Mishra, S.; Majumdar, D.K. Topical ocular delivery of fluoroquinolones. Expert Opin. Drug Deliv. 2013, 10, 691–711. [Google Scholar] [CrossRef] [PubMed]
- Velpandian, T. Intraocular penetration of antimicrobial agents in ophthalmic infections and drug delivery strategies. Expert Opin. Drug Deliv. 2009, 6, 255–270. [Google Scholar] [CrossRef] [PubMed]
- Christopher, K.L.; Hood, C.T.; Mian, S.I.; Ayres, B. Endophthalmitis in Advanced Microbial Keratitis: Risk Factors and Examination Findings. Cornea 2020, 39, 1096–1101. [Google Scholar] [CrossRef]
- Zafar, S.; Wang, P.; Woreta, F.A.; Aziz, K.; Makary, M.; Ghous, Z.; Srikumaran, D. Postoperative Complications in Medicare Beneficiaries Following Endothelial Keratoplasty Surgery. Am. J. Ophthalmol. 2020, 219, 1–11. [Google Scholar] [CrossRef]
- Ting, D.; Mckenna, M.; Sadiq, S.N.; Martin, J.; Mudhar, H.S.; Meeney, A.; Patel, T. Arthrographis kalrae Keratitis Complicated by Endophthalmitis: A Case Report with Literature Review. Eye Contact. Lens. 2020, 46, e59–e65. [Google Scholar] [CrossRef]
- Gower, E.W.; Lindsley, K.; Tulenko, S.E.; Nanji, A.A.; Leyngold, I.; McDonnell, P.J. Perioperative antibiotics for prevention of acute endophthalmitis after cataract surgery. Cochrane Database Syst. Rev. 2017, 2, D6364. [Google Scholar] [CrossRef]
- McCulley, J.P.; Caudle, D.; Aronowicz, J.D.; Shine, W.E. Fourth-generation fluoroquinolone penetration into the aqueous humor in humans. Ophthalmology 2006, 113, 955–959. [Google Scholar] [CrossRef]
- Pahuja, P.; Arora, S.; Pawar, P. Ocular drug delivery system: A reference to natural polymers. Expert Opin. Drug Deliv. 2012, 9, 837–861. [Google Scholar] [CrossRef]
- McClellan, K.A. Mucosal defense of the outer eye. Surv. Ophthalmol. 1997, 42, 233–246. [Google Scholar] [CrossRef]
- Sieg, J.W.; Robinson, J.R. Mechanistic studies on transcorneal permeation of pilocarpine. J. Pharm. Sci. 1976, 65, 1816–1822. [Google Scholar] [CrossRef] [PubMed]
- Terreni, E.; Chetoni, P.; Burgalassi, S.; Tampucci, S.; Zucchetti, E.; Chipala, E.; Alany, R.G.; Al-Kinani, A.A.; Monti, D. A hybrid ocular delivery system of cyclosporine-A comprising nanomicelle-laden polymeric inserts with improved efficacy and tolerability. Biomater. Sci. 2021, 9, 8235–8248. [Google Scholar] [CrossRef] [PubMed]
- Dubashynskaya, N.; Poshina, D.; Raik, S.; Urtti, A.; Skorik, Y.A. Polysaccharides in Ocular Drug Delivery. Pharmaceutics 2019, 12, 22. [Google Scholar] [CrossRef] [PubMed]
- Woodley, J. Bioadhesion: New possibilities for drug administration? Clin. Pharmacokinet. 2001, 40, 77–84. [Google Scholar] [CrossRef]
- Schenker, H.; Maloney, S.; Liss, C.; Gormley, G.; Hartenbaum, D. Patient preference, efficacy, and compliance with timolol maleate ophthalmic gel-forming solution versus timolol maleate ophthalmic solution in patients with ocular hypertension or open-angle glaucoma. Clin. Ther. 1999, 21, 138–147. [Google Scholar] [CrossRef]
- Liu, X.; Wang, N.L.; Wang, Y.L.; Ma, C.; Ma, L.; Gao, L.X.; Huang, Y.X.; Xiong, S.H.; Wang, K. Determination of drug concentration in aqueous humor of cataract patients administered gatifloxacin ophthalmic gel. Chin. Med. J. 2010, 123, 2105–2110. [Google Scholar]
- Scoper, S.V. Review of third-and fourth-generation fluoroquinolones in ophthalmology: In-vitro and in-vivo efficacy. Adv. Ther. 2008, 25, 979–994. [Google Scholar] [CrossRef]
- Duxfield, L.; Sultana, R.; Wang, R.; Englebretsen, V.; Deo, S.; Swift, S.; Rupenthal, I.; Al-Kassas, R. Development of gatifloxacin-loaded cationic polymeric nanoparticles for ocular drug delivery. Pharm. Dev. Technol. 2016, 21, 172–179. [Google Scholar] [CrossRef]
- Mustaev, A.; Malik, M.; Zhao, X.; Kurepina, N.; Luan, G.; Oppegard, L.M.; Hiasa, H.; Marks, K.R.; Kerns, R.J.; Berger, J.M.; et al. Fluoroquinolone-gyrase-DNA complexes: Two modes of drug binding. J. Biol. Chem. 2014, 289, 12300–12312. [Google Scholar] [CrossRef]
- Hariprasad, S.M.; Mieler, W.F.; Holz, E.R. Vitreous and aqueous penetration of orally administered gatifloxacin in humans. Arch. Ophthalmol. 2003, 121, 345–350. [Google Scholar] [CrossRef][Green Version]
- Inoue, Y.; Usui, M.; Ohashi, Y.; Shiota, H.; Yamazaki, T. Preoperative disinfection of the conjunctival sac with antibiotics and iodine compounds: A prospective randomized multicenter study. Jpn. J. Ophthalmol. 2008, 52, 151–161. [Google Scholar] [CrossRef] [PubMed]
- Ding, W.; Ni, W.; Chen, H.; Yuan, J.; Huang, X.; Zhang, Z.; Wang, Y.; Yu, Y.; Yao, K. Comparison of Drug Concentrations in Human Aqueous Humor after the Administration of 0.3% Gatifloxacin Ophthalmic Gel, 0.3% Gatifloxacin and 0.5% Levofloxacin Ophthalmic Solutions. Int. J. Med. Sci. 2015, 12, 517–523. [Google Scholar] [CrossRef]
- Benitez-Del-Castillo, J.; Verboven, Y.; Stroman, D.; Kodjikian, L. The role of topical moxifloxacin, a new antibacterial in Europe, in the treatment of bacterial conjunctivitis. Clin. Drug Investig. 2011, 31, 543–557. [Google Scholar] [CrossRef] [PubMed]
- Hesje, C.K.; Borsos, S.D.; Blondeau, J.M. Benzalkonium chloride enhances antibacterial activity of gatifloxacin and reduces its propensity to select for fluoroquinolone-resistant strains. J. Ocul. Pharmacol. Ther. 2009, 25, 329–334. [Google Scholar] [CrossRef]
- Hosaka, M.; Yasue, T.; Fukuda, H.; Tomizawa, H.; Aoyama, H.; Hirai, K. In vitro and in vivo antibacterial activities of AM-1155, a new 6-fluoro-8-methoxy quinolone. Antimicrob. Agents Chemother. 1992, 36, 2108–2117. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mah, F.S.; Romanowski, E.G.; Kowalski, R.P.; Yates, K.A.; Gordon, Y.J. Zymar (Gatifloxacin 0.3%) shows excellent Gram-negative activity against Serratia marcescens and Pseudomonas aeruginosa in a New Zealand White rabbit keratitis model. Cornea 2007, 26, 585–588. [Google Scholar] [CrossRef]
- Hariprasad, S.M.; Shah, G.K.; Chi, J.; Prince, R.A. Determination of aqueous and vitreous concentration of moxifloxacin 0.5% after delivery via a dissolvable corneal collagen shield device. J. Cataract. Refract. Surg. 2005, 31, 2142–2146. [Google Scholar] [CrossRef]
- Uda, T.; Suzuki, T.; Mitani, A.; Tasaka, Y.; Kawasaki, S.; Mito, T.; Ohashi, Y. Ocular penetration and efficacy of levofloxacin using different drug-delivery techniques for the prevention of endophthalmitis in rabbit eyes with posterior capsule rupture. J. Ocul. Pharmacol. Ther. 2014, 30, 333–339. [Google Scholar] [CrossRef]
- Burgalassi, S.; Monti, D.; Tampucci, S.; Chetoni, P. In vitro evaluation of some parameters involved in mucoadhesion of aqueous polymeric dispersions. Pharm. Dev. Technol. 2015, 20, 927–934. [Google Scholar] [CrossRef]
- Nair, A.B.; Shah, J.; Jacob, S.; Al-Dhubiab, B.E.; Sreeharsha, N.; Morsy, M.A.; Gupta, S.; Attimarad, M.; Shinu, P.; Venugopala, K.N. Experimental design, formulation and in vivo evaluation of a novel topical in situ gel system to treat ocular infections. PLoS ONE 2021, 16, e248857. [Google Scholar] [CrossRef]
- Hosny, K.M. Optimization of gatifloxacin liposomal hydrogel for enhanced transcorneal permeation. J. Liposome Res. 2010, 20, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Caretti, L.; La Gloria, V.A.; Piermarocchi, R.; Badin, G.; Verzola, G.; Masara, F.; Scalora, T.; Monterosso, C. Efficacy of carbomer sodium hyaluronate trehalose vs hyaluronic acid to improve tear film instability and ocular surface discomfort after cataract surgery. Clin. Ophthalmol. 2019, 13, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Yang, Y.; Tang, H. Gatifloxacin-Containing Ophthalmic Gel and Preparation Method Thereof. U.S. Patent 8,901,131, 2 December 2014. [Google Scholar]
- Nedelman, J.R.; Gibiansky, E.; Lau, D.T. Applying Bailer’s method for AUC confidence intervals to sparse sampling. Pharm. Res. 1995, 12, 124–128. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).