A Survey on Knowledge, Attitude, and Practices of Large-Animal Farmers towards Antimicrobial Use, Resistance, and Residues in Mymensingh Division of Bangladesh
Abstract
:1. Introduction
2. Results
2.1. Socio-Demographic Characteristics of the Respondents
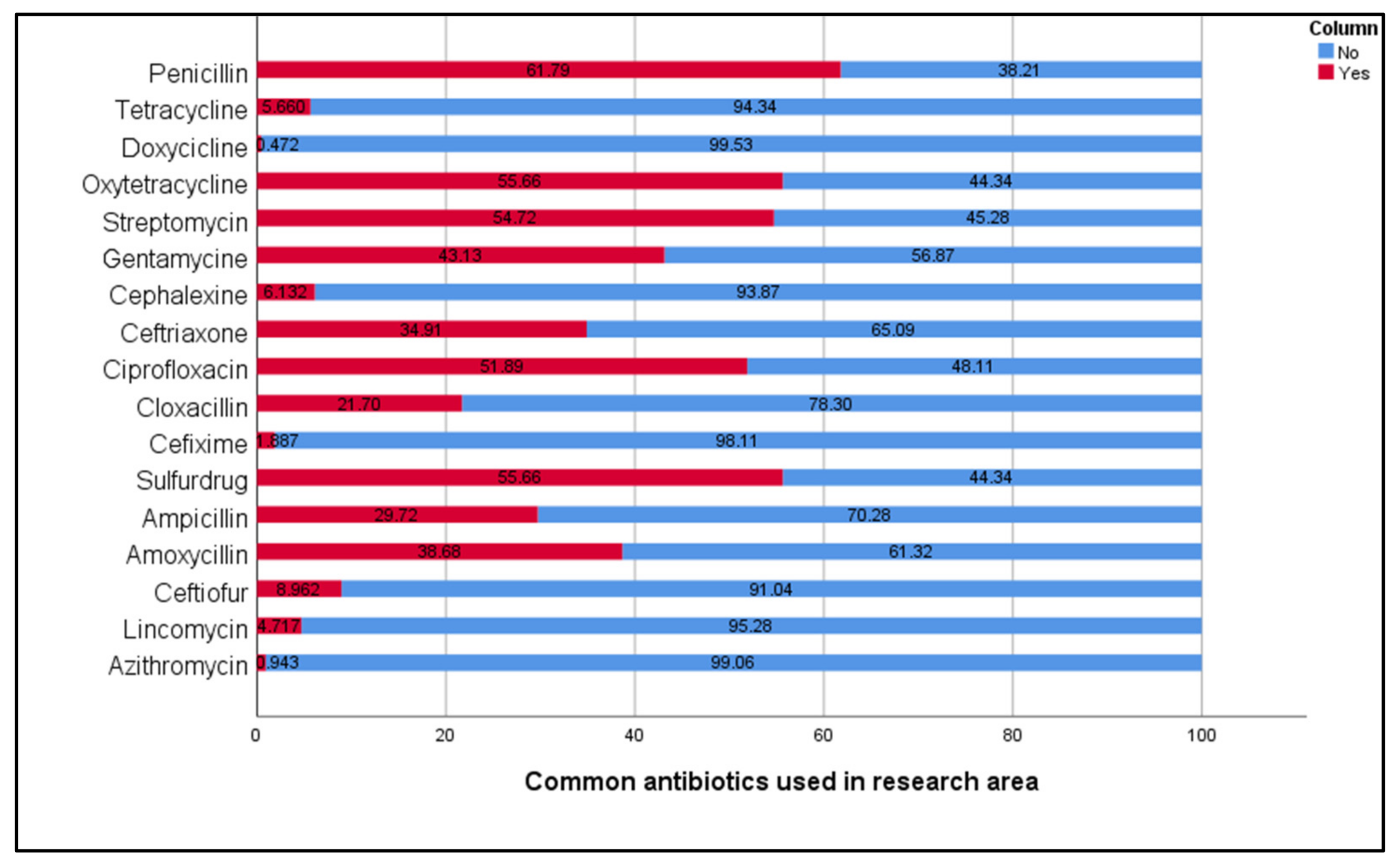
2.2. Common Antibiotics Used in the Study Area
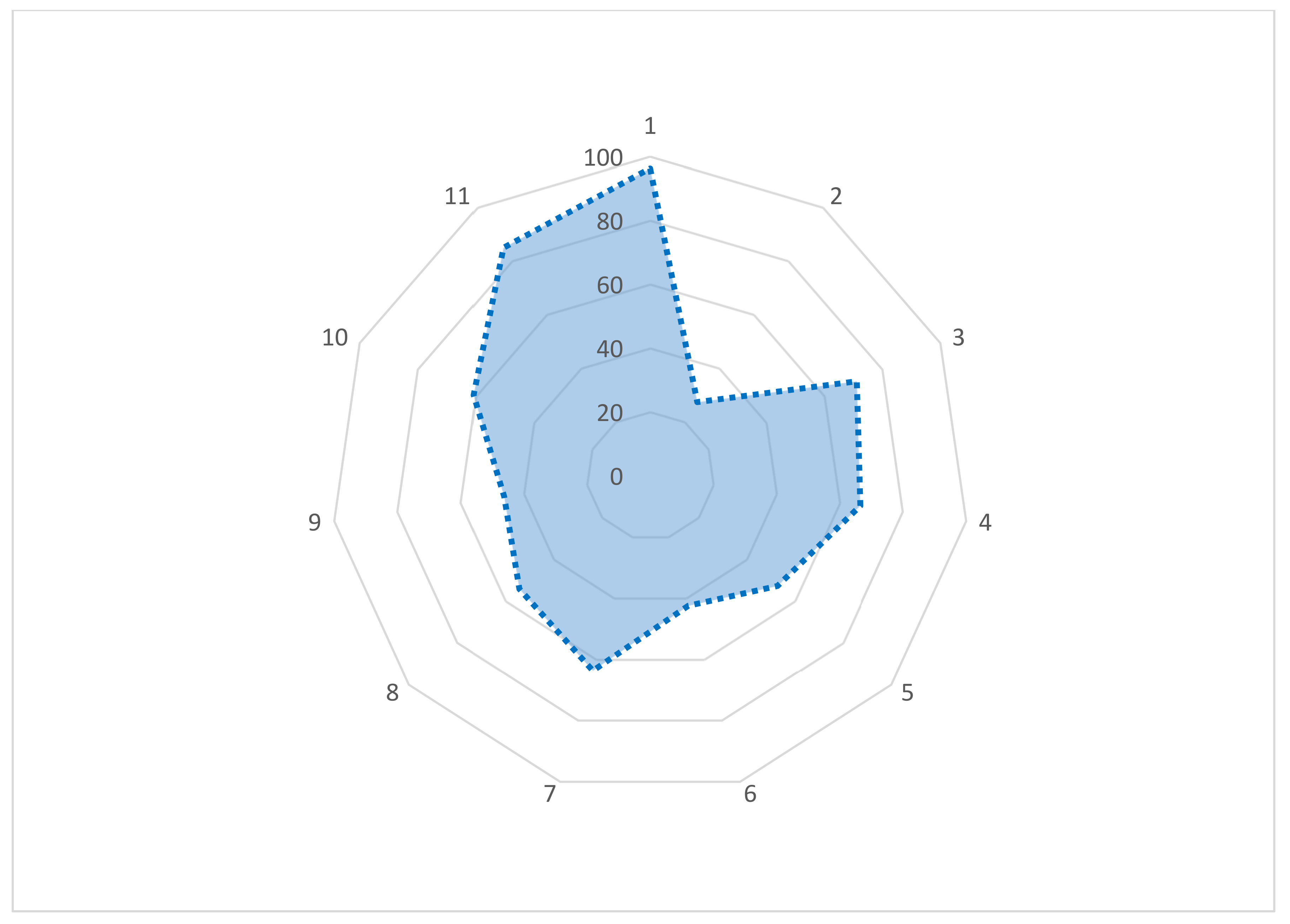
2.3. Knowledge of Large-Animal Farmers on AMU, AMR, and Antimicrobial Residue
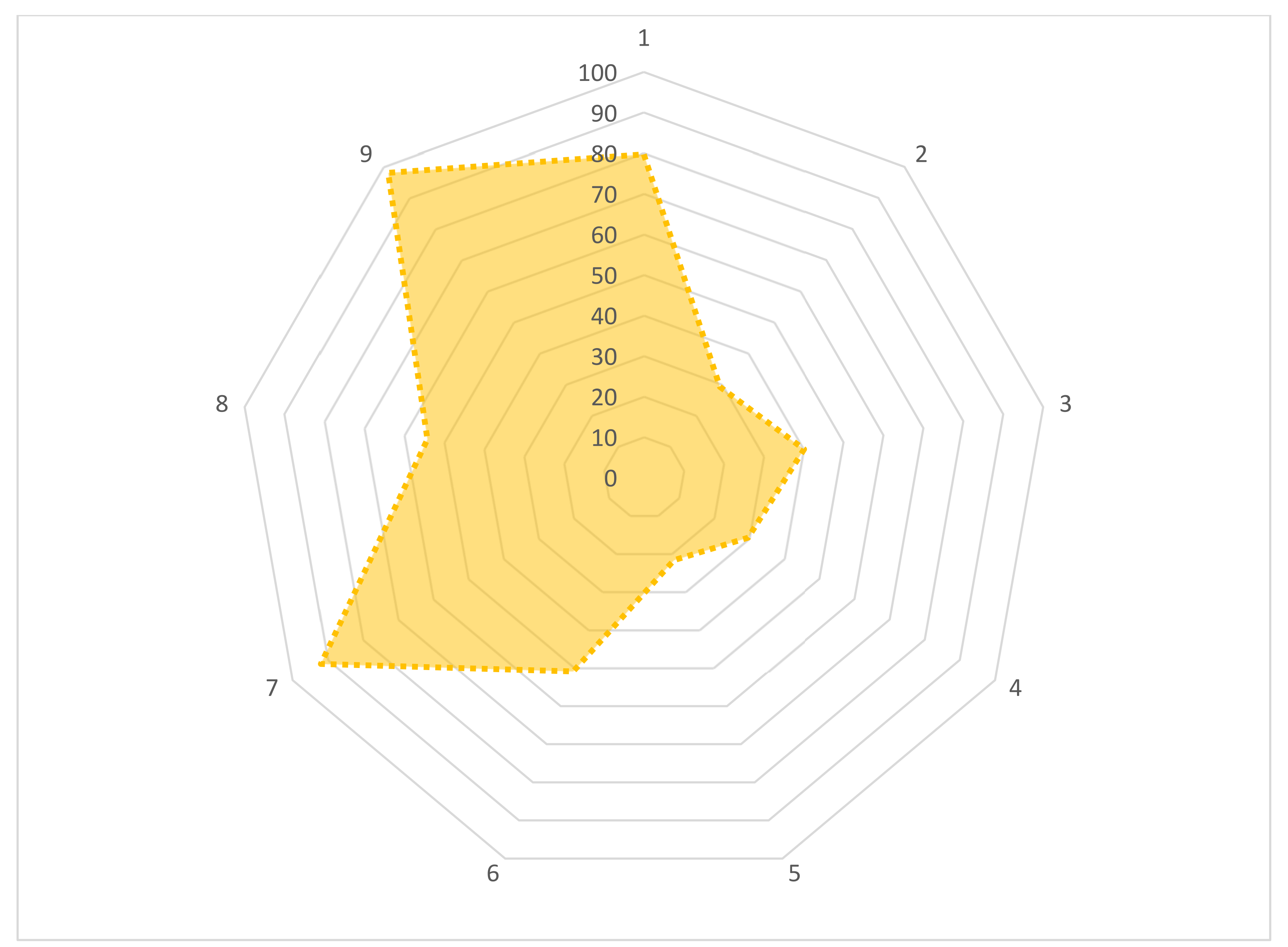
2.4. Attitudes of Large-Animal Farmers on AMU, AMR, and Antimicrobial Residue
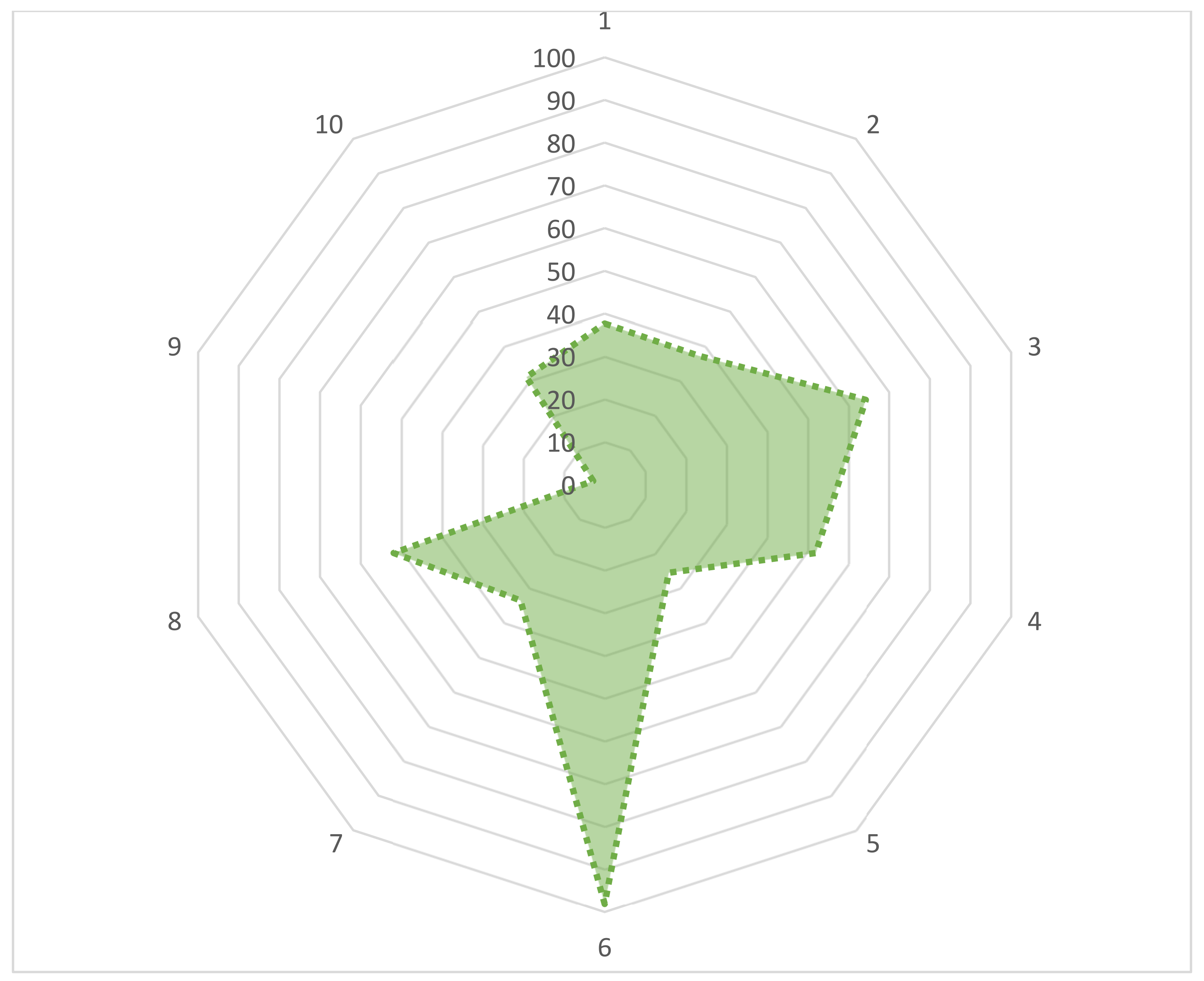
2.5. Practices of Large-Animal Farmers on AMU, AMR, and Antimicrobial Residue
2.6. Differences in Large-Animal Farmers’ Knowledge, Attitudes, and Practices
2.7. Differences in Respondents’ Knowledge, Attitudes, and Practices
2.8. Relationship among Knowledge, Attitudes, and Practices of AMU and AMR
3. Discussion
3.1. The Knowledge of Large-Animal Farmers Regarding AMU and AMR
3.2. The Attitudes of Large-Animal Farmers Regarding AMU and AMR
3.3. The Practices of Large-Animal Farmers Regarding AMU and AMR
3.4. Association of Socio-Demographic Data with KAP of Large-Animal Farmers
3.5. Limitations of the Study
4. Materials and Methods
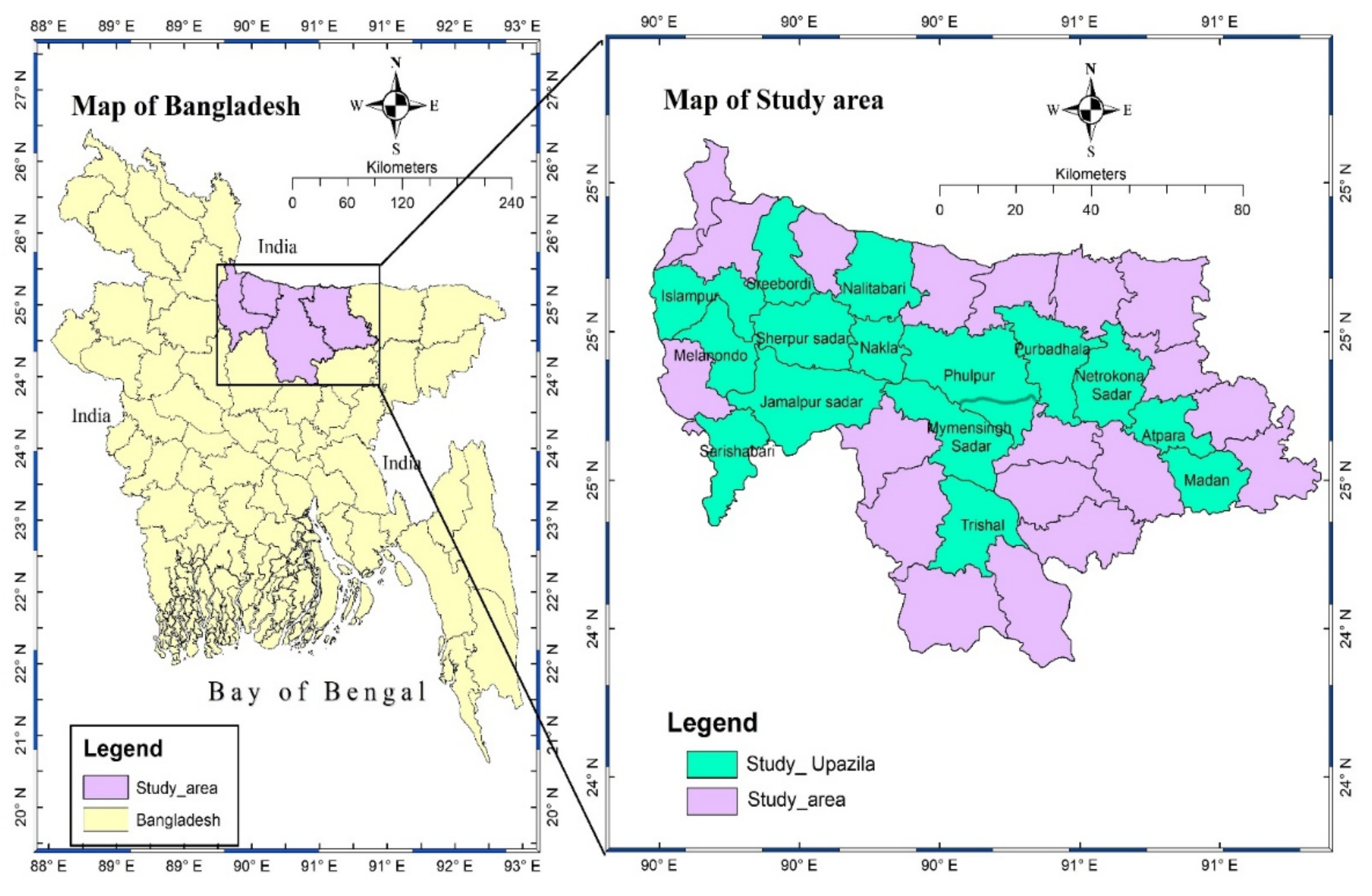
4.1. Study Location and Study Period
4.2. Study Design and Sampling
4.3. Preparation of Questionnaire
4.4. Questionnaire Administration
4.5. Data Management and Analysis
4.6. Pearson Chi-Square Test
4.7. Multivariable Logistic Regression Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Antimicrobial Resistance. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 17 November 2021).
- Singh, S.; Shukla, S.; Tandia, N.; Kumar, N.; Paliwal, R. Antibiotic Residues: A Global Challenge. Pharma Sci. Monit. 2014, 5, 184–197. [Google Scholar]
- Oliver, S.P.; Murinda, S.E.; Jayarao, B.M. Impact of antibiotic use in adult dairy cows on antimicrobial resistance of veterinary and human pathogens: A comprehensive review. Foodborne Pathog. Dis. 2011, 8, 337–355. [Google Scholar] [PubMed]
- Hall, D.C.; Ehui, S.; Delgado, C. The livestock revolution, food safety, and small-scale farmers: Why they matter to us all. J. Agric. Environ. Ethics 2004, 17, 425–444. [Google Scholar]
- Marshall, B.M.; Levy, S.B. Food Animals and Antimicrobials: Impacts on Human Health. Clin. Microbiol. Rev. 2011, 24, 718–733. [Google Scholar] [CrossRef] [Green Version]
- Graham, D.W.; Bergeron, G.; Bourassa, M.W.; Dickson, J.; Gomes, F.; Howe, A.; Kahn, L.H.; Morley, P.S.; Scott, H.M.; Simjee, S.; et al. Complexities in understanding antimicrobial resistance across domesticated animal, human, and environmental systems. Ann. N. Y. Acad. Sci. 2019, 1441, 17–30. [Google Scholar] [CrossRef]
- ECDC; EFSA; EMA. ECDC/EFSA/EMA first joint report on the integrated analysis of the consumption of antimicrobial agents and occurrence of antimicrobial resistance in bacteria from humans and food-producing animals. EFSA J. 2015, 13, 4006. [Google Scholar] [CrossRef]
- Robinson, T.P.; Bu, D.P.; Carrique-Mas, J.; Fèvre, E.M.; Gilbert, M.; Grace, D.; Hay, S.I.; Jiwakanon, J.; Kakkar, M.; Kariuki, S.; et al. Antibiotic resistance is the quintessential One Health issue. Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 377–380. [Google Scholar] [CrossRef]
- WHO. Antimicrobial Resistance: Global Report on Surveillance. 2014. Available online: https://reliefweb.int/report/world/antimicrobial-resistance-global-report-surveillance-2014?gclid=EAIaIQobChMIg4KG7Lax9gIVySFgCh1odA0lEAAYASAAEgL6tfD_BwE (accessed on 30 April 2014).
- Davies, J.; Davies, D. Origins and evolution of antibiotic resistance. Microbiol. Mol. Biol. Rev. 2010, 74, 417–433. [Google Scholar]
- Shaikh, S.; Fatima, J.; Shakil, S.; Rizvi, S.M.D.; Kamal, M.A. Antibiotic resistance and extended spectrum beta-lactamases: Types, epidemiology and treatment. Saudi J. Biol. Sci. 2015, 22, 90–101. [Google Scholar] [CrossRef] [Green Version]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations: Review on Antimicrobial Resistance; Government of the United Kingdom: London, UK, 2016. [Google Scholar]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance—The need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, A.M.; Gareib, M.M. Detection of some antibiotics residues in chicken meat and chicken luncheon. Egypt. J. Chem. Environ. Health 2016, 2, 315–323. [Google Scholar]
- Darwish, W.S.; Eldaly, E.A.; El-Abbasy, M.T.; Ikenaka, Y.; Nakayama, S.; Ishizuka, M. Antibiotic residues in food: The African scenario. Jpn. J. Vet. Res. 2013, 61, S13–S22. [Google Scholar] [PubMed]
- Gupta, R.C. Veterinary Toxicology: Basic and Clinical Principles; Academic Press: Cambridge, MA, USA, 2012. [Google Scholar]
- WHO. Evaluation of certain veterinary drug residues in food. WHO Tech. Rep. Ser. 2012, 969, 1–101. [Google Scholar]
- Ngangom, B.L.; Tamunjoh, S.S.A.; Boyom, F.F. Antibiotic residues in food animals: Public health concern. Acta Ecol. Sin. 2019, 39, 411–415. [Google Scholar]
- Hussein, M.A.; Khalil, S. Screening of some antibiotics and anabolic steroids residues in broiler fillet marketed in El-Sharkia governorate. Life Sci. J. 2013, 10, 2111–2118. [Google Scholar]
- Normanno, G.; La Salandra, G.; Dambrosio, A.; Quaglia, N.; Corrente, M.; Parisi, A.; Santagada, G.; Firinu, A.; Crisetti, E.; Celano, G. Occurrence, characterization and antimicrobial resistance of enterotoxigenic Staphylococcus aureus isolated from meat and dairy products. Int. J. Food Microbiol. 2007, 115, 290–296. [Google Scholar]
- Laxminarayan, R.; Malani, A. Extending the Cure: Policy Responses to the Growing Threat of Antibiotic Resistance; 1933115572; Resources for the Future: Washington, DC, USA, 2007. [Google Scholar]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar]
- Sutradhar, K.B.; Saha, A.; Huda, N.H.; Uddin, R. Irrational use of antibiotics and antibiotic resistance in southern rural Bangladesh: Perspectives from both the physicians and patients. Annu. Res. Rev. Biol. 2014, 4, 1421–1430. [Google Scholar]
- Al Amin, M.; Hoque, M.N.; Siddiki, A.Z.; Saha, S.; Kamal, M.M. Antimicrobial resistance situation in animal health of Bangladesh. Vet. World 2020, 13, 2713–2727. [Google Scholar] [CrossRef]
- Goff, D.A.; Kullar, R.; Goldstein, E.J.C.; Gilchrist, M.; Nathwani, D.; Cheng, A.C.; Cairns, K.A.; Escandón-Vargas, K.; Villegas, M.V.; Brink, A.; et al. A global call from five countries to collaborate in antibiotic stewardship: United we succeed, divided we might fail. Lancet Infect. Dis. 2017, 17, e56–e63. [Google Scholar] [CrossRef] [Green Version]
- WHO. Global Action Plan on Antimicrobial Resistance. Geneva. 2015. Available online: https://apps.who.int/iris/handle/10665/193736. (accessed on 5 May 2015).
- Chowdhury, S.; Ghosh, S.; Aleem, M.A.; Parveen, S.; Islam, M.A.; Rashid, M.M.; Akhtar, Z.; Chowdhury, F. Antibiotic Usage and Resistance in Food Animal Production: What Have We Learned from Bangladesh? Antibiotics 2021, 10, 1032. [Google Scholar] [CrossRef] [PubMed]
- Pham-Duc, P.; Cook, M.A.; Cong-Hong, H.; Nguyen-Thuy, H.; Padungtod, P.; Nguyen-Thi, H.; Dang-Xuan, S. Knowledge, attitudes and practices of livestock and aquaculture producers regarding antimicrobial use and resistance in Vietnam. PLoS ONE 2019, 14, e0223115. [Google Scholar]
- Caudell, M.A.; Dorado-Garcia, A.; Eckford, S.; Creese, C.; Byarugaba, D.K.; Afakye, K.; Chansa-Kabali, T.; Fasina, F.O.; Kabali, E.; Kiambi, S. Towards a bottom-up understanding of antimicrobial use and resistance on the farm: A knowledge, attitudes, and practices survey across livestock systems in five African countries. PLoS ONE 2020, 15, e0220274. [Google Scholar]
- Ferdous, J.; Sachi, S.; Noman, Z.A.; Hussani, S.M.A.K.; Sarker, Y.A.; Sikder, M.H. Assessing farmers’ perspective on antibiotic usage and management practices in small-scale layer farms of Mymensingh district, Bangladesh. Vet. World 2019, 12, 1441–1447. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Moffo, F.; Mouliom Mouiche, M.M.; Kochivi, F.L.; Dongmo, J.B.; Djomgang, H.K.; Tombe, P.; Mbah, C.K.; Mapiefou, N.P.; Mingoas, J.-P.K.; Awah-Ndukum, J. Knowledge, attitudes, practices and risk perception of rural poultry farmers in Cameroon to antimicrobial use and resistance. Prev. Vet. Med. 2020, 182, 105087. [Google Scholar] [CrossRef]
- Ahmed, I.; Rabbi, M.B.; Sultana, S. Antibiotic resistance in Bangladesh: A systematic review. Int. J. Infect. Dis. 2019, 80, 54–61. [Google Scholar] [CrossRef] [Green Version]
- Geta, K.; Kibret, M. Knowledge, attitudes and practices of animal farm owners/workers on antibiotic use and resistance in Amhara region, north western Ethiopia. Sci. Rep. 2021, 11, 21211. [Google Scholar] [CrossRef]
- Sawant, A.A.; Sordillo, L.M.; Jayarao, B.M. A Survey on Antibiotic Usage in Dairy Herds in Pennsylvania. J. Dairy Sci. 2005, 88, 2991–2999. [Google Scholar] [CrossRef] [Green Version]
- Higham, L.E.; Deakin, A.; Tivey, E.; Porteus, V.; Ridgway, S.; Rayner, A.C. A survey of dairy cow farmers in the United Kingdom: Knowledge, attitudes and practices surrounding antimicrobial use and resistance. Vet. Rec. 2018, 183, 746. [Google Scholar] [CrossRef]
- Adesokan, H.K.; Akanbi, I.M.; Akanbi, I.O.; Obaweda, R.A. Pattern of antimicrobial usage in livestock animals in south-western Nigeria: The need for alternative plans. Onderstepoort J. Vet. Res. 2015, 82, 1–6. [Google Scholar]
- Eagar, H.; Swan, G.; Van Vuuren, M. A survey of antimicrobial usage in animals in South Africa with specific reference to food animals. J. S. Afr. Vet. Assoc. 2012, 83, 1–8. [Google Scholar]
- Sadiq, M.B.; Syed-Hussain, S.S.; Ramanoon, S.Z.; Saharee, A.A.; Ahmad, N.I.; Mohd Zin, N.; Khalid, S.F.; Naseeha, D.S.; Syahirah, A.A.; Mansor, R. Knowledge, attitude and perception regarding antimicrobial resistance and usage among ruminant farmers in Selangor, Malaysia. Prev. Vet. Med. 2018, 156, 76–83. [Google Scholar] [CrossRef] [PubMed]
- WHO. Critically Important Antimicrobials for Human Medicine; World Health Organization: Geneva, Switzerland, 2018; ISBN 978-92-4-151552-8. [Google Scholar]
- Asredie, T.; Engdaw, T.A. Antimicrobial residues in cow milk and its public health significance. World J. Dairy Food Sci. 2015, 10, 147–153. [Google Scholar]
- Berghiche, A.; Khenenou, T.; Labiad, I. Antibiotics resistance in broiler chicken from the farm to the table in Eastern Algeria. J. World’s Poult. Res. 2018, 8, 95–99. [Google Scholar]
- Rayner, A.C.; Higham, L.E.; Gill, R.; Michalski, J.-P.; Deakin, A. A survey of free-range egg farmers in the United Kingdom: Knowledge, attitudes and practices surrounding antimicrobial use and resistance. Vet. Anim. Sci. 2019, 8, 100072. [Google Scholar] [CrossRef]
- Gemeda, B.A.; Amenu, K.; Magnusson, U.; Dohoo, I.; Hallenberg, G.S.; Alemayehu, G.; Desta, H.; Wieland, B. Antimicrobial Use in Extensive Smallholder Livestock Farming Systems in Ethiopia: Knowledge, Attitudes, and Practices of Livestock Keepers. Front. Vet. Sci. 2020, 7, 55. [Google Scholar] [CrossRef]
- Ozturk, Y.; Celik, S.; Sahin, E.; Acik, M.N.; Cetinkaya, B. Assessment of Farmers’ Knowledge, Attitudes and Practices on Antibiotics and Antimicrobial Resistance. Animals 2019, 9, 653. [Google Scholar]
- Hassan, M.M.; Kalam, M.A.; Alim, M.A.; Shano, S.; Nayem, M.R.; Badsha, M.R.; Al Mamun, M.A.; Hoque, A.; Tanzin, A.Z.; Nath, C.; et al. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Commercial Poultry Farmers in Bangladesh. Antibiotics 2021, 10, 784. [Google Scholar] [CrossRef]
- Imam, T.; Gibson, J.S.; Foysal, M.; Das, S.B.; Gupta, S.D.; Fournié, G.; Hoque, M.A.; Henning, J. A Cross-Sectional Study of Antimicrobial Usage on Commercial Broiler and Layer Chicken Farms in Bangladesh. Front. Vet. Sci. 2020, 7, 576113. [Google Scholar] [CrossRef]
- Khan, S.A.; Imtiaz, M.A.; Sayeed, M.A.; Shaikat, A.H.; Hassan, M.M. Antimicrobial resistance pattern in domestic animal-wildlife-environmental niche via the food chain to humans with a Bangladesh perspective; a systematic review. BMC Vet. Res. 2020, 16, 302. [Google Scholar]
- Gebeyehu, D.T.; Bekele, D.; Mulate, B.; Gugsa, G.; Tintagu, T. Knowledge, attitude and practice of animal producers towards antimicrobial use and antimicrobial resistance in Oromia zone, north eastern Ethiopia. PLoS ONE 2021, 16, e0251596. [Google Scholar] [CrossRef]
- Guido, D.M.; Crovato, S.; Pinto, A.; Dorotea, T.; Mascarello, G.; Brunetta, R.; Agnoletti, F.; Bonfanti, L. Farmers’ attitudes towards antimicrobial use and awareness of antimicrobial resistance: A comparative study among turkey and rabbit farmers. Ital. J. Anim. Sci. 2019, 18, 194–201. [Google Scholar] [CrossRef] [Green Version]
- Munengwa, A.; Nation, C.; Alban, M. Perceptions and practices on antimicrobial use by the farmers of the Chikomba District, Zimbabwe. Aceh J. Anim. Sci. 2020, 5, 73–80. [Google Scholar]
- Roess, A.A.; Winch, P.J.; Akhter, A.; Afroz, D.; Ali, N.A.; Shah, R.; Begum, N.; Seraji, H.R.; El Arifeen, S.; Darmstadt, G.L.; et al. Household Animal and Human Medicine Use and Animal Husbandry Practices in Rural Bangladesh: Risk Factors for Emerging Zoonotic Disease and Antibiotic Resistance. Zoonoses Public Health 2015, 62, 569–578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ekakoro, J.E.; Caldwell, M.; Strand, E.B.; Okafor, C.C. Drivers, alternatives, knowledge, and perceptions towards antimicrobial use among Tennessee beef cattle producers: A qualitative study. BMC Vet. Res. 2019, 15, 16. [Google Scholar] [CrossRef]
- Alhaji, N.B.; Haruna, A.E.; Muhammad, B.; Lawan, M.K.; Isola, T.O. Antimicrobials usage assessments in commercial poultry and local birds in North-central Nigeria: Associated pathways and factors for resistance emergence and spread. Prev. Vet. Med. 2018, 154, 139–147. [Google Scholar] [CrossRef]
- Amaechi, N. A survey on antibiotic usage in pigs and poultry birds in Abia State, Nigeria. Glob. J. Med. Res. 2014, 14, 10–13. [Google Scholar]
- Speksnijder, D.C.; Graveland, H.; Eijck, I.A.J.M.; Schepers, R.W.M.; Heederik, D.J.J.; Verheij, T.J.M.; Wagenaar, J.A. Effect of structural animal health planning on antimicrobial use and animal health variables in conventional dairy farming in the Netherlands. J. Dairy Sci. 2017, 100, 4903–4913. [Google Scholar] [CrossRef] [Green Version]
- Dankar, I.; Hassan, H.; Serhan, M. Knowledge, attitudes, and perceptions of dairy farmers regarding antibiotic use: Lessons from a developing country. J. Dairy Sci. 2022, 105, 1519–1532. [Google Scholar] [CrossRef]
- Abdelfattah, E.M.; Ekong, P.S.; Okello, E.; Williams, D.R.; Karle, B.M.; Rowe, J.D.; Marshall, E.S.; Lehenbauer, T.W.; Aly, S.S. 2019 Survey of Antimicrobial Drug Use and Stewardship Practices in Adult Cows on California Dairies: Post Senate Bill 27. Microorganisms 2021, 9, 1507. [Google Scholar] [CrossRef]
- Abdelfattah, A.; Freilich, S.; Bartuv, R.; Zhimo, V.Y.; Kumar, A.; Biasi, A.; Salim, S.; Feygenberg, O.; Burchard, E.; Dardick, C. Global analysis of the apple fruit microbiome: Are all apples the same? Environ. Microbiol. 2021, 23, 6038–6055. [Google Scholar] [PubMed]
- Green, A.L.; Carpenter, L.R.; Edmisson, D.E.; Lane, C.D.; Welborn, M.G.; Hopkins, F.M.; Bemis, D.A.; Dunn, J.R. Producer attitudes and practices related to antimicrobial use in beef cattle in Tennessee. J. Am. Vet. Med. Assoc. 2010, 237, 1292–1298. [Google Scholar] [PubMed]
- Boamah, V.; Agyare, C.; Odoi, H.; Dalsgaard, A. Practices and Factors Influencing the Use of Antibiotics in Selected Poultry Farms in Ghana. J. Antimicrob. 2016, 2, 120. [Google Scholar] [CrossRef]
- Hassan, M.M. Scenario of Antibiotic Resistance in Developing Countries. In Antimicrobial Resistance—A One Health Perspective; IntechOpen: London, UK, 2020. [Google Scholar]
- Hedman, H.D.; Vasco, K.A.; Zhang, L. A Review of Antimicrobial Resistance in Poultry Farming within Low-Resource Settings. Animals 2020, 10, 1264. [Google Scholar]
- Dyar, O.J.; Zhang, T.; Peng, Y.; Sun, M.; Sun, C.; Yin, J.; Ding, L.; Sun, C.; Wang, Y.; Sun, Q.; et al. Knowledge, attitudes and practices relating to antibiotic use and antibiotic resistance among backyard pig farmers in rural Shandong province, China. Prev. Vet. Med. 2020, 175, 104858. [Google Scholar] [CrossRef]
- Kalam, M.; Alim, M.; Shano, S.; Nayem, M.; Khan, R.; Badsha, M.; Mamun, M.; Al, A.; Hoque, A.; Tanzin, A.Z. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh. Vet. Sci. 2021, 8, 111. [Google Scholar]
- Harbarth, S.; Balkhy, H.H.; Goossens, H.; Jarlier, V.; Kluytmans, J.; Laxminarayan, R.; Saam, M.; Van Belkum, A. Pittet D and for the World Healthcare-Associated Infections Resistance Forum, p. Antimicrobial resistance: One world, one fight! Antimicrob. Resist. Infect. Control 2015, 4, 49. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, S.M.; Naher, N.; Hossain, T.; Rawal, L.B. Exploring the status of retail private drug shops in Bangladesh and action points for developing an accredited drug shop model: A facility based cross-sectional study. J. Pharm. Policy Pract. 2017, 10, 21. [Google Scholar] [CrossRef] [Green Version]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 47. [Google Scholar] [CrossRef]
- Jones, P.J.; Marier, E.A.; Tranter, R.B.; Wu, G.; Watson, E.; Teale, C.J. Factors affecting dairy farmers’ attitudes towards antimicrobial medicine usage in cattle in England and Wales. Prev. Vet. Med. 2015, 121, 30–40. [Google Scholar] [CrossRef]
- Cho, E.; Kim, S. Cronbach’s Coefficient Alpha: Well Known but Poorly Understood. Organ. Res. Methods 2015, 18, 207–230. [Google Scholar]
- Holt, H.R.; Eltholth, M.M.; Hegazy, Y.M.; El-Tras, W.F.; Tayel, A.A.; Guitian, J. Brucella spp. infection in large ruminants in an endemic area of Egypt: Cross-sectional study investigating seroprevalence, risk factors and livestock owner’s knowledge, attitudes and practices (KAPs). BMC Public Health 2011, 11, 341. [Google Scholar]
- Hosmer, D.W.; Hosmer, T.; Le Cessie, S.; Lemeshow, S. A comparison of goodness-of-fit tests for the logistic regression model. Stat. Med. 1997, 16, 965–980. [Google Scholar] [PubMed]
| Characteristics | Category | Frequency (Number) | Percentage (%) |
|---|---|---|---|
| District | Mymensingh | 53 | 25 |
| Sherpur | 52 | 24.5 | |
| Jamalpur | 54 | 25.5 | |
| Netrokona | 53 | 25 | |
| Sex | Male | 182 | 85.8 |
| Female | 30 | 14.2 | |
| Age | 18–30 years | 79 | 37.3 |
| 31–40 years | 71 | 33.5 | |
| 41–50 years | 42 | 19.8 | |
| >50 years | 20 | 9.4 | |
| Education | Illiterate | 43 | 20.3 |
| PSC | 45 | 21.2 | |
| JSC | 22 | 10.4 | |
| SSC | 31 | 14.6 | |
| HSC | 41 | 19.3 | |
| Graduate | 20 | 9.4 | |
| Masters | 10 | 4.7 | |
| Training | Not received | 110 | 51.9 |
| Received | 102 | 48.1 | |
| Farm type | Dairy | 96 | 45.3 |
| Buffalo | 20 | 9.4 | |
| Goat | 48 | 22.6 | |
| Sheep | 16 | 7.5 | |
| Beef Fattening | 32 | 15.1 | |
| Farm population size (number of animals on individual farm) | 3 to 5 | 45 | 21.2 |
| 6 to 10 | 93 | 43.9 | |
| 11 to 20 | 48 | 22.6 | |
| >20 | 26 | 12.3 |
| Characteristics | Category | Knowledge | Chi Square | Attitude | Chi Square | Practice | Chi Square | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Adequate | Inadequate | p-Value | Desirable | Undesirable | p-Value | Appropriate | In Appropriate | p-Value | ||
| District | Mymensingh | 21 (39.6%) | 32 (64.4%) | 0.786 | 23 (43.4%) | 30 (56.6%) | 0.908 | 11 (20.8%) | 42 (79.2%) | 0.982 |
| Sherpur | 24 (46.2%) | 28 (53.8%) | 24 (46.2%) | 28 (53.8%) | 12 (23.1%) | 40 (76.9%) | ||||
| Jamalpur | 20 (37%) | 34 (63%) | 22 (40.7%) | 32 (59.3%) | 11 (20.4%) | 43 (79.6%) | ||||
| Netrokona | 23 (43.4%) | 30 (56.6%) | 21 (39.6%) | 32 (60.4%) | 12 (22.6%) | 41 (77.4%) | ||||
| Sex | Male | 83 (45.6%) | 99 (54.4%) | 0.003 | 86 (47.3%) | 96 (52.7%) | <0.001 | 40 (22%) | 142 (78%) | 0.808 |
| Female | 5 (16.7%) | 25 (83.3%) | 4 (13.3%) | 26 (86.7%) | 6 (20.0%) | 24 (80.0%) | ||||
| Age | 18 to 30 years | 33 (41.8%) | 46 (58.2%) | 0.413 | 32 (40.5%) | 47 (59.5%) | 0.682 | 11 (13.9%) | 68 (86.1%) | 0.044 |
| 31 t0 40 years | 34 (47.9%) | 37 (52.1%) | 34 (47.9%) | 37 (52.1%) | 23 (32.4%) | 48 (67.6%) | ||||
| 41 to 50 years | 15 (35.7%) | 27 (64.3%) | 17 (40.5%) | 25 (59.5%) | 9 (21.4%) | 33 (78.6%) | ||||
| >50 years | 6 (30%) | 14 (70%) | 7 (35%) | 13 (65%) | 3 (15%) | 17 (85%) | ||||
| Education | Illiterate | 2 (4.7%) | 41 (95.3%) | <0.001 | 8 (18.6%) | 35 (81.4%) | <0.001 | 2 (4.7%) | 41 (95.3%) | <0.001 |
| PSC | 6 (13.3%) | 39 (86.7%) | 10 (22.2%) | 35 (77.8%) | 5 (1.1%) | 40 (88.9%) | ||||
| JSC | 13 (69.1%) | 9 (40.9%) | 10 (45.5%) | 12 (54.5%) | 3 (13.6%) | 19 (86.4%) | ||||
| SSC | 16 (51.6%) | 15 (48.4%) | 14 (45.2%) | 17 (54.8%) | 7 (22.6%) | 19 (86.4%) | ||||
| HSC | 26 (63.4%) | 15 (36.6%) | 25 (61.0%) | 16 (39%) | 12 (29.3%) | 29 (70.7%) | ||||
| Graduate | 17 (85%) | 3 (15%) | 14 (70%) | 6 (30%) | 10 (50%) | 10 (50%) | ||||
| Masters | 8 (80%) | 2 (20%) | 9 (90%) | 1 (10%) | 7 (70%) | 3 (3%) | ||||
| Training | Not received | 19 (17.3%) | 91 (82.7%) | <0.001 | 20 (18.2%) | 90 (81.8%) | <0.001 | 3 (2.7%) | 107 (97.3%) | <0.001 |
| Received | 69 (67.6%) | 33 (32.4%) | 70 (68.6%) | 32 (31.4%) | 43 (42.2%) | 59 (57.8%) | ||||
| Farm type | Dairy | 43 (44.8%) | 53 (55.2%) | 0.065 | 46 (47.9%) | 50 (52.1%) | 0.028 | 26 (27.1%) | 70 (72.9%) | 0.065 |
| Buffalo | 6 (30%) | 14 (70%) | 7 (35%) | 13 (65%) | 1 (5%) | 19 (95%) | ||||
| Goat | 14 (29.2%) | 34 (70.8%) | 14 (29.2%) | 34 (70.8%) | 7 (14.6%) | 41 (85.4%) | ||||
| Sheep | 6 (37.5%) | 10 (62.10%) | 4 (25%) | 12 (75%) | 2 (12.5%) | 14 (87.5%) | ||||
| Beef Fattening | 19 (59.4%) | 13 (40.6%) | 19 (59.4%) | 13 (40.6%) | 10 (31.3%) | 22 (68.8%) | ||||
| Farm size | 3 to 5 | 9 (20%) | 36 (80%) | <0.001 | 8 (17.8%) | 37 (82.2%) | <0.001 | 2 (4.4%) | 43 (95.6%) | <0.001 |
| 6 to 10 | 29 (31.2%) | 64 (68.8%) | 31 (33.3%) | 62 (66.7%) | 7 (7.5%) | 86 (92.5%) | ||||
| 11 to 20 | 28 (58.3%) | 20 (41.7%) | 27 (56.3%) | 21 (43.8%) | 19 (39.6%) | 29 (60.4%) | ||||
| >20 | 22 (84.6%) | 4 (15.4%) | 24 (92.3%) | 2 (7.7%) | 18 (69.2%) | 8 (30.8%) | ||||
| Variable | Category | Knowledge | Attitude | Practice | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio (Exp. B) | 95% C.I | Odds Ratio (Exp. B) | 95% C.I | Odds Ratio (Exp. B) | 95% C.I | |||||
| Lower | Higher | Lower | Higher | Lower | Higher | |||||
| Sex | Female | 1.000 | 1.000 | 1.000 | ||||||
| Male | 4.192 | 1.537 | 11.435 | 5.823 | 1.954 | 17.356 | 1.127 | 0.431 | 2.946 | |
| Age | 18–30 years | 1.000 | 1.000 | 1.000 | ||||||
| 31–40 years | 1.281 | 0.672 | 2.443 | 1.350 | 0.707 | 2.578 | 2.962 | 1.320 | 6.645 | |
| 41–50 years | 0.774 | 0.357 | 1.678 | 0.999 | 0.466 | 2.141 | 1.686 | 0.636 | 4.466 | |
| >50 years | 0.597 | 0.208 | 1.717 | 0.791 | 0.284 | 2.199 | 1.091 | 0.274 | 4.348 | |
| Education | Illiterate | 1.000 | 1.000 | 1.000 | ||||||
| PSC | 1.123 | 0.288 | 4.369 | 1.250 | 0.441 | 3.54 | 2.562 | 0.470 | 13.981 | |
| JSC | 1.987 | 0.470 | 8.394 | 3.646 | 1.169 | 11.373 | 3.237 | 0.499 | 21.003 | |
| SSC | 3.231 | 0.835 | 12.496 | 3.603 | 1.268 | 10.236 | 5.979 | 1.148 | 31.141 | |
| HSC | 2.816 | 0.799 | 9.928 | 6.836 | 2.535 | 18.43 | 8.483 | 1.764 | 40.801 | |
| Graduate | 2.045 | 0.430 | 9.717 | 10.208 | 2.994 | 34.807 | 20.500 | 3.866 | 108.698 | |
| Masters | 2.513 | 0.401 | 15.746 | 39.375 | 4.345 | 356.834 | 47.833 | 6.734 | 339.766 | |
| Training | Not received | 1.000 | 1.000 | 1.000 | ||||||
| Received | 10.014 | 5.252 | 19.094 | 9.844 | 5.19 | 18.67 | 25.994 | 7.730 | 87.414 | |
| Farm size | 3 to 5 | 1.000 | 1.000 | 1.000 | ||||||
| 6 to 10 | 1.840 | 0.569 | 5.950 | 2.313 | 0.962 | 5.561 | 1.750 | 0.349 | 8.786 | |
| 11 to 20 | 2.515 | 0.623 | 10.157 | 5.946 | 2.292 | 15.43 | 14.086 | 3.046 | 65.134 | |
| >20 | 23.147 | 4.214 | 127.131 | 55.500 | 10.848 | 283.951 | 48.375 | 9.344 | 250.451 | |
| Correlations | Knowledge | Attitude | Practice | ||
|---|---|---|---|---|---|
| Spearman’s rho | Knowledge | Correlation Coefficient | 1.000 | 0.593 ** | 0.393 ** |
| Sig. (2-tailed) | <0.001 | <0.001 | <0.001 | ||
| n | 212 | 212 | 212 | ||
| Attitude | Correlation Coefficient | 0.593 ** | 1.000 | 0.474 ** | |
| Sig. (2-tailed) | <0.001 | <0.001 | <0.001 | ||
| n | 212 | 212 | 212 | ||
| Practice | Correlation Coefficient | 0.393 ** | 0.474 ** | 1.000 | |
| Sig. (2-tailed) | <0.001 | <0.001 | <0.001 | ||
| n | 212 | 212 | 212 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hossain, M.T.; Rafiq, K.; Islam, M.Z.; Chowdhury, S.; Islam, P.; Haque, Z.; Samad, M.A.; Sani, A.A.; Ferdous, M.R.A.; Islam, M.R.; et al. A Survey on Knowledge, Attitude, and Practices of Large-Animal Farmers towards Antimicrobial Use, Resistance, and Residues in Mymensingh Division of Bangladesh. Antibiotics 2022, 11, 442. https://doi.org/10.3390/antibiotics11040442
Hossain MT, Rafiq K, Islam MZ, Chowdhury S, Islam P, Haque Z, Samad MA, Sani AA, Ferdous MRA, Islam MR, et al. A Survey on Knowledge, Attitude, and Practices of Large-Animal Farmers towards Antimicrobial Use, Resistance, and Residues in Mymensingh Division of Bangladesh. Antibiotics. 2022; 11(4):442. https://doi.org/10.3390/antibiotics11040442
Chicago/Turabian StyleHossain, Md. Tarek, Kazi Rafiq, Md. Zahorul Islam, Sharmin Chowdhury, Purba Islam, Ziaul Haque, Mohammed Abdus Samad, Aminatu Abubakar Sani, Most. Rifat Ara Ferdous, Md. Rafiqul Islam, and et al. 2022. "A Survey on Knowledge, Attitude, and Practices of Large-Animal Farmers towards Antimicrobial Use, Resistance, and Residues in Mymensingh Division of Bangladesh" Antibiotics 11, no. 4: 442. https://doi.org/10.3390/antibiotics11040442
APA StyleHossain, M. T., Rafiq, K., Islam, M. Z., Chowdhury, S., Islam, P., Haque, Z., Samad, M. A., Sani, A. A., Ferdous, M. R. A., Islam, M. R., Ahmed, N., Hossen, M. I., Khasruzzman, A. K. M., Bhuiyan, M. K. J., & Hossain, M. T. (2022). A Survey on Knowledge, Attitude, and Practices of Large-Animal Farmers towards Antimicrobial Use, Resistance, and Residues in Mymensingh Division of Bangladesh. Antibiotics, 11(4), 442. https://doi.org/10.3390/antibiotics11040442






