Antibiotic Prescribing in Dutch Daytime and Out-of-Hours General Practice during the COVID-19 Pandemic: A Retrospective Database Study
Abstract
1. Introduction
2. Results
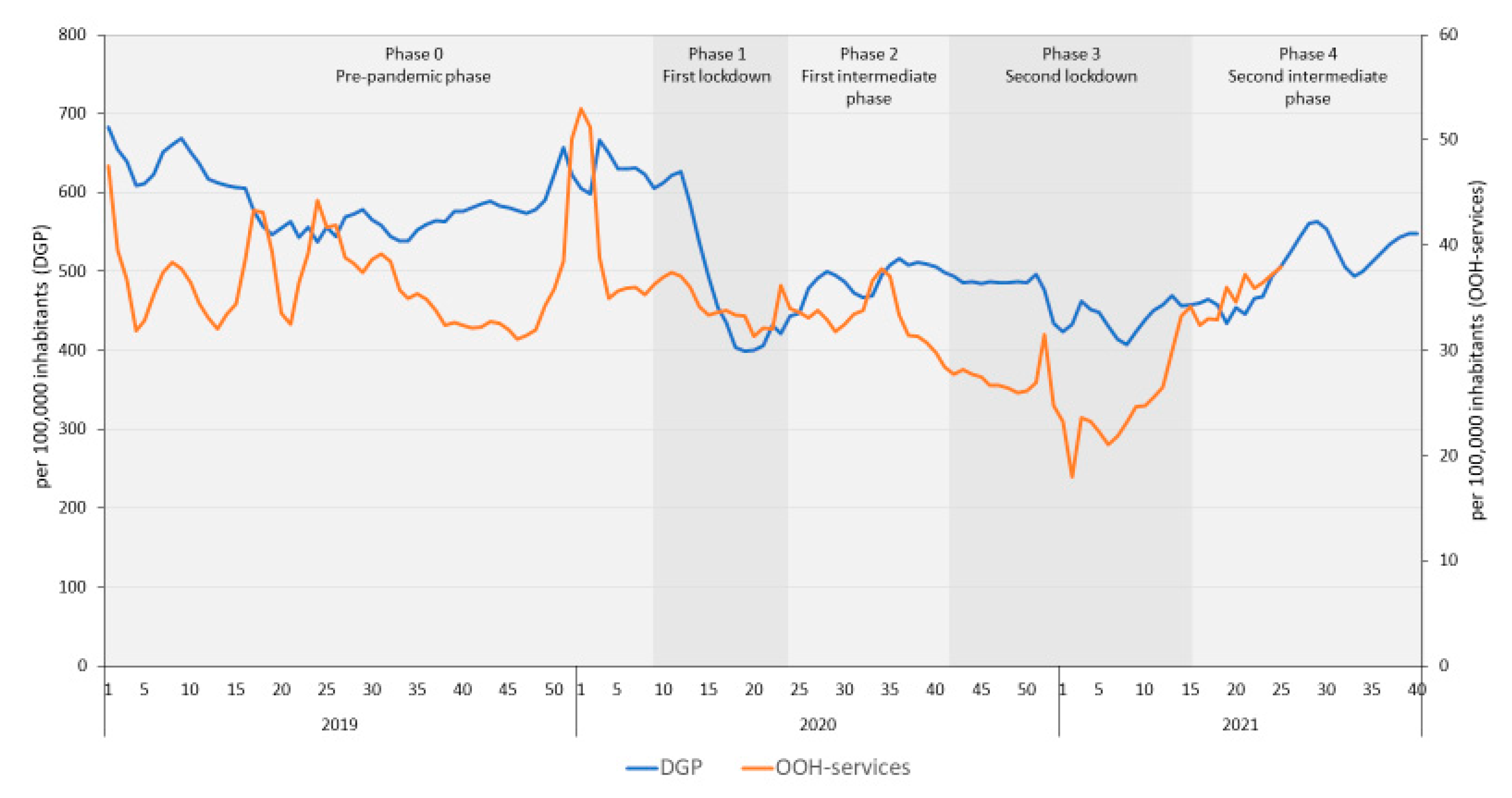
2.1. Trend in Antibiotic Prescribing in DGP and OOH-Services
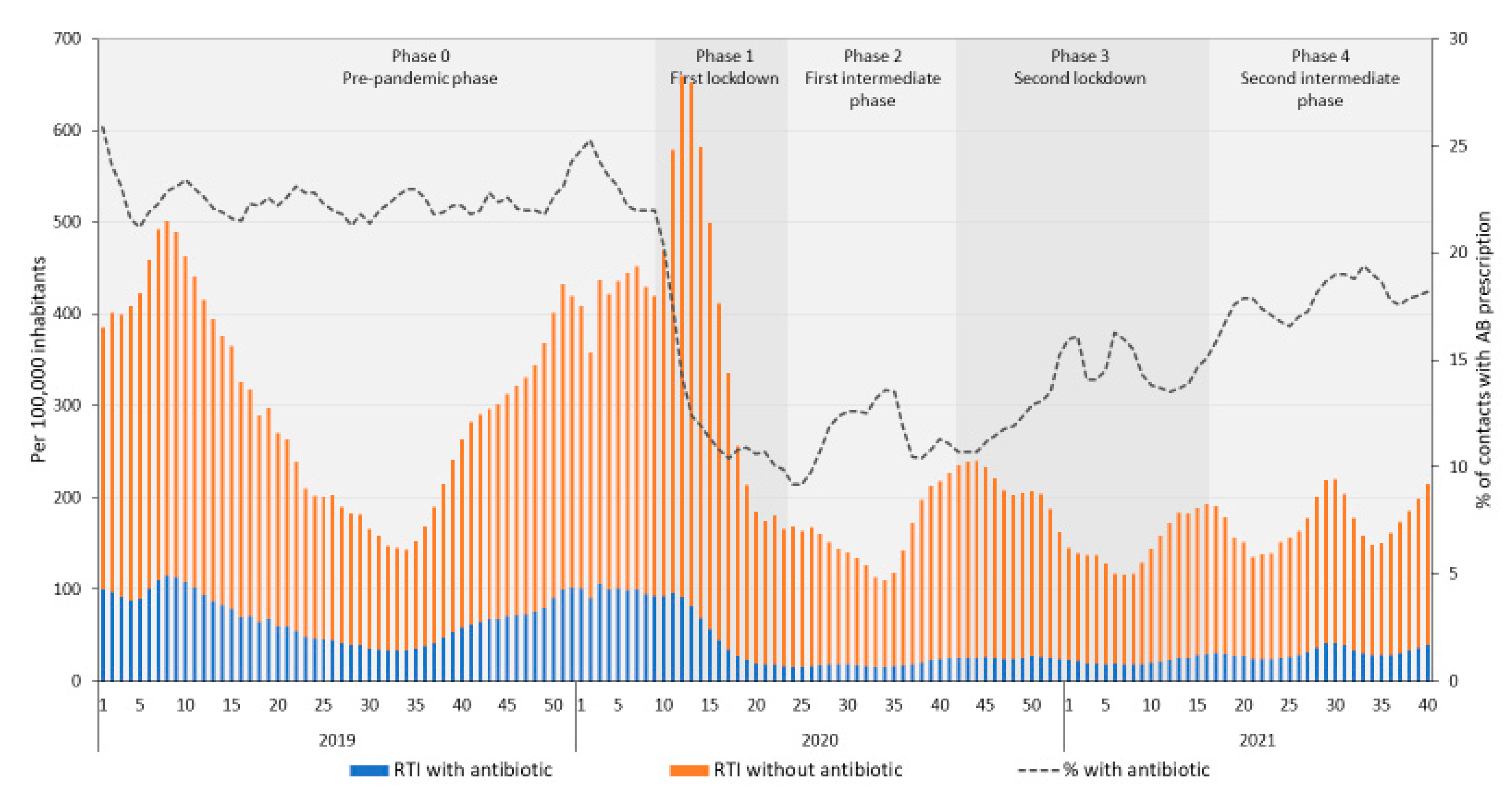
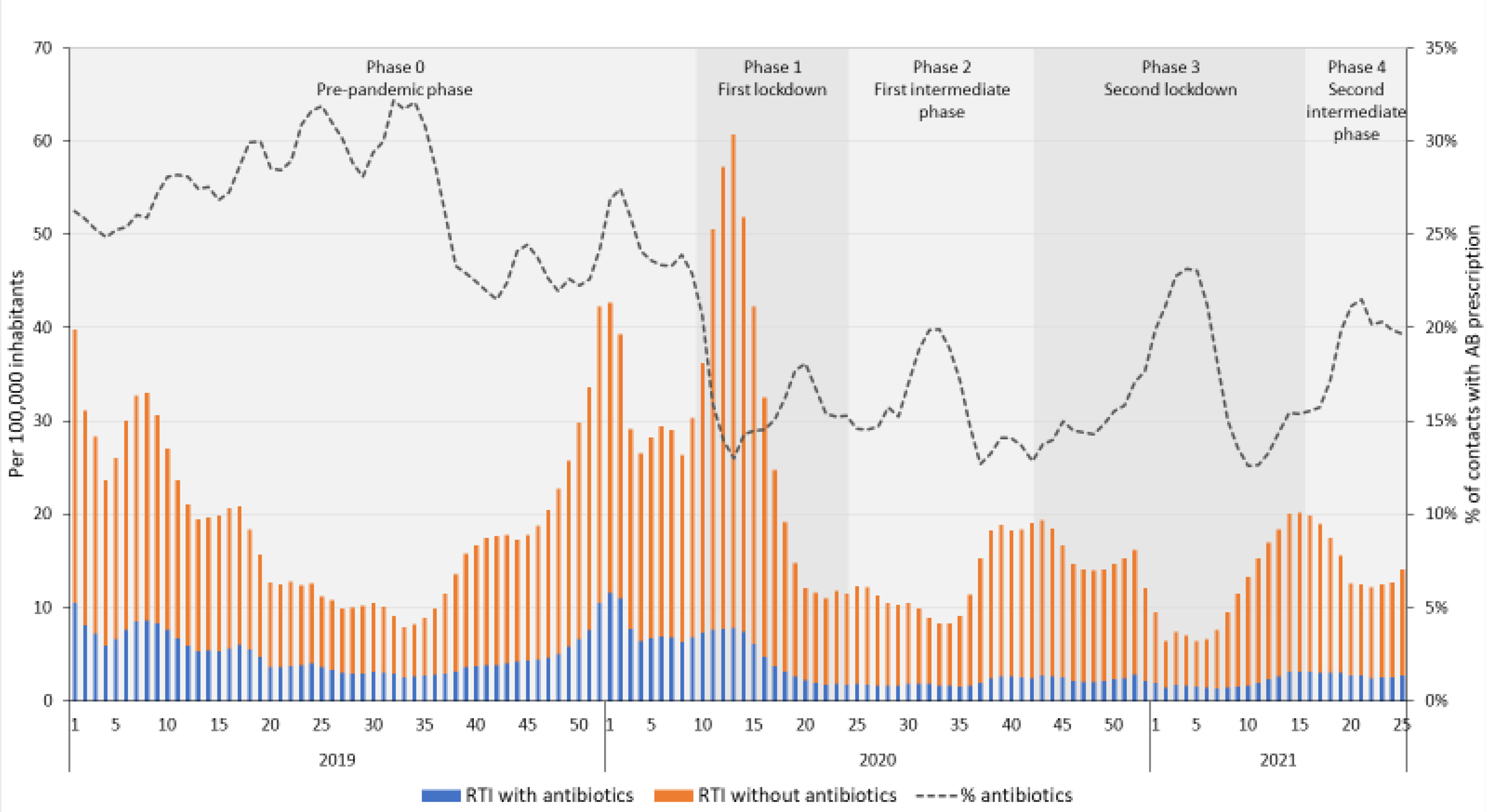
2.2. Trends for Respiratory Tract infections
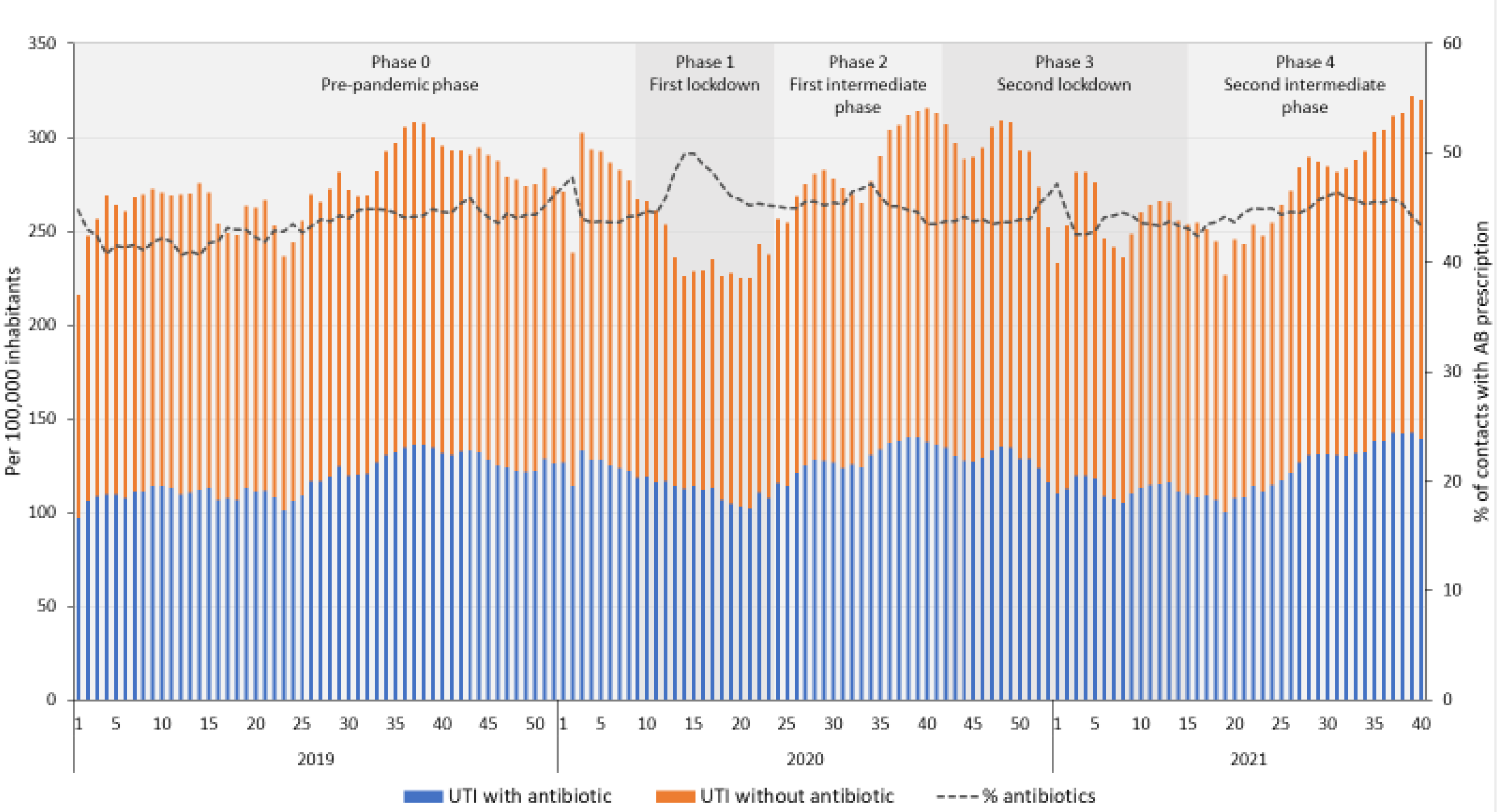
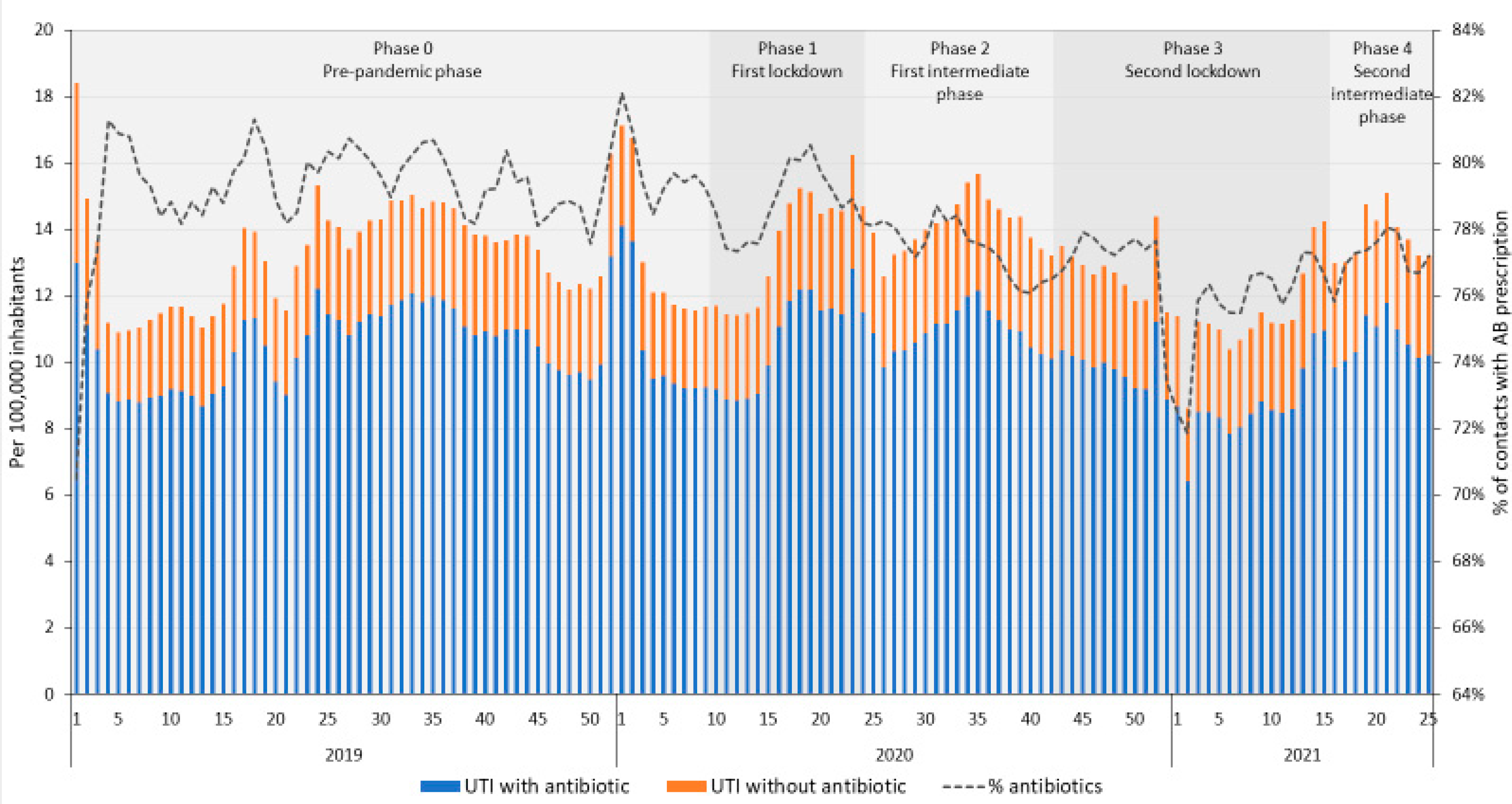
2.3. Trends for Urinary Tract Infections
2.4. Trends for Different Age Categories
3. Discussion
Strengths and Limitations of the Study
4. Materials and Methods
4.1. Design, Setting and Database
4.2. Data Analysis
4.3. Ethics
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gray, R.; Sanders, C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J. Interprof. Care 2020, 34, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135. [Google Scholar] [CrossRef] [PubMed]
- Ramerman, L.R.; Bos, N.; Flinterman, L.; Verheij, R.A. The use of out-of-hours primary care during the first year of the COVID-19 pandemic. submitted.
- Rawson, T.M.; Moore, L.S.; Castro-Sanchez, E.; Charani, E.; Davies, F.; Satta, G.; Ellington, M.J.; Holmes, A.H. COVID-19 and the potential long-term impact on antimicrobial resistance. J. Antimicrob. Chemother. 2020, 75, 1681–1684. [Google Scholar] [CrossRef]
- Collignon, P.; Beggs, J.J. CON: COVID-19 will not result in increased antimicrobial resistance prevalence. JAC-Antimicrob. Resist. 2020, 2, dlaa051. [Google Scholar] [CrossRef] [PubMed]
- Chan, K.H.; Lee, P.W.; Chan, C.Y.; Lam, K.B.H.; Ho, P.L. Monitoring respiratory infections in COVIDD-19 epidemics. BMJ 2020, 369, m1628. [Google Scholar] [CrossRef] [PubMed]
- Hayhoe, B.; Greenfield, G.; Majeed, A. Is it getting easier to obtain antibiotics in the UK? Br. J. Gen. Pract. 2019, 69, 54–55. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. Antibiotic prescribing in general practice during COVID-19. Lancet Infect. Dis. 2021, 21, e144. [Google Scholar] [CrossRef]
- Li, C.; Ong, C.; Morris, A.; Woollons, I.; Ashfaq, A.; Jagatia, R. Evaluating the Appropriateness of Antibiotic Treatment of Tonsillitis during COVID-19 in the North Wale Primary Healthcare Setting. J Prim. Care Community Health 2021, 12, 21501327211003687. [Google Scholar] [CrossRef]
- Colliers, A.; De Man, J.; Adriaenssens, N.; Verhoeven, V.; Anthierens, S.; De Loof, H.; Philips, H.; Coenen, S.; Morreel, S. Antibiotic Prescribing Trends in Belgian Out-of-Hours Primary Care during the COVID-19 Pandemic: Observational Study Using Routinely Collected Health Data. Antibiotics 2021, 10, 1488. [Google Scholar] [CrossRef]
- Han, S.M.; Greenfield, G.; Majeed, A.; Hayhoe, B. Impact of Remote Consultations on Antibiotic Prescribing in Primary Health Care: Systematic Review. J. Med. Internet Res. 2020, 22, e23482. [Google Scholar] [CrossRef]
- Högberg, L.D.; Vlahović-Palčevski, V.; Pereira, C.; Weist, K.; Monnet, D.L.; ESAC-Net Study Group. Decrease in community antibiotic consumption during the COVID-19 pandemic, EU/EEA, 2020. Eurosurveillance 2021, 26, 2101020. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.J.; McLeod, M.; McNulty, C.A.; Lecky, D.M.; Holmes, A.H.; Ahmad, R. Trends in Antibiotic Prescribing in Out-of-Hours Primary Care in England from January 2016 to June 2020 to Understand Behaviours during the First Wave of COVID-19. Antibiotics 2021, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Gillies, M.B.; Burgner, D.P.; Ivancic, L.; Nassar, N.; Miller, J.E.; Sullivan, S.G.; Todd, I.M.; Pearson, S.A.; Schaffer, A.L.; Zoega, H. Changes in antibiotic prescribing following COVID-19 restrictions: Lessons for post-pandemic antibiotic stewardship. Br. J. Clin. Pharmacol. 2021, 88, 1143–1151. [Google Scholar] [CrossRef] [PubMed]
- van de Pol, A.C.; Boeijen, J.A.; Venekamp, R.P.; Platteel, T.; Damoiseaux, R.A.; Kortekaas, M.F.; van der Velden, A.W. Impact of the COVID-19 Pandemic on Antibiotic Prescribing for Common Infections in The Netherlands: A Primary Care-Based Observational Cohort Study. Antibiotics 2021, 10, 196. [Google Scholar] [CrossRef]
- Rezel-Potts, E.; L’Esperance, V.; Gulliford, M.C. Antimicrobial stewardship in the UK during the COVID-19 pandemic: A population-based cohort study and interrupted time-series analysis. Br. J. Gen. Pract. 2021, 71, e331–e338. [Google Scholar] [CrossRef]
- Hussain, A.Z.; Paudyal, V.; Hadi, M.A. Impact of the COVID-19 Pandemic on the Prescribing Patterns of First-Line Antibiotics in English Primary Care: A Longitudinal Analysis of National Prescribing Dataset. Antibiotics 2021, 10, 591. [Google Scholar] [CrossRef]
- Baddock, K. COVID-19-the frontline (a GP perspective). N. Z. Med. J. 2020, 133, 8–10. [Google Scholar]
- Khan, N.; Jones, D.; Grice, A.; Alderson, S.; Bradley, S.; Carder, P.; Drinkwater, J.; Edwards, H.; Essang, B.; Richards, S.; et al. A brave new world: The new normal for general practice after the COVID-19 pandemic. BJGP Open 2020, 4, bjgpopen20X101103. [Google Scholar] [CrossRef]
- Morreel, S.; Philips, H.; Verhoeven, V. Organisation and characteristics of out-of-hours primary care during a COVID-19 outbreak: A real-time observational study. PLoS ONE 2020, 15, e0237629. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Koh, G.C.H.; Car, J. COVID-19: A remote assessment in primary care. BMJ 2020, 368, m1182. [Google Scholar] [CrossRef]
- van Summeren, J.; Meijer, A.; Aspelund, G.; Casalegno, J.S.; Erna, G.; Hoang, U.; Lina, B.; de Lusignan, S.; Teirlinck, A.C.; Thors, V.; et al. Low levels of respiratory syncytial virus activity in Europe during the 2020/21 season: What can we expect in the coming summer and autumn/winter? Eurosurveillance 2021, 26, 2100639. [Google Scholar] [CrossRef] [PubMed]
- Foley, D.A.; Phuong, L.K.; Peplinski, J.; Lim, S.M.; Lee, W.H.; Farhat, A.; Minney-Smith, C.A.; Martin, A.C.; Mace, A.O.; Sikazwe, C.T.; et al. Examining the interseasonal resurgence of respiratory syncytial virus in Western Australia. Arch. Dis. Child. 2021, 107, e7. [Google Scholar] [CrossRef] [PubMed]
- Opek, M.W.; Yeshayahu, Y.; Glatman-Freedman, A.; Kaufman, Z.; Sorek, N.; Brosh-Nissimov, T. Delayed respiratory syncytial virus epidemic in children after relaxation of COVID-19 physical distancing measures, Ashdod, Israel, 2021. Eurosurveillance 2021, 26, 2100706. [Google Scholar]
- Zhu, N.; Aylin, P.; Rawson, T.; Gilchrist, M.; Majeed, A.; Holmes, A. Investigating the impact of COVID-19 on primary care antibiotic prescribing in North West London across two epidemic waves. Clin. Microbiol. Infect. 2021, 27, 762–768. [Google Scholar] [CrossRef] [PubMed]
- Malcolm, W.; Seaton, R.A.; Haddock, G.; Baxter, L.; Thirlwell, S.; Russell, P.; Cooper, L.; Thomson, A.; Sneddon, J. Impact of the COVID-19 pandemic on community antibiotic prescribing in Scotland. JAC Antimicrob. Resist. 2020, 2, dlaa105. [Google Scholar] [CrossRef]
- Christensen, M.B.; Nørøxe, K.B.; Moth, G.; Vedsted, P.; Huibers, L. Drug prescriptions in Danish out-of-hours primary care: A 1-yearpopulation-based study. Scand. J. Prim. Health Care 2016, 34, 453–458. [Google Scholar] [CrossRef][Green Version]
- Heins, M.; Hek, K.; Hooiveld, M.; Hendriksen, J.; Korevaar, J. Impact Coronapandemie op Zorgvraag Bij Huisartsen (Factsheet A). Gevolgen Corona in de Huisartsenpraktijk; Nivel: Utrecht, The Netherlands, 2020. [Google Scholar]
- Group, P.T.C. Azithromycin for community treatment of suspected COVID-19 in people at increased risk of an adverse clinical course in the UK (PRINCIPLE): A randomised, controlled, open-label, adaptive platform trial. Lancet 2021, 397, 1063–1074. [Google Scholar]
- Butler, C.C.; Yu, L.M.; Dorward, J.; Gbinigie, O.; Hayward, G.; Saville, B.R.; Van Hecke, O.; Berry, N.; Detry, M.A.; Saunders, C.; et al. Doxycycline for community treatment of suspected COVID-19 in people at high risk of adverse outcomes in the UK (PRINCIPLE): A randomised, controlled, open-label, adaptive platform trial. Lancet Respir. Med. 2021, 9, 1010–1020. [Google Scholar] [CrossRef]
- Hooiveld, M.H.; Korevaar, J.C. Wekelijkse Surveillance Cijfers. Uit: Nivel Zorgregistraties Eerste Lijn; Nivel: Utrecht, The Netherlands, 2020. [Google Scholar]
- Nielen, M.M.; Weesie, Y.; Davids, R.; Winckers, M.; Korteweg, L.; Leeuw E de Urbanus, T.; Hasselaar, J.; Hek, K. Zorg Door de Huisarts. Nivel Zorgregistraties Eerste Lijn: Jaarcijfers 2020 en Trendcijfers; Nivel: Utrecht, The Netherlands, 2021. [Google Scholar]
- England, P.H. English Surveillance Programma for Antimicrobial Utilisation and Resistance (ESPAUR) Report; PHE Gateway number: GW-1648; Public Health England: London, UK, 2019.
- Ramerman, L.; Verheij, R.A. Cijfers Zorgverlening Huisartsenposten-Nivel Zorgregistraties Eerste Lijn. 2021. Available online: https://www.nivel.nl/nl/nivel-zorgregistraties-eerste-lijn/cijfers-zorgverlening-huisartsenposten (accessed on 19 January 2022).
- Dutch Civil Law (BW). Article 7:458 Data for Scientific Research. Available online: https://www.dutchcivillaw.com (accessed on 23 February 2022).
- Medical Research Involving Human Subject Act (WMO). Available online: https://english.ccmo.nl/investigators/legal-framework-for-medical-scientific-research (accessed on 23 February 2022).
- General Data Protection Regulation (GDPR). Regulation (EU) 2016/679 of the European Parliament and of the Council—of 27 April 2016—On the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/EC (General Data Protection Regulation) (europa.eu). Available online: https://gdpr-info.eu/ (accessed on 23 February 2022).
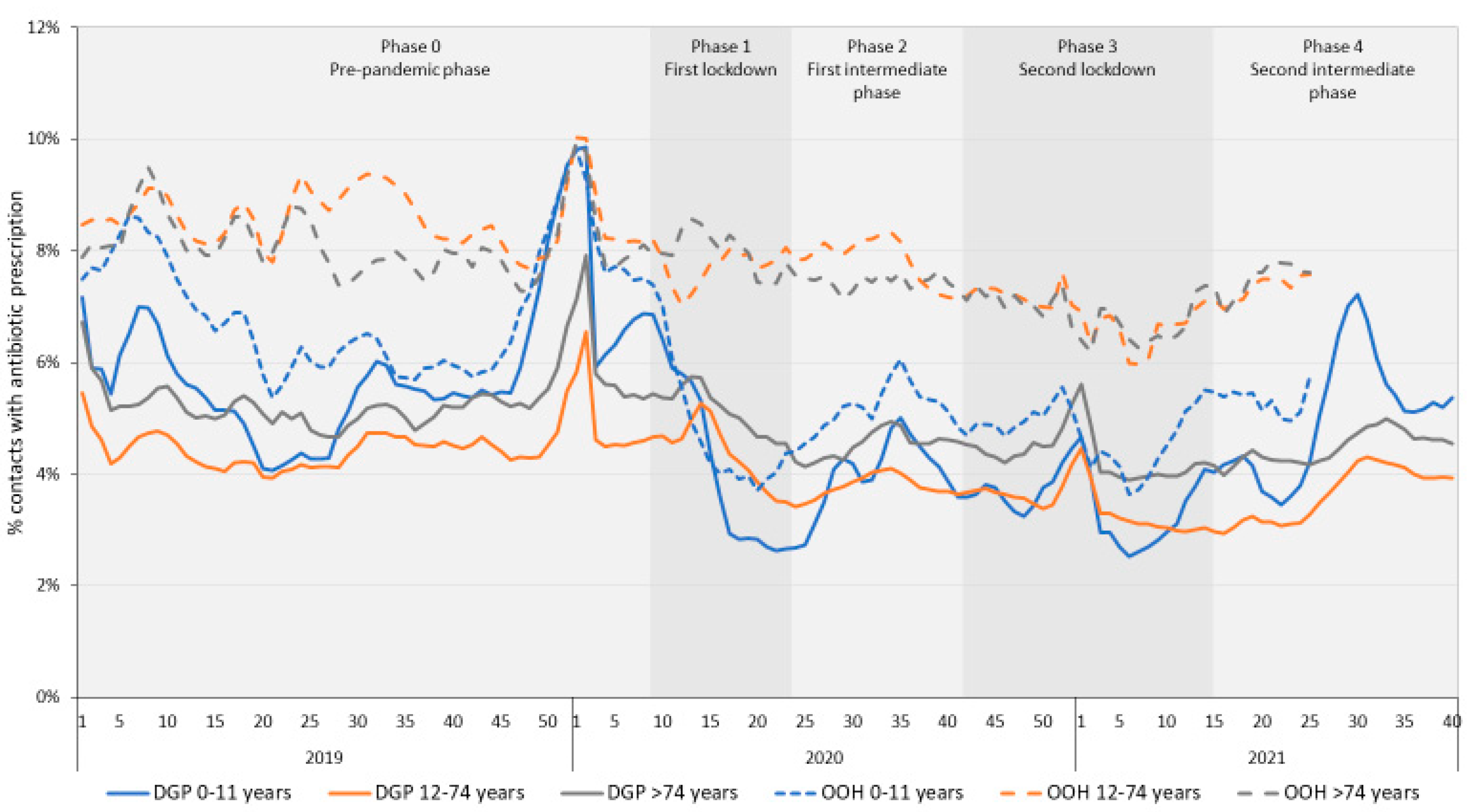
| DGP | OOH-Services | |||||
|---|---|---|---|---|---|---|
| Mean | SD | p-Value for Difference with the Previous Phase * | Mean | SD | p-Value for Difference with the Previous Phase * | |
| Overall incidence of antibiotic prescriptions | ||||||
| Phase 0 (pre-pandemic) | 595.160 | 39.066 | 36.162 | 7.539 | ||
| Phase 1 (first lockdown) | 492.190 | 89.872 | <0.001 | 34.210 | 3.356 | 1.000 |
| Phase 2 (first intermediate phase) | 491.812 | 18.996 | 1.000 | 32.403 | 3.693 | 1.000 |
| Phase 3 (second lockdown) | 459.830 | 26.314 | 0.195 | 26.240 | 5.947 | 0.008 |
| Phase 4 (second intermediate phase) | 510.815 | 39.772 | <0.001 | 36.610 | 3.183 | 0.012 |
| Incidence of antibiotic prescriptions for RTIs | ||||||
| Phase 0 (pre-pandemic) | 72.810 | 25.315 | 5.233 | 2.499 | ||
| Phase 1 (first lockdown) | 49.981 | 32.308 | 0.001 | 4.196 | 2.669 | 0.712 |
| Phase 2 (first intermediate phase) | 18.135 | 3.214 | <0.001 | 1.985 | 0.475 | 0.005 |
| Phase 3 (second lockdown) | 23.354 | 3.222 | 1.000 | 2.127 | 0.692 | 1.000 |
| Phase 4 (second intermediate phase) | 32.100 | 6.657 | 1.000 | 2.747 | 0.370 | 1.000 |
| Incidence of antibiotic prescriptions for UTIs | ||||||
| Phase 0 (pre-pandemic) | 119.272 | 10.052 | 10.376 | 2.144 | ||
| Phase 1 (first lockdown) | 111.606 | 5.414 | 0.069 | 10.677 | 1.778 | 1.000 |
| Phase 2 (first intermediate phase) | 129.900 | 7.416 | <0.001 | 10.943 | 0.745 | 1.000 |
| Phase 3 (second lockdown) | 119.500 | 9.627 | 0.009 | 9.172 | 2.148 | 0.042 |
| Phase 4 (second intermediate phase) | 125.596 | 13.008 | 0.258 | 10.871 | 1.134 | 1.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hek, K.; Ramerman, L.; Weesie, Y.M.; Lambooij, A.C.; Lambert, M.; Heins, M.J.; Hendriksen, J.M.T.; Verheij, R.A.; Cals, J.W.L.; van Dijk, L. Antibiotic Prescribing in Dutch Daytime and Out-of-Hours General Practice during the COVID-19 Pandemic: A Retrospective Database Study. Antibiotics 2022, 11, 309. https://doi.org/10.3390/antibiotics11030309
Hek K, Ramerman L, Weesie YM, Lambooij AC, Lambert M, Heins MJ, Hendriksen JMT, Verheij RA, Cals JWL, van Dijk L. Antibiotic Prescribing in Dutch Daytime and Out-of-Hours General Practice during the COVID-19 Pandemic: A Retrospective Database Study. Antibiotics. 2022; 11(3):309. https://doi.org/10.3390/antibiotics11030309
Chicago/Turabian StyleHek, Karin, Lotte Ramerman, Yvette M. Weesie, Anke C. Lambooij, Maarten Lambert, Marianne J. Heins, Janneke M. T. Hendriksen, Robert A. Verheij, Jochen W. L. Cals, and Liset van Dijk. 2022. "Antibiotic Prescribing in Dutch Daytime and Out-of-Hours General Practice during the COVID-19 Pandemic: A Retrospective Database Study" Antibiotics 11, no. 3: 309. https://doi.org/10.3390/antibiotics11030309
APA StyleHek, K., Ramerman, L., Weesie, Y. M., Lambooij, A. C., Lambert, M., Heins, M. J., Hendriksen, J. M. T., Verheij, R. A., Cals, J. W. L., & van Dijk, L. (2022). Antibiotic Prescribing in Dutch Daytime and Out-of-Hours General Practice during the COVID-19 Pandemic: A Retrospective Database Study. Antibiotics, 11(3), 309. https://doi.org/10.3390/antibiotics11030309







