The Impact of Antibiotic Usage Guidelines, Developed and Disseminated through Internet, on the Knowledge, Attitude and Prescribing Habits of Orthokeratology Contact Lens Practitioners in China
Abstract
:1. Introduction
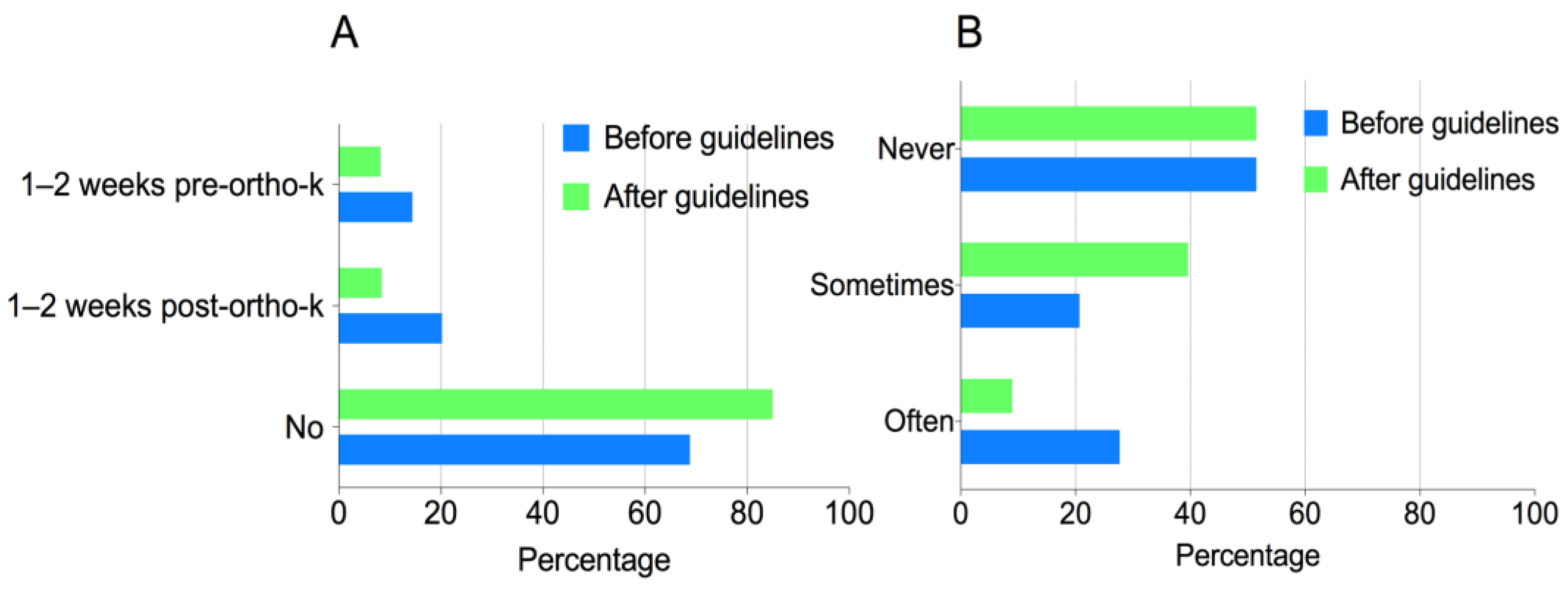
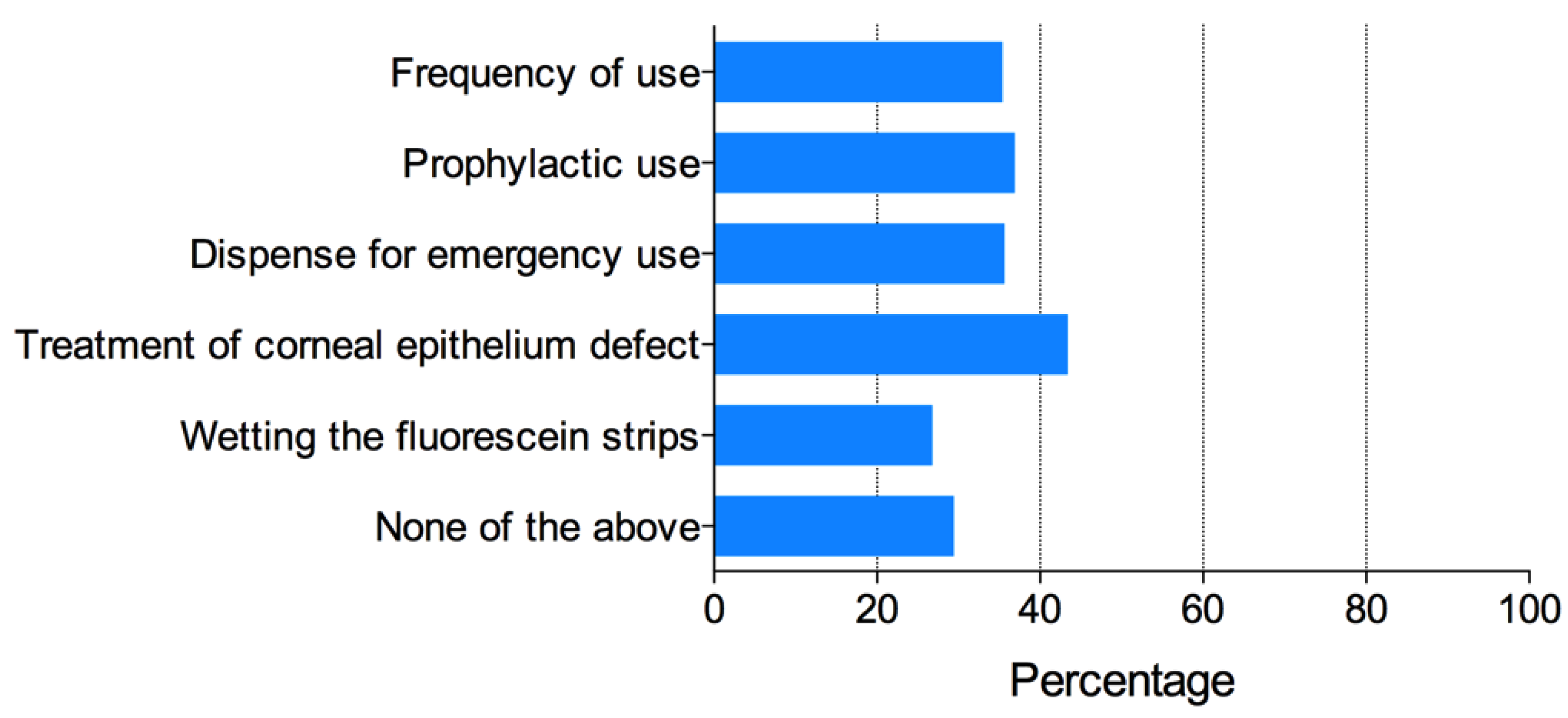
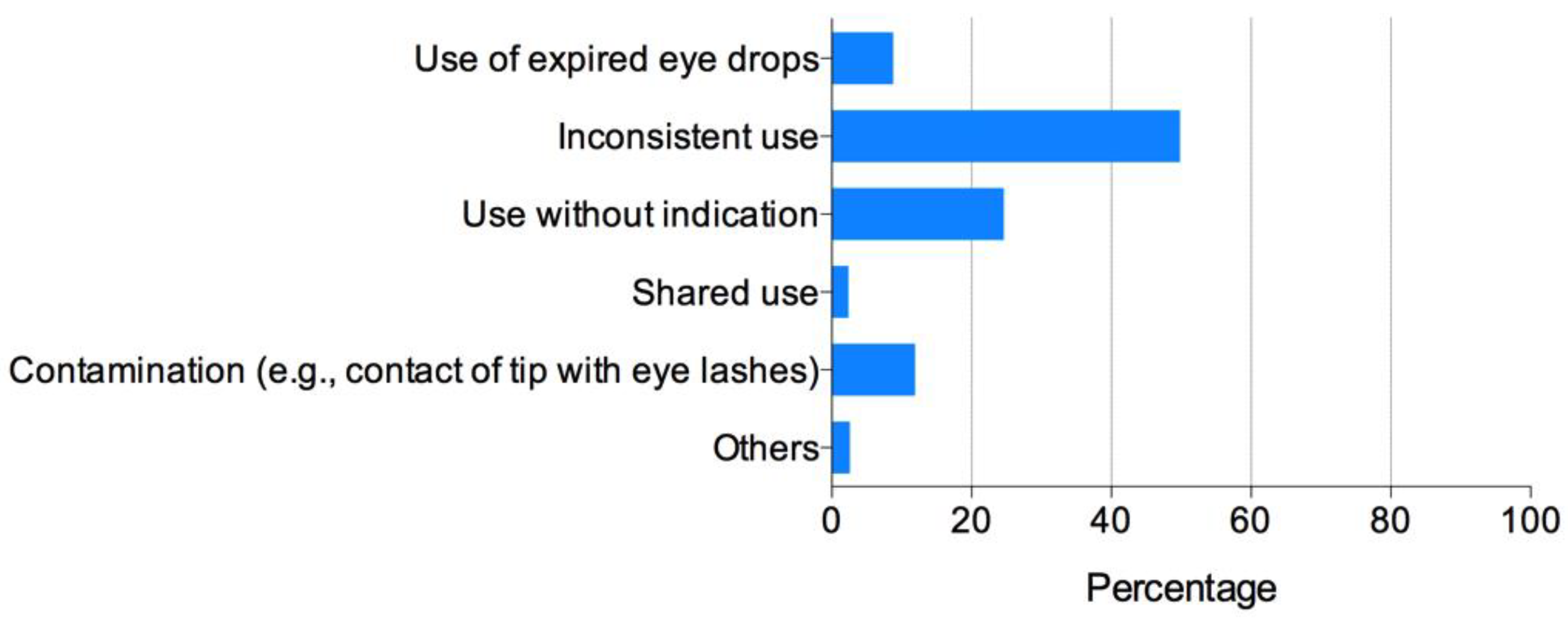
2. Results
3. Discussion
4. Materials and Methods
4.1. Preparation of the Questionnaire
- Do you prescribe prophylactic antibiotic eye drops before or after fitting ortho-k?
- Do you dispense antibiotic eye drops to patients for emergency use (at patients’ discretion)?
- Do you use antibiotic eye drops to wet fluorescein strips during ortho-k lens fitting?
4.2. Definition of Proper Antibiotic Use
- Do not use prophylactic antibiotic eye drops before or after fitting ortho-k lenses;
- Do not dispense antibiotic eye drops to patients for emergency use (when essential, dispense to patients along with written instructions);
- Do not use antibiotic eye drops to wet fluorescein strips during ortho-k lens fitting.
4.3. Distribution of Questionnaires
4.4. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Statement
References
- Nichols, J.J.; Marsich, M.M.; Nguyen, M.; Barr, J.T.; Bullimore, M.A. Overnight orthokeratology. Optom. Vis. Sci. 2000, 77, 252–259. [Google Scholar] [CrossRef]
- Alharbi, A.; Swarbrick, H. The effects of overnight orthokeratology lens wear on corneal thickness. Investig. Ophthalmol. Vis. Sci. 2003, 44, 2518–2523. [Google Scholar] [CrossRef]
- Maseedupally, V.; Gifford, P.; Lum, E.; Swarbrick, H. Central and paracentral corneal curvature changes during orthokeratology. Optom. Vis. Sci. 2013, 90, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- Cho, P.; Cheung, S.W. Retardation of myopia in orthokeratology (ROMIO) study: A 2-year randomized clinical trial. Investig. Ophthalmol. Vis. Sci. 2012, 53, 7077–7085. [Google Scholar] [CrossRef]
- Cho, P.; Cheung, S.W.; Edwards, M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: A pilot study on refractive changes and myopic control. Curr. Eye Res. 2005, 30, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, T.; Kakita, T.; Okamoto, F.; Takahashi, H.; Oshika, T. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: A 5-year follow-up study. Investig. Ophthalmol. Vis. Sci. 2012, 53, 3913–3919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walline, J.J.; Jones, L.A.; Sinnott, L.T. Corneal reshaping and myopia progression. Br. J. Ophthalmol. 2009, 93, 1181–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xie, P.; Guo, X. Chinese experiences on orthokeratology. Eye Contact Lens 2016, 42, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Hoddenbach, J.G.; Boekhoorn, S.S.; Wubbels, R.; Vreugdenhil, W.; Van Rooij, J.; Geerards, A.J. Clinical presentation and morbidity of contact lens-associated microbial keratitis: A retrospective study. Graefes Arch. Clin. Exp. Ophthalmol. 2014, 252, 299–306. [Google Scholar] [CrossRef] [PubMed]
- Bullimore, M.A.; Sinnott, L.T.; Jones-Jordan, L.A. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom. Vis. Sci. 2013, 90, 937–944. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Jiang, J.; Xu, J.; Yang, X.; Yang, Y.; Wang, K.; Song, H.; Yang, B.; Cho, P. Antibiotic eye drops prescription patterns by orthokeratology practitioners in china and the development of antibiotic usage guidelines. Contact Lens Anterior Eye 2021, 44, 101354. [Google Scholar] [CrossRef] [PubMed]
- Watt, K.G.; Swarbrick, H.A. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens 2007, 33, 373–377; discussion 382. [Google Scholar] [CrossRef] [PubMed]
- Cho, P.; Boost, M.; Cheng, R. Non-compliance and microbial contamination in orthokeratology. Optom. Vis. Sci. 2009, 86, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Cho, P.; Cheung, S.W.; Mountford, J.; White, P. Good clinical practice in orthokeratology. Contact Lens and Anterior Eye 2008, 31, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.Y.; Lam, C.S.; Tang, W.C.; Leung, M.; To, C.H. Defocus incorporated multiple segments spectacle lenses changed the relative peripheral refraction-a 2-year randomized clinical trial (DIMS). Investig. Ophthalmol. Vis. Sci. 2020, 61, 53. [Google Scholar] [CrossRef] [PubMed]
- Bao, J.; Yang, A.; Huang, Y.; Li, X.; Pan, Y.; Ding, C.; Lim, E.W.; Zheng, J.; Spiegel, D.P.; Drobe, B.; et al. One-year myopia control efficacy of spectacle lenses with aspherical lenslets. Br. J. Ophthalmol. 2021; online ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Chua, W.H.; Wen, L.; Fong, A.; Goon, Y.Y.; Tan, D. Atropine for the treatment of childhood myopia: Changes after stopping atropine 0.01%, 0.1% and 0.5%. Am. J. Ophthalmol. 2014, 157, 451–457.e1. [Google Scholar] [CrossRef] [PubMed]
- Yam, J.C.; Li, F.F.; Zhang, X.; Tang, S.M.; Yip, B.H.K.; Kam, K.W.; Ko, S.T.; Young, A.L.; Tham, C.C.; Chen, L.J.; et al. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: Phase 2 report. Ophthalmology 2019, 127, 910–919. [Google Scholar] [CrossRef] [PubMed]
| Frequency (%) | |
|---|---|
| 1. Occupation Ophthalmologist
| 114 (20.9) 7 (1.3) 8 (1.5) 99 (18.1) |
| Optometrist (degree or diploma) | 359 (65.5) |
| Other (nurse, optician, etc.) | 75 (13.6) |
| 2. Clinical setting | |
| General hospital | 142 (25.9) |
| Ophthalmic specialty hospital | 120 (21.9) |
| Private optometry clinic | 144 (26.3) |
| Ortho-k distributor fitting center | 142 (25.9) |
| 3. Level of practice | |
| Provincial level | 111 (20.3) |
| Municipal level | 307 (56.0) |
| County level | 55 (10.0) |
| Others | 75 (13.7) |
| 4. Age (years) | |
| <25 | 77 (14.1) |
| 25–30 | 174 (31.8) |
| 31–35 | 124 (22.6) |
| 36–40 | 76 (13.9) |
| >40 | 97 (17.7) |
| 5. Sex | |
| Male | 143 (26.1) |
| Female | 405 (73.9) |
| Do You Agree with the Statement | Strongly Agree | Agree | Not Sure | Disagree | Strongly Disagree |
|---|---|---|---|---|---|
| 1. “antibiotic eye drops may be used prophylactically before or after commencement of treatment to prevent corneal infection”? | 7 (1.3) | 42 (7.7) | 57 (10.4) | 321 (58.6) | 121 (22.0) |
| 2. “when bacterial keratitis is suspected, patients do not have to stop lens wear, but re-enforcement of lens care routines and use of broad-spectrum antibiotics is necessary”? | 4 (0.7) | 16 (2.9) | 24 (4.4) | 168 (30.7) | 336 (61.3) |
| 3. “avoid dispensing antibiotic eye drops to patients for emergency use (if unavoidable, dispense together with clear written instructions)”? | 98 (17.9) | 209 (38.1) | 41 (7.5) | 183 (33.4) | 17 (3.1) |
| 4. “it is very important to properly use antibiotic eye drops”? | 361 (65.9) | 128 (23.4) | 26 (4.7) | 28 (5.1) | 5 (0.9) |
| 5. “the article and the guidelines are useful”? | 342 (62.4) | 189 (34.5) | 12 (2.2) | 3 (0.5) | 2 (0.4) |
| 6. “I will consider more carefully when using antibiotics after reading the guidelines”? | 375 (68.4) | 168 (30.7) | 4 (0.7) | 1 (0.2) | 0 (0) |
| OR (95% CI) | p | ||
|---|---|---|---|
| Occupation | Ophthalmologist | Referent | |
| Optometrist (degree or diploma) | 0.68 (0.44–1.05) | 0.08 | |
| Other (nurse, optician, etc.) | 0.23 (0.11–0.48) | <0.001 | |
| Clinical setting | Private optometry clinic | Referent | |
| Ophthalmic specialty hospital | 1.08 (0.66–1.78) | 0.75 | |
| General hospital | 1.02 (0.64–1.65) | 0.92 | |
| Distributor fitting center | 0.27 (0.15–0.48) | <0.001 | |
| Practice level | Provincial | Referent | |
| Municipal | 0.77 (0.49–1.22) | 0.27 | |
| County | 1.01 (0.52–1.99) | 0.97 | |
| Others | 1.12 (0.61–2.05) | 0.72 | |
| Age | <25 | Referent | |
| 25–30 | 2.94 (1.5–5.74) | <0.001 | |
| 31–35 | 2.61 (1.3–5.27) | 0.01 | |
| 36–40 | 2.87 (1.35–6.12) | 0.01 | |
| >40 | 2.54 (1.22–5.26) | 0.01 | |
| Sex | Male | Referent | |
| Female | 1.46 (0.96–2.22) | 0.08 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, Z.; Wang, J.; Jiang, J.; Yang, B.; Cho, P. The Impact of Antibiotic Usage Guidelines, Developed and Disseminated through Internet, on the Knowledge, Attitude and Prescribing Habits of Orthokeratology Contact Lens Practitioners in China. Antibiotics 2022, 11, 179. https://doi.org/10.3390/antibiotics11020179
Chen Z, Wang J, Jiang J, Yang B, Cho P. The Impact of Antibiotic Usage Guidelines, Developed and Disseminated through Internet, on the Knowledge, Attitude and Prescribing Habits of Orthokeratology Contact Lens Practitioners in China. Antibiotics. 2022; 11(2):179. https://doi.org/10.3390/antibiotics11020179
Chicago/Turabian StyleChen, Zhi, Jifang Wang, Jun Jiang, Bi Yang, and Pauline Cho. 2022. "The Impact of Antibiotic Usage Guidelines, Developed and Disseminated through Internet, on the Knowledge, Attitude and Prescribing Habits of Orthokeratology Contact Lens Practitioners in China" Antibiotics 11, no. 2: 179. https://doi.org/10.3390/antibiotics11020179
APA StyleChen, Z., Wang, J., Jiang, J., Yang, B., & Cho, P. (2022). The Impact of Antibiotic Usage Guidelines, Developed and Disseminated through Internet, on the Knowledge, Attitude and Prescribing Habits of Orthokeratology Contact Lens Practitioners in China. Antibiotics, 11(2), 179. https://doi.org/10.3390/antibiotics11020179






