Antimicrobial Resistance and Community Pharmacists’ Perspective in Thailand: A Mixed Methods Survey Using Appreciative Inquiry Theory
Abstract
:1. Introduction
2. Results
2.1. Socio-Demographic Characteristics of Participants
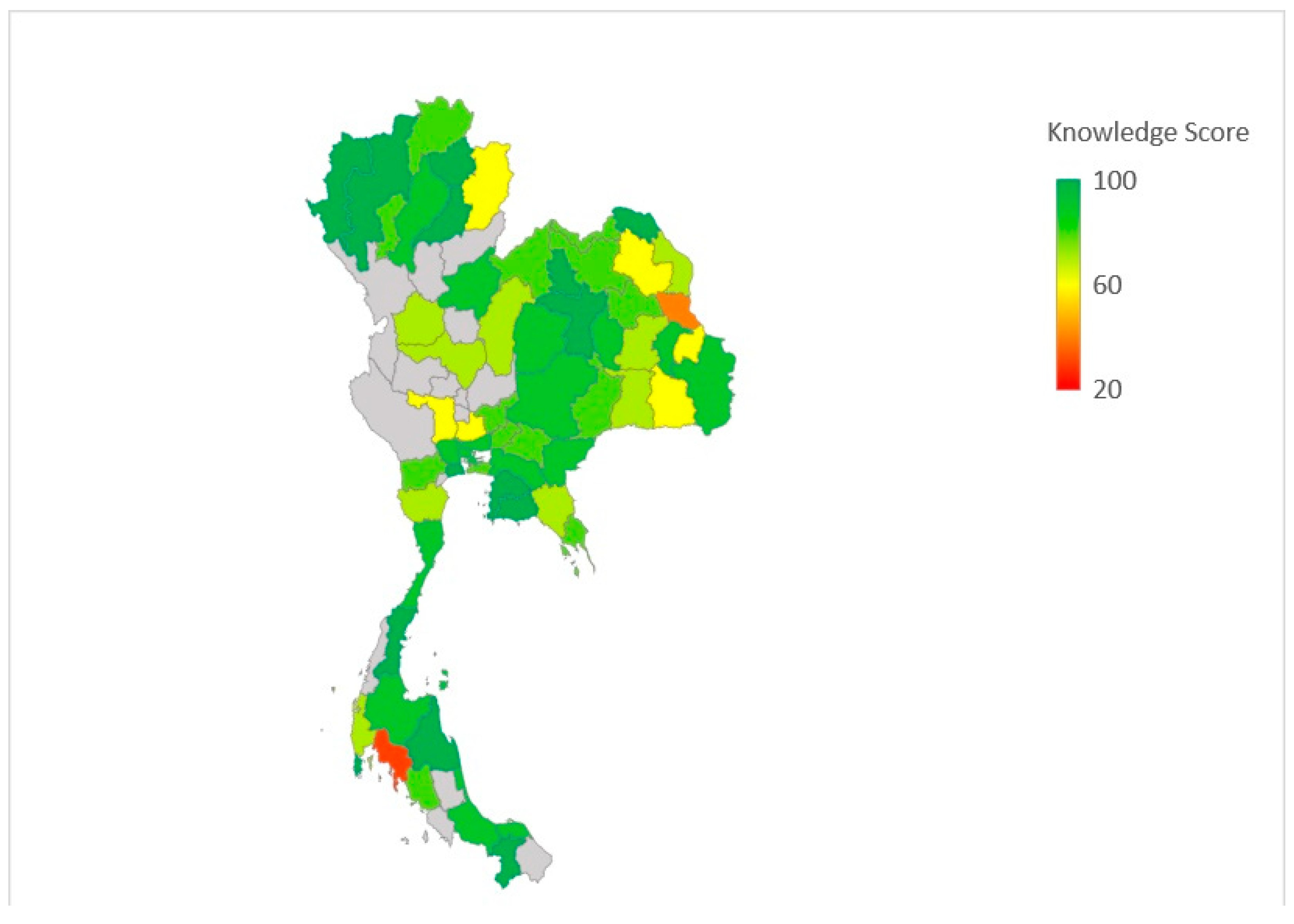
2.2. Community Pharmacists’ Knowledge regarding Antibiotic Resistance
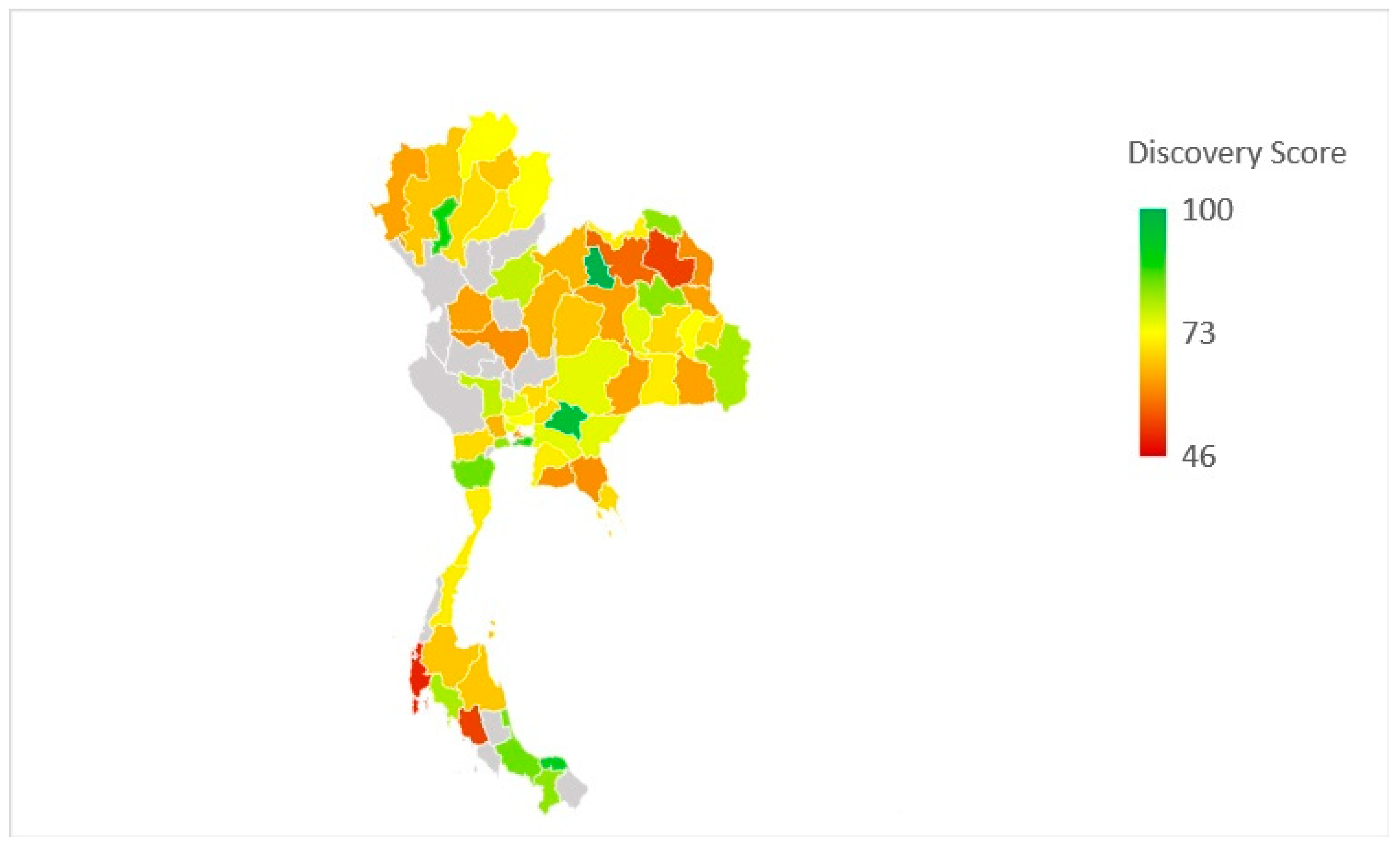
2.3. Community Pharmacists’ Attitude
2.4. Factors Associated with Attitude
2.5. Qualitative Results
2.5.1. Regulation
“[There are] guidelines for antibiotic use in the community pharmacy but a lack of regulation. So many community pharmacists are still improperly dispensing antibiotics.”
“I would like to see random official visits by provincial public health officers to evaluate the antibiotics prescription and dispensing practices of community pharmacists. These audits might help with enforcement [of the regulations].”
“The submission of assessment reports, detailing the amount and names of antibiotics dispensed in the community pharmacies, should be introduced. It might help to control antibiotic dispensing in the community settings.”
2.5.2. Local Guidelines
“I think the governmental organisation should create antibiotic dispensing/prescription guidelines for the treatment of infections in community pharmacies and then disseminate them via newsletters.”
“Standard practices and guidelines for rational antibiotic use in community pharmacies should be conveyed to the pharmacists throughout the country.”
2.5.3. Re-Classification
“Re-classification is a process of segmentation in group of antibiotics. Some can be dispensed by pharmacists in community pharmacies and some should be reserved for prescribing and dispensing only in the hospital setting for some severe infections”
“[There is a need for] re-classification antibiotics to a controlled drug group. This group in Thailand requires a prescription. I think it might promote rational antibiotic dispensing and use in the community settings.”
“Antibiotics re-classification might negatively affect patients’ experiences and outcomes including increased rates of death and disability, if they have delayed treatment of infections due to unavailable antibiotics in community pharmacists.”
“The first action should be to remove advertising of antibiotics from the internet, radio, or other online social media such as Lazada, Shopee, Facebook and others.”
2.5.4. Good Pharmacy Practice (GPP)
“The problem is some pharmacies that lack a pharmacist on duty during working hours. Non-pharmacist can illegally sell antibiotics. It allows for the increase irrational antibiotic use in the community.”
“The provincial public health officers or government sectors should audit individual pharmacies or chain pharmacies where there is no pharmacist on duty. I notice that, some chain pharmacies where operate 24 h-service, without a pharmacist during the working hours.”
“At present, there are a lot of pharmacies that lack pharmacist on duty. At this point, the sale of antibiotics by non-pharmacist may increase the problem of antibiotic resistance.”
2.5.5. Business Pressure
“I think an implementation step is a minor perform because the majority of pharmacies’ objectives are revenue and credibility. If pharmacists focus on professional ethics and have concerns about antibiotic resistance consequences, they will promote rational antibiotic practices.”
“Antibiotic accessibility should be gradually limited in the healthcare settings including community pharmacies. Then the loss of selling antibiotics revenue may be substitute by income of other treatment choices. I suggested the promotion of the use of herbal medicine or traditional medicine for preserving income.”
“Promote the use of alternative products, health promotion for preventing disease.”
“I think an intervention should be establishing a reward system the participating pharmacy where joining the antibiotic smart use programme. An incentive might be a token as operating costs of rational antibiotic practices. Because promoting the rational use of antibiotics can lead to less of income by decreasing antibiotic sales. Thus, some pharmacies do not follow RDU because there is no benefit.”
“ASU is a voluntary project as well as a lack of the incentive to promote the RDU programme. There may not be a long-term intervention.”
“I want the system for rewarding or giving incentives to the doctor who issued a prescription with dispensing by the pharmacist at the pharmacy. And the pharmacy can operate as a government agency that dispenses ABT without fee by using ABT supported by hospitals.”
2.5.6. Public Education and Awareness
“…[There is a need to] build on the negative effects of irrational antibiotic use, and then provide guidelines to reduce the irrational antibiotic use of antibiotics across the country (for example, banned plastic bags campaign.”
“I think basic knowledge of antibiotic use should integrate to the primary level of education so that the general public can easily understand and have access to broad knowledge. It will help to encourage pharmacists to counsel patients to understand more easily.”
“I think there is a need to encourage people to gain more knowledge and understanding of the use of [appropriate] antibiotics through various media such as TV commercials, online media.”
“Most irrational antibiotic use is rooted in patient’s belief that antibiotics at community pharmacies and easy to obtain.”
“…overclaimed radio advertising about antibiotic benefits have been found to lead/cultivate audiences to misuse antibiotics.”
“I think that we need brochures such as antibiotic knowledge brochures for giving customers. I suggested that the brochures should easy-to-understand.”
2.5.7. Antibiotic Stewardship Training
“They may send knowledge sheets/brochures to the pharmacies or organise additional training for the pharmacies via online platforms. Because it is difficult in some areas to attend face to face training. I think we will achieve the same practice in the prescribing of antibiotics.”
“The provision of free accredited training throughout the country is needed.”
“Rational antibiotic use is promoted but it still has a lack of continuity, up to date information and lack of media support to pharmacies.”
3. Discussion
4. Materials and Methods
4.1. Study Setting and Participants
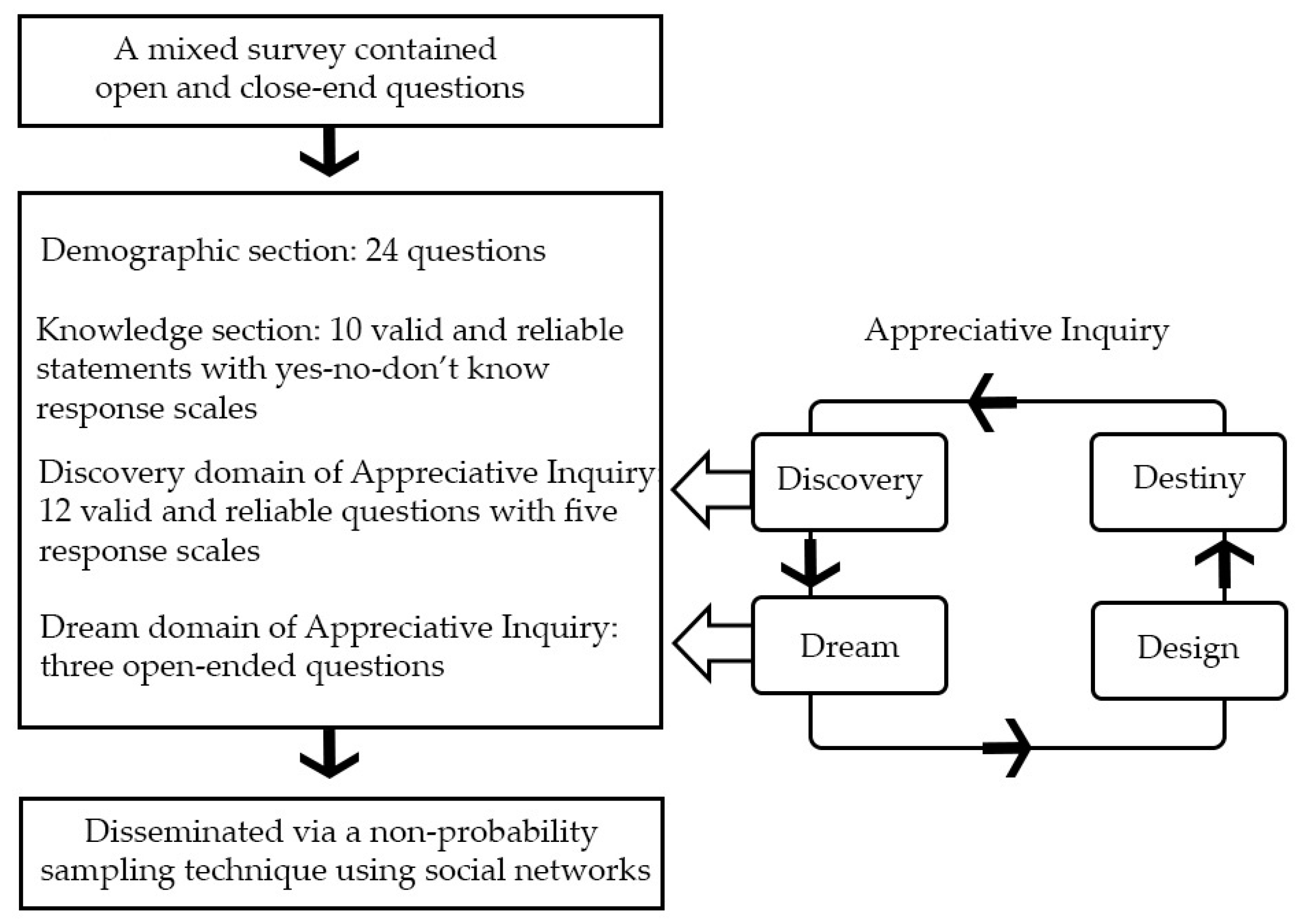
4.2. Theoretical Framework and Survey Design
4.3. Study Design and Sampling Technique
4.4. Data Analysis
4.5. Ethical Considerations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Aslam, B.; Wang, W.; Arshad, M.I.; Khurshid, M.; Muzammil, S.; Rasool, M.H.; Nisar, M.A.; Alvi, R.F.; Aslam, M.A.; Qamar, M.U.; et al. Antibiotic resistance: A rundown of a global crisis. Infect. Drug Resist. 2018, 11, 1645–1658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Littmann, J.; Zorzet, A.; Cars, O. Antimicrobial Resistance—A Threat to the World’s Sustainable Development—Dag Hammarskjöld Foundation. Ups. J. Med. Sci. 2016, 121, 159–164. [Google Scholar]
- ReAct–Action on Antibiotic. When the Drugs Don’t Work Antibiotic Resistance as a Global Development Problem; Dag Hammarskjöld Foundation: Uppsala, Sweden, 2019. [Google Scholar]
- Gajdács, M.; Urbán, E.; Stájer, A.; Baráth, Z. Antimicrobial Resistance in the Context of the Sustainable Development Goals: A Brief Review. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 71–82. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States. 2019. Available online: https://stacks.cdc.gov/view/cdc/82532 (accessed on 25 November 2020).
- World Health Organization. Global Action Plan on Antimicrobial Resistance. Available online: https://www.who.int/publications/i/item/9789241509763 (accessed on 1 December 2021).
- Anderson, M.; Cecchini, M.; Mossialos, E. Challenges to Tackling Antimicrobial Resistance; Figueras, J., McKee, M., Mossialos, E., Busse, R., Eds.; Cambridge University Press: Cambridge, UK, 2019. [Google Scholar]
- Årdal, C.; Outterson, K.; Hoff, S.J.; Ghafur, A.; Sharland, M.; Ranganathan, N.; Smith, R.; Zorzet, A.; Cohn, J.; Daulaire, N.; et al. Antimicrobials: Access and Sustainable Eff Ectiveness 5 International Cooperation to Improve Access to and Sustain Eff Ectiveness of Antimicrobials. Lancet 2016, 387, 296–307. [Google Scholar] [CrossRef] [Green Version]
- Chua, A.Q.; Verma, M.; Hsu, L.Y.; Legido-Quigley, H. An Analysis of National Action Plans on Antimicrobial Resistance in Southeast Asia Using a Governance Framework Approach. Lancet Reg. Health West. Pac. 2021, 7, 84. [Google Scholar] [CrossRef]
- Hoffman, S.J.; Caleo, G.M.; Daulaire, N.; Elbe, S.; Matsoso, P.; Mossialos, E.; Rizvi, Z.; Røttingen, J.-A. Strategies for Achieving Global Collective Action on Antimicrobial Resistance. Bull. World Health Organ. 2015, 93, 867–876. [Google Scholar] [CrossRef]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. Available online: http://amr-review.org (accessed on 29 April 2020).
- Aslam, A.; Gajdács, M.; Suraya Zin, C.; Syafinaz Ab Rahman, N.; Imran Ahmed, S.; Zeeshan Zafar, M.; Jamshed, S. Antibiotics Evidence of the Practice of Self-Medication with Antibiotics among the Lay Public in Low-and Middle-Income Countries: A Scoping Review. Antibiotics 2020, 9, 597. [Google Scholar] [CrossRef]
- Sommanustweechai, A.; Tangcharoensathien, V.; Malathum, K.; Sumpradit, N.; Kiatying-Angsulee, N.; Janejai, N.; Jaroenpoj, S. Implementing National Strategies on Antimicrobial Resistance in Thailand: Potential Challenges and Solutions. Public Health 2018, 157, 142–146. [Google Scholar] [CrossRef]
- Collignon, P.; Beggs, J.J.; Walsh, T.R.; Gandra, S.; Laxminarayan, R. Anthropological and Socioeconomic Factors Contributing to Global Antimicrobial Resistance: A Univariate and Multivariable Analysis. Lancet 2018, 2, e398–e405. [Google Scholar] [CrossRef]
- Do, N.T.T.; Vu, H.T.L.; Nguyen, C.T.K.; Punpuing, S.; Khan, W.A.; Gyapong, M.; Asante, K.P.; Munguambe, K.; Gómez-Olivé, F.X.; John-Langba, J.; et al. Community-Based Antibiotic Access and Use in Six Low-Income and Middle-Income Countries: A Mixed-Method Approach. Artic. Lancet Glob. Health 2021, 9, e610–e619. [Google Scholar] [CrossRef]
- Klein, E.Y.; Van Boeckel, T.P.; Martinez, E.M.; Pant, S.; Gandra, S.; Levin, S.A.; Goossens, H.; Laxminarayan, R. Global Increase and Geographic Convergence in Antibiotic Consumption between 2000 and 2015. Proc. Natl. Acad. Sci. USA 2018, 115, E3463–E3470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hermansyah, A.; Sainsbury, E.; Krass, I. Community Pharmacy and Emerging Public Health Initiatives in Developing Southeast Asian Countries: A Systematic Review. Health Soc. Care Community 2016, 24, e11–e22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dadgostar, P. Antimicrobial Resistance: Implications and Costs. Infect. Drug Resist. 2019, 12, 3903–3910. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chereau, F.; Opatowski, L.; Tourdjman, M.; Vong, S. Risk Assessment for Antibiotic Resistance in South East Asia. BMJ 2017, 358, 2–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Bank. World Development Indicators|DataBank. Available online: https://databank.worldbank.org/source/world-development-indicators (accessed on 20 October 2021).
- Sommanustweechai, A.; Chanvatik, S.; Sermsinsiri, V.; Sivilaikul, S.; Patcharanarumol, W.; Yeung, S.; Tangcharoensathien, V. Antibiotic Distribution Channels in Thailand: Results of Key-Informant Interviews, Reviews of Drug Regulations and Database Searches. Bull. World Health Organ. 2018, 96, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Auta, A.; Hadi, M.A.; Oga, E.; Adewuyi, E.O.; Abdu-Aguye, S.N.; Adeloye, D.; Strickland-Hodge, B.; Morgan, D.J. Global Access to Antibiotics without Prescription in Community Pharmacies: A Systematic Review and Meta-Analysis. J. Infect. 2019, 78, 8–18. [Google Scholar] [CrossRef]
- Panumart, P.; Phodha, T.; Thamlikitkul, V.; Riewpaiboon, A.; Prakongsai, P.; Limwattananon, S. Health and Economic Impacts of Antimicrobial Resistant Infections in Thailand: A Preliminary Study. J. Health Syst. Res. 2012, 6, 352–360. [Google Scholar] [CrossRef]
- Pearson, M.; Chandler, C. Knowing Antimicrobial Resistance in Practice: A Multi-Country Qualitative Study with Human and Animal Healthcare Professionals. Glob. Health Action 2019, 12, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Sumpradit, N.; Chongtrakul, P.; Anuwong, K.; Pumtong, S.; Kongsomboon, K.; Butdeemee, P.; Khonglormyati, J.; Chomyong, S.; Tongyoung, P.; Losiriwat, S.; et al. Antibiotics Smart Use: A Workable Model for Promoting the Rational Use of Medicines in Thailand. Bull. World Health Organ. 2012, 90, 905–913. [Google Scholar] [CrossRef]
- Sumpradit, N.; Wongkongkathep, S.; Malathum, K.; Janejai, N.; Paveenkittiporn, W.; Yingyong, T.; Chuxnum, T.; Vijitleela, A.; Boonyarit, P.; Akaleephan, C.; et al. Thailand’s National Strategic Plan on Antimicrobial Resistance: Progress and Challenges. Bull. World Health Organ. 2021, 99, 661–673. [Google Scholar] [CrossRef]
- Tuntayothin, W.; Sakulbumrungsil, R.; Tunpichart, S.; Kunok, P. The Evaluation of “The Antibiotic Smart Use (ASU)” Program in Pharyngitis in Community Pharmacy, Bangkok. Value Health 2018, 21, S68. [Google Scholar] [CrossRef]
- Ilardo, M.L.; Speciale, A. The Community Pharmacist: Perceived Barriers and Patient-Centered Care Communication. Int. J. Environ. Res. Public Health 2020, 17, 536. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chanakit, T.; Low, B.Y.; Wongpoowarak, P.; Moolasarn, S.; Anderson, C. Does a Transition in Education Equate to a Transition in Practice? Thai Stakeholder’s Perceptions of the Introduction of the Doctor of Pharmacy Programme. BMC Med. Educ. 2015, 15, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chanakit, T.; Low, B.Y.; Wongpoowarak, P.; Moolasarn, S.; Anderson, C. A Survey of Pharmacy Education in Thailand. Am. J. Pharm. Educ. 2014, 78, 6–8. [Google Scholar] [CrossRef] [Green Version]
- Parinyarux, P.; Kitikannakorn, N. Professional Competency for Pharmacist in Thailand and Other-Countries and Community Pharmacy Clerkship in Thailand. Isan J. Pharm. Sci. IJPS 2019, 15, 1–13. [Google Scholar] [CrossRef]
- The Royal Thai Government. Drug Act B.E. 1967. Available online: https://www.fda.moph.go.th/sites/logistics/Thelaws_Document/Drugs%20Act,%20B.E.%202510%20(1967)/DRUGSB.E.2510.pdf (accessed on 6 August 2019).
- Donsamak, S.; Weiss, M.C.; John, D.N. Evaluation of Antibiotic Supply Decisions by Community Pharmacists in Thailand: A Vignette Study. Antibiotics 2021, 10, 154. [Google Scholar] [CrossRef]
- RDU Pharmacy Eagle. Antibiotics Smart Use Complementary Guidance for Community Pharmacist. 2017. Available online: http://www.pharmacy.psu.ac.th/images/rdu-eagle2018.pdf (accessed on 6 August 2019).
- Thavornwattanayong, W.; Tangkiatkumjai, M.; Meesawatsom, P.; Sriboonruang, T.; Yotsombut, K.; Mangkang, K. Rational Drug Use in Community Pharmacy: Academic Committee for Promoting Rational Drug Use in Community Pharmacy. 2017. Available online: http://ndi.fda.moph.go.th/uploads/archives_file/20191011103233.pdf (accessed on 6 August 2019).
- Hadi, M.A.; Karami, N.A.; Al-Muwalid, A.S.; Al-Otabi, A.; Al-Subahi, E.; Bamomen, A.; Mohamed, M.M.A.; Elrggal, M.E. Community Pharmacists’ Knowledge, Attitude, and Practices towards Dispensing Antibiotics without Prescription (DAwP): A Cross-Sectional Survey in Makkah Province, Saudi Arabia. Int. J. Infect. Dis. 2016, 47, 95–100. [Google Scholar] [CrossRef] [Green Version]
- Mansour, O.; Al-Kayali, R. Community Pharmacistsꞌ Role in Controlling Bacterial Antibiotic Resistance in Aleppo, Syria. Iran. J. Pharm. Res. 2017, 16, 1612–1620. [Google Scholar]
- Mahmoud, M.A.; Aldhaeefi, M.; Sheikh, A.; Aljadhey, H. Community Pharmacists Perspectives about Reasons behind Antibiotics Dispensing without Prescription: A Qualitative Study. Biomed. Res. 2018, 29, 3792–3796. [Google Scholar] [CrossRef] [Green Version]
- Jamshed, S.; Padzil, F.; Shamsudin, S.; Bux, S.; Jamaluddin, A.; Bhagavathula, A.; Azhar, S.; Hassali, M. Antibiotic Stewardship in Community Pharmacies: A Scoping Review. Pharmacy 2018, 6, 92. [Google Scholar] [CrossRef] [Green Version]
- Siltrakool, B.; Berrou, I.; Griffiths, D.; Alghamdi, S. Antibiotics’ Use in Thailand: Community Pharmacists’ Knowledge, Attitudes and Practices. Antibiotics 2021, 10, 137. [Google Scholar] [CrossRef]
- Tangcharoensathien, V.; Sommanustweechai, A.; Chanvatik, S.; Kosiyaporn, H.; Tisocki, K. Addressing the Threat of Antibiotic Resistance in Thailand: Monitoring Population Knowledge and Awareness. WHO South-East Asia J. Public Health 2018, 7, 73–78. [Google Scholar] [CrossRef]
- Richer, M.-C.; Ritchie, J.; Marchionni, C. Appreciative Inquiry in Health Care. Br. J. Healthc. Manag. 2010, 16, 164–172. [Google Scholar] [CrossRef]
- Trajkovski, S.; Schmied, V.; Vickers, M.; Jackson, D. Using Appreciative Inquiry to Transform Health Care. Contemp. Nurse 2013, 45, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Hung, L. Using Appreciative Inquiry to Research Practice Development. Int. Pract. Dev. J. 2017, 7, 1–7. [Google Scholar] [CrossRef]
- Netthong, R.; Ahmadi, K.; Kane, R. Antimicrobial Resistance, Pharmacists, and Appreciative Inquiry: Development of a Novel Measurement Tool. Antibiotics 2020, 9, 798. [Google Scholar] [CrossRef] [PubMed]
- Trevitt Scott, J.; Cheryl Armstrong, A. Disrupting the Deficit Discourse: Reframing Metaphors for Professional Learning in the Context of Appreciative Inquiry. Prof. Dev. Educ. 2018, 45, 114–124. [Google Scholar] [CrossRef]
- Curtis, K.; Gallagher, A.; Ramage, C.; Montgomery, J.; Martin, C.; Leng, J.; Theodosius, C.; Glynn, A.; Anderson, J.; Wrigley, M. Using Appreciative Inquiry to Develop, Implement and Evaluate a Multi-Organisation ‘Cultivating Compassion’ Programme for Health Professionals and Support Staff. J. Res. Nurs. 2017, 22, 150–165. [Google Scholar] [CrossRef] [Green Version]
- Whitney, D.K.; Trosten-Bloom, A. The Power of Appreciative Inquiry: A Practical Guide to Positive Change; Berrett-Koehler Publishers: San Francisco, CA, USA, 2010. [Google Scholar]
- Lambert, H.; Chen, M.; Cabral, C. Antimicrobial Resistance, Inflammatory Responses: A Comparative Analysis of Pathogenicities, Knowledge Hybrids and the Semantics of Antibiotic Use. Palgrave Commun. 2019, 5, 1–13. [Google Scholar] [CrossRef]
- Cooperrider, D.L.; Whitney, D.K. Appreciative Inquiry: A Positive Revolution in Change, 1st ed.; Berrett-Koehler Publishers: San Francisco, CA, USA, 2005. [Google Scholar]
- Dryden, M.S.; Cooke, J.; Davey, P. Antibiotic Stewardship-More Education and Regulation Not More Availability? J. Antimicrob. Chemother. 2009, 64, 885–888. [Google Scholar] [CrossRef]
- Držaić, M.; Kummer, I.; Mucalo, I.; Bruno, A.; Hadžiabdić, M.O. Identifying Self-Assessed Competencies and Areas for Improvement within Community Pharmacist-Preceptors Support during Pre-Registration Training. BMC Med. Educ. 2018, 18, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zeitoun, A.; Sacre, H.; Hallit, S.; Zeenny, R.M.; Sili, G.; Salameh, P. Clinical Preceptor Competencies for a Better Pharmacy Education: A Suggested Framework for Lebanon. J. Pharm. Policy Pract. 2000, 13, 1–4. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The Legal and Regulatory Framework for Community Pharmacies in the WHO European Region; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2019. [Google Scholar]
- Alkhateeb, F.M.; Clauson, K.A.; Latif, D.A. Availability and Perceived Value of Masters of Business Administration Degree Programs in Pharmaceutical Marketing and Management. Am. J. Pharm. Educ. 2012, 76, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Charani, E.; Castro-Sanchéz, E.; Bradley, S.; Nathwani, D.; Holmes, A.H.; Davey, P. Implementation of Antibiotic Stewardship in Different Settings-Results of an International Survey. Antimicrob. Resist. Infect. Control 2019, 8, 1–6. [Google Scholar] [CrossRef]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The Threat of Antimicrobial Resistance in Developing Countries: Causes and Control Strategies. Antimicrob. Resist. Infect. Control 2017, 6, 1–8. [Google Scholar] [CrossRef]
- Rusic, D.; Bukić, J.; Perisin, A.S.; Leskur, D.; Modun, D.; Petric, A.; Vilovic, M.; Bozic, J. Are We Making the Most of Community Pharmacies? Implementation of Antimicrobial Stewardship Measures in Community Pharmacies: A Narrative Review. Antibiotics 2021, 10, 63. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Sridhar, D.; Blaser, M.; Wang, M.; Woolhouse, M. Achieving Global Targets for Antimicrobial Resistance. Science 2016, 353, 874–875. [Google Scholar] [CrossRef] [Green Version]
- Rogers, S.; Katwyk, V.; Hoffman, S.J.; Mendelson, M.; Taljaard, M.; Grimshaw, J.M. Strengthening the Science of Addressing Antimicrobial Resistance: A Framework for Planning, Conducting and Disseminating Antimicrobial Resistance Intervention Research. Health Res. Policy Syst. 2020, 18, 1–13. [Google Scholar] [CrossRef]
- Veepanattu, P.; Singh, S.; Mendelson, M.; Nampoothiri, V.; Edathadatil, F.; Surendran, S.; Bonaconsa, C.; Mbamalu, O.; Ahuja, S.; Birgand, G.; et al. Building Resilient and Responsive Research Collaborations to Tackle Antimicrobial Resistance—Lessons Learnt from India, South Africa, and UK. Int. J. Infect. Dis. 2020, 100, 278–282. [Google Scholar] [CrossRef]
- Alhomoud, F.; Almahasnah, R.; Kais Alhomoud, F. “You Could Lose When You Misuse”-Factors Affecting over-the-Counter Sale of Antibiotics in Community Pharmacies in Saudi Arabia: A Qualitative Study. BMC Health Serv. Res. 2018, 18, 1–9. [Google Scholar] [CrossRef]
- Founou, R.C.; Founou, L.L.; Essack, S.Y. Clinical and Economic Impact of Antibiotic Resistance in Developing Countries: A Systematic Review and Meta-Analysis. PLoS ONE. 2017, 12, e0189621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotwani, A.; Wattal, C.; Joshi, P.C.; Holloway, K. Irrational Use of Antibiotics and Role of the Pharmacist: An Insight from a Qualitative Study in New Delhi, India. J. Clin. Pharm. Ther. 2012, 37, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Porter, G.; Kotwani, A.; Bhullar, L.; Joshi, J. Over-the-Counter Sales of Antibiotics for Human Use in India: The Challenges and Opportunities for Regulation. Med. Law Int. 2021, 21, 147–173. [Google Scholar] [CrossRef]
- Tangcharoensathien, V.; Chanvatik, S.; Sommanustweechai, A. Complex Determinants of Inappropriate Use of Antibiotics. Bull. World Health Organ. 2018, 96, 141–144. [Google Scholar] [CrossRef]
- Khan, F.U.; Khan, F.U.; Hayat, K.; Ahmad, T.; Khan, A.; Chang, J.; Malik, U.R.; Khan, Z.; Lambojon, K.; Fang, Y. Knowledge, Attitude, and Practice on Antibiotics and Its Resistance: A Two-Phase Mixed-Methods Online Study among Pakistani Community Pharmacists to Promote Rational Antibiotic Use. Int. J. Environ. Res. Public Health 2021, 18, 1320. [Google Scholar] [CrossRef]
- Whitaker, C.; Stevelink, S.; Fear, N. The Use of Facebook in Recruiting Participants for Health Research Purposes: A Systematic Review. J. Med. Internet Res. 2017, 19, e290. [Google Scholar] [CrossRef] [Green Version]
- Smith, W.G. Does Gender Influence Online Survey Participation? San José State University: San Jose, CA, USA, 2008. [Google Scholar]
- Janzen, D.; Fitzpatrick, K.; Jensen, K.; Suveges, L. Women in Pharmacy: A Preliminary Study of the Attitudes and Beliefs of Pharmacy Students. Can. Pharm. J. 2013, 146, 109–116. [Google Scholar] [CrossRef] [Green Version]
- Thailand|Institute for Health Metrics and Evaluation. Available online: http://www.healthdata.org/thailand (accessed on 2 August 2019).
- Gibson, C.B. Elaboration, Generalization, Triangulation, and Interpretation: On Enhancing the Value of Mixed Method Research. Organ. Res. Methods 2017, 20, 193–223. [Google Scholar] [CrossRef] [Green Version]
- World Bank. Thailand Overview. Available online: https://www.worldbank.org/en/country/thailand/overview (accessed on 10 July 2019).
- Sarwar, M.R.; Saqib, A.; Iftikhar, S.; Sadiq, T. Knowledge of Community Pharmacists about Antibiotics, and Their Perceptions and Practices Regarding Antimicrobial Stewardship: A Cross-Sectional Study in Punjab, Pakistan. Infect. Drug Resist. 2018, 11, 133–145. [Google Scholar] [CrossRef] [Green Version]
- Siltrakool, B. Assessment of Community Pharmacists ’ Knowledge, Attitude and Practice Regarding Non-Prescription Antimicrobial Use and Resistance in Thailand. Fulfilment of the Requirements for The University of Hertfordshire. 2017. Unpublished. Available online: https://uhra.herts.ac.uk/handle/2299/19619 (accessed on 2 September 2019).
- López-Vázquez, P.; Vázquez-Lago, J.M.; Gonzalez-Gonzalez, C.; Piñeiro-Lamas, M.; López-Durán, A.; Herdeiro, M.T.; Figueiras, A.; Caamaño-Isorna, F.; Gestal-Otero, J.J.; Taracido, M.; et al. Development and Validation of the Knowledge and Attitudes Regarding Antibiotics and Resistance (KAAR-11) Questionnaire for Primary Care Physicians. J. Antimicrob. Chemother. 2016, 71, 2972–2979. [Google Scholar] [CrossRef]
- Truter, I.; Knoesen, B.C. Perceptions towards the Prescribing of Antibiotics by Pharmacists and the Use of Antibiotics in Primary Care in South Africa. J. Infect. Dev. Ctries. 2018, 12, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Hardy-Holbrook, R.; Aristidi, S.; Chandnani, V.; Dewindt, D.; Dinh, K. Antibiotic Resistance and Prescribing in Australia: Current Attitudes and Practice of GPs. Healthc. Infect. 2013, 18, 147–151. [Google Scholar] [CrossRef] [Green Version]
- Mccarthy, B. Appreciative Inquiry: An Alternative to Behaviour Management. Dementia 2016, 16, 249–253. [Google Scholar] [CrossRef] [PubMed]
- Qualtrics. Qualtrics: Provo, Utah, USA. 2005. Available online: https://www.qualtrics.com (accessed on 10 October 2020).
- RStudio Team. RStudio: Integrated Development for R; RStudio, PBC: Boston, MA, USA, 2020; Available online: http://www.rstudio.com/ (accessed on 10 October 2020).
- Davidson, C.; Australia, C.R. Transcription: Imperatives for Qualitative Research. Int. J. Qual. Methods 2009, 8, 35–52. [Google Scholar] [CrossRef]
- QSR International Pty Ltd. NVivo (Version 12). 2018. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home (accessed on 10 October 2020).
| Characteristics | N = 387 (%) |
|---|---|
| Gender | |
| Male | 131 (33.85) |
| Female | 256 (66.15) |
| Age | |
| Less than 30 | 163 (42.12) |
| 30–39 | 162 (41.86) |
| 40–49 | 42 (10.85) |
| 50–59 | 13 (3.36) |
| 60 and above | 7 (1.81) |
| Postgraduate qualification | |
| Yes | 47 (12.14) |
| No | 340 (87.86) |
| Location in Thailand | |
| Central | 149 (38.50%) |
| Northeastern (Isan) | 117 (30.23%) |
| Eastern | 39 (10.08%) |
| Southern | 38 (9.82%) |
| Northern | 22 (5.68%) |
| Western | 5 (1.29%) |
| Statements | Those Who Chose the Right Answer | Those Who Chose the Wrong Answer |
|---|---|---|
| Dispensing antibiotics without a prescription is a legal practice in Thailand. | 93.80% (n = 363) | 6.20% (n = 24) |
| Dispensing antibiotics without a prescription is a common practice among community pharmacists in Thailand. | 96.38% (n = 373) | 3.62% (n = 14) |
| Dispensing antibiotics without a prescription is contributing to the development of antibiotic resistance. | 55.81% (n = 216) | 44.19% (n = 171) |
| Dispensing antibiotics without a prescription is contributing to the inappropriate use of antibiotics by patients. | 57.62% (n = 223) | 42.38% (n = 164) |
| Antibiotics are indicated to reduce any kind of pain and inflammation. | 3.36% (n = 13) | 96.64% (n = 374) |
| Antibiotics are useful for bacterial infections. | 97.93% (n = 379) | 2.07% (n = 8) |
| Antibiotics can cause secondary infections after killing the normal flora of the human body. | 93.54% (n = 362) | 6.46% (n = 25) |
| Superbugs are microorganisms which generate antimicrobial resistance. They include bacteria, fungal, viruses or parasites. | 71.32% (n = 276) | 28.68% (n = 111) |
| Resistance DNA in bacteria can transfer to other bacteria by a virus (bacteriophage). | 73.90% (n = 286) | 26.10% (n = 98) |
| The main objective of antibiotic stewardship is the achievement of the most effective clinical outcome with the least adverse reactions. | 89.92% (n = 348) | 10.08% (n = 39) |
| Questions | Very Good | Good | Unsure | Poor | Very Poor |
|---|---|---|---|---|---|
| How do you rate the implementation of local guidelines such as Antibiotic Smart Use (ASU) by the Ministry of Health, before dispensing antibiotics? | 22.74% (n = 88) | 64.60% (n = 250) | 12.14% (n = 47) | 0.52% (n = 2) | 0% (n = 0) |
| How do you rate the clarity of the advice given to the patients about their dispensed antibiotics? | 35.65% (n = 138) | 61.76% (n = 239) | 2.58% (n = 10) | 0% (n = 0) | 0% (n = 0) |
| How do you rate the acknowledgment of the patients’ understanding of the advice given to them about their dispensed antibiotics? | 10.85% (n = 42) | 51.68% (n = 200) | 34.63% (n = 134) | 2.58% (n = 10) | 0.26% (n = 1) |
| How do you rate the answering of patients’ questions about their dispensed antibiotics? | 36.18% (n = 140) | 61.76% (n = 239) | 2.07% (n = 8) | 0% (n = 0) | 0% (n = 0) |
| How do you rate patients’ satisfaction with antibiotic dispensing? | 19.64% (n = 76) | 60.98% (n = 236) | 19.12% (n = 74) | 0.26% (n = 1) | 0% (n = 0) |
| How do you rate the patients’ knowledge about antibiotic stewardship before counseling? | 4.65% (n = 18) | 26.87% (n = 104) | 32.56% (n = 126) | 31.01% (n = 120) | 4.91% (n = 19) |
| How do you rate the Thai- FDA support to implement antibiotic stewardship in community pharmacy? | 4.39% (n = 17) | 34.89% (n = 135) | 45.74% (n = 177) | 12.40% (n = 48) | 2.58% (n = 10) |
| How do you rate engagement with antibiotic awareness campaigns? | 17.83% (n = 69) | 62.01% (n = 240) | 17.83% (n = 69) | 2.33% (n = 9) | 0% (n = 0) |
| How do you rate engagement with health promotion campaigns on prevention/reduction transmission of infection? | 17.05% (n = 66) | 59.17% (n = 229) | 20.16% (n = 78) | 3.10% (n = 12) | 0.52% (n = 2) |
| How do you rate collaboration (such as referral) with other healthcare professionals to implement antibiotic stewardship? | 27.91% (n = 108) | 54.01% (n = 209) | 15.50% (n = 60) | 2.33% (n = 9) | 0.26% (n = 1) |
| How do you rate the relationship between clients/patients and pharmacists in regards with antibiotic stewardship? | 15.76% (n = 61) | 68.48% (n = 265) | 13.95% (n = 54) | 1.81% (n = 7) | 0% (n = 0) |
| Variables | Attitude | |||
|---|---|---|---|---|
| β 1 | SE 2 | 95% CI 3 | p-Value | |
| Age | 0.34 | 0.57 | 0.78–1.46 | 0.5550 |
| Male | −2.37 | 1.07 | −4.46–−0.28 | 0.0265 * |
| Postgraduate education | 5.16 | 1.50 | 2.21–8.11 | 0.000664 ** |
| Variables | N = 387 (%) | Attitude | ||||
|---|---|---|---|---|---|---|
| β 1 | SE 2 | 95% CI 3 | p-Value | |||
| Knowledge | Mean = 82.96 | −0.01 | 0.03 | −0.08–0.6 | 0.82 | |
| Training experience during pharmacy course | ||||||
| No | 211 (54.52) | 1.78 | 1.01 | −0.21–3.77 | 0.0804 | |
| Yes | 97 (25.07) | |||||
| Not sure | 79 (20.41) | |||||
| Training experience since degree qualified | ||||||
| Yes | 120 (31.01) | 2.07 | 1.09 | −0.07–4.21 | 0.0593 # | |
| No | 267 (68.99) | |||||
| Sources of knowledge a | ||||||
| Training session | 274 | 3.14 | 1.11 | 0.96–5.31 | 0.00485 ** | |
| Special literature | 245 | 2.63 | 1.04 | 0.58–4.69 | 0.0122 * | |
| Patient information leaflet | 139 | −0.12 | 1.06 | −2.19–1.97 | 0.9140 | |
| Sales representative | 106 | 2.38 | 1.13 | 0.14–4.60 | 0.0365 * | |
| Articles in CCPE | 297 | 0.82 | 1.21 | −1.55–3.18 | 0.4980 | |
| Guidelines | 258 | 1.51 | 1.07 | −0.60–3.62 | 0.1600 | |
| Others | 9 | −2.74 | 3.37 | −9.36–3.87 | 0.4160 | |
| Variables | N = 387 (%) | Attitude | |||
|---|---|---|---|---|---|
| β 1 | SE 2 | 95% CI 3 | p-Value | ||
| Professional degree a | |||||
| BSc in Pharmacy | 202 (52.20) | 0.41 | 1.02 | −1.58–2.41 | 0.68 |
| PharmD (Pharmaceutical Care) | 150 (38.76) | −0.69 | 1.04 | −2.74–1.36 | 0.507 |
| PharmD (Industrial Pharmacy) | 31 (8.00) | 0.84 | 1.87 | −2.83–4.52 | 0.651 |
| PharmD (Pharmaceutical and Health Consumer Protection) | 2 (0.52) | 0.38 | 7.08 | −13.55–14.30 | 0.9570 |
| PharmD (English programme) | 2 (0.52) | −0.63 | 7.08 | −14.55–13.30 | 0.9290 |
| Clerkship a | |||||
| Community pharmacy | 329 | 1.36 | 1.42 | −1.42–4.15 | 0.3380 |
| Hospital pharmacy | 319 | 0.06 | 1.33 | −2.55–2.68 | 0.9630 |
| Manufacturing | 105 | 1.65 | 1.14 | −0.59–3.88 | 0.1490 |
| Drug registration | 31 | 2.85 | 1.86 | −0.81–6.50 | 0.1280 |
| Regulation and jurisdiction | 44 | 2.81 | 1.59 | −0.31–5.93 | 0.0787 # |
| Research and development | 56 | 2.22 | 1.42 | −0.58–5.02 | 0.1210 |
| Variables | N = 387 (%) | Attitude | |||
|---|---|---|---|---|---|
| β 1 | SE 2 | 95% CI 3 | p-Value | ||
| Experience as community pharmacist | |||||
| Year | Mean = 5.59 | 0.07 | 0.08 | −0.09–0.23 | 0.0593 # |
| Student internships | |||||
| No | 303 (78.29) | 4.28 | 1.21 | 1.91–6.66 | 0.000463 *** |
| Yes | 84 (21.71) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Netthong, R.; Kane, R.; Ahmadi, K. Antimicrobial Resistance and Community Pharmacists’ Perspective in Thailand: A Mixed Methods Survey Using Appreciative Inquiry Theory. Antibiotics 2022, 11, 161. https://doi.org/10.3390/antibiotics11020161
Netthong R, Kane R, Ahmadi K. Antimicrobial Resistance and Community Pharmacists’ Perspective in Thailand: A Mixed Methods Survey Using Appreciative Inquiry Theory. Antibiotics. 2022; 11(2):161. https://doi.org/10.3390/antibiotics11020161
Chicago/Turabian StyleNetthong, Rojjares, Ros Kane, and Keivan Ahmadi. 2022. "Antimicrobial Resistance and Community Pharmacists’ Perspective in Thailand: A Mixed Methods Survey Using Appreciative Inquiry Theory" Antibiotics 11, no. 2: 161. https://doi.org/10.3390/antibiotics11020161
APA StyleNetthong, R., Kane, R., & Ahmadi, K. (2022). Antimicrobial Resistance and Community Pharmacists’ Perspective in Thailand: A Mixed Methods Survey Using Appreciative Inquiry Theory. Antibiotics, 11(2), 161. https://doi.org/10.3390/antibiotics11020161








