Surgical Excision of Unusual Sacked Neck and Mediastinum Abscess of Odontogenic Origin
Abstract
1. Introduction
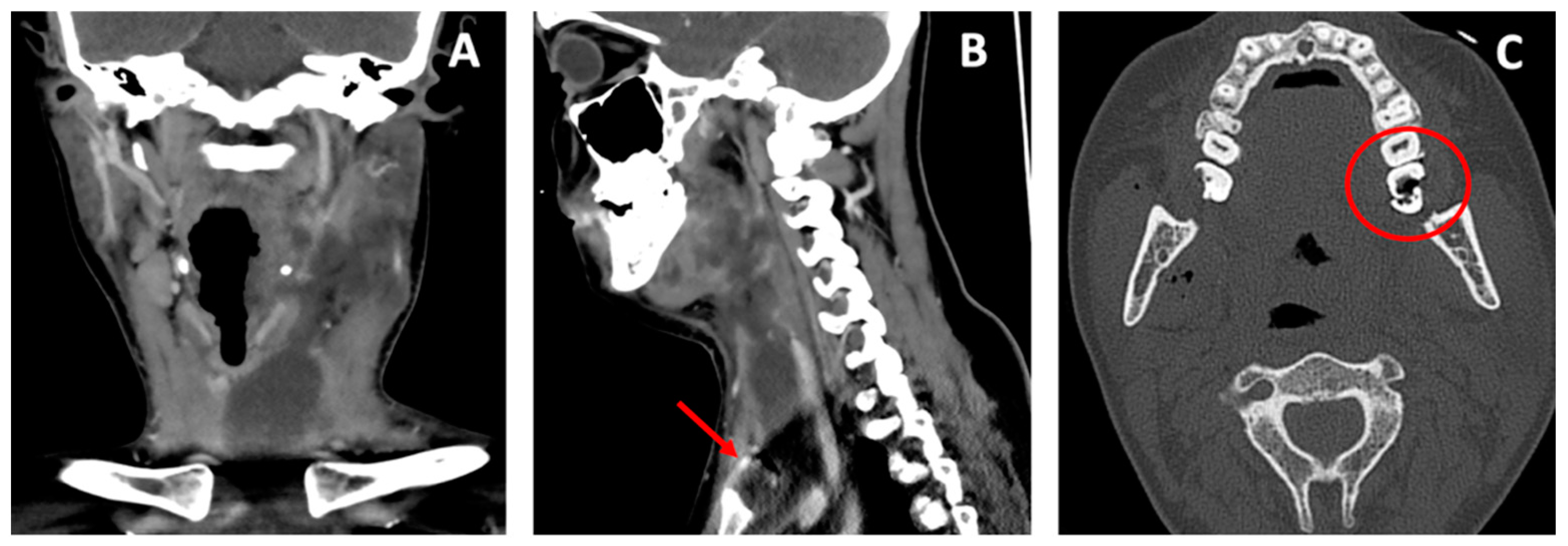
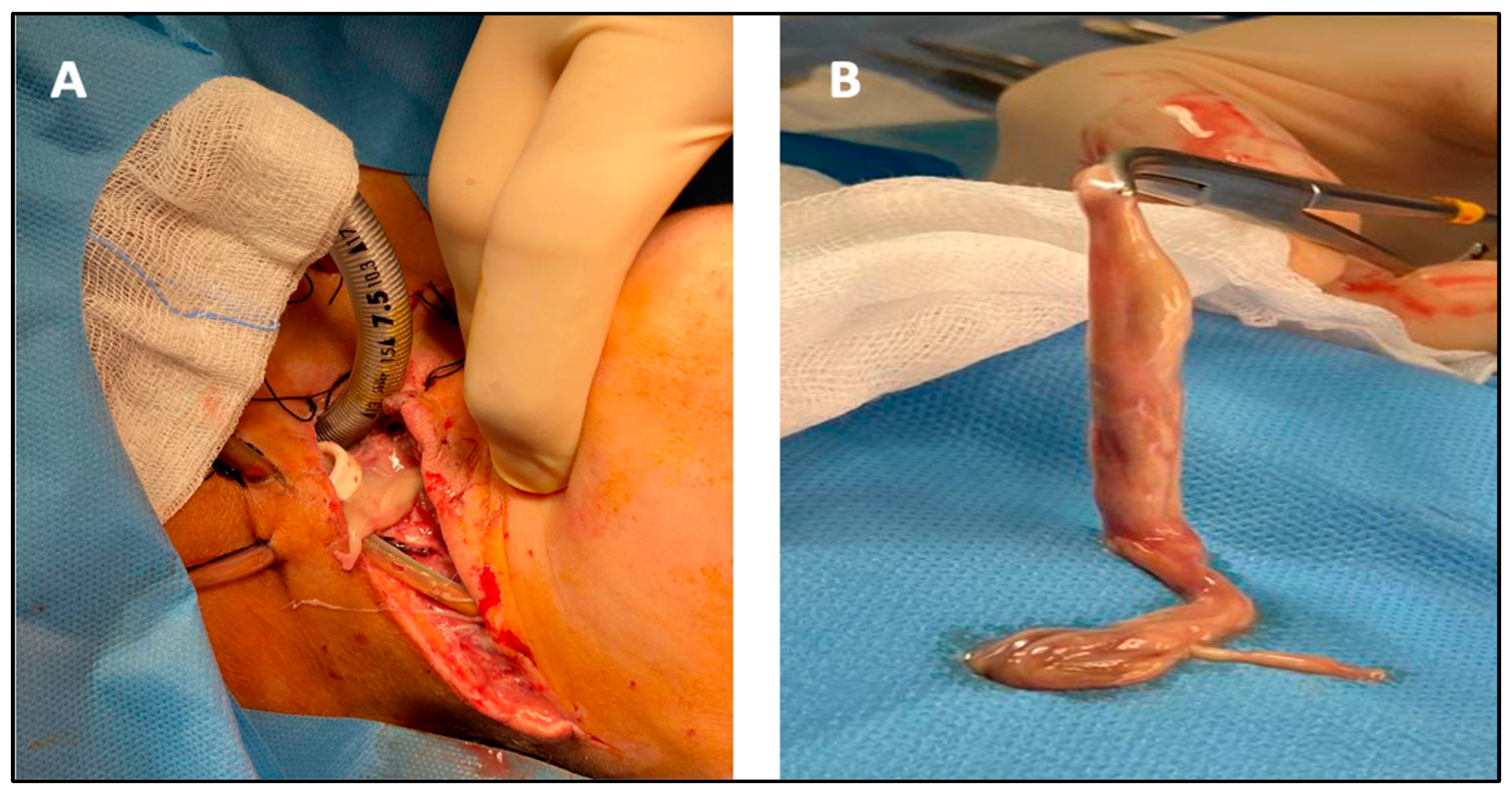
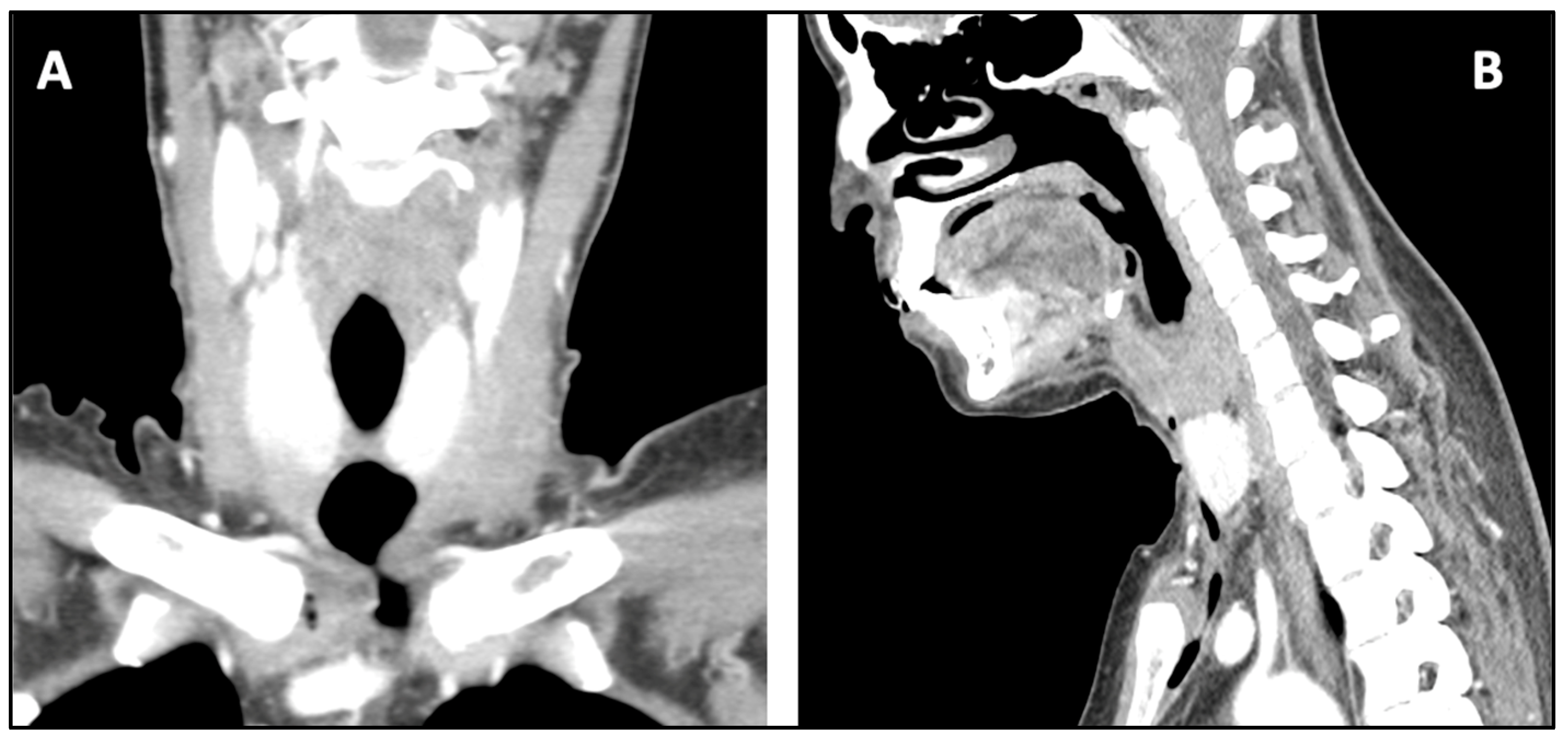
2. Case Report
3. Discussion
4. Limits of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ogle, O.E. Odontogenic Infections. Dent. Clin. N. Am. 2017, 61, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Arweiler, N.B.; Netuschil, L. The Oral Microbiota. Microbiota Hum. Body 2016, 902, 45–60. [Google Scholar] [CrossRef]
- Galli, M.; De Soccio, G.; Cialente, F.; Candelori, F.; Federici, F.R.; De Vincentiis, M.; Minni, A. Chronic maxillary sinusitis of dental origin and oroantral fistula: The results of combined surgical approach in an Italian university hospital. Bosn. J. Basic Med. Sci. 2020, 20, 524–530. [Google Scholar] [CrossRef]
- Johri, A.; Piecuch, J.F. Should Teeth Be Extracted Immediately in the Presence of Acute Infection? Oral Maxillofac. Surg. Clin. N. Am. 2011, 23, 507–511. [Google Scholar] [CrossRef] [PubMed]
- Abyaneh, M.-A.Y.; Griffith, R.; Falto-Aizpurua, L.; Nouri, K. Famous Lines in History. JAMA Dermatol. 2014, 150, 1087. [Google Scholar] [CrossRef] [PubMed]
- Aboh, I.V.; Chisci, G.; Salini, C.; Gennaro, P.; Cascino, F.; Gabriele, G.; Iannetti, G. Submandibular Ossifying Lipoma. J. Craniofacial Surg. 2015, 26, 973–974. [Google Scholar] [CrossRef] [PubMed]
- Cambria, F.; Fusconi, M.; Candelori, F.; Galli, M.; Stanganelli, F.R.F.; Venuta, F.; Valentini, V.; de Vincentiis, M. Surgical multidisciplinary approach in the management of odontogenic or non-odontogenic neck infections. Acta Otorhinolaryngol. Ital. 2021, 41, S138–S144. [Google Scholar] [CrossRef] [PubMed]
- López-Marcos, J.F. Aetiology, classification and pathogenesis of pulp and periapical disease. Med. Oral Patol. Oral Cir. Bucal. 2004, 9, 52–62. [Google Scholar]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- D’Erme, G.; Galli, M.; Federici, F.R.; Colizza, A.; Ralli, M.; de Vincentiis, M. Report of a rare case of Lemierre’s syndrome associated with a multidrug resistant dental abscess. Otorhinolaryngology 2020, 70, 6–10. [Google Scholar] [CrossRef]
- Almutairi, D.M.; Alqahtani, R.M.; Alshareef, N.; Alghamdi, Y.S.; Al-Hakami, H.A.; Algarni, M. Deep Neck Space Infections: A Retrospective Study of 183 Cases at a Tertiary Hospital. Cureus 2020, 12, e6841. [Google Scholar] [CrossRef] [PubMed]
- Guillier, D.; Moris, V.; Al Hindi, A.; Rem, K.; Chatel, H.; See, L.-A.; Revol, M.; Dorval, S.M. Surgical approaches in neck dissection: Comparing functional, oncologic and aesthetic aspects of transverse cervicotomy to Paul André’s approach. In Annales de Chirurgie Plastique Esthétique; Elsevier Masson: Amsterdam, The Netherlands, 2017; Volume 63, pp. 140–147. [Google Scholar] [CrossRef]
- Endo, S.; Murayama, F.; Hasegawa, T.; Yamamoto, S.; Yamaguchi, T.; Sohara, Y.; Fuse, K.; Miyata, M.; Nishino, H. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Gen. Thorac. Cardiovasc. Surg. 1999, 47, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Cirino, L.M.I.; Elias, F.M.; De Almeida, J.L.J. Descending mediastinitis: A review. Sao Paulo Med. J. 2006, 124, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Prado-Calleros, H.M.; Jiménez-Fuentes, E.; Jiménez-Escobar, I. Descending necrotizing mediastinitis: Systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck 2016, 38, E2275–E2283. [Google Scholar] [CrossRef] [PubMed]
- Adly, A.; Youssef, T.A.; El-Begermy, M.M.; Younis, H.M. Timing of tracheostomy in patients with prolonged endotracheal intubation: A systematic review. Eur. Arch. Oto-Rhino-Laryngol. 2017, 275, 679–690. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Colizza, A.; D’Erme, G.; Ciofalo, A.; D’Angeli, G.; Federici, F.R.; Galli, C.; De Vincentiis, M.; Galli, M. Surgical Excision of Unusual Sacked Neck and Mediastinum Abscess of Odontogenic Origin. Antibiotics 2022, 11, 1757. https://doi.org/10.3390/antibiotics11121757
Colizza A, D’Erme G, Ciofalo A, D’Angeli G, Federici FR, Galli C, De Vincentiis M, Galli M. Surgical Excision of Unusual Sacked Neck and Mediastinum Abscess of Odontogenic Origin. Antibiotics. 2022; 11(12):1757. https://doi.org/10.3390/antibiotics11121757
Chicago/Turabian StyleColizza, Andrea, Giovanni D’Erme, Andrea Ciofalo, Giacomo D’Angeli, Francesca Romana Federici, Carlotta Galli, Marco De Vincentiis, and Massimo Galli. 2022. "Surgical Excision of Unusual Sacked Neck and Mediastinum Abscess of Odontogenic Origin" Antibiotics 11, no. 12: 1757. https://doi.org/10.3390/antibiotics11121757
APA StyleColizza, A., D’Erme, G., Ciofalo, A., D’Angeli, G., Federici, F. R., Galli, C., De Vincentiis, M., & Galli, M. (2022). Surgical Excision of Unusual Sacked Neck and Mediastinum Abscess of Odontogenic Origin. Antibiotics, 11(12), 1757. https://doi.org/10.3390/antibiotics11121757







