Abstract
Staphylococcal infections represent a challenge in companion animals and hospitalized patients. This study aimed to assess the resistance of Staphylococcus pseudintermedius isolates, against a broad panel of antibacterials, including exclusive to human medicine. A total of 40 S. pseudintermedius were collected from clinical specimens of dogs (n = 31) and cats (n = 5). All strains were tested for 20 antibacterials, namely 14 Critical Important and eight Highly Important Antibacterials (CIA and HIA, respectively), indicative for 18 antimicrobial classes. All strains were susceptible to seven antibiotics (daptomycin, fosfomycin, fusidic acid, linezolid, quinupristin-dalfopristin, teicoplanin/vancomycin, tigecycline). The highest resistance was against penicillin (97.5% Confidence Interval [CI]: 83.8–100.0), whereas the lowest against telavancin (2.5%, CI: 0.0–16.2). Resistance versus Highest Priority CIA was observed, namely against macrolides (70.0, CI: 52.1–84.3), quinolones (62.5, CI: 44.5–78.3), 5th generation cephalosporins (7.5, CI: 1.3–21.6), and glycopeptides (2.5%, CI: 0.0–14.2). Among High Priority CIA, strains were resistant only to aminoglycosides (65.0, CI: 47.0–80.4) and ansamycins (12.5, CI: 3.8–28.1). We observed the highest resistance against veterinary medicine antibacterials, but there was also resistance against antibacterials exclusive to human medicine, namely ceftaroline (7.5, CI: 1.0–23.8) and telavancin. S. pseudintermedius zoonotic potential and its rate of acquisition of new resistance should encourage surveillance on a broad spectrum of antibacterials.
1. Introduction
Staphylococcus pseudintermedius was first discovered in 2005 and rapidly gained plenty of fame due to its pathogenic potential [1]. To date, there are more than 700 articles on PubMed [2] on this topic. In dogs, S. pseudintermedius is present as a normal inhabitant of the skin [3] but also as an opportunistic pathogen that causes skin, ear, and surgical-site infections. In cats, it has a lower prevalence [4], and some authors suggested that it could be due to the antagonism by Staphylococcus felis [5]. It is preferentially transmitted via direct animal–animal contact, but it has been reported to infect humans through dog–human transmission [6,7,8]. The first human case was reported in 2006; growing evidence has been pointing to this bacterium as a human pathogen of concern especially in elderly, diabetic and immunocompromised patients or in people that work in close proximity to animals [9]. Similar to other coagulase-positive staphylococci, S. pseudintermedius typically expresses various virulence factors (e.g., coagulase, cytotoxin, enterotoxin, hemolysin, leukocidins, proteases, thermonuclease, etc.) [10] and can acquire resistance to a variety of antibiotics via the acquisition of resistance genes (e.g., blaZ and mecA for β-lactams, tetK and tetM for tetracyclines, erm for erythromycin, etc.) [11]. Since its discovery, it has been of increasing concern due to its high genetic heterogeneity, which makes it hard to type [12]. Companion animals sharing the same environment with their owners can transmit not only pathogens but resistance genes as well [13,14]. In recent years, the EU legislation curtailed the number of antibacterials available for veterinary prescription to lower the risk of antimicrobial resistance (AMR) derived from treatment in veterinary medicine [15]. With a similar aim, the World Health Organization (WHO) developed the criteria to rank antibacterials depending on their importance in human medicine [16,17]. The list of antimicrobials important for human medicine—first presented in Canberra in 2005—was revised multiple times until 2018. The purpose of this document was to increase the awareness of public and animal health authorities, physicians, and veterinarians about the prudent use of antimicrobials, especially the critically important. To draft it, two different criteria were implemented: (C1) “The antimicrobial class is the sole, or one of limited available therapies, to treat serious bacterial infections in people”, and (C2) “The antimicrobial class is used to treat infections in people caused by either: (1) bacteria that may be transmitted to humans from non-human sources, or (2) bacteria that may acquire resistance genes from non-human sources” [17]. Following these criteria, antimicrobials were defined as critically important (CIA) when they meet both C1 and C2, highly important (HIA) if they meet either C1 or C2, or important (IA) when neither C1 nor C2 is met. Three further prioritization factors were applied to subdivide CIA having high (HCIA) or the highest priority (HPCIA), depending on the amount of evidence that shows frequent transmission of resistant bacteria or genetic elements.
In 2017, WHO developed the Access, Watch, Reserve (AWaRe) classification of antibacterials to emphasize the importance of their prudent use [18]. More than 250 antimicrobials have been classified into three groups, Access, Watch and Reserve, depending on their relevance for antimicrobial resistance. The Access group includes antibacterials with low resistance potential and are active on a wide range of susceptible pathogens; the Watch group are antibacterials with a higher resistance potential, most of them being CIA; the Reserve group includes the antibacterials that should be used only as last resort options to treat confirmed or suspected infections due to multi-drug-resistant organisms [18].
Since 2014, the European Medicines Agency (EMA) expert group has been updating the categorization of antibacterials for veterinary medicine, acknowledging the WHO’s CIA list. This categorization was intended to promote the responsible use of antibacterials to protect public and animal health [15]. It subdivides antimicrobials into four categories: cat. A “Avoid” includes those not authorized in veterinary medicine and exclusive to human medicine; cat. B “Restrict” includes all HPCIA not in cat. A except for macrolides; cat. C “Caution” are antibacterials with an alternative in human medicine but still at risk of developing resistance to a substance in cat. A, or without a less hazardous alternative in veterinary medicine; cat. D “Prudence” includes antibacterials with available alternatives in veterinary medicine that do not select for resistance to cat. A substances. It is noteworthy that cat. A comprehends all newly discovered substances, which may be used only for individual treatment in companion animals and under exceptional circumstances.
Reducing the number of antibiotics available for veterinary prescription determined the concomitant reduction in the number of antimicrobial susceptibility tests performed for clinical purposes in many veterinary laboratories. However, since S. pseudintermedius is of concern also for public health, it is of utmost importance to monitor the progress of its resistance pattern toward a broad panel of antibacterials that includes cat. A substances as well. However, one of the main problems of antimicrobial susceptibility testing (AST) in veterinary medicine is the absence of reliable clinical breakpoints for many pathogen-species-administration route combinations. The paucity of veterinary-specific data forces laboratories to refer alternatively to standards provided for human medicine by the Clinical Laboratory Standard Institute (CLSI) or the European Committee for AST (EUCAST).
This study aimed to assess the resistance of zoo-pathogenic S. pseudintermedius strains against a broad spectrum of antimicrobials of many different classes, including some exclusive to human medicine.
2. Results
All the strains were resistant to at least one antibiotic. They were all susceptible to seven antibacterials, namely tigecycline, fosfomycin, fusidic acid, linezolid, teicoplanin/vancomycin, daptomycin, and streptogramins. The highest resistance was observed against penicillin since all but one isolates were resistant (97.5%, CI: 88.7–99.9). The lowest was reported for glycopeptides, with only one strain resistant to telavancin (2.5%, CI: 0.1–11.3). Resistance higher than 50% was recorded for six classes of antibacterials, namely against macrolides and lincosamides (70.0%, CI: 56.0–81.7%), aminoglycosides (65.0%, CI: 50.8–77.4%), fluoroquinolones (62.5%, CI: 48.3–75.3%), sulfamethoxazole-trimethoprim (60.0%, CI: 45.8–73.1%), and tetracyclines (57.5%, CI: 45.8–73.1%). Lower resistance was observed towards chloramphenicol (27.5%, CI: 16.3–41.4%) and rifampicin (12.5%, CI: 5.1–24.5%).
Among the 39 strains resistant to penicillin, 24 (61.5%) were resistant to oxacillin, thus being classified as methicillin-resistant S. pseudintermedius (MRSP). Furthermore, out of 24 MRSP, 3 (12.5%) were resistant (R) to 5th generation cephalosporins and another 3 were susceptible to increased dosage (I) only (Table 1).

Table 1.
Results of antimicrobial susceptibility testing. Absolute frequency of sensitive (S), sensitive to increased dosage (I) and resistant (R) strains are reported along with the prevalence of R strains and 90% confidence intervals (CI) for each antibacterial tested.
Resistance versus HPCIA was observed, namely against macrolides, quinolones, 5th-generation cephalosporins, and glycopeptides. Regarding HCIA, strains were resistant only to aminoglycosides and ansamycins. Up to four strains were resistant against antibacterials in the Reserve category, namely three to ceftaroline and one to telavancin. A similar situation is reported for cat. A antibacterials, where four strains were resistant to rifampicin, two to ceftaroline, one to telavancin, and one to rifampicin and ceftaroline (Table 2).

Table 2.
Results of antimicrobial susceptibility tests aggregated by World Health Organization (WHO and AWaRe) and European Medicines Agency (AMEG) classifications of antibacterials. The absolute frequency of sensitive (S), sensitive to increased dosage (I), and resicannt (R) strains is reported along with the prevalence of R strains with 90% confidence intervals (CI).
There was no difference among WHO categories since resistance to CIA quite matched HIA (Figure 1a). Regarding the AWaRe classification, the highest prevalence of resistant strains was observed against Access antibacterials, followed by Watch and Reserve (Figure 1b). The prevalence of strains resistant to Access antibacterials was significantly higher than those of the Reserve (p = 0.005). Regarding AMEG classification, the prevalence of strains resistant to cat. A antibacterials was significantly lower, compared to cat. C (p = 0.027). However, up to 12.5% prevalence was observed for rifampicin and 7.5% for ceftaroline, also with three strains susceptible to increased dosage (I). Four out of five cat. D antibacterials had a point-estimated resistance of over 50% with the only exception of fusidic acid.
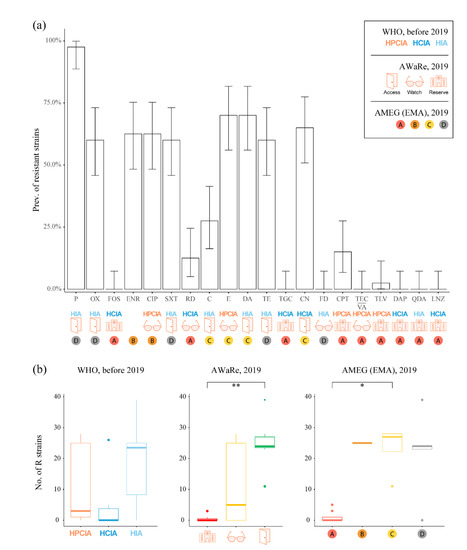
Figure 1.
Bar plot of the prevalence of resistant strains (a). The height of the bars represents the point estimate prevalence of resistantstrains (R) to each antibacterial, with error bars indicating the 90% confidence intervals. Under the antibacterial name, World Health Organization (WHO and AWaRe) and European Medicines Agency (AMEG) classifications are reported. Box plots of the frequency of R strains (b). Data are aggregated by WHO, AWaRe and AMEG categories (*: p < 0.05; **: p < 0.01). Category abbreviations: HPCIA: Highest Priority, Critically Important Antimicrobials; HCIA: High priority, Critically Important Antimicrobials; HIA: Highly Important Antimicrobials. Antibacterial abbreviations: P: penicillin G; OX: oxacillin; FOS: fosfomycin; ENR: enrofloxacin; CIP: ciprofloxacin; SXT: trimethoprim-sulfamethoxazole; RD: rifampicin; C: chloramphenicol; E: erythromycin; DA: clindamycin; TE: tetracycline; TGC: tigecycline; CN: gentamycin; FD: fusidic acid; CPT: ceftaroline; TEC/VA: teicoplanin/vancomycin; TLV: telavancin; DAP: daptomycin; QDA: quinupristin-dalfopristin; LNZ: linezolid. Note: the colours are those used by WHO and EMA to identify the categories of antibacterials.
Nineteen different antimicrobial-resistance (AMR) profiles (from A to S) were identified, which are resistant to a median of 8.5 antibacterials (mean ± standard deviation = 6.9 ± 3.5). A total of 2 of them were resistant to 11 antibacterials, 3 to 10, 5 to 9 and 1 to 8, whereas 8 were resistant to no more than 6 antibacterials each. Among them, only profile K was resistant to telavancin, along with penicillin and gentamycin. The highest frequency was recorded for profile B (freq = 7), which was susceptible to all antibacterials but penicillin, followed by profile E (freq. = 6, resistance to 9 antibacterials), C (freq. = 3, resistance to 8 antibacterials) and F (freq. = 3, resistance to 10 antibacterials).
Eleven profiles (57.9%) were attributable to MRSP. Except for Q, the other profiles of methicillin-susceptible S. pseudintermedius (MSSP) were resistant to no more than six antibacterials. Accordingly, MRSP strains were significantly (p < 0.0001) resistant to more antibacterials (median = 9, mean ± standard deviation = 8.9 ± 2.3) than MSSP strains (median = 2, mean ± s.d. = 3.3 ± 2.9). MRSP strains were significantly more resistant to aminoglycosides (p < 0.0001), macrolides and lincosamides (p < 0.001), quinolones (p < 0.0001), sulfamethoxazole-trimethoprim (p < 0.001), and tetracyclines (p = 0.0245). The proportion of strains resistant to chloramphenicol was not significantly higher in MRSP than in MSSP (p = 0.4732), and it was identical for rifampicin.
Resistance to ceftaroline was observed in profiles D, L, and M, which were resistant to 10, 9, and 11 antibacterials, respectively. (Table 3).

Table 3.
Resistance profiles with World Health Organization (WHO, AWaRe) and European Medicine Agency (AMEG) classifications. For each antibacterial and MDR, the prevalence of resistant profiles is reported.
Only 3 out of 19 AMR profiles (15.8%) were not multi-drug resistant (B, I, and P). Overall, the prevalence of MDR strains was 75.0% (CI: 61.3–85.8%). A total of 60.0% of the strains (CI: 45.8–73.1%) were multi-resistant to CIA (i.e., resistant to 3 or more classes of CIA), whereas only 20.0% (CI: 10.4–33.2%) of strains were multi-resistant to antibacterials in Watch and/or Reserve categories. The prevalence of strains resistant to three or more classes of cat. A, B or C combined was 70.0% (CI: 56.0–81.7%). No extensively drug-resistant (XDR) nor pan-drug resistant (PDR) strains were observed. The overall multiple antimicrobial resistance (MAR) index was 0.34, but it ranged from 0.18 in MSSP to 0.49 in MRSP strains.
3. Discussion
This study assessed the resistance of forty zoo-pathogenic S. pseudintermedius strains against a broad spectrum of antimicrobials of many different classes, including some exclusive to human medicine. The explorative aim of the study was more of epidemiologic than of clinical relevance. In fact, the applicability of the results to veterinary clinics is limited by the lack of several clinical breakpoints for S. pseudintermedius. However, for epidemiological purposes, it is important to monitor the resistance to human-specific antibacterials, in particular for bacterial species with zoonotic potential, such as S. pseudintermedius.
During a one-year period, all cases matching the inclusion criteria that occurred at the veterinary teaching hospital of the University of Torino were enrolled. From 36 animals, 40 S. pseudintermedius strains were isolated. The 36 cases came from different locations of the province of Torino in the north-west of Italy, thus representing the geographic area where the study was conducted. The sample size was satisfactory for a preliminary assessment in terms of prevalence of resistant strains, even if having collected cases over a longer period would have helped the generalizability of the results. The proportion of feline patients confirmed the low prevalence observed in cats [19] and the higher occurrence of S. pseudintermedius infection in dogs [20].
All strains were susceptible to seven antibacterials, although some were resistant to other antibacterials of the same classes. Noticeably, all strains were susceptible to fusidic acid, conversely more than what was reported elsewhere [10]. The prevalence of resistant strains is similar to a previous report in Italy [11] but higher than reported in other geographical areas [4,10,19,20,21]. Most strains were resistant to penicillin and up to 60% were resistant to oxacillin, a percentage higher than recently reported in dogs [10,20,21] and cats [19,20]. In staphylococci, methicillin-resistance is noticeable not only because it involves the resistance to many beta-lactams and cephalosporins but also because it is related to increased resistance towards other antibacterials [21]. Our results confirm these findings, since MRSP strains were more resistant to most of the tested antibacterials, apart from rifampicin and chloramphenicol. Moreover, on average, they were resistant to more antibacterials compared to MSSP. In addition, this was supported by AMR profiles and their frequency.
One third of the MRSP were resistant to ceftaroline as well, based on human-specific clinical breakpoints. This is of particular concern because 5th generation cephalosporins, especially ceftaroline, are currently regarded as the antibacterials of choice against difficult-to-treat multidrug-resistant Gram-positive organisms, such as methicillin-resistant staphylococci [22].
The strains resistant to aminoglycosides, macrolides and lincosamides, quinolones, sulfamethoxazole-trimethoprim, and tetracyclines were over 50%, again, percentages higher than recently reported in recent studies [19,20,21] but in line with others [10,11]. Accordingly, the 60%prevalence of multi-drug resistant strains was higher as well. We observed resistance to no more than 11 antibacterials per strain, thus no extensively drug resistant nor pan-drug resistant strains were detected. An overall MAR index of 0.34 indicated a moderate degree of multi-drug resistance. This was even higher in MRSP, which were resistant to nine antibacterials, on average. Analyzing the AMR profiles, it was possible to identify the most recurrent pattern of resistance. For example, the resistance to chloramphenicol, although having a low prevalence, was recorded only in MDR strains, in association with beta-lactams and macrolides resistance. As expected, resistance to ceftaroline was compounded by the fact that it is found in multi-resistant strains.
The AMR profile analysis, as well testing for a broad spectrum of antibacterials, allowed us to observe that the resistance was higher to antibacterials available in veterinary medicine, suggesting that the major determinant of AMR is the selective pressure exerted by the treatment [23]. Indeed, this finding does not rule out the hypothesis that sharing the same environment with humans leads to the selection of strains resistant to human-specific antibacterials. In fact, antimicrobial resistance in companion animals is known to be acquired not only through treatment but also via transmission back and forth with their owners, which occurs on a regular basis when sharing the same environment [13,14,24]. Moreover, the same antimicrobial classes are used in human medicine, too.
It was of particular interest to examine the results by antimicrobial categorization. The focus was on the EMA categories for veterinary antibacterials and the WHO categories for human antibacterials. Such categorizations have been useful in differentiating substances according to their relevance and in suggesting a reasonable cascade for prescribing [15]. In addition, AMEG classification contemplates the tendency of certain antibacterials to select strains resistant to other categories as a criterion of choice for the treatment. However, the AWaRe categorization appeared to best represent the observed resistance. In fact, the highest resistance was observed for Access substances, which are the most widespread and least relevant, while the lowest resistance was against the Reserve substances, which should be avoided except as a last resort.
Broadening the panel of tested substances has a rebound on the prevalence of MDR strains, in fact it increases the chance of finding them. Therefore, we additionally evaluated the prevalence of strains multi-resistant to “critical” antibacterials, which depended on the categorization. It ranged from 20% for Watch + Reserve categories up to 70% versus cat. A, B or C combined. Additionally, it is notable that there were very different levels of resistance versus cat. D antibacterials. In fact, all but one strains were resistant to benzylpenicillin, while all strains were susceptible to fusidic acid, which has recently made a comeback for the treatment of skin infections [25]. Eventually, even if the resistance to cat. A antibacterials was low, more than half the strains were at the same time resistant to most antibacterials in cat. D, C, and B.
4. Materials and Methods
4.1. Sampling
We hypothesized that S. pseudintermedius isolates from clinical specimens of dogs and cats harbored resistance to antibiotics that are exclusive to human medicine. To confirm this hypothesis, cases admitted to the Veterinary Teaching Hospital (VTH) of the Department of Veterinary Science of the University of Turin (Italy) from July 2019 to May 2020 were collected. Eligibility criteria for case enrolment were the admission to the VTH for bacteriological infection and the isolation of S. pseudintermedius alone or as the primary pathogen. After the isolation of S. pseudintermedius, the previous clinical history of the subjects was checked to exclude all patients that received antibacterial treatment in the previous 90 days.
Forty S. pseudintermedius strains were isolated from 36 animals of which 31 were dogs (86.1%) and 5 were cats (13.8%). In descending order of frequency, the reasons for admission were orthopedic surgeries, skin infections or wounds, ear infections or surgeries, urinary tract infections, and reproductive system infections (Table 4).

Table 4.
Reason for admission at the Veterinary Teaching Hospital of the dogs and cats from whom S. pseudintermedius strains were isolated. Data are reported in decreasing order of frequency.
Overall, seven strains with diverse resistance profiles came from three different dogs. In July 2019, a dog was diagnosed with chronic pyoderma and a S. pseudintermedius strain was isolated: based on AST results, a fusidic acid ointment was administered locally for a month. At a second sampling, in March 2020, another strain of S. pseudintermedius, still susceptible to fusidic acid but with a different resistance profile, was isolated.
Two S. pseudintermedius strains were derived from a crossbred dog with external otitis. The first was isolated in November 2019 during an ear canal ablation surgery. It was treated with amoxicillin-clavulanate. Four months later, in April 2020, the second was obtained from a surgical revision due to the presence of an abscess. The two isolates were considered different from each other based on the AST.
On the 17 September 2019, a crossbred dog was admitted to the VTH for right femur fracture. During the orthopedic surgery for a hip replacement, the first strain of S. pseudintermedius was isolated. In January 2020, the dog was hospitalized for surgical site infection, and two different strains of S. pseudintermedius were isolated from a screw of the surgical implant and a swab. The strains showed different resistance profiles.
4.2. S. pseudintermedius Identification
The sampling procedure depended on the source of infection and was performed by the clinician during the examination. Samples were stored at 4 ± 2 °C and inoculated within 24 h from collection. Staphylococcus spp. strains were isolated by culture on Columbia colistin and nalicanic acid (CNA) blood agar (Oxoid, Basingstoke, UK) and identified to the species level by MALDI-TOF mass spectrometry. The samples were prepared for mass spectrometry following the guidelines of the manufacturer for extended Direct Transfer (eDT) procedure, e.g., transferring on single colony direct on steel plate using a toothpick, applying 1 μL of formic acid and allowing it to dry, then covering with α-cyano-4-hydroxycinnamic acid (HCCA) matrix and allowing it to dry completely. Due to the known difficulties in Staphylococcus intermedius group (SIG) species discrimination, MALDI scores above 1.60 were considered satisfactory if the first three or more species suggested by the algorithm were S. pseudintermedius. Eventually, the identification of all strains was confirmed by PCR for the S. pseudintermedius species-specific nuc gene [26].
4.3. Antimicrobial Susceptibility Testing
For this study, antibacterials were selected to represent as many classes as possible, starting from the list proposed by Magiorakos et al. for evaluating multi-drug resistance [27]. Among different antibacterials of the same class, the choice was made based on the availability of clinical breakpoints. Eventually, 20 antibacterials were tested (Table 5), namely 11 CIA (ceftaroline, ciprofloxacin, daptomycin, erythromycin, fosfomycin, gentamycin, linezolid, rifampicin, teicoplanin/vancomycin, telavancin, tigecycline) and 8 HIA (chloramphenicol, clindamycin, fusidic acid, oxacillin, penicillin G, quinuprstin-dalfopristin, tetracycline, trimethoprim-sulfamethoxazole), indicative of 18 different antimicrobial classes; 6 of them (ceftaroline, daptomycin, linezolid, quinupristin-dalfopristin, teicoplanina/vancomycin, telavancin) were tested by measuring minimum inhibitory concentration (MIC) with MIC-test strips (Liofilchem Inc., Waltham MA, USA) and the others (chloramphenicol, ciprofloxacin, clindamycin, enrofloxacin, erythromycin, fosfomycin, fusidic acid, gentamycin, oxacillin, penicillin, rifampicin, sulfamethoxazole-trimethoprim, tetracycline, tigecycline) by the agar disk diffusion (ADD) method. To interpret the MIC and inhibition halos diameters, clinical breakpoints of the European Committee of Antimicrobial Susceptibility Testing (EUCAST, 2019) [28] were used except for enrofloxacin for which we referred to the Clinical Laboratory Standard Institute for veterinary medicine (CLSI Vet, 2018) [29] and for fosfomycin, which was evaluated based on the breakpoints provided by the Comité de l’Antibiogramme de la Société Française de Microbiologie (CASFM, 2013) [30]. Following t’e manufacturer's instructions, MIC values, which fell between two-fold dilutions were rounded up to the next standard upper value. Some of the antibacterials are considered markers of resistance for other classes, such as oxacillin for cephalosporins from 1st to 4th generation and carbapenems, thus increasing the number of classes evaluated.

Table 5.
List of the 20 tested antibacterials and their classes/groups. The table reports the disk content (for ADD), the clinical breakpoint standards used for interpretation, and WHO, AWaRe and EMA AMEG classifications for each antibacterial.
4.4. Statistical Analysis
Based on the results of AST, a multi-drug resistant (MDR) strain was defined as being resistant to at least one antibacterial in more than three antibacterial classes. Extensively drug-resistant (XDR) was defined as nonsusceptibility to at least one agent in all but two or fewer antibacterial classes. Strains resistant to at least one antimicrobial in all antimicrobial classes were defined as pan-drug resistant (PDR) [27]. Based on the most recent definition of susceptibility categories (S, I, and R) provided by EUCAST [31], S and I were both considered susceptible and lumped together to estimate the prevalence of resistant strains. The prevalence proportion was calculated as the number of isolates not susceptible to the antibacterial over the total number of isolates. After the evaluation of Wald’s, Wilson’s, and Clopper-Pearson’s confidence interval [32], the latter was chosen for being the most conservative.
The comparison between MRSP and MSSP strains was performed using Fisher’s test for contingency tables and Wilcoxon rank-sum test. The prevalence of resistant strains was compared among categories for each antibacterial categorization (WHO, AMEG, and AWaRe), using Fisher’s exact test for contingency tables and the Kruskal–Wallis test. For comparisons between two categories, we used a pairwise Wilcoxon rank-sum test with Bonferroni correction for multiple tests.
To evaluate the number of antibacterials to which strains were resistant, the Multiple Antimicrobial Resistance (MAR) index was calculated, as described by Krumperman [33]. To avoid the risk of MAR underestimation, only one antibacterial of the same class was included.
The selection process of some estimates to be presented in the abstract adds additional uncertainty, which confidence intervals do not account for. Therefore, we corrected the intervals accordingly [34].
5. Conclusions
Our findings confirm that the resistance of S. pseudintermedius strains was higher towards antibacterials commonly used in veterinary medicine than to human-exclusive substances. Nonetheless, some resistance to these last is present. Since S. pseudintermedius is a major cause of disease in companion animals and is increasingly reported in human patients as well, we would encourage the monitoring of its evolution, and the introduction of new categories of multi-drug resistant strains devoted to critically important antibacterials.
Based on the results of this study, there is no evidence that it is necessary to broaden the spectrum of antibacterials to be tested routinely. Nonetheless, it is essential to carefully consider many factors when choosing the appropriate treatment, not only the susceptibility of the strain. To this end, the classifications of antibacterials provide proper guidance, although the emergence of multi-resistant strains is making some of them obsolete. Regardless of a treatment being administered to an animal or a human being, it is necessary to reiterate the extreme importance of prudent antibiotic use since we all operate in a one-health context.
Author Contributions
Conceptualization, P.N., P.R. and A.B.; methodology, P.N., M.C.S. and D.S.; analysis, L.S., M.C.S., A.B. and D.S.; investigation, A.B.; software, A.B.; writing—original draft preparation, A.B.; writing—review and editing, A.B., P.N. and P.R.; funding acquisition, P.N. All authors have read and agreed to the published version of the manuscript.
Funding
This work was financially supported by Ministero dell’Istruzione, dell’Università e della Ricerca (MIUR) under the programme “Dipartimenti di Eccellenza ex L.232/2016”.
Institutional Review Board Statement
Ethical review and approval were waived for this study because investigations were performed in samples collected for clinical purposes in the benefit of the patient. The study does not fall within the application areas of Italian Legislative Decree 26/2014, which governs the protection of animals used for scientific or educational purposes. Furthermore, ethics approval was not required for this study, as defined by the Ethical Committee of the Department of Veterinary Science of Turin, Italy. A written consent form was signed by the owners of dogs and cats before enrolment in the study. They gave permission for the use of diagnostic results for research purposes.
Informed Consent Statement
All informed consent is stored in the physical archive of the Department of Veterinary Science of the University of Torino (L.go Paolo Braccini 2, Grugliasco, Italy).
Data Availability Statement
Not applicable.
Acknowledgments
This study was supported by Ministero dell’Istruzione, dell’Università e della Ricerca (MIUR) under the programme “Dipartimenti di Eccellenza ex L.232/2016” to the Department of Veterinary Science, University of Turin.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Devriese, L.A.; Vancanneyt, M.; Baele, M.; Vaneechoutte, M.; De Graef, E.; Snauwaert, C.; Cleenwerck, I.; Dawyndt, P.; Swings, J.; Decostere, A.; et al. Staphylococcus pseudintermedius sp. nov., a coagulase-positive species from animals. Int. J. Syst. Evol. Microbiol. 2005, 55, 1569–1573. [Google Scholar] [CrossRef] [PubMed]
- PubMed. Staphylococcus pseudintermedius—Search Results. Available online: https://pubmed.ncbi.nlm.nih.gov/?term=Staphylococcus+pseudintermedius&sort=date (accessed on 21 October 2022).
- Bannoehr, J.; Guardabassi, L. Staphylococcus pseudintermedius in the dog: Taxonomy, diagnostics, ecology, epidemiology and pathogenicity. Vet. Dermatol. 2012, 23, 253–266. [Google Scholar] [CrossRef] [PubMed]
- Bierowiec, K.; Korzeniowska-Kowal, A.; Wzorek, A.; Rypuła, K.; Gamian, A. Prevalence of Staphylococcus Species Colonization in Healthy and Sick Cats. BioMed Res. Int. 2019, 2019, e4360525. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, A.M.; Worthing, K.A.; Kulkarni, N.; Li, F.; Nakatsuji, T.; McGrosso, D.; Mills, R.H.; Kalla, G.; Cheng, J.Y.; Norris, J.M.; et al. Antimicrobials from a feline commensal bacterium inhibit skin infection by drug-resistant S. pseudintermedius. eLife 2021, 10, e66793. [Google Scholar] [CrossRef] [PubMed]
- Carroll, K.C.; Burnham, C.-A.D.; Westblade, L.F. From canines to humans: Clinical importance of Staphylococcus pseudintermedius. PLoS Pathog. 2021, 17, e1009961. [Google Scholar] [CrossRef]
- Guardabassi, L.; Larsen, J.; Weese, J.S.; Butaye, P.; Battisti, A.; Kluytmans, J.; Lloyd, D.H.; Skov, R.L. Public health impact and antimicrobial selection of meticillin-resistant staphylococci in animals. J. Glob. Antimicrob. Resist. 2013, 1, 55–62. [Google Scholar] [CrossRef]
- Laarhoven, L.M.; de Heus, P.; van Luijn, J.; Duim, B.; Wagenaar, J.A.; van Duijkeren, E. Longitudinal study on methicillin-resistant Staphylococcus pseudintermedius in households. PLoS ONE 2011, 6, e27788. [Google Scholar] [CrossRef]
- Yarbrough, M.L.; Lainhart, W.; Burnham, C.-A.D. Epidemiology, Clinical Characteristics, and Antimicrobial Susceptibility Profiles of Human Clinical Isolates of Staphylococcus intermedius Group. J. Clin. Microbiol. 2018, 56, e01788-17. [Google Scholar] [CrossRef]
- Hritcu, O.M.; Schmidt, V.M.; Salem, S.E.; Maciuca, I.E.; Moraru, R.F.; Lipovan, I.; Mareş, M.; Solcan, G.; Timofte, D. Geographical Variations in Virulence Factors and Antimicrobial Resistance Amongst Staphylococci Isolated from Dogs from the United Kingdom and Romania. Front. Vet. Sci. 2020, 7, 414. [Google Scholar] [CrossRef]
- Meroni, G.; Soares Filipe, J.F.; Drago, L.; Martino, P.A. Investigation on Antibiotic-Resistance, Biofilm Formation and Virulence Factors in Multi Drug Resistant and Non Multi Drug Resistant Staphylococcus pseudintermedius. Microorganisms 2019, 7, 702. [Google Scholar] [CrossRef]
- Żarnowska, S.; Piechowicz, L.; Haras, K.; Garbacz, K.; Dąbrowska-Szponar, M. Heterogeneity of methicillin-sensitive Staphylococcus pseudintermedius strains isolated from diseased dogs. Pol. J. Vet. Sci. 2011, 14, 283–284. [Google Scholar]
- Frosini, S.M.; Bond, R.; McCarthy, A.J.; Feudi, C.; Schwarz, S.; Lindsay, J.A.; Loeffler, A. Genes on the Move: In Vitro Transduction of Antimicrobial Resistance Genes between Human and Canine Staphylococcal Pathogens. Microorganisms 2020, 8, 2031. [Google Scholar] [CrossRef]
- Paul, N.C.; Moodley, A.; Ghibaudo, G.; Guardabassi, L. Carriage of methicillin-resistant Staphylococcus pseudintermedius in small animal veterinarians: Indirect evidence of zoonotic transmission. Zoonoses Public Health 2011, 58, 533–539. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Categorisation of Antibiotics in the European Union Answer to the Request from the European Commission for Updating the Scientific Advice on the Impact on Public Health and Animal Health of the Use of Antibiotics in Animals; EMA: Amsterdam, The Netherlands, 2017. [Google Scholar]
- Collignon, P.C.; Conly, J.M.; Andremont, A.; McEwen, S.A.; Aidara-Kane, A.; World Health Organization Advisory Group, Bogotá Meeting on Integrated Surveillance of Antimicrobial Resistance (WHO-AGISAR); Agerso, Y.; Andremont, A.; Collignon, P.C.; Conly, J.; et al. World Health Organization Ranking of Antimicrobials According to Their Importance in Human Medicine: A Critical Step for Developing Risk Management Strategies to Control Antimicrobial Resistance from Food Animal Production. Clin. Infect. Dis. 2016, 63, 1087–1093. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Critically Important Antimicrobials for Human Medicine, 6th ed.; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO. Access, Watch, Reserve (AWaRe) Classification of Antibiotics for Evaluation and Monitoring of Use, 2021; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Bierowiec, K.; Miszczak, M.; Korzeniowska-Kowal, A.; Wzorek, A.; Płókarz, D.; Gamian, A. Epidemiology of Staphylococcus pseudintermedius in cats in Poland. Sci. Rep. 2021, 11, 18898. [Google Scholar] [CrossRef]
- Feßler, A.T.; Scholtzek, A.D.; Schug, A.R.; Kohn, B.; Weingart, C.; Schink, A.-K.; Bethe, A.; Lübke-Becker, A.; Schwarz, S. Antimicrobial and Biocide Resistance among Feline and Canine Staphylococcus aureus and Staphylococcus pseudintermedius Isolates from Diagnostic Submissions. Antibiotics 2022, 11, 127. [Google Scholar] [CrossRef]
- Lai, C.-H.; Ma, Y.-C.; Shia, W.-Y.; Hsieh, Y.-L.; Wang, C.-M. Risk Factors for Antimicrobial Resistance of Staphylococcus Species Isolated from Dogs with Superficial Pyoderma and Their Owners. Vet. Sci. 2022, 9, 306. [Google Scholar] [CrossRef]
- Steed, M.E.; Rybak, M.J. Ceftaroline: A new cephalosporin with activity against resistant gram-positive pathogens. Pharmacotherapy 2010, 30, 375–389. [Google Scholar] [CrossRef]
- Baharoglu, Z.; Garriss, G.; Mazel, D. Multiple Pathways of Genome Plasticity Leading to Development of Antibiotic Resistance. Antibiotics 2013, 2, 288–315. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Reflection Paper on the Risk of Antimicrobial Resistance Transfer from Companion Animals; EMA: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Falagas, M.E.; Grammatikos, A.P.; Michalopoulos, A. Potential of old-generation antibiotics to address current need for new antibiotics. Expert Rev. Anti-Infect. Ther. 2008, 6, 593–600. [Google Scholar] [CrossRef]
- Sasaki, T.; Tsubakishita, S.; Tanaka, Y.; Sakusabe, A.; Ohtsuka, M.; Hirotaki, S.; Kawakami, T.; Fukata, T.; Hiramatsu, K. Multiplex-PCR Method for Species Identification of Coagulase-Positive Staphylococci. J. Clin. Microbiol. 2010, 48, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- The European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint Tables for Interpretation of MICs and Zone Diameters; Version 12.0; EUCAST: Växjö, Sweden, 2022; Available online: https://www.eucast.org/clinical_breakpoints (accessed on 12 May 2022).
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing: Fifteenth Informational Supplement M100-S15; CLSI: Wayne, PA, USA, 2005. [Google Scholar]
- Comité de l’Antibiogramme de la Société Française de Microbiologie (CASFM)—Recommandations 2013. Available online: https://www.sfm-microbiologie.org/wp-content/uploads/2020/07/CASFM_2013.pdf (accessed on 12 May 2022).
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Guidance on the 2019 Modifications of Susceptibility Categories S., I and R Categories; EUCAST: Växjö, Sweden, 2018; Available online: https://www.eucast.org/eucastguidancedocuments (accessed on 12 May 2022).
- Agresti, A.; Coull, B.A. Approximate is Better than “Exact” for Interval Estimation of Binomial Proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar]
- Krumperman, P.H. Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl. Environ. Microbiol. 1983, 46, 165–170. [Google Scholar] [CrossRef]
- Carugno, M.; Consonni, D.; Randi, G.; Catelan, D.; Grisotto, L.; Bertazzi, P.A.; Biggeri, A.; Baccini, M. Air pollution exposure, cause-specific deaths and hospitalizations in a highly polluted Italian region. Environ. Res. 2016, 147, 415–424. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).