Qualitative Analysis of a Twitter-Disseminated Survey Reveals New Patient Perspectives on the Impact of Urinary Tract Infection
Abstract
1. Introduction
2. Results
2.1. Population Demographics, Survey Response Rate, and Twitter Analytics
2.2. UTI Relationship and Type
“This year of my life has been hell. I’ve had a chronic, embedded UTI infection from an acute infection in October 2019. The infection was resistant to trimethoprim and kept recurring. Since March 2020 [presently 1/2021] symptoms became constant, yet my urine cultures no longer showed bacteria. I had severe UTI symptoms, stinging, burning, frequency, urgency, and it has changed my life. I no longer could work. My doctors diagnosed me with interstitial cystitis, but I knew it was a UTI as antibiotics were the only thing to bring me relief. It spread to my kidneys over Christmas, and I had a kidney infection, which was painful. I’m now seeing urologist Dr. X and he did a DNA sequencing test on my urine and found the hidden bacteria and diagnosed me with a chronic, embedded UTI”.(New Zealand, 123568474)
2.3. Thematic Analysis
2.4. Theme 1: Physical Health Impacts
Some participants cited suffering from severe complications of UTI, such as sepsis (n = 3) or hospitalization (n = 11). A participant from Canada reported the following:“[I’ve been] in pain every day [for] 5 years. Some days [are] so bad that I can only cry, and some days it’s more manageable”.(Sweden, 123597744)
“I was diagnosed [with] having a chronic UTI after I failed to recover from an acute UTI infection in June of 2020, which quickly became relapsing kidney infections, hospitalizations, and turning septic”.(Canada, 123557167)
2.5. Theme 2: Mental Health
2.5.1. Recurrent UTIs Cause or Exacerbate Anxiety and Fear for Many
Others were afraid or had anxiety about engaging in activities they used to enjoy should they lead to infection. One participant wrote,“I can hardly ever go away from home, not to speak for a long time. When I go somewhere, I need to find a toilet immediately, so I feel stressed about leaving home”.(Finland, 123563071)
Participants lived in fear of future infections and the possibility they would never see substantial improvement. One respondent shared,“I love sex, but every time I have it, I am full of anxiety (instead of pleasure and joy) because it feels like a gamble. Am I going to get a UTI this time?”(Australia, 124115084)
Survey participants also reported fear of eventual lack of viable treatment options should they acquire antibiotic-resistant bacteria or a chronic UTI that no longer responds to available treatments:“When in periods of little or no pain, I am constantly aware of my bladder and live in terror of another flare”.(Spain, 123563410)
“It makes me afraid of antibiotic-resistant bugs”.(UK, 124016833)
2.5.2. UTIs Are Very Embarrassing to Some, and Misinformation about the Disease Can Lead to Lowered Self-Esteem
“Once a week, I do a hike with a pal. Despite wearing the maximum absorbency pad, I usually have to have a change of clothing when I get home. Once, I leaked on her car seat, which was really humiliating. It makes you feel like an infant”.(UK, 126777479)
“Spreading of misinformation when it comes to UTI “facts”, “hints” and “tips”. This is VERY damaging, especially for young girls experiencing their first UTI, and too often sets them up for a lifetime of embarrassment, shame, and UTI misery”.(Australia, 124113868)
2.5.3. A True Disease and Its Ties to Depression
Patients also felt a sense of hopelessness—one respondent from the UK shared,“Daily tasks are challenging… swimming upstream every day”.(US, 123542211)
In extreme cases, participants reported feeling so depressed due to sequelae caused by UTIs that they had suicidal ideations. A respondent from the UK wrote,“… there is the sense that nothing will ever change, and there is no help”.(UK, 124235774)
“At the age of 23, I feel like my life has ended before its even properly started. Suicide is on my mind most days. Most of the things I enjoyed in life I cannot do. I feel like a shell of the person I used to be”.(UK, 123552632)
2.6. Theme 3: UTIs Severely Limit Many Aspects of Life
2.6.1. UTIs Limit Diet, Exercise, and Productivity and Create a Reliance on Restroom Facilities
Other participants mentioned that UTIs limited their ability to exercise and participate in normal, day-to-day activities:“I’ve changed my lifestyle and eating habits out of fear of another UTI. No alcohol, less sex, can’t go anywhere without a full water bottle, get anxious when not near a bathroom, etc”.(US, 124135087)
“Living with constant UTIs limits my normal activities due to my need to pee so often. Hiking, shopping, fishing, camping, traveling, and visiting friends are challenging when the proximity of a bathroom is vital”.(US, 124124959)
“It has destroyed my career, my ability to work, my fitness, health and mental health, and my ability to earn a high income”.(Australia, 124114670)
2.6.2. Social Relationships, Sexual Health, and Family Life Impacts
For some participants, the effects on their intimate relationships have been more severe, causing them to abstain from sexual intercourse for 10 years out of fear of getting a UTI. Another Australian participant reflected on being controlled by her chronic UTIs because she cannot prevent them, have intimacy with her husband, and engage with her family.“I can hardly go out and socialize with friends and family due to being in constant pain and needing to use the toilet frequently”.(Australia, 123574965)
Some specifically reported on their experience with UTIs and trying to conceive and even maintain a healthy pregnancy:“I feel controlled by my chronic UTIs… I grieve the impact on my sex life. I have even wondered whether it would be kinder to my husband to divorce him so he can have a normal sex life with someone. It’s devastating… It put stress on our relationship, and we’ve had many fights about it over the years… I am less engaged in family life”.(Australia, 124115084)
“The worst part of it all is that the infection caused me to have a late miscarriage”.(UK, 127183812)
2.6.3. UTIs Are the Main Cause of Decreased Quality of Life
“It controls every aspect of your life and stops you from living your life. You end up just existing like a shadow of your former self”.(UK, 123565842)
2.7. Theme 4: Treatment and Management Experience
2.7.1. Antibiotic Duration or Dose Is Not Adequate
“The constant back and forth to doctors, explaining how debilitating UTIs are on my daily life and trying to get more than a 3–5 day antibiotic [course]!! It’s never long enough!!! The UTI cycle just repeats after antibiotics finish”.(UK, 127185976)
2.7.2. UTI Sufferers Perceived They Received Inadequate Care
Another commented on the unwillingness of their doctor to examine emerging research:“Getting the correct antibiotic when you need them. It’s well documented in my records the amount I suffer, yet I have to explain and beg for a prescription”.(UK, 124289918)
“Lack of understanding by doctors and unwilling to look at possible treatment protocols. Doctors refused to look at the research articles I provided and often were offended when I asked questions and sought help”.(Australia, 124126189)
Several participants mentioned that instead of having a UTI diagnosis, patients are diagnosed with interstitial cystitis.“As a patient, your symptoms are often ignored, and since a lot of infections aren’t even picked up by the current urine tests, you are told, “It’s all in your head”. It’s an absolute disgrace how patients are treated and then sentenced to a life in pain when really, they are suffering from chronic infections”.(UK, 123599248)
“I was told I had [interstitial cystitis] because cultures were negative, but it turns out I had an embedded UTI. MicroGen showed a high bacteria load. It is crazy that I spent years of my life misdiagnosed and getting the wrong treatment”.(US, 123576621)
2.7.3. Many Participants Reported Negative Interactions with Clinicians
A respondent from the UK commented that the lack of support and understanding from clinicians was the biggest challenge in managing their illness.“My infection didn’t show on tests, and doctors didn’t believe me. I found this more traumatising than the childhood and domestic violence I’ve been through”.(UK, 123553386)
“The lack of understanding you are given. We are gaslit and undermined, so it turns the illness onto you, and you start questioning your sanity and whether you’re the problem, not the illness. We need more support!”(UK, 123554397)
2.7.4. Barriers to Accessing Chronic UTI Specialists, Treatments, and Diagnostics
“Finding a doctor who will prescribe long-term antibiotics. I will have to travel from Ireland to the UK to get treatment”.(Ireland, 123584210)
“I spent about 7 years being fobbed off by general practitioners and then it took a year from being referred to a specialist to actually have an appointment”.(UK, 124016545)
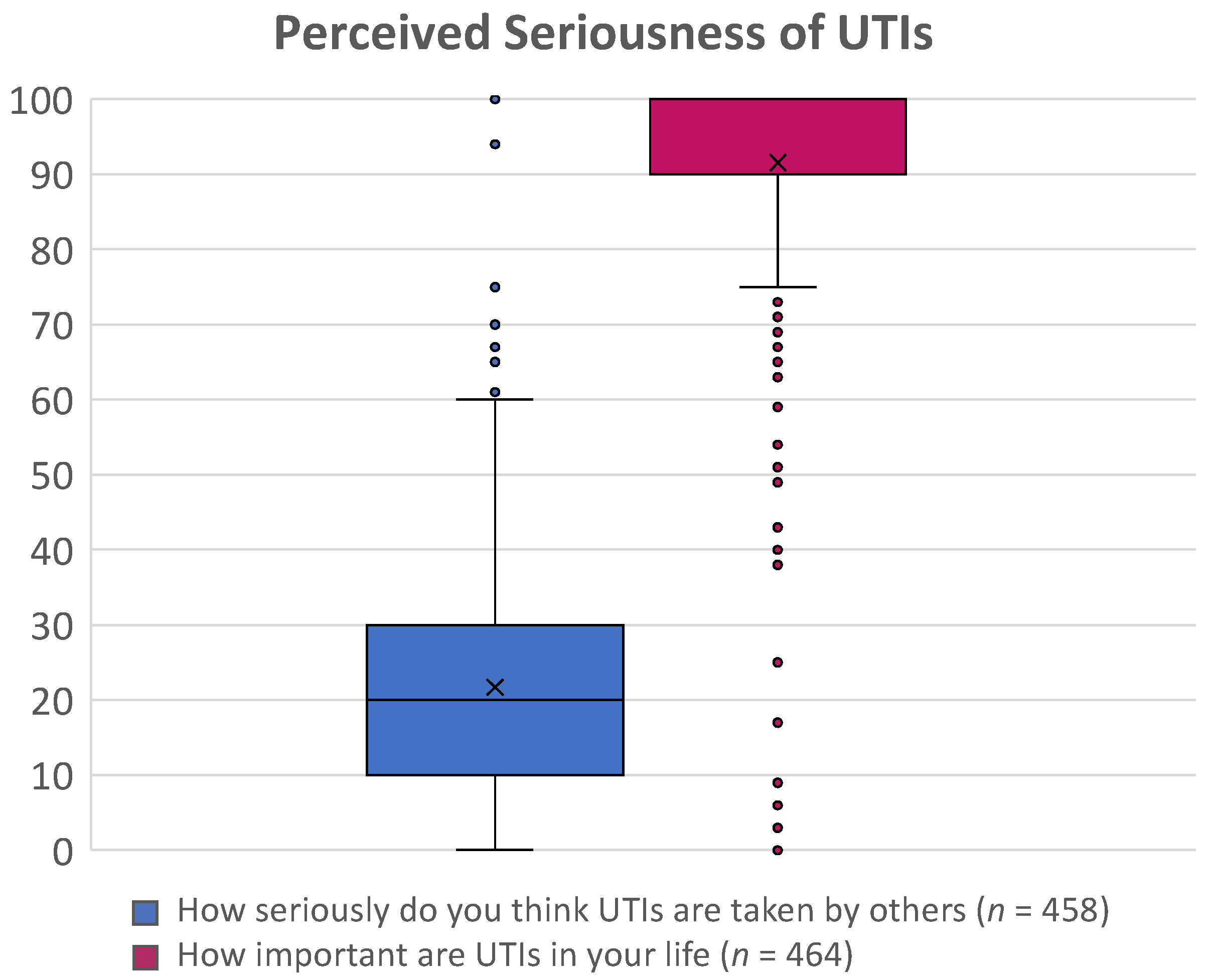
2.8. Theme 5: Limited Knowledge and Awareness of UTI Treatment, Burden, and Relationship with Gender
“I have also been given a lot of contradicting information over the years; this makes me wonder if there is a gap in knowledge or just ignorance to this issue”.(UK, 124121525)
“Doctors seem to have very little understanding of how crippling they can be” (UK, 123606133) and “underestimate the devastation it brings”.(UK, 124156585)
“They also need to acknowledge chronic UTI—that the bacteria can become embedded in the bladder lining, which stops the antibiotics from working until the bladder lining has been shed”.(Australia, 124118726)
“gender bias in healthcare”, where “women are often not listened to or taken seriously by healthcare professionals, and it is quite frankly killing us”.(UK, 12355917795)
“It [a UTI] mostly affects women. Women are not taken seriously, and assumptions are made—pain is in the head, etc. At one point, I was told that “we’d be far more worried if you were a man””.(UK, 12356921739)
2.9. Theme 6: Research Needs
2.9.1. Improvement in Diagnostics for the Detection of UTI Is Imperative
“In [my infectious disease specialist’s] words: urine cultures do not grow everything and can miss infections”.(Canada, 123557167)
“Please, we need a change in the way that urine is tested. The current testing is outdated and extremely unpredictable… The laboratory doesn’t culture it long enough. The Kass index is too high, [as the] bacterial load has to be 10,000 [colony forming units (CFU)/mL] to be classed as a UTI. If you come back with 9,999 [CFU/mL], general practitioners say that it’s not a UTI. It’s absolutely ridiculous”.(UK, 123554985)
“Review the symptoms of the person, in addition to the lab tests. Please find better lab testing and research to support embedded infection. Doctors need to see that the infection can stay in the body, even if the lab tests are clear”.(US, 123578005)
2.9.2. Treatment Guidelines Are Hurdles to Care
“The NHS [National Health Service] in the UK will only do dip[stick] testing. Most of my symptoms occur, but no infection shows on a dip[stick] test, so I’m told I’m fine. It was only when I learned more and found the right help that they found bacteria after growing it in the lab and further in my bladder wall after a biopsy”.(UK, 123552364)
“There is an umbrella approach of treatment with short-term antibiotics, which is simply not the answer for many patients who need a long-term solution (for embedded infections, etc.)”.(UK, 123558492)
2.9.3. Research of Chronic UTI Pathophysiology and Existence Must Be Undertaken
“There must be a consensus (drawn from current available research and perhaps new studies) that chronic UTI is a real condition (e.g., intracellular bacteria), [and] is distinct from acute UTI (e.g., planktonic bacteria), and cannot be treated, or expected to respond to treatment the same as an acute UTI… No one wants to be on antibiotics for months or years. There must be at once an acceptance that long-term antibiotics are the only thing that appears to help this cohort of patients in any measurable and effective way and a call to action to find better treatment alternatives”.(US, 124505833)
2.9.4. Validated and Improved Treatments Are Desperately Needed, Especially for Chronic UTI
“Please, please find a cure for chronic UTI. It is the most miserable condition which needs to be addressed urgently. I am often contemplating suicide as I feel so awful”.(UK, 124124074)
2.9.5. Research on the Impact of UTIs on Quality of Life Needs to Be Explored and Disseminated
“Ensure you report on the impacts that they have on people’s lives. Medically speaking, they are not serious, but they literally ruin people’s ability to go about daily life as seriously as cancer treatment does”.(UK, 124018170)
3. Discussion
Strengths and Limitations
4. Materials and Methods
4.1. Survey Design and Survey Questions
4.2. Qualitative Analyses of Participants’ Responses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zeng, Z.; Zhan, J.; Zhang, K.; Chen, H.; Cheng, S. Global, regional, and national burden of urinary tract infections from 1990 to 2019: An analysis of the global burden of disease study 2019. World J. Urol. 2022, 40, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Foxman, B.; Barlow, R.; D’Arcy, H.; Gillespie, B.; Sobel, J.D. Urinary tract infection: Self-reported incidence and associated costs. Ann. Epidemiol. 2000, 10, 509–515. [Google Scholar] [CrossRef] [PubMed]
- Aronin, S.I.; Gupta, V.; Dunne, M.W.; Watts, J.A.; Yu, K.C. Regional Differences in Antibiotic-resistant Enterobacterales Urine Isolates in the United States: 2018–2020. Int. J. Infect. Dis. 2022, 119, 142–145. [Google Scholar] [CrossRef]
- Antimicrobial Resistance, C. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Goebel Melanie, C.; Trautner Barbara, W.; Grigoryan, L. The Five Ds of Outpatient Antibiotic Stewardship for Urinary Tract Infections. Clin. Microbiol. Rev. 2021, 34, e00003-20. [Google Scholar] [CrossRef]
- Foxman, B. The epidemiology of urinary tract infection. Nat. Rev. Urol. 2010, 7, 653–660. [Google Scholar] [CrossRef]
- Drekonja, D.M.; Rector, T.S.; Cutting, A.; Johnson, J.R. Urinary tract infection in male veterans: Treatment patterns and outcomes. JAMA Intern. Med. 2013, 173, 62–68. [Google Scholar] [CrossRef]
- Foxman, B.; Gillespie, B.; Koopman, J.; Zhang, L.; Palin, K.; Tallman, P.; Marsh, J.V.; Spear, S.; Sobel, J.D.; Marty, M.J.; et al. Risk factors for second urinary tract infection among college women. Am. J. Epidemiol. 2000, 151, 1194–1205. [Google Scholar] [CrossRef]
- Ikaheimo, R.; Siitonen, A.; Heiskanen, T.; Karkkainen, U.; Kuosmanen, P.; Lipponen, P.; Makela, P.H. Recurrence of urinary tract infection in a primary care setting: Analysis of a 1-year follow-up of 179 women. Clin. Infect. Dis. 1996, 22, 91–99. [Google Scholar] [CrossRef]
- Anger, J.; Lee, U.; Ackerman, A.L.; Chou, R.; Chughtai, B.; Clemens, J.Q.; Hickling, D.; Kapoor, A.; Kenton, K.S.; Kaufman, M.R.; et al. Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. J. Urol. 2019, 202, 282–289. [Google Scholar] [CrossRef]
- Ennis, S.S.; Guo, H.; Raman, L.; Tambyah, P.A.; Chen, S.L.; Tiong, H.Y. Premenopausal women with recurrent urinary tract infections have lower quality of life. Int. J. Urol. 2018, 25, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Boeri, L.; Capogrosso, P.; Ventimiglia, E.; Scano, R.; Graziottin, A.; Deho, F.; Montanari, E.; Montorsi, F.; Salonia, A. Six Out of Ten Women with Recurrent Urinary Tract Infections Complain of Distressful Sexual Dysfunction—A Case-Control Study. Sci. Rep. 2017, 7, 44380. [Google Scholar] [CrossRef] [PubMed]
- McKertich, K.; Hanegbi, U. Recurrent UTIs and cystitis symptoms in women. Aust. J. Gen. Pract. 2021, 50, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Kwok, M.; McGeorge, S.; Mayer-Coverdale, J.; Graves, B.; Paterson, D.L.; Harris, P.N.A.; Esler, R.; Dowling, C.; Britton, S.; Roberts, M.J. Guideline of guidelines: Management of recurrent urinary tract infections in women. BJU Int. 2022. [Google Scholar] [CrossRef]
- Scott, V.C.S.; Thum, L.W.; Sadun, T.; Markowitz, M.; Maliski, S.L.; Ackerman, A.L.; Anger, J.T.; Kim, J.H. Fear and Frustration among Women with Recurrent Urinary Tract Infections: Findings from Patient Focus Groups. J. Urol. 2021, 206, 688–695. [Google Scholar] [CrossRef]
- Grigoryan, L.; Mulgirigama, A.; Powell, M.; Schmiemann, G. The emotional impact of urinary tract infections in women: A qualitative analysis. BMC Womens Health 2022, 22, 182. [Google Scholar] [CrossRef]
- Flower, A.; Bishop, F.L.; Lewith, G. How women manage recurrent urinary tract infections: An analysis of postings on a popular web forum. BMC Fam. Pract. 2014, 15, 162. [Google Scholar] [CrossRef]
- Eriksson, I.; Olofsson, B.; Gustafson, Y.; Fagerstrom, L. Older women’s experiences of suffering from urinary tract infections. J. Clin. Nurs. 2014, 23, 1385–1394. [Google Scholar] [CrossRef]
- Sillence, E. Giving and receiving peer advice in an online breast cancer support group. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 480–485. [Google Scholar] [CrossRef]
- Hearn, J.H.; Selvarajah, S.; Kennedy, P.; Taylor, J. Stigma and self-management: An Interpretative Phenomenological Analysis of the impact of chronic recurrent urinary tract infections after spinal cord injury. Spinal Cord Ser. Cases 2018, 4, 12. [Google Scholar] [CrossRef]
- Izett-Kay, M.; Barker, K.L.; McNiven, A.; Toye, F. Experiences of urinary tract infection: A systematic review and meta-ethnography. Neurourol. Urodyn. 2022, 41, 724–739. [Google Scholar] [CrossRef]
- Mulvey, M.A.; Schilling, J.D.; Hultgren, S.J. Establishment of a persistent Escherichia coli reservoir during the acute phase of a bladder infection. Infect. Immun. 2001, 69, 4572–4579. [Google Scholar] [CrossRef] [PubMed]
- Justice, S.S.; Hung, C.; Theriot, J.A.; Fletcher, D.A.; Anderson, G.G.; Footer, M.J.; Hultgren, S.J. Differentiation and developmental pathways of uropathogenic Escherichia coli in urinary tract pathogenesis. Proc. Natl. Acad. Sci. USA 2004, 101, 1333–1338. [Google Scholar] [CrossRef] [PubMed]
- Anderson, G.G.; Palermo, J.J.; Schilling, J.D.; Roth, R.; Heuser, J.; Hultgren, S.J. Intracellular bacterial biofilm-like pods in urinary tract infections. Science 2003, 301, 105–107. [Google Scholar] [CrossRef]
- Hannan, T.J.; Mysorekar, I.U.; Hung, C.S.; Isaacson-Schmid, M.L.; Hultgren, S.J. Early severe inflammatory responses to uropathogenic E. coli predispose to chronic and recurrent urinary tract infection. PLoS Pathog. 2010, 6, e1001042. [Google Scholar] [CrossRef]
- Schilling, J.D.; Lorenz, R.G.; Hultgren, S.J. Effect of trimethoprim-sulfamethoxazole on recurrent bacteriuria and bacterial persistence in mice infected with uropathogenic Escherichia coli. Infect. Immun. 2002, 70, 7042–7049. [Google Scholar] [CrossRef]
- Robino, L.; Scavone, P.; Araujo, L.; Algorta, G.; Zunino, P.; Vignoli, R. Detection of intracellular bacterial communities in a child with Escherichia coli recurrent urinary tract infections. Pathog. Dis. 2013, 68, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Rosen, D.A.; Hooton, T.M.; Stamm, W.E.; Humphrey, P.A.; Hultgren, S.J. Detection of intracellular bacterial communities in human urinary tract infection. PLoS Med. 2007, 4, e329. [Google Scholar] [CrossRef]
- Scott, V.C.; Haake, D.A.; Churchill, B.M.; Justice, S.S.; Kim, J.H. Intracellular Bacterial Communities: A Potential Etiology for Chronic Lower Urinary Tract Symptoms. Urology 2015, 86, 425–431. [Google Scholar] [CrossRef]
- Wojcik, S.; Hughes, A. Sizing up Twitter Users; Pew Research Center: Washington, DC, USA, 2019. [Google Scholar]
- Schmiemann, G.; Kniehl E Fau-Gebhardt, K.; Gebhardt K Fau-Matejczyk, M.M.; Matejczyk Mm Fau-Hummers-Pradier, E.; Hummers-Pradier, E. The diagnosis of urinary tract infection: A systematic review. Dtsch. Ärzteblatt Int. 2010, 107, 361. [Google Scholar]
- Althubaiti, A. Information bias in health research: Definition, pitfalls, and adjustment methods. J. Multidiscip. Healthc. 2016, 9, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Kuper, A.; Lingard, L.; Levinson, W. Critically appraising qualitative research. BMJ 2008, 337, a1035. [Google Scholar] [CrossRef]
- Guion, L. Triangulation: Establishing the Validity of Qualitative Studies; FCS6014; University of Florida Cooperative Extension Service: Gainesville, FL, USA, 2002; pp. 1–3. [Google Scholar]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.R. A General Inductive Approach for Analyzing Qualitative Evaluation Data. Am. J. Eval. 2006, 27, 237–246. [Google Scholar] [CrossRef]


| Gender | Number (%) |
|---|---|
| Female | 200 (96.6) |
| Male | 7 (3.4) |
| Age Range | |
| 18 to 40 | 57 (27.5) |
| 41 to 60 | 80 (38.6) |
| 61 to 80 | 69 (33.3) |
| >80 | 1 (0.5) |
| Race | |
| White | 196 (94.7) |
| Other b | 11 (5.3) |
| Participant Region | |
| United Kingdom/Ireland | 257 (55.2) |
| United States/Canada | 127 (27.3) |
| Oceania c | 52 (11.2) |
| Europe | 25 (5.4) |
| Other d | 5 (1.2) |
| Theme and Subcodes | No. | Theme and Subcodes | No. |
|---|---|---|---|
| Physical health | UTI treatment and management | ||
| General pain | 282 | Antibiotic dose or duration not adequate | 92 |
| Chronic pain | 89 | Perception of inadequate care | 129 |
| Severe pain | 54 | Negative clinician interactions | 162 |
| Genitourinary symptoms | 174 | Accessing care: | |
| Fatigue | 27 | Chronic UTI specialist or treatment | 85 |
| Malaise | 15 | Travel | 12 |
| Mental health | Timeliness | 15 | |
| General mental health | 66 | ||
| Anxiety | 72 | Limited knowledge and awareness of UTI treatment, burden, and relationship with gender | |
| Depression | 50 | ||
| Distress/stress | 32 | Among medical communities | 184 |
| Embarrassment | 11 | UTIs considered trivial | 55 |
| Fear | 41 | Disbelief or knowledge of chronic UTI | 46 |
| Frustration | 45 | Gender gap | 52 |
| Suicidal ideation | 29 | ||
| Limitations | Research gaps | ||
| Quality of life | 128 | Improved diagnostics | 143 |
| Overall functioning | 113 | Treatment guidelines as hurdles to care | 52 |
| Diet | 38 | Prevention | 20 |
| Exercise | 40 | Cure | 48 |
| Sleep | 40 | Quality of Life | 38 |
| Work, school, or economic | 148 | Chronic UTI: | |
| Unpredictability of UTIs | 56 | Pathophysiology | 52 |
| Dependency a | 107 | Treatment | 38 |
| Social health and family life | 191 | Establish as a medical diagnosis | 17 |
| Sexual health and intimacy | 69 | ||
| Family planning b | 16 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valentine-King, M.; Laytner, L.; Hines-Munson, C.; Olmeda, K.; Trautner, B.; Justice, S.; Ching, C.; Grigoryan, L. Qualitative Analysis of a Twitter-Disseminated Survey Reveals New Patient Perspectives on the Impact of Urinary Tract Infection. Antibiotics 2022, 11, 1687. https://doi.org/10.3390/antibiotics11121687
Valentine-King M, Laytner L, Hines-Munson C, Olmeda K, Trautner B, Justice S, Ching C, Grigoryan L. Qualitative Analysis of a Twitter-Disseminated Survey Reveals New Patient Perspectives on the Impact of Urinary Tract Infection. Antibiotics. 2022; 11(12):1687. https://doi.org/10.3390/antibiotics11121687
Chicago/Turabian StyleValentine-King, Marissa, Lindsey Laytner, Casey Hines-Munson, Kiara Olmeda, Barbara Trautner, Sheryl Justice, Christina Ching, and Larissa Grigoryan. 2022. "Qualitative Analysis of a Twitter-Disseminated Survey Reveals New Patient Perspectives on the Impact of Urinary Tract Infection" Antibiotics 11, no. 12: 1687. https://doi.org/10.3390/antibiotics11121687
APA StyleValentine-King, M., Laytner, L., Hines-Munson, C., Olmeda, K., Trautner, B., Justice, S., Ching, C., & Grigoryan, L. (2022). Qualitative Analysis of a Twitter-Disseminated Survey Reveals New Patient Perspectives on the Impact of Urinary Tract Infection. Antibiotics, 11(12), 1687. https://doi.org/10.3390/antibiotics11121687









