Mechanism and Efficacy of Cu2O-Treated Fabric
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
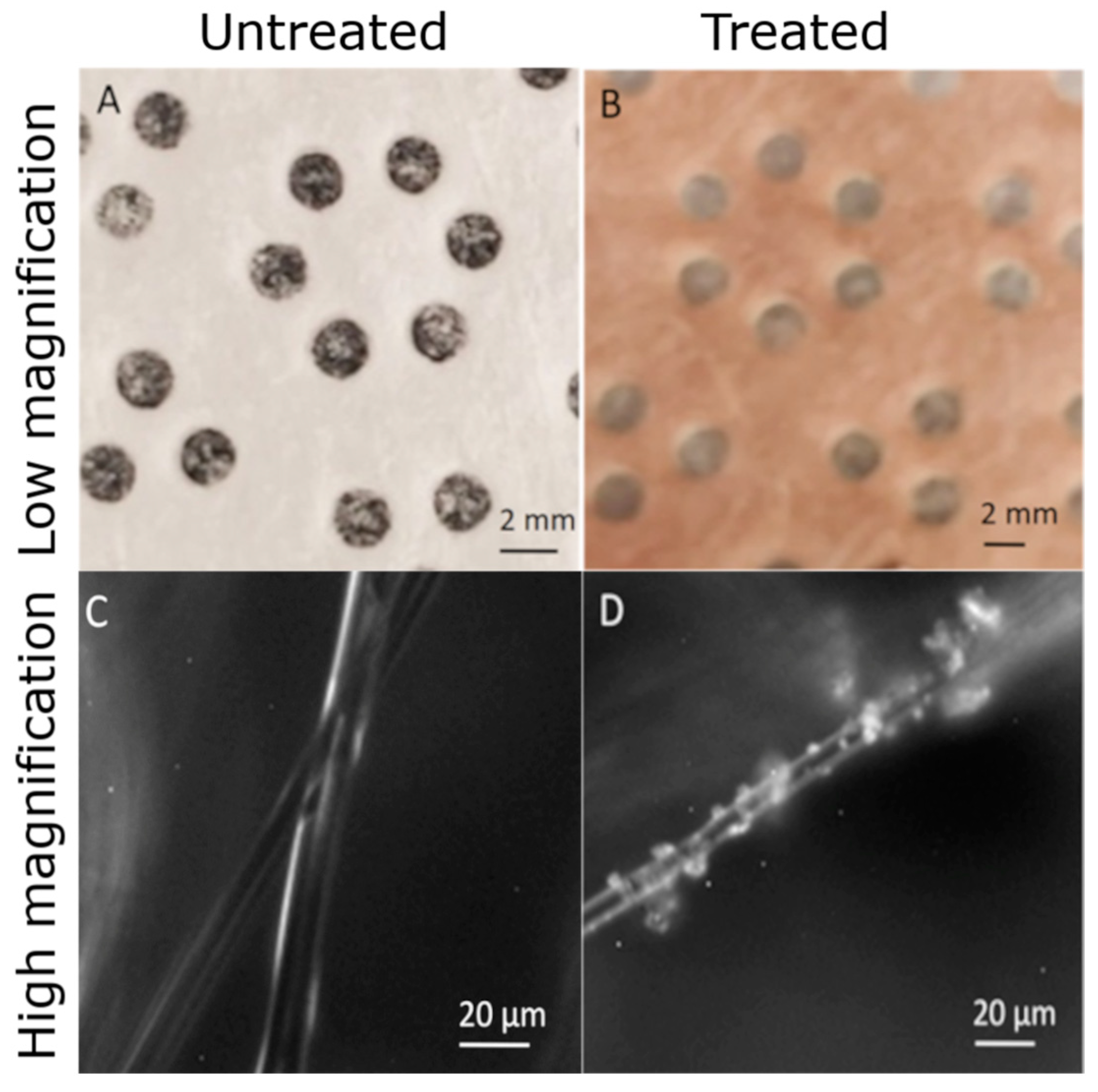
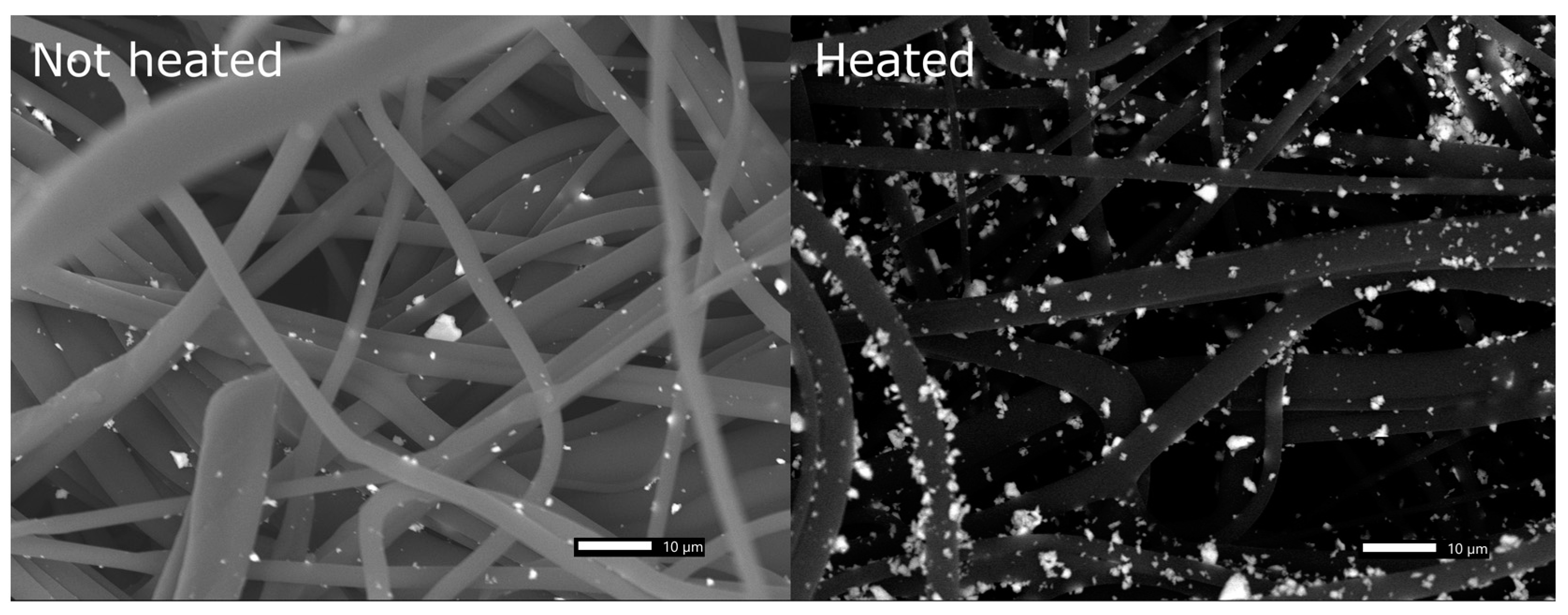
2.2. Treatment of Polypropylene Fabric
2.3. Antibacterial Assay
2.4. Durability of Treated Fabric to Airflow
2.5. Effect of Leached Copper Ions on Bacterial Survival
2.6. Effect of Droplet Evaporation on Antimicrobial Effects
2.7. Statistics
3. Results and Discussion
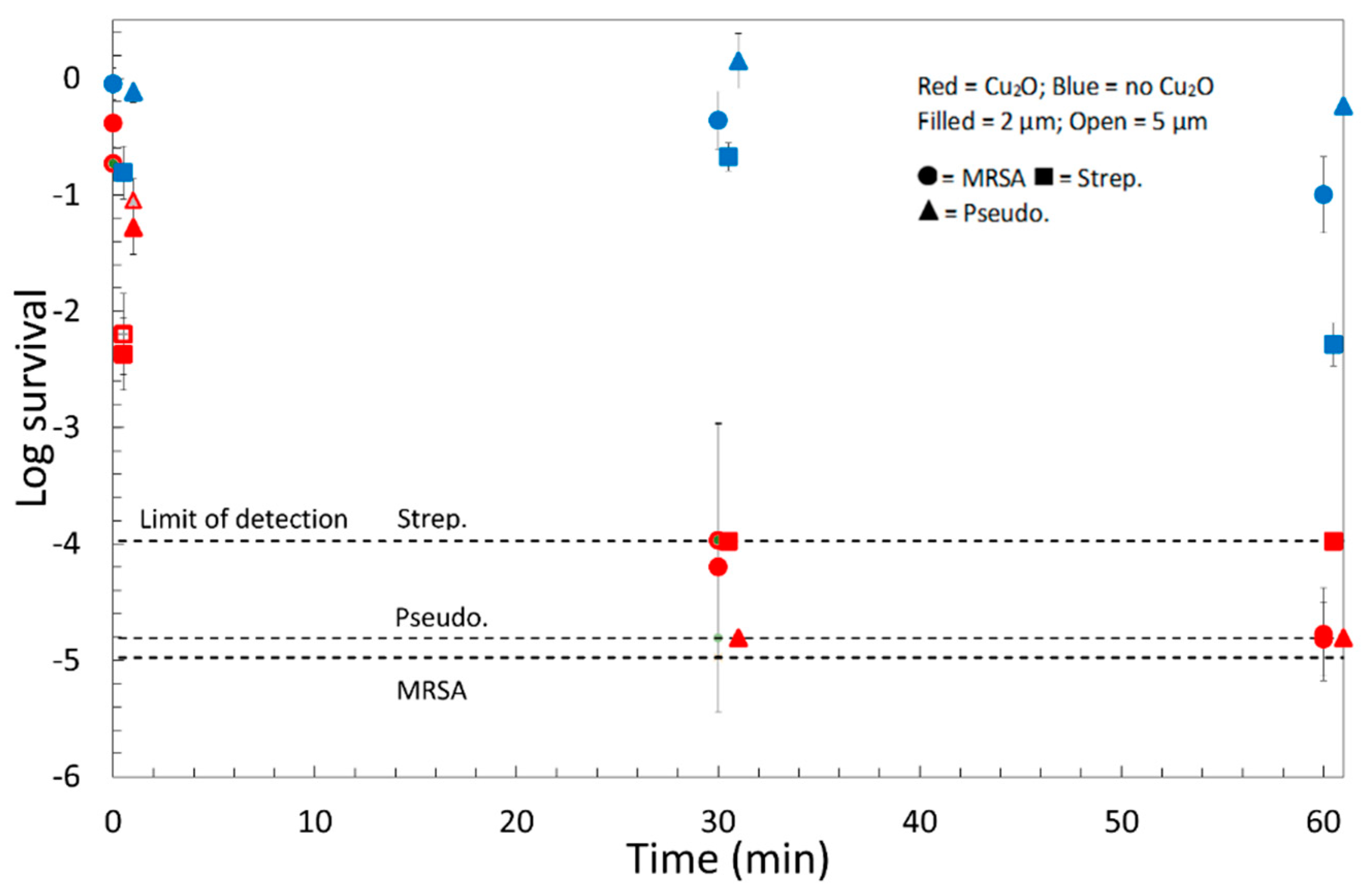
3.1. Treated Polypropylene Fabric Rapidly Kills Bacteria Responsible for HAIs
3.2. Both Drying and the Copper Ion Concentration of the Test Droplet Affect the Survival of Bacteria
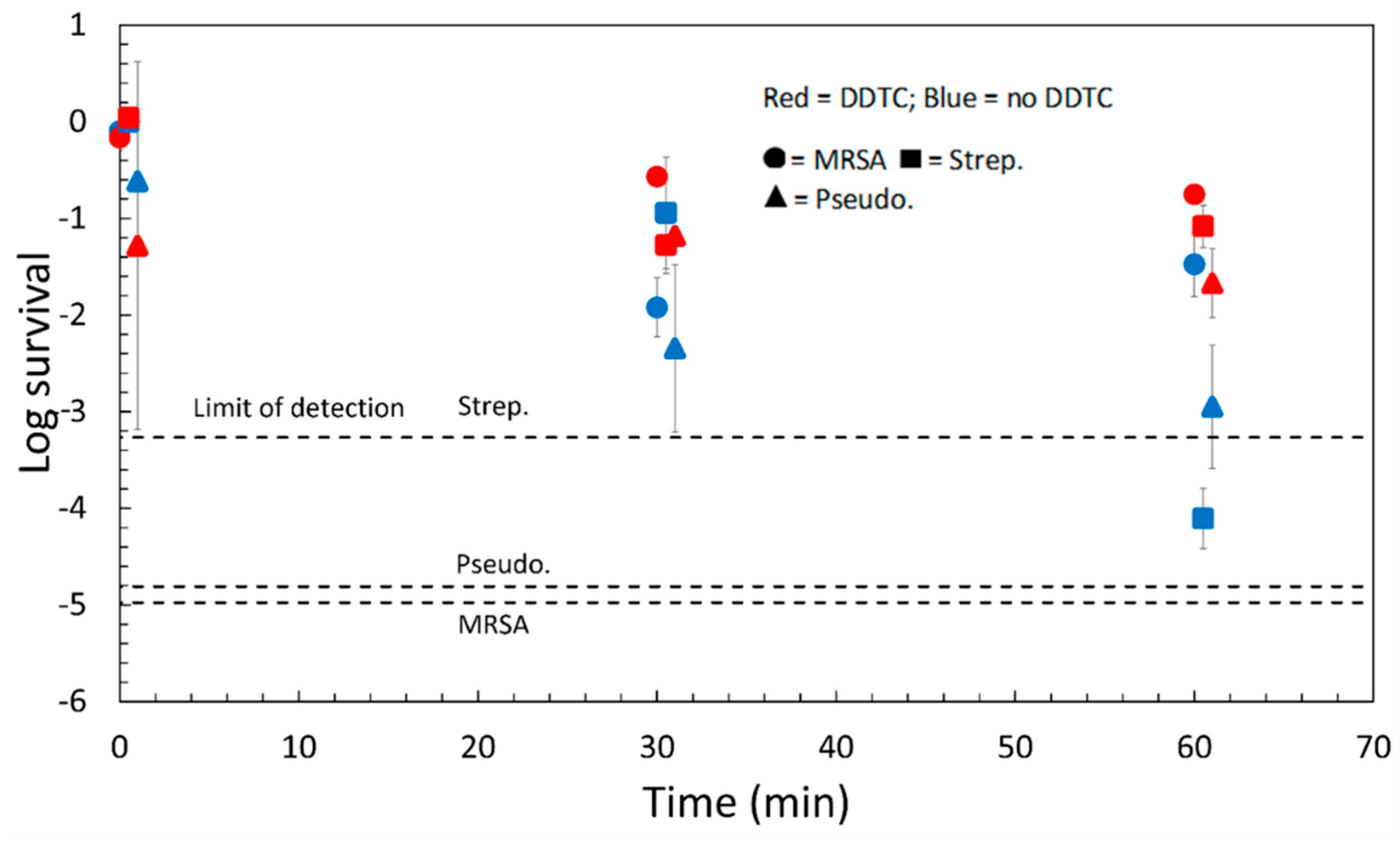
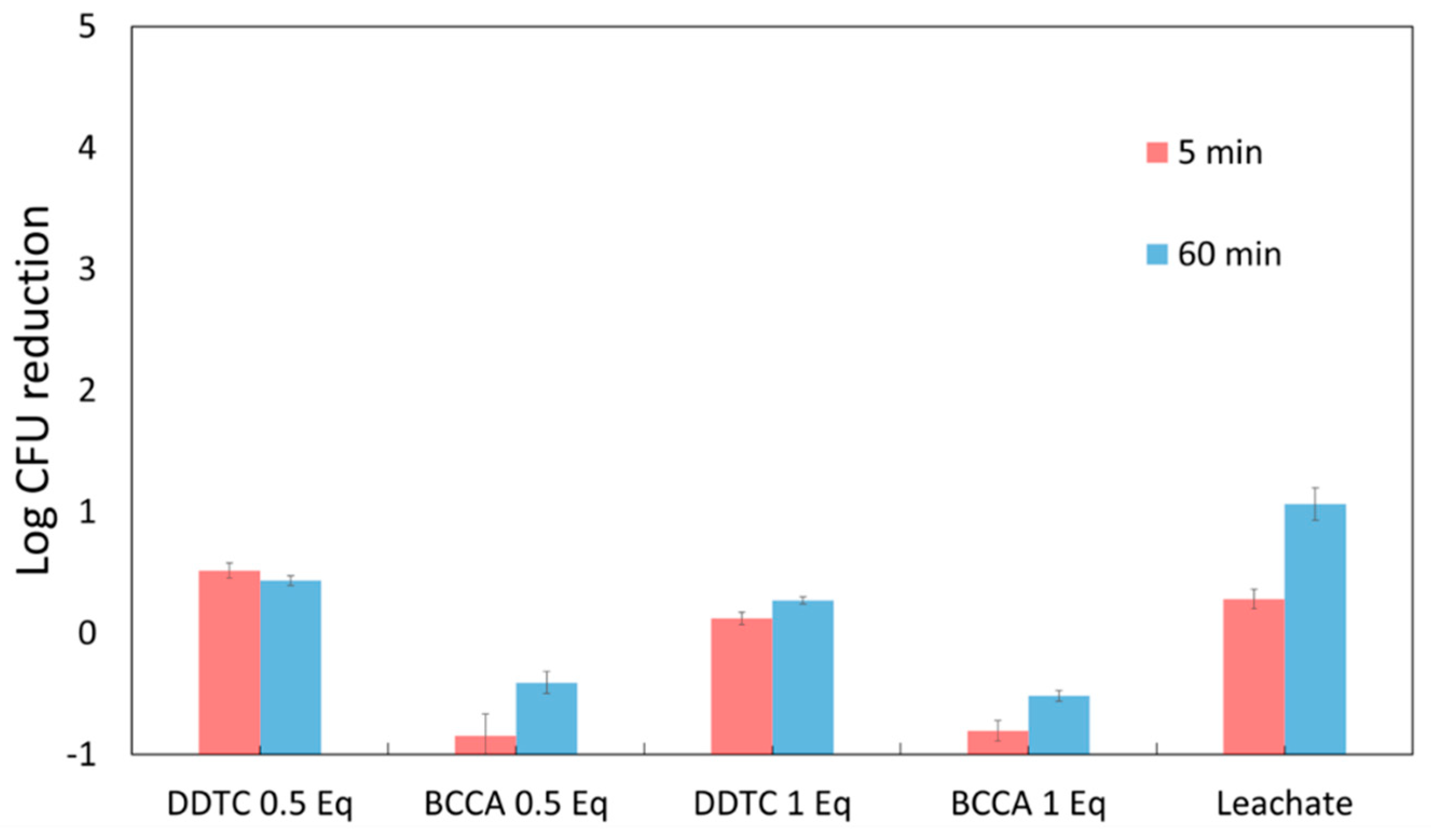
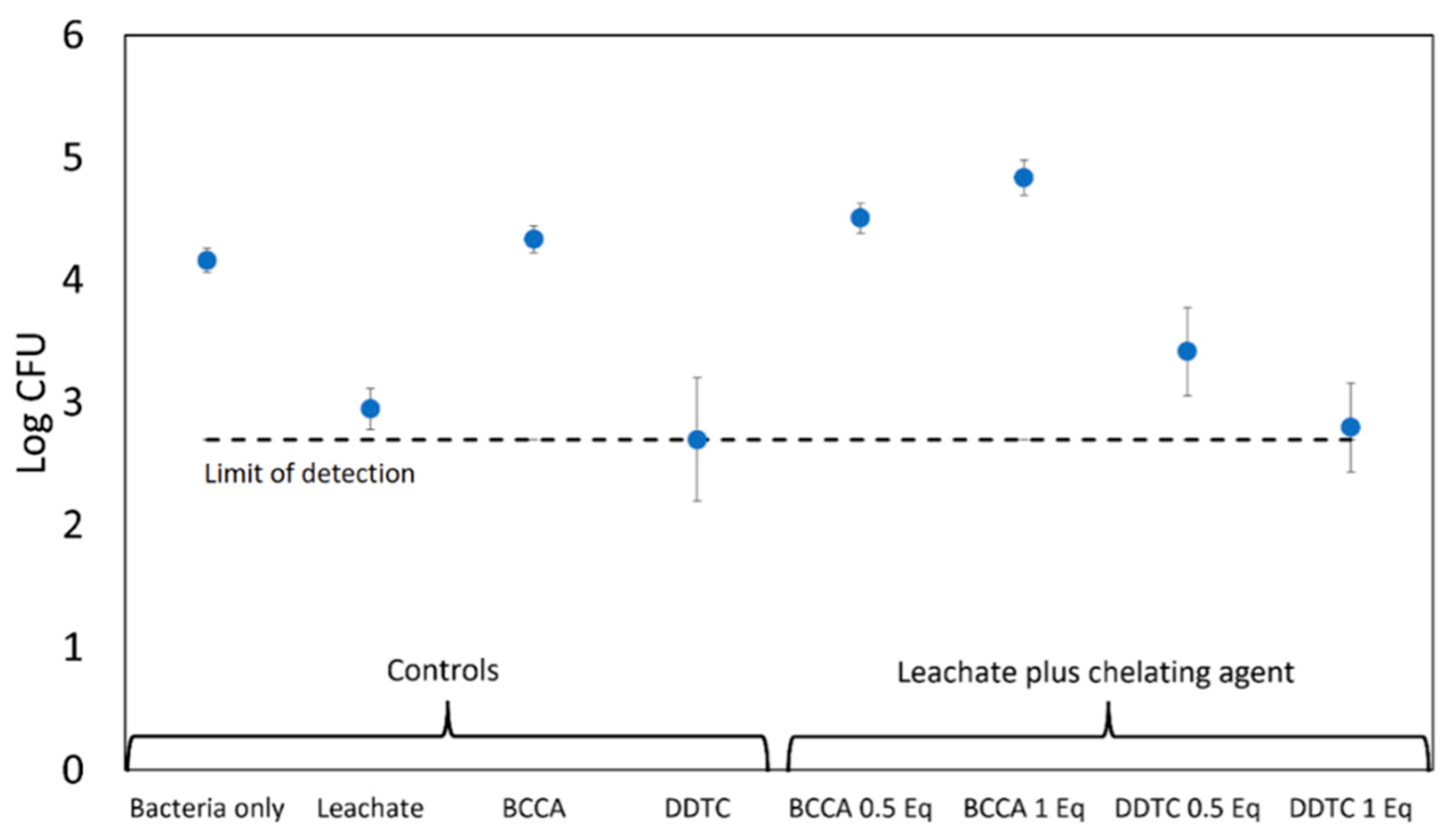
3.3. Chelating Agents “Neutralize” Copper Ions
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Klevens, R.M.; Edwards, J.R.; Richards, C.L.; Horan, T.C.; Gaynes, R.P.; Pollock, D.A.; Cardo, D.M. Estimating Health Care-Associated Infections and Deaths in U.S. Hospitals, 2002. Public Health Rep. 2007, 122, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Gund, M.; Isack, J.; Hannig, M.; Thieme-Ruffing, S.; Gärtner, B.; Boros, G.; Rupf, S. Contamination of surgical mask during aerosol-producing dental treatments. Clin. Oral Investig. 2020, 25, 3173–3180. [Google Scholar] [CrossRef] [PubMed]
- Russotto, V.; Cortegiani, A.; Raineri, S.M.; Giarratano, A. Bacterial contamination of inanimate surfaces and equipment in the intensive care unit. J. Intensive Care 2015, 3, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Ellingson, K.D.; Ellingson, K.D.; Pogreba-Brown, K.; Gerba, C.P.; Elliott, S.P. Impact of a Novel Antimicrobial Surface Coating on Health Care-Associated Infections and Environmental Bioburden at 2 Urban Hospitals. Clin. Infect. Dis. 2020, 71, 1807–1820. [Google Scholar] [CrossRef] [PubMed]
- Karpanen, T.J.; Casey, A.L.; Lambert, P.A.; Cookson, B.D.; Nightingale, P.; Miruszenko, L.; Elliott, T.S.J. The Antimicrobial Efficacy of Copper Alloy Furnishing in the Clinical Environment: A Crossover Study. Infect. Control Hosp. Epidemiol. 2012, 33, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Tamimi, A.H.; Carlino, S.; Gerba, C.P. Long-Term efficacy of a self-disinfecting coating in an intensive care unit. Am. J. Infect. Control 2014, 42, 1178–1181. [Google Scholar] [CrossRef]
- Behzadinasab, S.; Chin, A.; Hosseini, M.; Poon, L.; Ducker, W.A. A Surface Coating that Rapidly Inactivates SARS-CoV-2. ACS Appl. Mater. Interfaces 2020, 12, 34723–34727. [Google Scholar] [CrossRef]
- Gabbay, J.; Borkow, G.; Mishal, J.; Magen, E.; Zatcoff, R.; Shemer-Avni, Y. Copper Oxide Impregnated Textiles with Potent Biocidal Activities. J. Ind. Text. 2006, 35, 323–335. [Google Scholar] [CrossRef]
- Sunada, K.; Minoshima, M.; Hashimoto, K. Highly efficient antiviral and antibacterial activities of solid-state cuprous compounds. J. Hazard. Mater. 2012, 235–236, 265–270. [Google Scholar] [CrossRef]
- Ran, Y.; Liu, Y.; Sun, H.; Zhang, H.; Dong, H.; Yang, Y.; Zhao, N.; Xu, J. Surface modification of cuprous oxide nanoparticles with improved chemical stability and antibacterial activity. Appl. Surf. Sci. 2021, 565, 150566. [Google Scholar] [CrossRef]
- Behzadinasab, S.; Hosseini, M.; Williams, M.D.; Ivester, H.M.; Allen, I.C.; Falkinham, J.O.; Ducker, W.A. Antimicrobial activity of cuprous oxide-coated and cupric oxide-coated surfaces. J. Hosp. Infect. 2022, 129, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Bezza, F.A.; Tichapondwa, S.M.; Chirwa, E.M.N. Fabrication of monodispersed copper oxide nanoparticles with potential application as antimicrobial agents. Sci. Rep. 2020, 10, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Borkow, G. Safety of Using Copper Oxide in Medical Devices and consumer Products. Curr. Chem. Biol. 2012, 6, 86–92. [Google Scholar] [CrossRef]
- Borkow, G.; Salvatori, R.; Kanmukhla, V.K. Drastic Reduction of Bacterial, Fungal and Viral Pathogen Titers by Cuprous Oxide Impregnated Medical Textiles. J. Funct. Biomater. 2021, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- CDC. Antibiotic Resistance Threats in the United States. Available online: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf (accessed on 1 January 2021).
- Thurman, R.B.; Gerba, C.P.; Bitton, G. The molecular mechanisms of copper and silver ion disinfection of bacteria and viruses. Crit. Rev. Environ. Sci. Technol. 1989, 18, 295–315. [Google Scholar] [CrossRef]
- Mathews, S.; Kumar, R.; Solioz, M. Copper reduction and contact killing of bacteria by iron surfaces. Appl. Environ. Microbiol. 2015, 81, 6399–6403. [Google Scholar] [CrossRef]
- Borkow, G.; Gabbay, J. Copper, an ancient remedy returning to fight microbial, fungal and viral infections. Curr. Chem. Biol. 2009, 3, 272–278. [Google Scholar]
- Mathews, S.; Hans, M.; Mücklich, F.; Solioz, M. Contact Killing of Bacteria on Copper Is Suppressed if Bacterial-Metal Contact Is Prevented and Is Induced on Iron by Copper Ions. Appl. Environ. Microbiol. 2013, 79, 2605–2611. [Google Scholar] [CrossRef]
- Galante, A.J.; Haghanifar, S.; Romanowski, E.G.; Shanks, R.M.Q.; Leu, P.W. Superhemophobic and Antivirofouling Coating for Mechanically Durable and Wash-Stable Medical Textiles. ACS Appl. Mater. Interfaces 2020, 12, 22120–22128. [Google Scholar] [CrossRef]
- Pleil, J.D.; Ariel Geer Wallace, M.; Davis, M.D.; Matty, C.M. The physics of human breathing: Flow, timing, volume, and pressure parameters for normal, on-demand, and ventilator respiration. J. Breath Res. 2021, 15, 042002. [Google Scholar] [CrossRef]
- Lin, K.; Marr, L.C. Humidity-Dependent Decay of Viruses, but Not Bacteria, in Aerosols and Droplets Follows Disinfection Kinetics. Environ. Sci. Technol. 2020, 54, 1024–1032. [Google Scholar] [CrossRef]
- Biryukov, J.; Boydston, J.A.; Dunning, R.A.; Yeager, J.J.; Wood, S.; Reese, A.L.; Ferris, A.; Miller, D.; Weaver, W.; Zeitouni, N.E.; et al. Increasing Temperature and Relative Humidity Accelerates Inactivation of SARS-CoV-2 on Surfaces. mSphere 2020, 5, 1–9. [Google Scholar] [CrossRef]
- Toy, A.D.; Chaston, S.H.H.; Pilbrow, J.R.; Smith, T.D. Electron spin resonance study of the copper(II) chelates of certain monothio-β-diketones and diethyldithiocarbamate. Inorg. Chem. 1971, 10, 2219–2225. [Google Scholar] [CrossRef]
- Chanthal, S.; Suwamart, N.; Ruangviriyachai, C. Solid-Phase Extraction with Diethyldithiocarbamate as Chelating Agent for Preconcentration and Trace Determination of Copper, Iron and Lead in Fruit Wine and Distilled Spirit by Flame Atomic Absorption Spectrometry. E-J. Chem. 2011, 8, 1280–1292. [Google Scholar] [CrossRef]
- Palmer, D.A.; Benezeth, P. Solubility of Copper Oxides in Water and Steam. In Proceedings of the 14th International Conference on the Properties of Water and Steam, Kyoto, Japan, 29 August–3 September 2004; pp. 491–496. [Google Scholar]
- Yin, I.X.; Zhang, J.; Zhao, I.S.; Mei, M.L.; Li, Q.; Chu, C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020, 15, 2555–2562. [Google Scholar] [CrossRef]
- Morones, J.R.; Elechiguerra, J.L.; Camacho, A.; Holt, K.; Kouri, J.B.; Ramirez, J.T.; Yacaman, M.J. The bactericidal effect of silver nanoparticles. Nanotechnology 2005, 16, 2346. [Google Scholar] [CrossRef]
- Feng, Q.L.; Wu, J.; Chen, G.Q.; Cui, F.Z.; Kin, T.N.; Kim, J.O. A mechanistic study of the antibacterial effect of silver ions on Escherichia coli and Staphylococcus aureus. J. Biomed. Mater. Res. 2000, 52, 662–668. [Google Scholar] [CrossRef]
| Organism | Time (min) | Survival | |
|---|---|---|---|
| Evap. | No. Evap. | ||
| MRSA | 0 | 0.41 | 0.80 |
| 30 | 0.00006 | 0.012 | |
| 60 | 0.00001 | 0.03 | |
| Strep | 0 | 0.004 | 1.0 |
| 30 | 0.0001 (<) | 0.11 | |
| 60 | 0.0001 (<) | 0.00008 | |
| Pseudomonas | 0 | 0.052 | 0.24 |
| 30 | 0.00001 (<) | 0.005 | |
| 60 | 0.00001 (<) | 0.001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benmamoun, Z.; Wyhopen, T.; Li, Y.; Ducker, W.A. Mechanism and Efficacy of Cu2O-Treated Fabric. Antibiotics 2022, 11, 1633. https://doi.org/10.3390/antibiotics11111633
Benmamoun Z, Wyhopen T, Li Y, Ducker WA. Mechanism and Efficacy of Cu2O-Treated Fabric. Antibiotics. 2022; 11(11):1633. https://doi.org/10.3390/antibiotics11111633
Chicago/Turabian StyleBenmamoun, Zachary, Trent Wyhopen, You Li, and William A. Ducker. 2022. "Mechanism and Efficacy of Cu2O-Treated Fabric" Antibiotics 11, no. 11: 1633. https://doi.org/10.3390/antibiotics11111633
APA StyleBenmamoun, Z., Wyhopen, T., Li, Y., & Ducker, W. A. (2022). Mechanism and Efficacy of Cu2O-Treated Fabric. Antibiotics, 11(11), 1633. https://doi.org/10.3390/antibiotics11111633







