A Formative Assessment of Antibiotic Dispensing/Prescribing Practices and Knowledge and Perceptions of Antimicrobial Resistance (AMR) among Healthcare Workers in Lahore Pakistan
Abstract
1. Introduction
2. Results
2.1. Demographics
2.2. Healthcare Facilities
2.3. Antibiotic Dispensing and Prescribing
2.4. Familiarity with Guidelines and Policies
2.5. Knowledge and Perceptions of AMR
3. Discussion
4. Materials and Methods
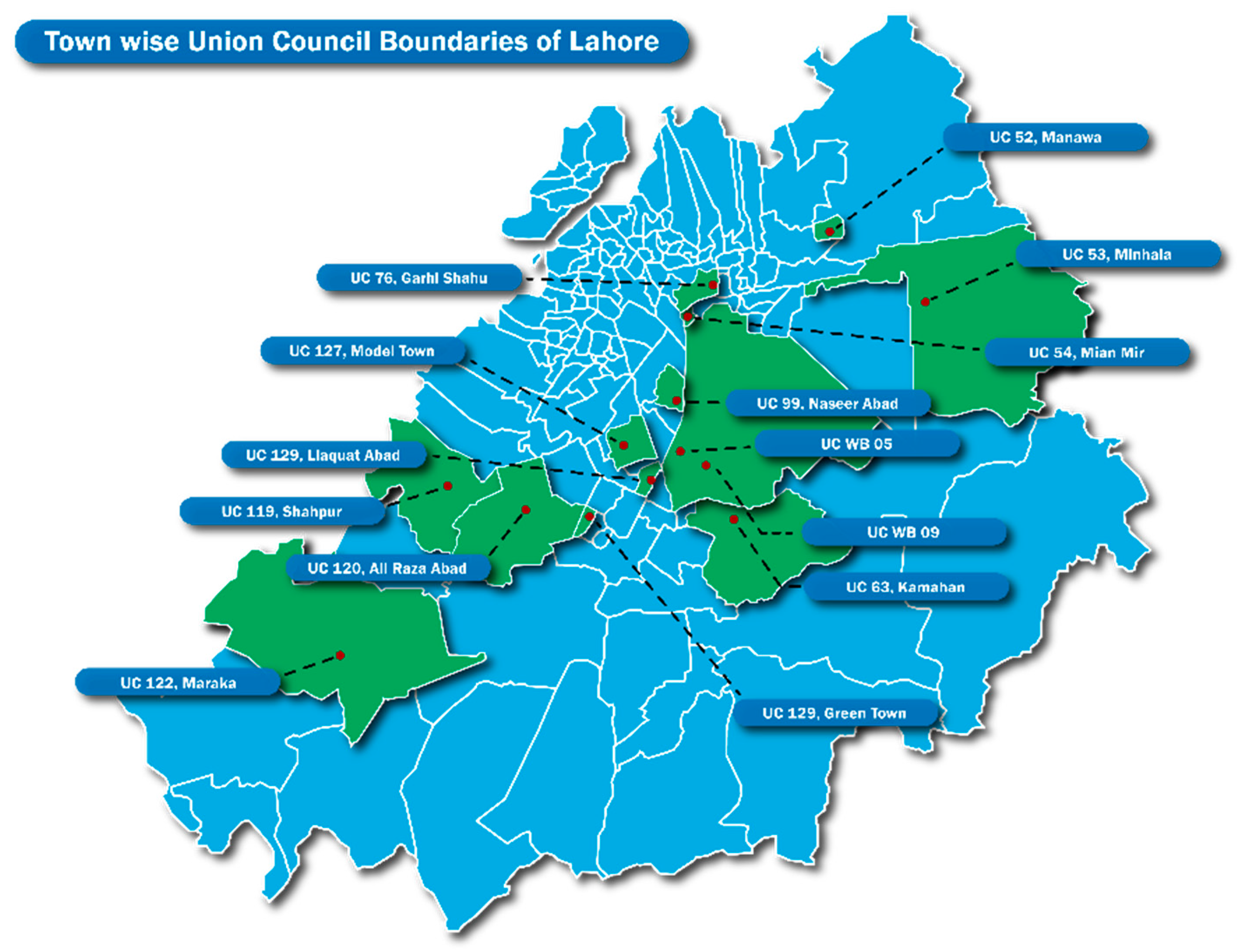
4.1. Research Site
4.2. Healthcare in Lahore
4.3. Research Design
4.4. Research Populations
4.5. Survey Development
4.6. Pilot of the Survey Instrument
4.7. Survey Sample Size and Sampling Strategy
4.8. Survey Data Collection and Management
4.9. Survey Data Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Duffy, E.; Ritchie, S.; Metcalfe, S.; Van Bakel, B.; Thomas, M.G. Antibacterials dispensed in the community comprise 85–95% of total human antibacterial consumption. J. Clin. Pharm. Ther. 2018, 43, 59–64. [Google Scholar] [CrossRef]
- Res, R.; Hoti, K.; Charrois, T.L. Pharmacists’ perceptions regarding optimization of antibiotic prescribing in the community. J. Pharm. Pract. 2017, 30, 146–153. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations; The Review on Antimicrobial Resistance; Wellcome Trust: London, UK, 2016. [Google Scholar]
- Planta, M.B. The role of poverty in antimicrobial resistance. J. Am. Board. Fam. Med. 2007, 20, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.A.; Vlieghe, E.; Mendelson, M.; Wertheim, H.; Ndegwa, L.; Villegas, M.V.; Gould, I.; Hara, G.L. Antibiotic stewardship in low-and middle-income countries: Same, but different? Clin. Microbiol. Infect. 2017, 23, 812–818. [Google Scholar] [CrossRef]
- Jayatilleke, K. Challenges in Implementing Surveillance Tools of High-Income Countries (HICs) in Low Middle Income Countries (LMICs). Curr. Treat. Options Infect Dis. 2020, 12, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, S.; Nishtar, N.; Aleem, N.; Rashidian, A. Access to Essential Medicines: In Pakistan Identifying Policy Research and Concerns. PloS ONE 2013, 8, e63515. [Google Scholar] [CrossRef]
- World Health Organization. Primary Healthcare Systems: Comprehensive Case Study from Pakistan. 2017. Available online: WHO-HIS-HSR-17.37-eng.pdf (accessed on 29 August 2022).
- Khan, M.S.; Durrance-Bagale, A.; Legido-Quigley, H.; Mateus, A.; Hasan, R.; Spencer, J.; Hanefeld, J. ‘LMICs as reservoirs of AMR’: A comparative analysis of policy discourse on antimicrobial resistance with reference to Pakistan. Health Policy Plan 2019, 34, 178–187. [Google Scholar] [CrossRef]
- UNICEF—UN Children’s Fund; Bureau of Statistics, Planning and Development Department, Government of Sindh. Sindh: Monitoring the Situation of Children and Women. Document #2060847. 2015. Available online: https://reliefweb.int/report/pakistan/sindh-multiple-indicator-cluster-survey-2018-19-survey-findings-report-monitoring (accessed on 30 August 2022).
- Ashraf, F.; Hafeez, A.; Imtiaz, F.; Ayub, A.; Imtiaz, H. Antibiotic dispensing and prescription patterns in pharmacies in Islamabad and Rawalpindi, Pakistan. Int. J. Collab. Res. Intern. Med. Public Health 2019. Available online: https://internalmedicine.imedpub.com/antibiotic-dispensing-and-prescription-pattern-inpharmacies-of-islamabad-and-rawalpindi-pakistan.php?aid=19360 (accessed on 30 August 2022).
- Acharya, Y.; Nepal, P.; Yang, D.; Karki, K.; Bajracharya, D.; Prentiss, T.; Davis, S.L.; Kaljee, L. Economic and social drivers of antibiotic dispensing practices among community pharmacies in Nepal. Trop. Med. Int. Health 2021, 26, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Farooqui, H.H.; Mehta, A.; Selvaraj, S. Outpatient antibiotic prescription rate and pattern in the private sector in India: Evidence from medical audit data. PLoS ONE 2019, 14, e0224848. [Google Scholar] [CrossRef]
- Yam, E.; Hsu, L.Y.; Yap, E.P.H.; Yeo, T.W.; Lee, V.; Schlundt, J.; Lwin, M.O.; Limmathurotsakul, D.; Jit, M.; Dedon, P.; et al. Antimicrobial resistance in the Asia Pacific region: A meeting report. Antimicrob. Resist. Infect. Control 2019, 8. Available online: https://aricjournal.biomedcentral.com/articles/10.1186/s13756-019-0654-8 (accessed on 25 August 2022). [CrossRef] [PubMed]
- Abrar, S.; Hussain, S.; Khan, R.A.; Ain, N.U.; Haider, H.; Riaz, X. Prevalence of extended-sprectrum beta-lactamese-producing Enterobacteriaceae: First systematic meta-analysis report from Pakistan. Antimicrob. Resist. Infect. Control 2018, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.M.; Simon, R. The Gathering Storm: Is Untreatable Typhoid Fever on the Way? mBio 2018, 9, e00482-18. [Google Scholar] [CrossRef]
- Dyar, O.J.; Huttner, B.; Schouten, J.; Pulcini, C.; ESGAP (ESCMID Study Group for Antimicrobial stewardship). What is antimicrobial stewardship? Clin. Microbiol. Infect. 2017, 23, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Joshi, R.D.; Zervos, M.; Kaljee, L.M.; Shrestha, B.; Maki, G. Evaluation of a Hospital-Based Post-Prescription Review and Feedback Pilot in Kathmandu, Nepal. Am. J. Trop. Med. Hyg. 2019, 101, 923–928. [Google Scholar] [CrossRef] [PubMed]
- Maki, G.; Smith, I.; Paulin, S.; Kaljee, L.; Kasambara, W.; Mlotha, J. Feasibility Study of the World Health Organization Health Care Facility-Based Antimicrobial Stewardship Toolkit for Low- and Middle-Income Countries. Antibiotics 2020, 9, 556. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. COVID-19 and Antimicrobial Resistance. 2022. Available online: https://www.cdc.gov/drugresistance/pdf/covid19-impact-report-508.pdf (accessed on 30 August 2022).
- Bendala Estrada, A.D.; Calderón Parra, J.; Fernández Carracedo, E.; Muiño Míguez, A.; Ramos Martínez, A.; Muñez Rubio, E. Inadequate use of antibiotics in the COVID-19 era: Effectiveness of antibiotic therapy. BMC Infect. Dis. 2021, 21, 1144. [Google Scholar] [CrossRef]
- Gras, M.; Gras-Champel, V.; Moragny, J.; Delaunay, P.; Laugier, D.; Masmoudi, K. Impact of the COVID-19 outbreak on the reporting of adverse drug reactions associated with self-medication. Ann. Pharm. Fr. 2021, 79, 522–529. [Google Scholar] [CrossRef]
- Lucien, M.A.B.; Canarie, M.F.; Kilgore, P.E.; Jean-Denis, G.; Fénélon, N.; Pierre, M.; Cerpa, M.; Joseph, G.A.; Maki, G.; Zervos, M.J.; et al. Antibiotics and antimicrobial resistance in the COVID-19 era: Perspective from resource-limited settings. Int J Infect Dis. 2021, 104, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Nino-Orrego, M.J.; Baracaldo-Santamaría, D.; Patricia Ortiz, C.; Zuluaga, H.P.; Cruz-Becerra, S.A.; Soler, F.; Pérez-Acosta, A.M.; Delgado, D.R.; Calderon-Ospina, C.A. Prescription for COVID-19 by non-medical professionals during the pandemic in Colombia: A cross-sectional study. Ther. Adv. Drug Saf. 2022, 13, 20420986221101964. [Google Scholar] [CrossRef] [PubMed]
- Tomczyk, S.; Taylor, A.; Brown, A.; de Kraker, M.E.A.; El-Saed, A.; Alshamrani, M.; Hendriksen, R.S.; Jacob, M.; Löfmark, S.; Perovic, O.; et al. WHO AMR Surveillance and Quality Assessment Collaborating Centres Network. Impact of the COVID-19 pandemic on the surveillance, prevention and control of antimicrobial resistance: A global survey. J. Antimicrob. Chemother. 2021, 76, 3045–3058. [Google Scholar] [CrossRef]
- Ghosh, S.; Bornman, C.; Zafer, M.M. Antimicrobial Resistance Threats in the emerging COVID-19 pandemic: Where do we stand? J. Infect. Public Health 2021, 14, 555–560. [Google Scholar] [CrossRef]
- Miller, R.; Goodman, C. Performance of retail pharmacies in low- and middle-income Asian settings: A systematic review. Health Policy Plan 2016, 31, 940–953. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antimicrobial Stewardship Programmes in Health-Care Facilities in Low- and Middle-Income Countries: A WHO Practical Toolkit. 2019. Available online: https://apps.who.int/iris/handle/10665/329404 (accessed on 30 August 2022).
- World Health Organization. Infection Prevention and Control in Primary Care: A Toolkit of Resources. 2021. Available online: https://apps.who.int/iris/handle/10665/346694 (accessed on 30 August 2022).
- World Health Organization. AWaRe Classifications. 2021. Available online: https://www.who.int/publications/i/item/2021-aware-classification (accessed on 30 August 2022).
- World Health Organization. Adopt AWaRe. Available online: https://adoptaware.org/ (accessed on 30 August 2022).
- Saleem, Z.; Saeed, H.; Akbar, Z.; Saeed, A.; Khalid, S.; Farrukh, L. WHO key access antibiotics price, availability and affordability in private sector pharmacies in Pakistan. Cost. Eff. Resour. Alloc. 2021, 19, 10. [Google Scholar] [CrossRef]
- Saleem, Z.; Hassali, M.A.; Godman, B.; Fatima, M.; Ahmad, Z.; Sajid, A. Sale of WHO AWaRe groups antibiotics without a prescription in Pakistan: A simulated client study. J. Pharm. Policy Pract. 2020, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Majid Aziz, M.; Haider, F.; Rasool, M.F.; Hashmi, F.K.; Bahsir, S.; Li, P. Dispensing of Non-Prescribed Antibiotics from Community Pharmacies of Pakistan: A Cross-Sectional Survey of Pharmacy Staff’s Opinion. Antibiotics 2021, 10, 482. [Google Scholar] [CrossRef] [PubMed]
- Asghar, S.; Atif, M.; Mushtaq, I.; Malik, I.; Hayat, K.; Babar, Z.U. Factors associated with inappropriate dispensing of antibiotics among non-pharmacist pharmacy workers. Res. Social Adm. Pharm. 2020, 16, 805–811. [Google Scholar] [CrossRef]
- Provinsional Province-Wise Population by Sex and Rural/Urban Areas: Pakistan. 2017. Available online: https://web.archive.org/web/20170829164748/http://www.pbscensus.gov.pk/sites/default/files/DISTRICT_WISE_CENSUS_RESULTS_CENSUS_2017.pdf#page=6 (accessed on 30 August 2022).
- Charan, J.; Biswas, T. How to calculate sample size for different study designs in medical research. Indian J. Psychol. Med. 2013, 35, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
| Physician (N = 41) | Nurse (N = 29) | LHW or LHV * (N = 10) | Midwife (N = 18) | Pharmacy Manager or Clerk (N = 49) | Medicine Shop Owner or Compounder (N = 23) | Medical Technician (N = 7) | ||
|---|---|---|---|---|---|---|---|---|
| Gender c | Male | 34.1% (14) | 3.4% (1) | 0 | 0 | 85.7% (42) | 100.0% (23) | 57.1% (4) |
| Female | 65.9% (27) | 96.6% (28) | 100.0% (10) | 100.0% (18) | 14.3% (7) | 0 | 42.9%(3) | |
| Age | Mean (SD) | 36.4 (11.8) | 30.3 (6.6) | 38.7 (12.8) | 32.7 (7.2) | 27.7 (6.3) | 34.3 (12.1) | 34.7 (12.7) |
| Site c | Rural | 9.8% (4) | 0 | 40.0% (4) | 5.6% (1) | 0 | 13.0% (3) | 0 |
| Urban | 90.2%(37) | 100.0% (29) | 60.0% (6) | 94.4% (17) | 100.0% (49) | 87.0% (20) | 100.0% (7) |
| Private Clinics | BHUs | Pharmacies and Medicine Shops | Referral Hospitals | |
|---|---|---|---|---|
| Upper Respiratory Infection a | 2.9 (1.6) | 2.1 (1.3) | 2.8 (1.4) | 2.2 (1.1) |
| Gastrointestinal b | 2.5 (1.3) | 2.6 (1.1) | 1.9 (0.9) | 2.2 (1.2) |
| Urinary Tract Infection (UTI) c | 2.4 (1.1) | 4.0 (1.2) | 3.4 (1.1) | 2.9 (1.1) |
| Skin/Wound Infection c | 3.7 (1.4) | 2.8 (1.3) | 2.6 (1.2) | 4.1 (1.1) |
| Pelvic Inflammatory Disease (PID) c | 3.7 (1.3) | 3.5 (1.3) | 4.5 (0.9) | 3.6 (1.4) |
| Physician | Nurse | LHW or LHV * | Midwife | Pharmacy Manager or Clerk | Medicine Shop owner or Compounder | Medical Technician | |
|---|---|---|---|---|---|---|---|
| Amoxicillin/Augmentin b | 1.7 (SD 1.3) | 2.7 (SD 1.6) | 1.6 (SD 0.8) | 1.9 (SD 1.0) | 3.0 (SD 1.5) | 2.5 (SD 1.8) | 1.7 (SD 1.4) |
| Ampicillin c | 4.0 (SD 4.3) | 2.6 (SD 2.8) | 1.7 (SD 2.5) | 2.0 (SD 2.7) | 5.3 (SD 1.4) | 4.0 (SD 2.9) | 3.4 (SD 2.6) |
| Azithromycin b | 3.7 (SD 2.3) | 2.8 (SD 2.3) | 1.9 (SD 2.6) | 1.7 (SD 2.3) | 2.2 (SD 1.3) | 1.8 (SD 1.5) | 2.3 (SD 2.6) |
| Cefixime a | 2.4 (SD 1.6) | 2.4 (SD 1.9) | 1.5 (SD 1.8) | 1.3 (SD 1.6) | 2.6 (SD 1.4) | 3.0 (SD 1.1) | 3.4 (SD 2.0) |
| Ceftriaxone (injectable) c | 3.3 (SD 2.4) | 1.6 (SD 1.3) | 1.6 (SD 2.7) | 1.4 (SD 1.7) | 5.7 (SD 1.8) | 5.1 (SD 1.7) | 3.6 (SD 2.6) |
| Ciprofloxacin c | 3.3 (SD 1.6) | 2.5 (SD 1.4) | 1.2 (SD 0.9) | 2.1 (SD 1.5) | 3.2 (SD 1.4) | 3.0 (SD 1.6) | 3.3 (SD 2.0) |
| Co-trimoxazole c | 4.1 (SD 2.7) | 3.3 (SD 3.3) | 2.5 (SD 1.8) | 2.0 (SD 2.7) | 5.5 (SD 1.6) | 4.8 (SD 1.9) | 4.4 (SD 2.8) |
| Physician | Nurse | LHW or LHV * | Midwife | Pharmacy Manager or Clerk | Medicine Shop Owner or Compounder | Medical Technician | |
|---|---|---|---|---|---|---|---|
| Fever a | 48.8% (20) | 37.9% (11) | 30.0% (3) | 44.4% (8) | 21.7% (10) | 21.7% (5) | 0 |
| Cough | 26.8% (11) | 41.4% (4) | 40.0% (4) | 33.3% (6) | 26.5% (13) | 34.8% (8) | 0 |
| Sore Throat a | 75.6% (31) | 44.8% (13) | 60.0% (6) | 52.9% (9) | 47.9% (23) | 43.5% (10) | 42.9% (3) |
| Diarrhea b (lasting more than one day) | 51.2% (21) | 65.5% (19) | 50.0% (5) | 61.1% (11) | 43.8% (21) | 30.4% (7) | 28.6% (2) |
| Physician | Nurse | LHW or LHV * | Midwife | Pharmacy Manager or Clerk | Medicine Shop Owner or Compounder | Medica Technician | |
|---|---|---|---|---|---|---|---|
| Fever | 48.8% (20) | 44.8% (13) | 60.0% (6) | 55.6% (10) | 36.7% (18) | 60.9% (14) | 42.9% (3) |
| Cough | 31.7% (13) | 41.4% (12) | 40.0% (4) | 55.6% (10) | 51.0% (25) | 43.5% (10) | 28.6% (2) |
| Sore Throat | 70.0% (28) | 58.6% (17) | 80.0% (8) | 55.6% (10) | 77.6% (38) | 65.2% (15) | 28.6% (2) |
| Diarrhea b (lasting more than one day) | 58.5% (24) | 55.2% (16) | 80.0% (8) | 61.1% (11) | 70.8% (34) | 39.1% (9) | 42.9% (3) |
| Burning sensation when urinating | 63.4% (28) | 55.2% (16) | 90.0% (9) | 61.1% (11) | 43.8% (21) | 56.5% (13) | 28.6% (2) |
| Physician | Nurse | LHW or LHV * | Midwife | Pharmacy manager or Clerk | Medicine Shop owner or Compounder | Medical Technician | |
|---|---|---|---|---|---|---|---|
| Redness and/or swelling around a wound b | 85.4% (35) | 62.1% (18) | 100.0% (10) | 88.9% (16) | 58.3% (28) | 65.2% (15) | 28.6% (2) |
| Discharge from wound b | 87.8% (36) | 69.0% (20) | 100.0% (10) | 94.4% (17) | 79.2% (38) | 69.6% (16) | 14.3% (1) |
| Physician | Nurse | LHW or LHV * | Midwife | Pharmacy Manager or Clerk | Medicine Shop owner or Compounder | Medical Technician | |
|---|---|---|---|---|---|---|---|
| Knowledge c Possible range 0 to 12 | 7.4 (SD 1.7) | 8.4 (SD 1.7) | 8.7 (SD 1.6) | 8.7 (SD 1.5) | 9.2 (SD 1.7) | 8.4 (SD 1.5) | 8.0 (SD 2.3) |
| Severity c Possible range 4 to 16 | 13.1 (SD 1.8) | 11.2 (SD 1.8) | 11.9 (SD 1.3) | 11.7 (SD 1.2) | 11.8 (SD 1.5) | 11.8 (SD 1.4) | 11.3 (SD 1.0) |
| Self-efficacy c Possible range 3 to 12 | 9.8 (SD 1.1) | 8.7 (SD 1.2) | 8.5 (SD 1.3) | 9.3 (SD 1.0) | 9.0 (SD 1.2) | 8.7 (SD 1.1) | 8.0 (SD 1.0) |
| Response efficacy Possible range 2 to 8 | 5.8 (SD 0.8) | 5.2 (SD 0.8) | 5.4 (SD 0.7) | 5.6 (SD 0.8) | 5.4 (SD 1.0) | 5.4 (SD 0.7) | 5.4 (SD 1.3) |
| Response cost c Possible range 2 to 8 | 4.3 (SD 1.1) | 4.1 (SD 0.9) | 4.4 (SD (1.3) | 4.8 (SD 1.0) | 5.2 (SD 1.1) | 5.0 (SD 1.3) | 4.1 (SD 1.1) |
| Knowledge (Range 0 to 12) Response Options: True/False | Antibiotics have saved millions of lives |
| Antibiotics are good for treating infections caused by viruses | |
| Antibiotic kill bacteria that cause illness | |
| Antibiotics kill good bacteria that protect the body from infection | |
| Antibiotics can cure colds and flu | |
| Antibiotics can be used to treat COVID-19 | |
| It is safe to use antibiotics from family, friends and others | |
| Some people have allergies to antibiotics | |
| A person should only stop using an antibiotic after consulting the prescriber (physician) | |
| Antibiotic resistance is not a concern because new antibiotics will be available in the future | |
| Antibiotic resistance is a significant problem in Pakistan | |
| The majority of antibiotic use occurs in inpatient hospital settings in Pakistan | |
| Severity of AMR (Range 4 to 16) Response Options: Strongly Agree, Agree, Disagree, Strongly Disagree | Antibiotic resistance affects my patients’/customers’ health and well-being |
| Antibiotic resistance affects my ability to help my patients’/customers’ recover from infectious diseases | |
| Antibiotic resistance increases the cost of health care | |
| Antibiotic resistance could affect my family’s health and well-being | |
| Self-efficacy to Make Changes (Range 3 to 12) Response Options: Strongly Agree, Agree, Disagree, Strongly Disagree | I can change my antibiotic prescribing/dispensing practices based on government guidelines |
| I can explain to my patients/customers why they do NOT need an antibiotic in certain situations (e.g., viral infections | |
| I can be an advocate for antibiotic stewardship with my peers and colleagues | |
| Response-Efficacy (Range 2 to 8) Response Options: Strongly Agree, Agree, Disagree, Strongly Disagree | I can contribute to decreasing antibiotic resistance by changing my prescribing/dispensing practices |
| The few antibiotics that I prescribe/dispense do not affect antibiotic resistance in Pakistan | |
| Response Costs (Range 2 to 8) Response Options: Strongly Agree, Agree, Disagree, Strongly Disagree | I will lose customers or patients if I decrease prescribing/dispensing antibiotics |
| I would be considered an irresponsible healthcare provider if I did not provide antibiotics to patients/customers when they request them |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rakhshani, N.S.; Kaljee, L.M.; Khan, M.I.; Prentiss, T.; Turab, A.; Mustafa, A.; Khalid, M.; Zervos, M. A Formative Assessment of Antibiotic Dispensing/Prescribing Practices and Knowledge and Perceptions of Antimicrobial Resistance (AMR) among Healthcare Workers in Lahore Pakistan. Antibiotics 2022, 11, 1418. https://doi.org/10.3390/antibiotics11101418
Rakhshani NS, Kaljee LM, Khan MI, Prentiss T, Turab A, Mustafa A, Khalid M, Zervos M. A Formative Assessment of Antibiotic Dispensing/Prescribing Practices and Knowledge and Perceptions of Antimicrobial Resistance (AMR) among Healthcare Workers in Lahore Pakistan. Antibiotics. 2022; 11(10):1418. https://doi.org/10.3390/antibiotics11101418
Chicago/Turabian StyleRakhshani, Noor Sabah, Linda Marie Kaljee, Mohammad Imran Khan, Tyler Prentiss, Ali Turab, Ali Mustafa, Memoona Khalid, and Marcus Zervos. 2022. "A Formative Assessment of Antibiotic Dispensing/Prescribing Practices and Knowledge and Perceptions of Antimicrobial Resistance (AMR) among Healthcare Workers in Lahore Pakistan" Antibiotics 11, no. 10: 1418. https://doi.org/10.3390/antibiotics11101418
APA StyleRakhshani, N. S., Kaljee, L. M., Khan, M. I., Prentiss, T., Turab, A., Mustafa, A., Khalid, M., & Zervos, M. (2022). A Formative Assessment of Antibiotic Dispensing/Prescribing Practices and Knowledge and Perceptions of Antimicrobial Resistance (AMR) among Healthcare Workers in Lahore Pakistan. Antibiotics, 11(10), 1418. https://doi.org/10.3390/antibiotics11101418





