Exploring the Relationships between Structure and Antimicrobial Potency of Quinolinequinones
Abstract
1. Introduction
2. Materials and Methods
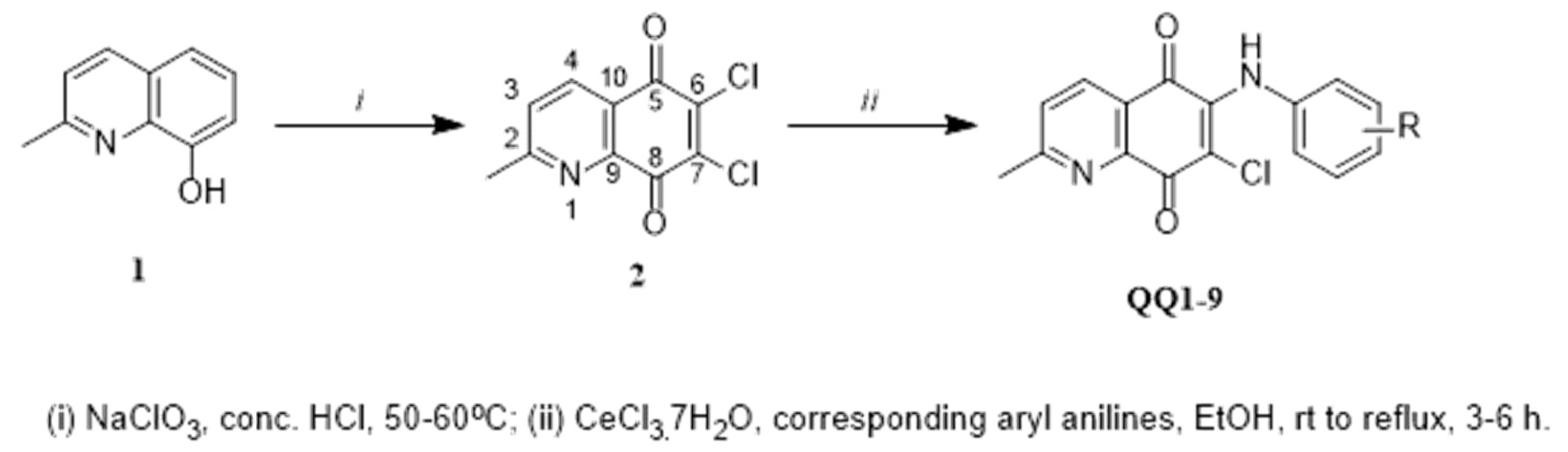
2.1. Chemistry
2.2. In Vitro Antimicrobial Activity
2.2.1. Determination of Minimum Inhibitory Concentrations (MICs)
2.2.2. Determination of Bactericidal Effects by Time-Kill Curve Kinetics (TKC)
2.2.3. Biofilm Attachment and Inhibition of Biofilm Formation Assays
2.3. Statistical Analysis
3. Results
3.1. Chemistry
3.2. Library Screening
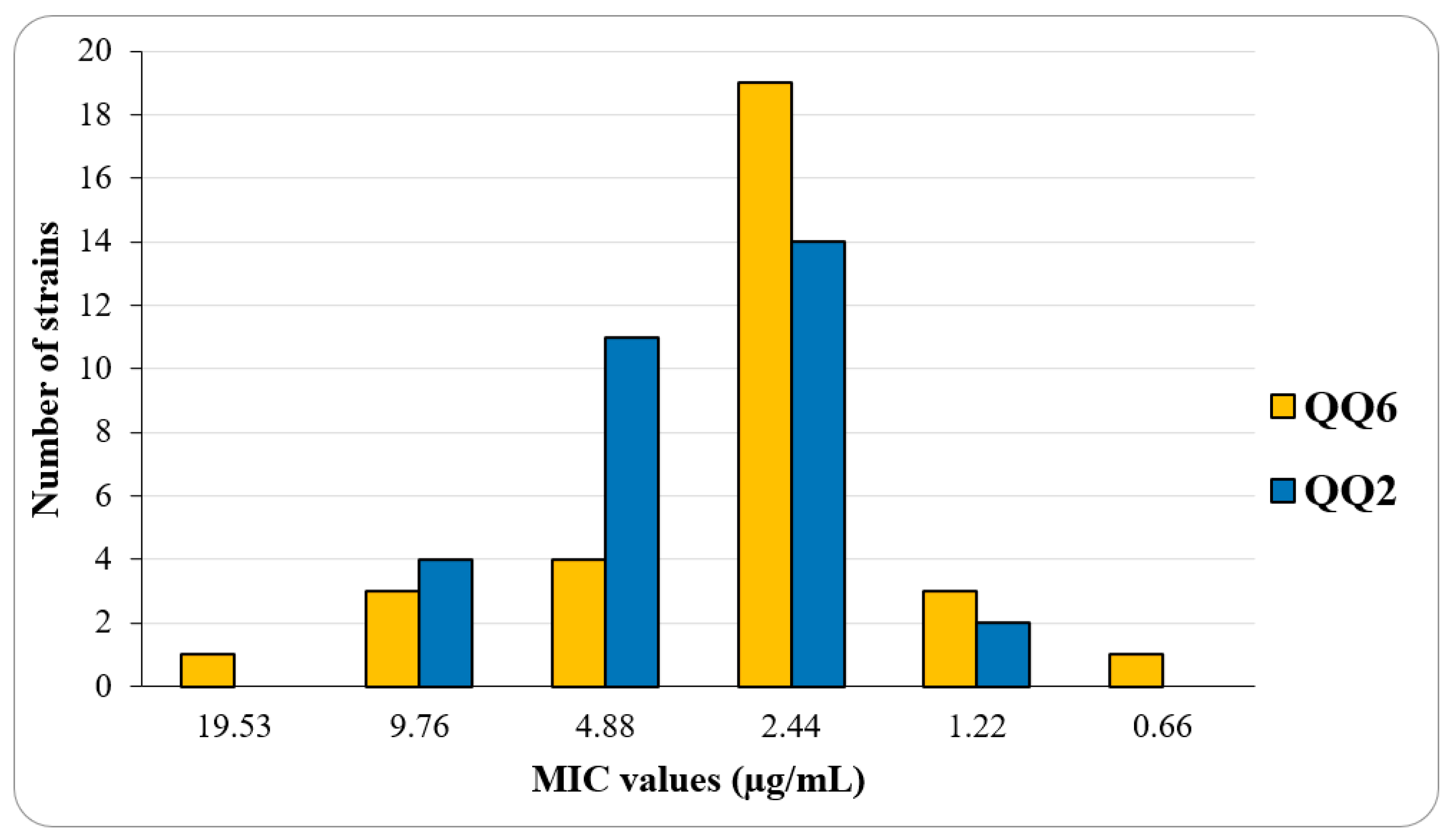
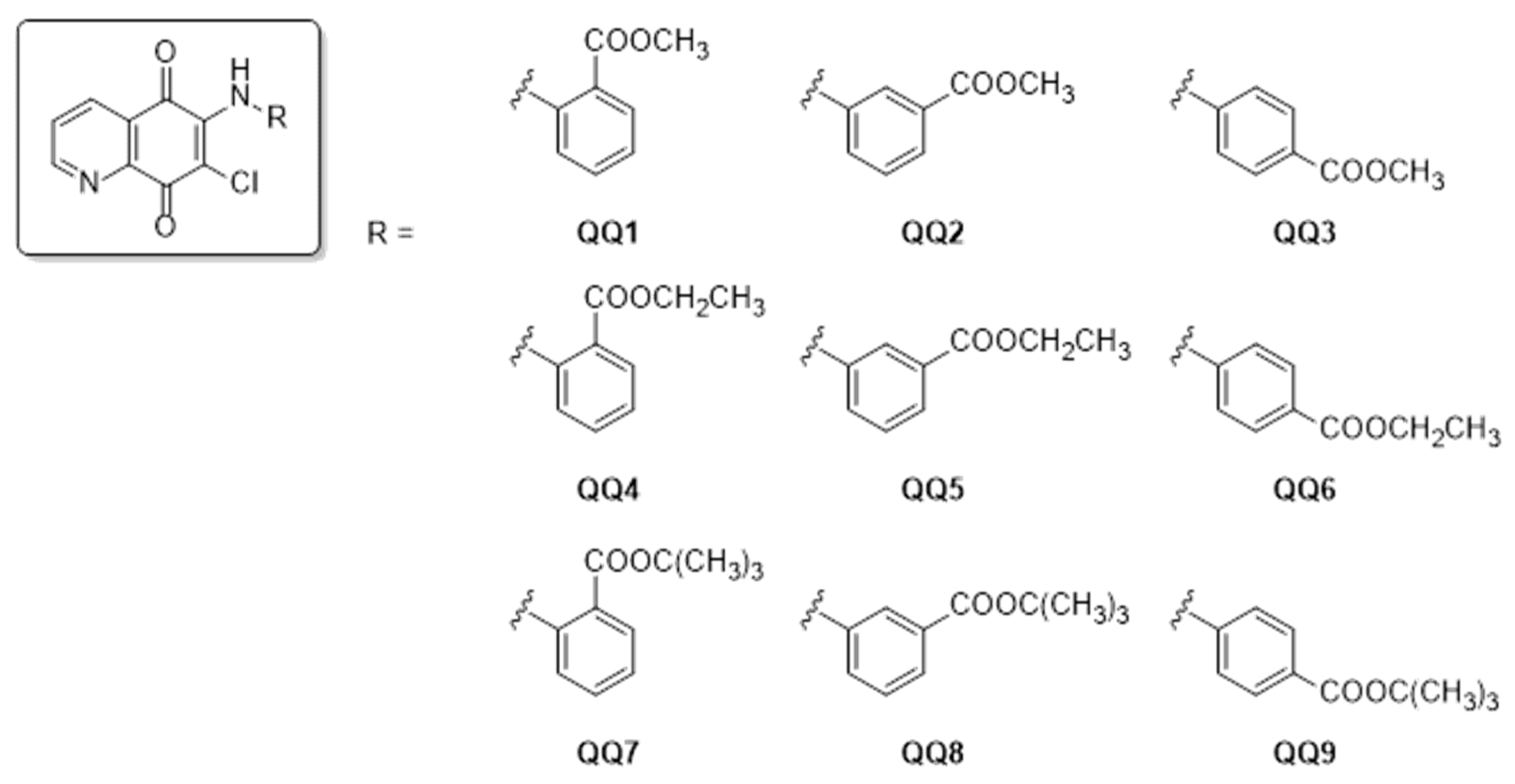
3.3. Structure–Activity Relationships (SARs) Study for Biological Evaluation
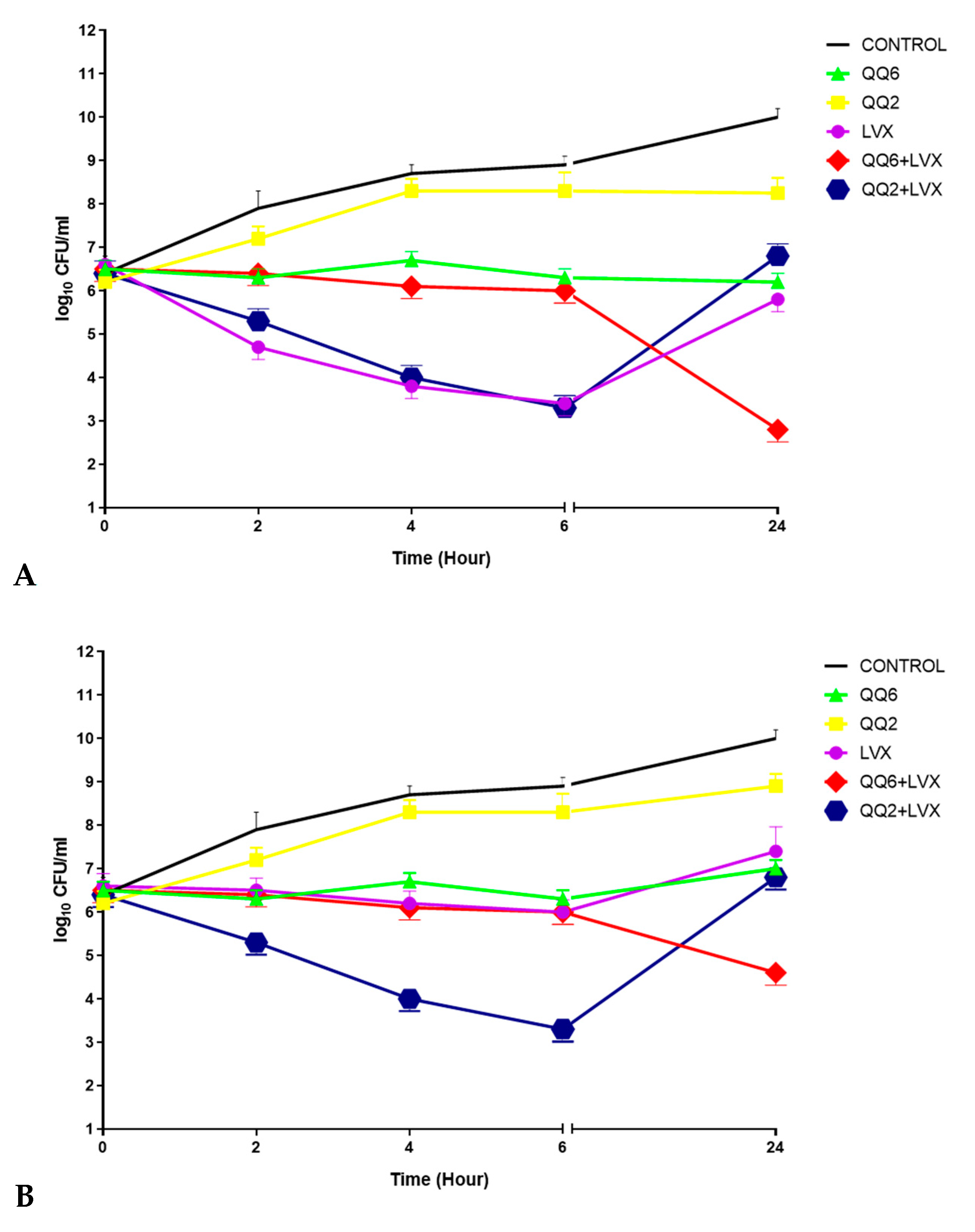
3.4. Bactericidal Effects by Time-Kill Curve Kinetic Study
3.5. Effect of Quinolinequinones on Biofilm Formation
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| APIs | Active pharmaceutical ingredients |
| ATCC® | American Type Culture Collection |
| CLSI | Clinical Laboratory Standards Institute |
| MRSA | Methicillin-resistant Staphylococcus aureus |
| MICs | Minimum inhibitory concentrations |
| NCCLS | National Committee for Clinical Laboratory Standards |
| PBMCs | Peripheral blood mononuclear cells |
| SAR | Structure–activity relationship models |
| TKC | Time-kill Curve |
References
- Sharifi-Rad, J.; Ozleyen, A.; Tumer, T.B.; Adetunji, C.O.; El Omari, N.; Balahbib, A.; Taheri, Y.; Bouyahya, A.; Martorell, M.; Martins, N.; et al. Natural Products and Synthetic Analogs as a Source of Antitumor Drugs. Biomolecules 2019, 9, 679. [Google Scholar] [CrossRef] [PubMed]
- Duval, R.E.; Grare, M.; Demore, B. Fight Against Antimicrobial Resistance: We Always Need New Antibacterials but for Right Bacteria. Molecules 2019, 24, 3152. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, J.F.A.; Saito, A.; Bido, A.T.; Kobarg, J.; Stassen, H.K.; Cardoso, M.B. Defeating Bacterial Resistance and Preventing Mammalian Cells Toxicity Through Rational Design of Antibiotic-Functionalized Nanoparticles. Sci. Rep. 2017, 7, 1326. [Google Scholar] [CrossRef]
- Pan, L.; Chai, H.B.; Kinghorn, A.D. Discovery of new anticancer agents from higher plants. Front. Biosci. 2012, 4, 142–156. [Google Scholar] [CrossRef] [PubMed]
- Durand, G.A.; Raoult, D.; Dubourg, G. Antibiotic discovery: History, methods and perspectives. Int. J. Antimicrob. Ag. 2019, 53, 371–382. [Google Scholar] [CrossRef]
- Nain-Perez, A.; Barbosa, L.C.A.; Maltha, C.R.A.; Forlani, G. First total synthesis and phytotoxic activity of Streptomyces sp. metabolites abenquines. Tetrahedron Lett. 2016, 57, 1811–1814. [Google Scholar] [CrossRef]
- Schatz, A.; Bugie, E.; Waksman, S.A. Streptomycin, a Substance Exhibiting Antibiotic Activity Against Gram-Positive and Gram-Negative Bacteria. Proc. Soc. Exp. Biol. Med. 1944, 55, 66–69. [Google Scholar] [CrossRef]
- Zhang, Z.; Yu, X.; Wang, Z.; Wu, P.; Huang, J. Anthracyclines potentiate anti-tumor immunity: A new opportunity for chemoimmunotherapy. Cancer Lett. 2015, 369, 331–335. [Google Scholar] [CrossRef]
- Ravelo, A.G.; Estevez-Braun, A.; Chavez-Orellana, H.; Perez-Sacau, E.; Mesa-Siverio, D. Recent Studies on Natural Products as Anticancer Agents. Curr. Top. Med. Chem. 2004, 4, 241–265. [Google Scholar] [CrossRef]
- Cordell, G.A. Changing Strategies in Natural-Products Chemistry. Phytochemistry 1995, 40, 1585–1612. [Google Scholar] [CrossRef]
- Silverman, L.; Campbell, R.; Broach, J.R. New assay technologies for high-throughput screening. Curr. Opin. Chem. Biol. 1998, 2, 397–403. [Google Scholar] [CrossRef]
- Liu, W.J.; Li, Q.S.; Hu, J.H.; Wang, H.X.; Xu, F.B.; Bian, Q. Application of natural products derivatization method in the design of targeted anticancer agents from 2000 to 2018. Bioorg. Med. Chem. 2019, 27, 115150. [Google Scholar] [CrossRef] [PubMed]
- Gali-Muhtasib, H.; Roessner, A.; Schneider-Stock, R. Thymoquinone: A promising anti-cancer drug from natural sources. Int. J. Biochem. Cell B 2006, 38, 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Hariharan, P.; Paul-Satyaseela, M.; Gnanamani, A. In vitro profiling of antimethicillin-resistant Staphylococcus aureus activity of thymoquinone against selected type and clinical strains. Lett. Appl. Microbiol. 2016, 62, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Houdkova, M.; Rondevaldova, J.; Doskocil, I.; Kokoska, L. Evaluation of antibacterial potential and toxicity of plant volatile compounds using new broth microdilution volatilization method and modified MTT assay. Fitoterapia 2017, 118, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Kawamukai, M. Biosynthesis and applications of prenylquinones. Biosci. Biotech. Bioch. 2018, 82, 963–977. [Google Scholar] [CrossRef]
- Ryu, C.K.; Park, R.E.; Ma, M.Y.; Nho, J.H. Synthesis and antifungal activity of 6-arylamino-phthalazine-5,8-diones and 6,7-bis(arylthio)-phthalazine-5,8-diones. Bioorg. Med. Chem. Lett. 2007, 17, 2577–2580. [Google Scholar] [CrossRef]
- Kruschel, R.D.; Buzid, A.; Khandavilli, U.B.R.; Lawrence, S.E.; Glennon, J.D.; McCarthy, F.O. Isoquinolinequinone N-oxides as anticancer agents effective against drug resistant cell lines. Org. Biomol. Chem. 2020, 18, 557–568. [Google Scholar] [CrossRef]
- Dias Flaviana, R.F.; Novais, J.S.; Devillart, S.; da Silva, W.A.; Fereirra, M.O.; Loureiro, R.d.S.; Campos, V.R.; Fereirra, V.F.; de Souza, M.C.B.V.; Castro, H.C.; et al. Synthesis and antimicrobial evaluation of amino sugar-based naphthoquinones and isoquinoline-5,8-diones and their halogenated compounds. Eur. J. Med. Chem. 2018, 156, 1–12. [Google Scholar] [CrossRef]
- Shaikh, I.A.; Johnson, F.; Grollman, A.P. Streptonigrin.1. Structure-Activity-Relationships among Simple Bicyclic Analogs—Rate Dependence of DNA-Degradation on Quinone Reduction Potential. J. Med. Chem. 1986, 29, 1329–1340. [Google Scholar] [CrossRef]
- Lown, J.W.; Sim, S.K.; Chen, H.H. Hydroxyl radical production by free and DNA-bound aminoquinone antibiotics and its role in DNA degradation. Electron spin resonance detection of hydroxyl radicals by spin trapping. Can. J. Biochem. 1978, 56, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Bayrak, N.; Ciftci, H.I.; Yildiz, M.; Yildirim, H.; Sever, B.; Tateishi, H.; Otsuka, M.; Fujita, M.; Tuyun, A.F. Structure based design, synthesis, and evaluation of anti-CML activity of the quinolinequinones as LY83583 analogs. Chem. Biol. Interact. 2021, 345, 109555. [Google Scholar] [CrossRef] [PubMed]
- Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania 19087, USA, 2020. Available online: https://www.nih.org.pk/wp-content/uploads/2021/02/CLSI-2020.pdf?utm_medium=email&utm_source=transaction (accessed on 1 August 2022).
- Clinical and Laboratory Standards Institute. Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts, 2nd ed.; Approved Standard; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 1997. [Google Scholar]
- National Committee for Clinical Laboratory Standards. Methods for Determining Bactericidal Activity of Antimicrobial Agents; NCCLS: Wayne, PA, USA, 1999. [Google Scholar]
- Bayrak, N.; Yildiz, M.; Yildirim, H.; Mataraci-Kara, E.; Tuyun, A.F. Novel plastoquinone analogs containing benzocaine and its analogs: Structure-based design, synthesis, and structural characterization. Res. Chem. Intermediat. 2021, 47, 2125–2141. [Google Scholar] [CrossRef]
- Mataraci-Kara, E.; Bayrak, N.; Yildiz, M.; Yildirim, H.; Ozbek-Celik, B.; Tuyun, A.F. Discovery and structure-activity relationships of the quinolinequinones: Promising antimicrobial agents and mode of action evaluation. Drug Dev. Res 2021, 83, 628–636. [Google Scholar] [CrossRef]
- Pulverer, G. Taxonomy of Staphylococcus-Aureus. Zbl. Bakt. Int. J. Med. M. 1986, 262, 425–437. [Google Scholar] [CrossRef]
- Melter, O.; Radojevic, B. Small colony variants of Staphylococcus aureus – review. Folia Microbiol. 2010, 55, 548–558. [Google Scholar] [CrossRef]
- Tong, S.Y.C.; Davis, J.S.; Eichenberger, E.; Holland, T.L.; Fowler, V.G. Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management. Clin. Microbiol. Rev. 2015, 28, 603–661. [Google Scholar] [CrossRef]
- Wu, X.W.; Wu, Z.P.; Wang, L.X.; Zhang, H.B.; Chen, J.W.; Zhang, W.; Gu, L.Q.; Huang, Z.S.; An, L.K. Synthesis, antimicrobial activity and possible mechanism of action of 9-bromo-substituted indolizinoquinoline-5,12-dione derivatives. Eur. J. Med. Chem. 2011, 46, 4625–4633. [Google Scholar] [CrossRef]
- Yildirim, H. Arylthio analogs of 5,8-quinolinedione: Synthesis, characterization, antibacterial, and antifungal evaluations. Phosphorus Sulfur 2020, 195, 516–522. [Google Scholar] [CrossRef]
- Bayrak, N. Novel azanaphtoquinone compounds with aromatic amino moiety: Synthesis, structural characterization, and antimicrobial features. J. Mol. Struct. 2019, 1195, 411–416. [Google Scholar] [CrossRef]
- Joshi, K.M.; Shelar, A.; Kasabe, U.; Nikam, L.K.; Pawar, R.A.; Sangshetti, J.; Kale, B.B.; Singh, A.V.; Patil, R.; Chaskar, M.G. Biofilm inhibition in Candida albicans with biogenic hierarchical zinc-oxide nanoparticles. Biomater. Adv. 2022, 134, 112592. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.V.; Kayal, A.; Malik, A.; Maharjan, R.S.; Dietrich, P.; Thissen, A.; Siewert, K.; Curato, C.; Pande, K.; Prahlad, D.; et al. Interfacial Water in the SARS Spike Protein: Investigating the Interaction with Human ACE2 Receptor and In Vitro Uptake in A549 Cells. Langmuir 2022, 38, 7976–7988. [Google Scholar] [CrossRef] [PubMed]
- Fu, K.P.; Lafredo, S.C.; Foleno, B.; Isaacson, D.M.; Barrett, J.F.; Tobia, A.J.; Rosenthale, M.E. In vitro and in vivo antibacterial activities of levofloxacin (l-ofloxacin), an optically active ofloxacin. Antimicrob. Agents Chemother. 1992, 36, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Rohner, P.; Herter, C.; Auckenthaler, R.; Pechere, J.C.; Waldvogel, F.A.; Lew, D.P. Synergistic effect of quinolones and oxacillin on methicillin-resistant Staphylococcus species. Antimicrob. Agents Chemother. 1989, 33, 2037–2041. [Google Scholar] [CrossRef] [PubMed]
- Rabin, N.; Zheng, Y.; Opoku-Temeng, C.; Du, Y.X.; Bonsu, E.; Sintim, H.O. Agents that inhibit bacterial biofilm formation. Future Med. Chem. 2015, 7, 647–671. [Google Scholar] [CrossRef]
- Di Marco, N.I.; Paez, P.L.; Lucero-Estrada, C.S.M.; Pungitore, C.R. Naphthoquinones inhibit formation and viability of Yersinia enterocolitica biofilm. World J. Microbiol. Biotechnol. 2021, 37, 30. [Google Scholar] [CrossRef]
- Vuong, C.; Otto, M. Staphylococcus epidermidis infections. Microbes Infect. 2002, 4, 481–489. [Google Scholar] [CrossRef]
- Wang, R.; Khan, B.A.; Cheung, G.Y.; Bach, T.H.; Jameson-Lee, M.; Kong, K.F.; Queck, S.Y.; Otto, M. Staphylococcus epidermidis surfactant peptides promote biofilm maturation and dissemination of biofilm-associated infection in mice. J. Clin. Invest. 2011, 121, 238–248. [Google Scholar] [CrossRef]
- Novais, J.S.; Moreira, C.S.; Silva, A.C.J.A.; Loureiro, R.S.; Figueiredo, A.M.S.; Ferreira, V.F.; Castro, H.C.; da Rocha, D.R. Antibacterial naphthoquinone derivatives targeting resistant strain Gram-negative bacteria in biofilms. Microb. Pathog. 2018, 118, 105–114. [Google Scholar] [CrossRef]
- Bayrak, N.; Yildirim, H.; Tuyun, A.F.; Kara, E.M.; Celik, B.O.; Gupta, G.K.; Ciftci, H.I.; Fujita, M.; Otsuka, M.; Nasiri, H.R. Synthesis, Computational Study, and Evaluation of In Vitro Antimicrobial, Antibiofilm, and Anticancer Activities of New Sulfanyl Aminonaphthoquinone Derivatives. Lett. Drug Des. Discov. 2017, 14, 647–661. [Google Scholar] [CrossRef]
- Tuyun, A.F.; Yıldız, M.; Bayrak, N.; Yıldırım, H.; Kara, E.M.; Jannuzzi, A.T.; Celik, B.O. Discovery of a new family of heterocyclic amine linked plastoquinone analogs for antimicrobial evaluation. Drug Dev. Res. 2019, 80, 1098–1109. [Google Scholar] [CrossRef] [PubMed]
- Stapleton, P.D.; Taylor, P.W. Methicillin resistance in Staphylococcus aureus: Mechanisms and modulation. Sci. Prog. 2002, 85, 57–72. [Google Scholar] [CrossRef] [PubMed]

| ID | Microorganisms | ||||||
|---|---|---|---|---|---|---|---|
| Gram-Negative Bacteria (MIC, μg/mL) | Gram-Positive Bacteria (MIC, μg/mL) a | ||||||
| P. aeruginosa | E. coli | K. pneumoniae | P. mirabilis | S. aureus | S. epidermidis | E. faecalis | |
| QQ1 | - b | 625 | 1250 | 1250 | 1.22 (6.84) | 1.22 (6.84) | 625 (3503.76) |
| QQ2 | 1250 | 1250 | 1250 | 1250 | 2.44 (13.69) | 1.22 (6.84) | 19.53 (109.49) |
| QQ3 | 1250 | 1250 | 625 | 1250 | 2.44 (13.69) | 1.22 (6.84) | 9.76 (54.75) |
| QQ4 | 1250 | 1250 | 1250 | 1250 | - | 625 (3371.21) | 1250 (6742.43) |
| QQ5 | 1250 | 1250 | - | 1250 | 1.22 (6.58) | 1.22 (6.58) | 19.53 (105.35) |
| QQ6 | 1250 | 625 | 625 | 625 | 1.22 (6.58) | 1.22 (6.58) | 4.88 (26.34) |
| QQ7 | - | - | - | - | - | 156.25 (784.97) | - |
| QQ8 | 625 | - | - | - | - | 156.25 (784.97) | - |
| QQ9 | - | - | - | - | 1250 (6279.78) | 1250 (6279.78) | - |
| Ceftazidime | 2.44 (8.93) | - | - | - | - | - | - |
| Cefuroxime-Na | - | 4.88 (21.88) | 4.88 (21.88) | 2.44 (10.94) | 1.22 (5.47) | - | - |
| Cefuroxime | - | - | - | - | - | 9.76 (46.02) | - |
| Amikacin | - | - | - | - | - | - | 128 (223.84) |
| ID | Microorganisms | ||
|---|---|---|---|
| Fungi (MIC, μg/mL) a | |||
| C. albicans | C. parapsilosis | C. tropicalis | |
| QQ1 | 1250 (7007.52) | 156.25 (875.94) | 625 (3503.76) |
| QQ2 | 156.25 (875.94) | 156.25 (875.94) | 1250 (7007.52) |
| QQ3 | 1250 (7007.52) | 156.25 (875.94) | 625 (3503.76) |
| QQ4 | 1250 (6742.43) | 625 (3371.21) | 1250 (6742.43) |
| QQ5 | 1250 (6742.43) | 78.12 (421.40) | 625 (3371.21) |
| QQ6 | 1250 (6742.43) | 156.25 (842.80) | 625 (3371.21) |
| QQ7 | 4.88 (24.53) | 4.88 (24.53) | - b |
| QQ8 | 4.88 (24.53) | 2.44 (12.27) | - |
| QQ9 | 78.12 (392.49) | 312.50 (1569.94) | - |
| Clotrimazole | 4.88 (14.50) | - | - |
| Amphotericin B | - | 0.5 (0.83) | 1 (1.35) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mataracı-Kara, E.; Bayrak, N.; Yıldız, M.; Yıldırım, H.; TuYuN, A.F. Exploring the Relationships between Structure and Antimicrobial Potency of Quinolinequinones. Antibiotics 2022, 11, 1397. https://doi.org/10.3390/antibiotics11101397
Mataracı-Kara E, Bayrak N, Yıldız M, Yıldırım H, TuYuN AF. Exploring the Relationships between Structure and Antimicrobial Potency of Quinolinequinones. Antibiotics. 2022; 11(10):1397. https://doi.org/10.3390/antibiotics11101397
Chicago/Turabian StyleMataracı-Kara, Emel, Nilüfer Bayrak, Mahmut Yıldız, Hatice Yıldırım, and Amaç Fatih TuYuN. 2022. "Exploring the Relationships between Structure and Antimicrobial Potency of Quinolinequinones" Antibiotics 11, no. 10: 1397. https://doi.org/10.3390/antibiotics11101397
APA StyleMataracı-Kara, E., Bayrak, N., Yıldız, M., Yıldırım, H., & TuYuN, A. F. (2022). Exploring the Relationships between Structure and Antimicrobial Potency of Quinolinequinones. Antibiotics, 11(10), 1397. https://doi.org/10.3390/antibiotics11101397






