Knowledge, Attitudes, and Common Practices of Livestock and Poultry Veterinary Practitioners Regarding the AMU and AMR in Bangladesh
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Population, and Recruitment
2.2. Questionnaire Development
2.3. Sampling Procedure
2.4. Ethical Statement
2.5. Statistical Analysis
3. Results
3.1. Demographic and Socio-economic Characteristics of Respondents
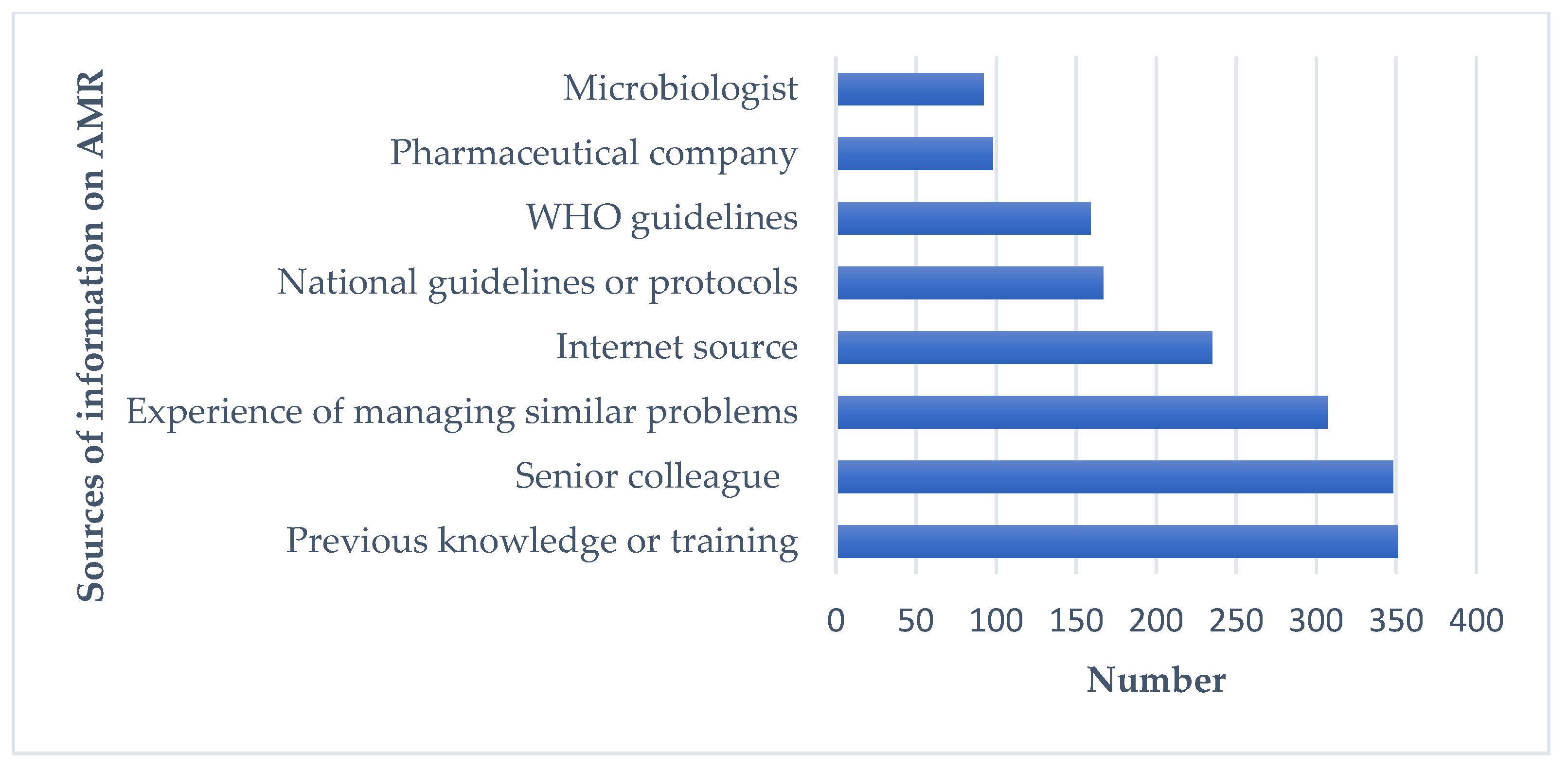
3.2. Sources of Information on AMU and AMR
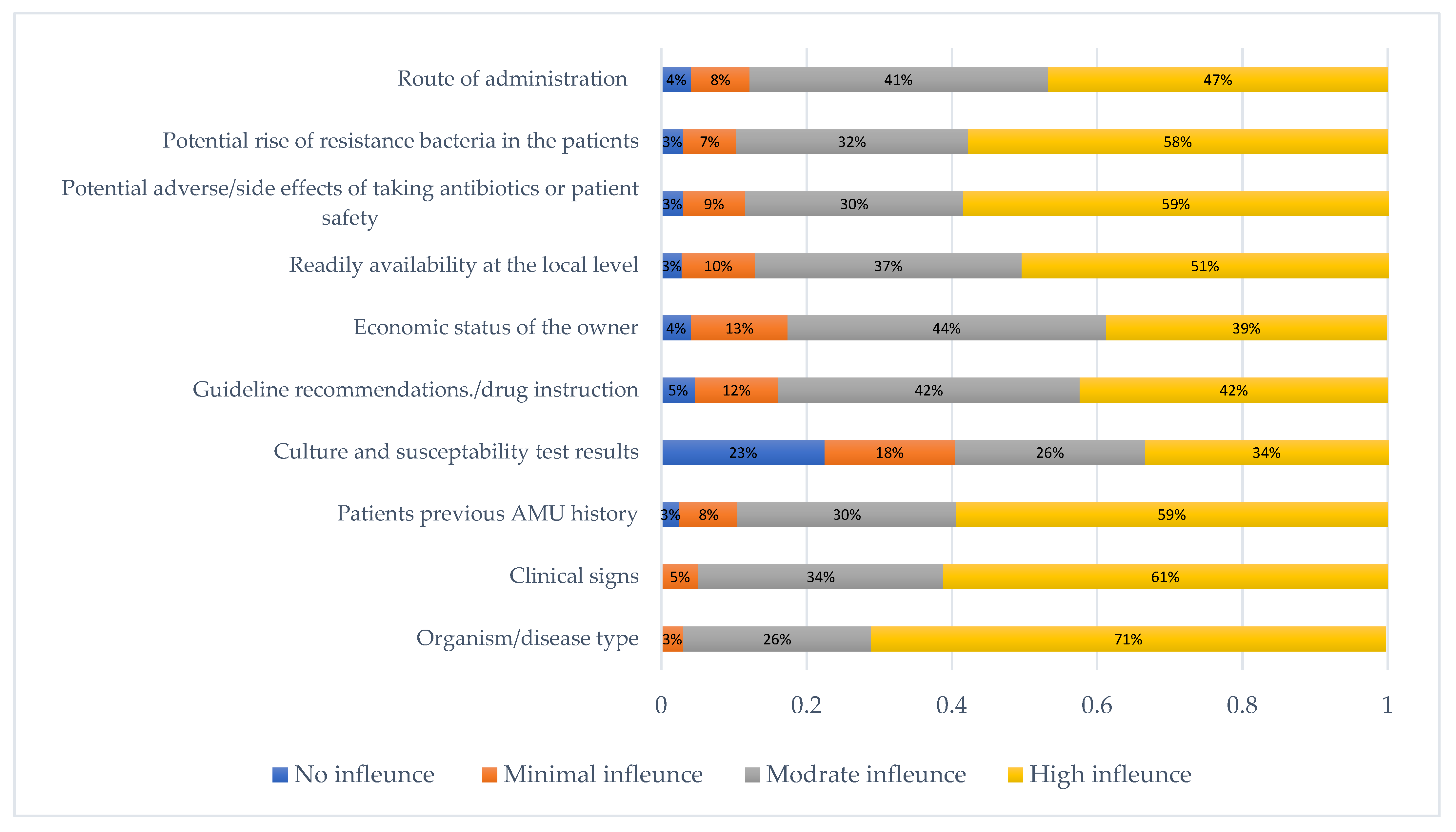
3.3. Role of Clinical Etiological and Other Factors Influencing the Selection of Appropriate Antimicrobials
3.4. Knowledge Factors in Prescribing Antimicrobials
3.5. Attitude Factors
3.6. Practice Factors on AMU and AMR
3.7. Associations with the Level of Antimicrobial Knowledge, Attitudes, and Practices
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferri, M.; Ranucci, E.; Romagnoli, P.; Giaccone, V. Antimicrobial resistance: A global emerging threat to public health systems. Crit. Rev. Food Sci. Nutr. 2017, 57, 2857–2876. [Google Scholar] [CrossRef]
- Hassan, M.; Ahaduzzaman, M.; Alam, M.; Bari, M.; Amin, K.; Faruq, A. Antimicrobial resistance pattern against E. coli and Salmonella spp. in environmental effluents. Int. J. Nat. Sci. 2015, 5, 52–58. [Google Scholar] [CrossRef]
- Ahaduzzaman, M.; Hassan, M.M.; Alam, M.; Islam, S.; Uddin, I. Antimicrobial resistance pattern against Staphylococcus aureus in environmental effluents. Res. J. Vet. Pract. 2014, 2, 13–16. [Google Scholar] [CrossRef]
- Faruq, A.; Hassan, M.M.; Uddin, M.M.; Rahman, M.L.; Rakib, T.M.; Alam, M.; Islam, A. Prevalence and multidrug resistance pattern of Salmonella isolated from resident wild birds of Bangladesh. Int. J. One Health 2016, 2, 35–41. [Google Scholar] [CrossRef]
- Rahman, M.; Islam, A.; Samad, M.; Islam, S.; Uddin, M.; Rumi, M.; Rostal, M.; Hagan, E.; Epistein, J.; Flora, M. Epidemiological assessment of antimicrobial resistance of Salmonella species from wildlife at human-animal interface in Bangladesh. Int. J. Infect. Dis. 2020, 101, 70. [Google Scholar] [CrossRef]
- Wall, B.; Mateus, A.; Marshall, L.; Pfeiffer, D.; Lubroth, J.; Ormel, H.; Otto, P.; Patriarchi, A. Drivers, Dynamics and Epidemiology of Antimicrobial Resistance in Animal Production; Food and Agriculture Organization of the United Nations: Rome, Italy, 2016. [Google Scholar]
- Hassan, M.M.; El Zowalaty, M.E.; Lundkvist, Å.; Järhult, J.D.; Nayem, M.R.K.; Tanzin, A.Z.; Badsha, M.R.; Khan, S.A.; Ashour, H.M. Residual antimicrobial agents in food originating from animals. Trends Food Sci. Technol. 2021, 111, 141–150. [Google Scholar] [CrossRef]
- Economou, V.; Gousia, P. Agriculture and food animals as a source of antimicrobial-resistant bacteria. Infect. Drug Resist. 2015, 8, 49. [Google Scholar] [CrossRef]
- Khan, S.A.; Shawn, A.I.; Syeed, A.; Shaikat, A.H.; Hassan, M.M. Antimicrobial Resistance Pattern in Domestic Animal-Wildlife-Environmental niche via the food chain to humans with a Bangladesh perspective; A systemic review. BMC Vet. Res. 2020, 16, 1–13. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277. [Google Scholar]
- Hockenhull, J.; Turner, A.E.; Reyher, K.K.; Barrett, D.C.; Jones, L.; Hinchliffe, S.; Buller, H.J. Antimicrobial use in food-producing animals: A rapid evidence assessment of stakeholder practices and beliefs. Vet. Rec. 2017, 181, 510. [Google Scholar] [CrossRef]
- Xiong, W.; Sun, Y.; Zeng, Z. Antimicrobial use and antimicrobial resistance in food animals. Environ. Sci. Pollut. Res. 2018, 25, 18377–18384. [Google Scholar] [CrossRef]
- Chantziaras, I.; Boyen, F.; Callens, B.; Dewulf, J. Correlation between veterinary antimicrobial use and antimicrobial resistance in food-producing animals: A report on seven countries. J. Antimicrob. Chemother. 2014, 69, 827–834. [Google Scholar] [CrossRef]
- Chowdhury, S.; Hassan, M.M.; Alam, M.; Sattar, S.; Bari, M.S.; Saifuddin, A.; Hoque, M.A. Antibiotic residues in milk and eggs of commercial and local farms at Chittagong, Bangladesh. Vet. World 2015, 8, 467. [Google Scholar] [CrossRef]
- Islam, A.; Saifuddin, A.; Al Faruq, A.; Islam, S.; Shano, S.; Alam, M.; Hassan, M.M. Antimicrobial residues in tissues and eggs of laying hens at Chittagong, Bangladesh. Int. J. One Health 2016, 2, 75–80. [Google Scholar] [CrossRef]
- Sattar, S.; Hassan, M.M.; Islam, S.; Alam, M.; Al Faruk, M.S.; Chowdhury, S.; Saifuddin, A. Antibiotic residues in broiler and layer meat in Chittagong district of Bangladesh. Vet. World 2014, 7, 7. [Google Scholar] [CrossRef]
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic use in agriculture and its consequential resistance in environmental sources: Potential public health implications. Molecules 2018, 23, 795. [Google Scholar] [CrossRef]
- Van den Bogaard, A.; London, N.; Driessen, C.; Stobberingh, E. Antibiotic resistance of faecal Escherichia coli in poultry, poultry farmers and poultry slaughterers. J. Antimicrob. Chemother. 2001, 47, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Mather, A.; Reid, S.; Maskell, D.; Parkhill, J.; Fookes, M.; Harris, S.; Brown, D.; Coia, J.; Mulvey, M.; Gilmour, M. Distinguishable epidemics of multidrug-resistant Salmonella Typhimurium DT104 in different hosts. Science 2013, 341, 1514–1517. [Google Scholar] [CrossRef] [PubMed]
- Al Amin, M.; Hoque, M.N.; Siddiki, A.Z.; Saha, S.; Kamal, M.M. Antimicrobial resistance situation in animal health of Bangladesh. Vet. World 2020, 13, 2713. [Google Scholar] [CrossRef]
- Hassan, M.M. Scenario of Antibiotic Resistance in Developing Countries. In Antimicrobial Resistance—A One Health Perspective; IntechOpen: London, UK, 2020. [Google Scholar]
- Frieden, T. Antibiotic Resistance Threats in the United States, 2013; Centers for Disease Control and Prevention, US Department of Health and Human Services: Atlanta, GA, USA, 2013; Volume 23, pp. 11–28.
- Lushniak, B.D. Surgeon general’s perspectives. Public Health Rep. 2014, 129, 314. [Google Scholar] [CrossRef]
- O’Neill, J. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations; UK Government: London, UK, 2016.
- Boeckel, T.; Brower, C.; Gilbert, M.; Grenfel, B.T.; Levin, S.A.; Robinson, T.P.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef]
- Alam, S.B.; Mahmud, M.; Akter, R.; Hasan, M.; Sobur, A.; Nazir, K.; Noreddin, A.; Rahman, T.; El Zowalaty, M.E.; Rahman, M. Molecular detection of multidrug resistant Salmonella species isolated from broiler farm in Bangladesh. Pathogens 2020, 9, 201. [Google Scholar] [CrossRef]
- Rahman, M.A.; Rahman, A.A.; Islam, M.A.; Alam, M.M. Multi–drug resistant Staphylococcus aureus isolated from milk, chicken meat, beef and egg in Bangladesh. Res. Agric. Livest. Fish. 2018, 5, 175–183. [Google Scholar] [CrossRef]
- Hoque, R.; Ahmed, S.M.; Naher, N.; Islam, M.A.; Rousham, E.K.; Islam, B.Z.; Hassan, S. Tackling antimicrobial resistance in Bangladesh: A scoping review of policy and practice in human, animal and environment sectors. PLoS ONE 2020, 15, e0227947. [Google Scholar] [CrossRef] [PubMed]
- Parvin, M.; Talukder, S.; Ali, M.; Chowdhury, E.H.; Rahman, M.; Islam, M. Antimicrobial resistance pattern of Escherichia coli isolated from frozen chicken meat in Bangladesh. Pathogens 2020, 9, 420. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Amin, K.B.; Ahaduzzaman, M.; Alam, M.; Faruk, M.S.; Uddin, I. Antimicrobial resistance pattern against E. coli and Salmonella in layer poultry. Res. J. Vet. Pract. 2014, 2, 30–35. [Google Scholar] [CrossRef]
- Mahmud, T.; Hassan, M.M.; Alam, M.; Khan, M.M.; Bari, M.S.; Islam, A. Prevalence and multidrug-resistant pattern of Salmonella from the eggs and egg-storing trays of retail markets of Bangladesh. Int. J. One Heath 2016, 2, 7–11. [Google Scholar] [CrossRef]
- Kalam, M.; Alim, M.; Shano, S.; Nayem, M.; Khan, R.; Badsha, M.; Mamun, M.; Al, A.; Hoque, A.; Tanzin, A.Z. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Poultry Drug and Feed Sellers in Bangladesh. Vet. Sci. 2021, 8, 111. [Google Scholar] [CrossRef] [PubMed]
- Hassan, M.M.; Kalam, M.; Alim, M.; Shano, S.; Nayem, M.; Khan, R.; Badsha, M.; Al Mamun, M.; Hoque, A.; Tanzin, A.Z. Knowledge, Attitude, and Practices on Antimicrobial Use and Antimicrobial Resistance among Commercial Poultry Farmers in Bangladesh. Antibiotics 2021, 10, 784. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Family Welfare. National Action Plan: Antimicrobial Resistance Containment in Bangladesh 2017–2022; Directorate General of Health Services: Dhaka, Bangladesh, 2017; pp. 1–12.
- Orubu, E.S.F.; Zaman, M.H.; Rahman, M.T.; Wirtz, V.J. Veterinary antimicrobial resistance containment in Bangladesh: Evaluating the national action plan and scoping the evidence on implementation. J. Glob. Antimicrob. Resist. 2020, 21, 105–115. [Google Scholar] [CrossRef]
- McCullough, A.; Rathbone, J.; Parekh, S.; Hoffmann, T.; Del Mar, C. Not in my backyard: A systematic review of clinicians’ knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2015, 70, 2465–2473. [Google Scholar] [CrossRef] [PubMed]
- Scherpenzeel, C.; Santman-Berends, I.; Lam, T. Veterinarians’ attitudes toward antimicrobial use and selective dry cow treatment in the Netherlands. J. Dairy Sci. 2018, 101, 6336–6345. [Google Scholar] [CrossRef]
- Smith, M.; King, C.; Davis, M.; Dickson, A.; Park, J.; Smith, F.; Currie, K.; Flowers, P. Pet owner and vet interactions: Exploring the drivers of AMR. Antimicrob. Resist. Infect. Control 2018, 7, 46. [Google Scholar] [CrossRef]
- Servia-Dopazo, M.; Taracido-Trunk, M.; Figueiras, A. Non-clinical factors determining the prescription of antibiotics by veterinarians: A systematic review. Antibiotics 2021, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Hardefeldt, L.Y.; Gilkerson, J.; Billman-Jacobe, H.; Stevenson, M.; Thursky, K.; Bailey, K.; Browning, G. Barriers to and enablers of implementing antimicrobial stewardship programs in veterinary practices. J. Vet. Intern. Med. 2018, 32, 1092–1099. [Google Scholar] [CrossRef] [PubMed]
- Adekanye, U.O.; Ekiri, A.B.; Galipó, E.; Muhammad, A.B.; Mateus, A.; La Ragione, R.M.; Wakawa, A.; Armson, B.; Mijten, E.; Alafiatayo, R. Knowledge, attitudes and practices of veterinarians towards antimicrobial resistance and stewardship in Nigeria. Antibiotics 2020, 9, 453. [Google Scholar] [CrossRef]
- Cattaneo, A.; Wilson, R.; Doohan, D.; LeJeune, J. Bovine veterinarians’ knowledge, beliefs, and practices regarding antibiotic resistance on Ohio dairy farms. J. Dairy Sci. 2009, 92, 3494–3502. [Google Scholar] [CrossRef]
- Wangmo, K.; Dorji, T.; Pokhrel, N.; Dorji, T.; Dorji, J.; Tenzin, T. Knowledge, attitude, and practice on antibiotic use and antibiotic resistance among the veterinarians and para-veterinarians in Bhutan. PLoS ONE 2021, 16, e0251327. [Google Scholar] [CrossRef]
- De Briyne, N.; Atkinson, J.; Pokludová, L.; Borriello, S.; Price, S. Factors influencing antibiotic prescribing habits and use of sensitivity testing amongst veterinarians in Europe. Vet. Rec. 2013, 173, 475. [Google Scholar] [CrossRef]
- Ekakoro, J.E.; Okafor, C.C. Antimicrobial use practices of veterinary clinicians at a veterinary teaching hospital in the United States. Vet. Anim. Sci. 2019, 7, 100038. [Google Scholar] [CrossRef]
- Fowler, H.; Davis, M.; Perkins, A.; Trufan, S.; Joy, C.; Buswell, M.; McElwain, T.; Moore, D.; Worhle, R.; Rabinowitz, P. Survey of veterinary antimicrobial prescribing practices, Washington State 2015. Vet. Rec. 2016, 179, 651. [Google Scholar] [CrossRef]
- Norris, J.M.; Zhuo, A.; Govendir, M.; Rowbotham, S.J.; Labbate, M.; Degeling, C.; Gilbert, G.L.; Dominey-Howes, D.; Ward, M.P. Factors influencing the behaviour and perceptions of Australian veterinarians towards antibiotic use and antimicrobial resistance. PLoS ONE 2019, 14, e0223534. [Google Scholar]
- Tompson, A.C.; Chandler, C.I.; Mateus, A.L.; O’Neill, D.G.; Chang, Y.-M.; Brodbelt, D.C. What drives antimicrobial prescribing for companion animals? A mixed-methods study of UK veterinary clinics. Prev. Vet. Med. 2020, 183, 105117. [Google Scholar] [CrossRef] [PubMed]
- Chapot, L.; Sarker, M.S.; Begum, R.; Hossain, D.; Akter, R.; Hasan, M.M.; Bupasha, Z.B.; Bayzid, M.; Salauddin, M.; Parvej, M.S. Knowledge, Attitudes and Practices Regarding Antibiotic Use and Resistance among Veterinary Students in Bangladesh. Antibiotics 2021, 10, 332. [Google Scholar] [CrossRef] [PubMed]
- Odoi, A.; Samuels, R.; Carter, C.N.; Smith, J. Antibiotic prescription practices and opinions regarding antimicrobial resistance among veterinarians in Kentucky, USA. PLoS ONE 2021, 16, e0249653. [Google Scholar] [CrossRef]
- Weese, J.; Giguère, S.; Guardabassi, L.; Morley, P.; Papich, M.; Ricciuto, D.; Sykes, J.E. ACVIM consensus statement on therapeutic antimicrobial use in animals and antimicrobial resistance. J. Vet. Intern. Med. 2015, 29, 487–498. [Google Scholar] [CrossRef]
| Variables | n (%) | |
|---|---|---|
| Respondent’s gender | Female | 73 (16.7) |
| Male | 363 (83.3) | |
| Age (years) | 18–25 | 159 (36.5) |
| 26–30 | 160 (36.7) | |
| 31–35 | 55 (12.6) | |
| 36–40 | 41 (9.4) | |
| 41 or more | 21 (4.82) | |
| Level of education | DVM | 284 (65.14) |
| Master’s/post-graduate | 152 (34.86) | |
| Experience (years) | Intern | 168 (38.5) |
| Up to 3 | 134 (30.7) | |
| 4–6 | 50 (11.5) | |
| 7 or more | 84 (19.3) | |
| Current workplace | Private | 136 (31.2) |
| Government hospital | 235 (53.9) | |
| Medicine/feed company | 65 (14.9) | |
| Training on antimicrobial use | Non-trained | 246 (56.4) |
| Trained | 190 (43.6) | |
| Items | Not at All N (%) | Poor N (%) | Medium N (%) | Good N (%) |
|---|---|---|---|---|
| Knowledge of different classes and generations of antibiotics | - | 6 (1.4) | 155 (35.6) | 275 (63.1) |
| Knowledge on interpreting microbiological/ laboratory results | 3 (0.7) | 57 (13.1) | 217 (49.8) | 159 (36.5) |
| Knowledge on choosing the correct antimicrobial | 1 (0.2) | 14 (3.2) | 194 (44.5) | 227 (52.1) |
| Knowledge on choosing the correct dose/dosage of antimicrobials | 2 (0.5) | 8 (1.8) | 144 (33.0) | 282 (64.7) |
| Knowledge on choosing routes of antimicrobial administration (oral vs. intravenous vs. topical) | - | 7 (1.6) | 102 (23.4) | 327 (75.0) |
| Knowledge on using a combination of antimicrobials if appropriate | 3 (0.7) | 33 (7.6) | 243 (55.7) | 157 (36.0) |
| Knowledge on planning the duration of the specific antimicrobial treatment | 3 (0.7) | 21 (4.8) | 189 (43.4) | 223 (51.2) |
| Knowledge on modifying/stopping antimicrobial treatments if required | 3 (0.7) | 35 (8.0) | 210 (48.2) | 188 (43.1) |
| Knowledge about reserve group of antimicrobials | 9 (2.1) | 61 (14.0) | 181 (41.5) | 185 (42.4) |
| Knowledge of critically important list of antimicrobials specified by World Health Organization (WHO) | 19 (4.4) | 76 (17.4) | 178 (40.8) | 163 (37.4) |
| Knowledge of National Action Plan for Antimicrobial Resistance (NAP AMR) | 15 (3.4) | 78 (17.9) | 211 (48.4) | 132 (30.3) |
| Knowledge on the mechanism and causes of AMR | 9 (2.1) | 37 (8.5) | 127 (29.1) | 263 (60.3) |
| Items | Strongly Disagree N (%) | Disagree N (%) | Agree N (%) | Strongly Agree N (%) |
|---|---|---|---|---|
| Antimicrobial resistance is a big threat for livestock and Poultry production | 2 (0.5) | 3 (0.7) | 47 (10.8) | 384 (88.1) |
| A single course of antibiotics can cause antimicrobial resistance | 12 (2.8) | 90 (20.6) | 170 (39.0) | 164 (37.6) |
| Irrational antibiotic use in animals leads to antibiotic resistance in humans | 2 (0.5) | 17 (3.9) | 152 (34.9) | 265 (60.8) |
| Antimicrobial resistance is a natural as well as anthropogenic phenomenon | 15 (3.4) | 99 (22.7) | 216 (49.5) | 106 (24.3) |
| Antimicrobial resistance will become a greater clinical problem in the future than it is today | - | 8 (1.8) | 77 (17.7) | 351 (80.5) |
| In recent years I have become more aware of the impacts of antimicrobial resistance | 2 (0.5) | 11 (2.5) | 149 (34.2) | 274 (62.8) |
| I find it hard to select the correct antimicrobial | 7 (1.6) | 80 (18.4) | 229 (52.5) | 120 (27.5) |
| I have enough sources of information about antimicrobials and their uses | 6 (1.4) | 81 (18.6) | 230 (52.8) | 119 (27.3) |
| New antimicrobials will be developed that will keep up with the problem of antimicrobial resistance | 15 (3.4) | 85 (19.5) | 226 (51.8) | 110 (25.2) |
| Restricting “priority antibiotics” for human use only | 18 (4.1) | 66 (15.1) | 157 (36.0) | 195 (44.7) |
| Items | Never N (%) | Rarely N (%) | Frequently N (%) | Regularly N (%) |
|---|---|---|---|---|
| How often do you give advice about the withdrawal period of antimicrobials? | 8 (1.8) | 75 (17.2) | 116 (26.6) | 237 (54.4) |
| How often do you give advice to the farmers to keep records of antimicrobials? | 16 (3.7) | 61 (14.0) | 153 (35.1) | 206 (47.3) |
| How often do you advise the farmer on administering antimicrobials through telephone conversations? | 51 (11.7) | 172 (39.5) | 127 (29.1) | 86 (19.7) |
| How often do you use antibiotics for prophylaxis? | 57 (13.1) | 154 (35.3) | 162 (37.2) | 63 (14.5) |
| How often do you use bacterial culture and susceptibility testing to select the most appropriate antibiotics for your treatment? | 115 (26.4) | 176 (40.4) | 99 (22.71) | 46 (10.6) |
| How often do you prescribe more than one antimicrobial in a single prescription? | 64 (14.7) | 200 (45.8) | 127 (29.1) | 45 (10.3) |
| How often do you advise the farmer about completing the full course of antimicrobials that you prescribed? | 2 (0.5) | 14 (3.2) | 68 (15.6) | 352 (80.7) |
| How often do you use antimicrobials due to the demand of farmers in a situation which does not require their use? | 146 (33.5) | 134 (30.7) | 93 (21.3) | 63 (14.5) |
| How often do you write prescriptions for antimicrobials to farmers who come to you without their animals? | 82 (18.8) | 163 (37.4) | 136 (31.2) | 55 (12.6) |
| How often do you use a higher dose of antimicrobials for rapid recovery of your patient? | 71 (16.3) | 196 (45.0) | 120 (27.5) | 49 (11.2) |
| How often do you use different alternatives of antimicrobials? | 12 (2.8) | 137 (31.4) | 217 (49.8) | 70 (16.1) |
| How often do you advise farmers about proper vaccination to reduce the use of antimicrobials? | 5 (1.2) | 20 (4.6) | 81 (18.6) | 330 (75.7) |
| Variables | Knowledge | Attitudes | Practices | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incorrect N (%) | Moderate N (%) | Correct N (%) | p | Unfavorable N (%) | Moderate N (%) | Favorable N (%) | p | Bad: N (%) | Moderate N (%) | Good: N (%) | p | ||
| Gender | Female | 7 (9.6) | 35 (48.0) | 31 (42.5) | 0.502 | 6 (8.2) | 37 (50.7) | 30 (41.1) | 0.472 | 4 (5.5) | 48 (65.8) | 21 (28.8) | 0.016 |
| Male | 28 (7.7) | 154 (42.4) | 181 (42.4) | 33 (9.1) | 208 (57.3) | 122 (33.6) | 70 (19.3) | 206 (56.8) | 87 (24.0) | ||||
| Age (years) | 18–25 | 12 (7.6) | 84 (52.8) | 63 (39.6) | 0.003 | 11 (6.9) | 92 (57.9) | 56 (35.2) | 0.720 | 24 (15.1) | 104 (65.4) | 31 (19.5) | 0.198 |
| 26–30 | 14 (8.8) | 70 (43.8) | 76 (47.5) | 15 (9.4) | 90 (56.3) | 55 (34.4) | 30 (18.8) | 91 (56.9) | 39 (24.4) | ||||
| 31–35 | 3 (5.5) | 22 (40.0) | 30 (54.6) | 6 (10.9) | 28 (50.9) | 21 (38.2) | 11 (20.0) | 28 (50.9) | 16 (29.1) | ||||
| 36–40 | 5 (12.2)) | 11 (26.8) | 25 (61.0) | 5 (12.2) | 26 (63.4) | 10 (24.4) | 8 (19.5) | 19 (46.3) | 14 (34.2) | ||||
| 41 or more | 1 (4.8) | 2 (9.5) | 18 (85.7) | 2 (9.5) | 9 (42.9) | 10 (47.6) | 1 (4.8) | 12 (57.1) | 8 (38.1) | ||||
| Level of education | Undergraduate | 25 (8.8) | 134 (47.2) | 125 (44.0) | 0.031 | 19 (6.7) | 167 (58.8) | 98 (34.5) | 0.059 | 49 (17.3) | 176 (62.0) | 59 (20.8) | 0.027 |
| Master’s/post-graduate | 10 (6.6) | 55 (36.2) | 152 (57.2) | 20 (13.2) | 78 ((51.3) | 54 (35.5) | 25 (16.5) | 78 (51.3) | 49 (32.2) | ||||
| Years of experience | Intern | 14 (8.3) | 88 (52.4) | 66 (39.3) | 0.018 | 13 (7.7) | 94 (56.0) | 61 (36.3) | 0.526 | 27 (16.1) | 110 (65.5) | 31 (18.5) | 0.124 |
| Up to 3 | 10 (7.5) | 59 (44.0) | 65 (48.5) | 13 (9.7) | 77 (57.5) | 44 (32.8) | 27 (20.2) | 73 (54.5) | 34 (25.4) | ||||
| 4–6 | 5 (10.0) | 17 (34.0) | 28 (56.0) | 6 (12.0) | 32 (64.0) | 12 (24.0) | 8 (16.0) | 28 (56.0) | 14 (28.0) | ||||
| 7 or more | 6 (7.1) | 25 (29.8) | 53 (63.1) | 7 (8.3) | 42 (50.0) | 35 (41.7) | 12 (14.3) | 43 (51.2) | 29 (34.5) | ||||
| Current workplace | Private practice | 11 (8.1) | 60 (44.1) | 65 (47.8) | 0.562 | 15 (11.0) | 72 (52.9) | 49 (36.0) | 0.196 | 29 (21.3) | 68 (50.0) | 39 (28.7) | 0.170 |
| Government hospital | 17 (7.2) | 97 (41.3) | 121 (51.5) | 21 (8.9) | 128 (54.5) | 86 (36.6) | 37 (15.7) | 146 (62.1) | 52 (22.1) | ||||
| Medicine/feed company | 7 (10.8) | 32 (49.2) | 65 (40.0) | 3 (4.6) | 45 (69.2) | 17 (26.2) | 8 (12.3) | 40 (61.5) | 17 (26.2) | ||||
| Training on AMU and AMR | No training | 23 (9.4) | 126 (51.2) | 97 (39.4) | 0.000 | 27 (11.0) | 138 (56.1) | 81 (32.9) | 0.201 | 39 (15.9) | 155 (63.0) | 52 (21.1) | 0.060 |
| Received training | 12 (6.3) | 63 (33.2) | 115 (60.5) | 12 (6.3) | 107 (56.3) | 71 (37.8) | 35 (18.4) | 99 (52.1) | 56 (29.5) | ||||
| Variables | Knowledge | Attitudes | Practices | |
|---|---|---|---|---|
| OR, 95%CI, p | OR, 95%CI, p | OR, 95%CI, p | ||
| Gender | Female | Ref | Ref | Ref |
| Male | 1.38, 0.79–2.38, 0.257 | 1.10, 0.63–1.93, 0.729 | 0.59, 0.32–1.06, 0.077 | |
| Age (years) | 18–25 | Ref | Ref | Ref |
| 26–30 | 0.92, 0.46–1.84, 0.814 | 1.20, 0.60–2.45, 0.608 | 0.66, 0.33–1.34, 0.252 | |
| 31–35 | 0.75, 0.25–2.30,0.620 | 0.44, 0.14–1.35, 0.152 | 1.38, 0.45–4.26, 0.570 | |
| 36–40 | 0.81, 0.20–3.20, 0.760 | 0.24, 0.06–0.97, 0.043 | 0.79, 0.20–3.15, 0.733 | |
| 41 or more | 2.71, 0.38–19.3, 0.319 | 0.29, 0.06–1.54, 0.147 | 0.81, 0.16–4.18, 0.799 | |
| Level of education | Undergraduate | Ref | Ref | Ref |
| Master’s/post-graduate | 1.23, 0.71–2.12, 0.465 | 1.16, 0.67–2.00, 0.598 | 1.33, 0.78–2.27, 0.295 | |
| Experience (years) | Intern | Ref | Ref | Ref |
| Up to 3 | 1.11, 0.52–2.38, 0.779 | 1.02, 0.47–2.21, 0.954 | 0.95, 0.44–2.04, 0.896 | |
| 4–6 | 2.03, 0.70–5.89, 0.193 | 1.69, 0.57–4.99, 0.345 | 0.79, 0.28–2.19, 0.645 | |
| 7 or more | 1.49, 0.41–5.50, 0.547 | 3.63, 0.95–13.95, 0.060 | 1.53, 0.40–5.87, 0.534 | |
| Current workplace | Medicine/feed company | Ref | Ref | Ref |
| Private practice | 1.48, 0.77–2.85, 0.244 | 0.96, 0.48–1.89, 0.899 | 0.83, 0.42–1.65, 0.599 | |
| Government hospital | 2.09, 1.06–4.10, 0.032 | 1.15, 0.58–2.28, 0.698 | 0.60, 0.30–1.19, 0.154 | |
| Training | No training | Ref | Ref | Ref |
| Trained | 1.92, 1.23–2.97, 0.004 | 2.09, 1.35–3.25, 0.001 | 0.76, 0.50–1.16, 0.024 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kalam, M.A.; Rahman, M.S.; Alim, M.A.; Shano, S.; Afrose, S.; Jalal, F.A.; Akter, S.; Khan, S.A.; Islam, M.M.; Uddin, M.B.; et al. Knowledge, Attitudes, and Common Practices of Livestock and Poultry Veterinary Practitioners Regarding the AMU and AMR in Bangladesh. Antibiotics 2022, 11, 80. https://doi.org/10.3390/antibiotics11010080
Kalam MA, Rahman MS, Alim MA, Shano S, Afrose S, Jalal FA, Akter S, Khan SA, Islam MM, Uddin MB, et al. Knowledge, Attitudes, and Common Practices of Livestock and Poultry Veterinary Practitioners Regarding the AMU and AMR in Bangladesh. Antibiotics. 2022; 11(1):80. https://doi.org/10.3390/antibiotics11010080
Chicago/Turabian StyleKalam, Md. Abul, Md. Sahidur Rahman, Md. Abdul Alim, Shahanaj Shano, Sharmin Afrose, Faruk Ahmed Jalal, Samira Akter, Shahneaz Ali Khan, Md. Mazharul Islam, Md Bashir Uddin, and et al. 2022. "Knowledge, Attitudes, and Common Practices of Livestock and Poultry Veterinary Practitioners Regarding the AMU and AMR in Bangladesh" Antibiotics 11, no. 1: 80. https://doi.org/10.3390/antibiotics11010080
APA StyleKalam, M. A., Rahman, M. S., Alim, M. A., Shano, S., Afrose, S., Jalal, F. A., Akter, S., Khan, S. A., Islam, M. M., Uddin, M. B., Islam, A., Magalhães, R. J. S., & Hassan, M. M. (2022). Knowledge, Attitudes, and Common Practices of Livestock and Poultry Veterinary Practitioners Regarding the AMU and AMR in Bangladesh. Antibiotics, 11(1), 80. https://doi.org/10.3390/antibiotics11010080












