Treating Critically Ill Patients Experiencing SARS-CoV-2 Severe Infection with Ig-M and Ig-A Enriched Ig-G Infusion
Abstract
1. Introduction
2. Results
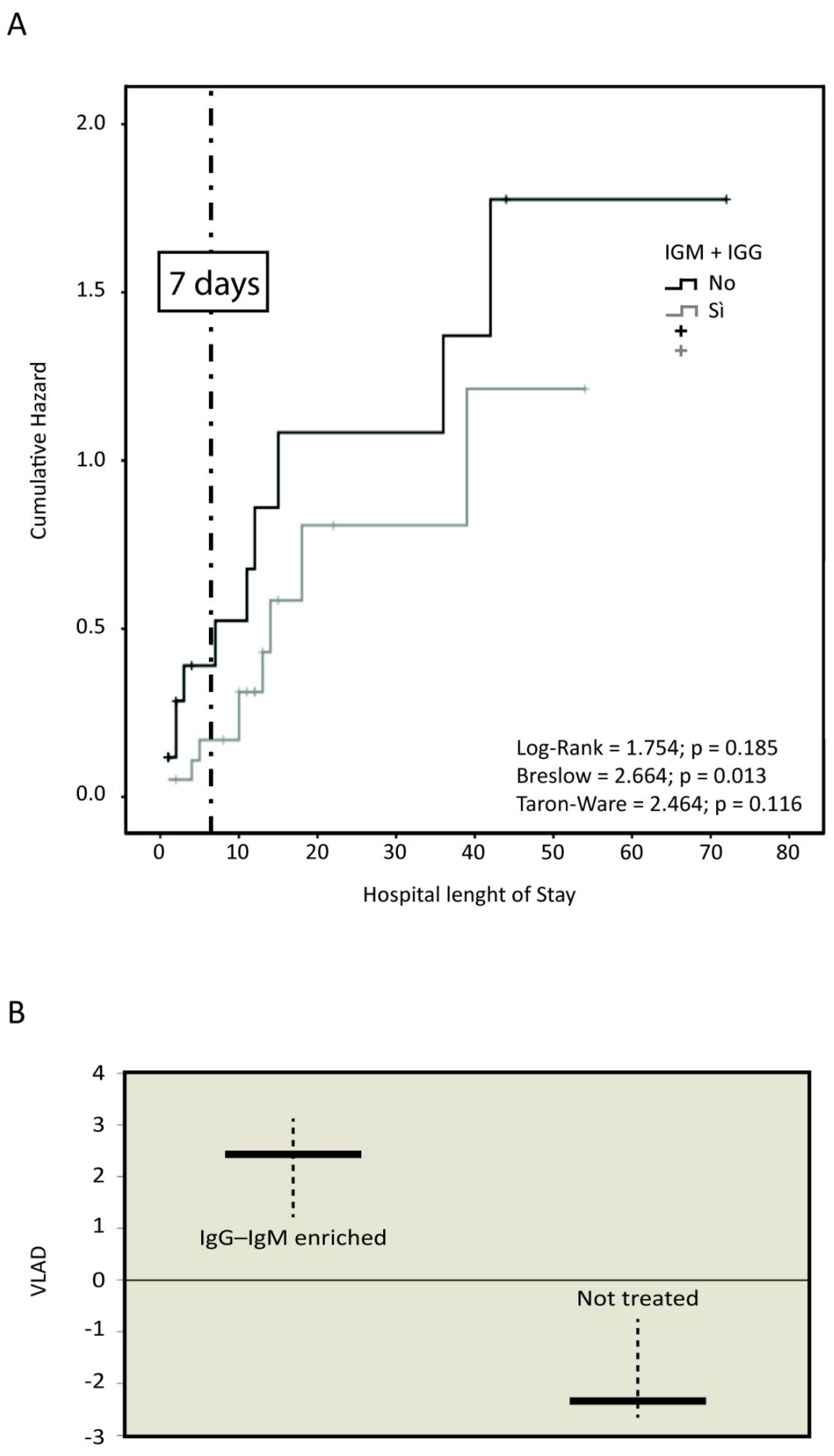
Mortality
3. Discussion
4. Materials and Methods
- age, history of the disease, including the length of stay (LOS), diagnostic and therapeutic procedure received until transfer to the ICU;
- clinical characteristics of the patients, including laboratory tests;
- comorbidities like hypertension, heart disease, COPD, neoplasms, diabetes, chronic renal failure, vascular tree diseases, chronic pathological or iatrogenic immunosuppression;
- sepsis-related Organ Failure Assessment (SOFA) score and Simplified Acute Physiology Score II (SAPS II);
- previous non-invasive positive pressure ventilation (NIPPV);
- the following parameters/events recorded during the staying in ICU were analyzed for our study (Table 2). Other parameters are reported in Tables S1 and S2 (Supplementary Materials);
- death;
- severe pulmonary embolization;
- continuous renal replacement therapy (CRRT) and its duration;
- echocardiographic signs of myocardial failure;
- hepatic insufficiency and alteration of hepatic cytolysis and cholestatic indices;
- variable life adjustment display (VLAD), a type of indicator used to measure healthcare quality and patient outcomes. VLAD allows to ascertain the difference between expected mortality (indicated by SMR (standardized mortality rate) derived from SAPS II and recorded mortality) (for the explanations see Supplementary Materials) [43,44].
4.1. Therapy
4.2. Primary Outcomes
4.3. Secondary Outcomes
- Infection rate and septic shock;
- Occurrence of severe pathological complications.
4.4. Statistical Analysis
4.5. Mortality
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- John Hopkins Coronavirus Resource Centre. Available online: https://coronavirus.jhu.edu/data/mortality (accessed on 17 May 2021).
- Parasher, A. COVID-19: Current understanding of its Pathophysiology, Clinical presentation and Treatment. Postgrad. Med. J. 2021, 97, 312–320. [Google Scholar] [CrossRef]
- Zumla, A.; Hui, D.S.; Azhar, E.I.; Memish, Z.A.; Maeurer, M. Reducing mortality from 2019-nCoV: Host-directed therapies should be an option. Lancet 2020, 395, e35–e36. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Mehta, P.; McAuley, D.F.; Brown, M.; Sanchez, E.; Tattersall, R.S.; Manson, J.J. COVID-19: Consider cytokine storm syndromes and immunosuppression. Lancet 2020, 395, 1033–1034. [Google Scholar] [CrossRef]
- Yang, Y.; Shen, C.; Li, J.; Yuan, J.; Wei, J.; Huang, F.; Wang, F.; Li, G.; Li, Y.; Xing, L.; et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J. Allergy Clin. Immunol. 2020, 146, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xu, J.; Zhou, C.; Wu, Z.; Zhong, S.; Liu, J.; Luo, W.; Chen, T.; Qin, Q.; Deng, P. Characterization of cytokine/chemokine profiles of severe acute respiratory syndrome. Am. J. Respir. Crit. Care Med. 2005, 171, 850–857. [Google Scholar] [CrossRef]
- Liu, Y.; Yan, L.M.; Wan, L.; Xiang, T.X.; Le, A.; Liu, J.M.; Peiris, M.; Poon, L.L.M.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef]
- Giamarellos-Bourboulis, E.J.; Netea, M.G.; Rovina, N.; Akinosoglou, K.; Antoniadou, A.; Antonakos, N.; Damoraki, G.; Gkavogianni, T.; Adami, M.E.; Katsaounou, P.; et al. Complex Immune Dysregulation in COVID-19 Patients with Severe Respiratory Failure. Cell Host Microbe 2020, 27, 992–1000. [Google Scholar] [CrossRef]
- Vaninov, N. In the eye of the COVID-19 cytokine storm. Nat. Rev. Immunol. 2020, 20, 277. [Google Scholar] [CrossRef]
- Quah, P.; Li, A.; Phua, J. Mortality rates of patients with COVID-19 in the intensive care unit: A systematic review of the emerging literature. Crit. Care 2020, 24, 285. [Google Scholar] [CrossRef]
- Nierhaus, A.; Berlot, G.; Kindgen-Milles, D.; Müller, E.; Girardis, M. Best-practice IgM- and IgA-enriched immunoglobulin use in patients with sepsis. Ann. Intensive Care 2020, 10, 132. [Google Scholar] [CrossRef]
- Carannante, N.; Fiorentino, G.; Corcione, A.; Di Sarno, R.; Spatarella, M.; Maturo, N.; Fragranza, F.; Di Micco, P. Administration of Immunoglobulins in SARS-CoV-2-Positive Patient Is Associated With Fast Clinical and Radiological Healing: Case Report. Front. Med. 2020, 7, 388. [Google Scholar] [CrossRef] [PubMed]
- Domizi, R.; Adrario, E.; Damiani, E.; Scorcella, C.; Carsetti, A.; Giaccaglia, P.; Casarotta, E.; Gabbanelli, V.; Pantanetti, S.; Lamura, E.; et al. IgM-enriched immunoglobulins (Pentaglobin) may improve the microcirculation in sepsis: A pilot randomized trial. Ann. Intensive Care 2019, 9, 135. [Google Scholar] [CrossRef]
- NIH. COVID-19 Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 17 May 2021).
- Shenoy, S. Coronavirus (COVID-19) sepsis: Revisiting mitoch ondrial dysfunction in pathogenesis, aging, inflammation, and mortality. Inflamm. Res. Off. J. Eur. Histamine Res. Soc. 2020, 69, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Seymour, C.W.; Kennedy, J.N.; Wang, S.; Chang, C.H.; Elliott, C.F.; Xu, Z.; Berry, S.; Clermont, G.; Cooper, G.; Gomez, H.; et al. Derivation, Validation, and Potential Treatment Implications of Novel Clinical Phenotypes for Sepsis. JAMA 2019, 321, 2003–2017. [Google Scholar] [CrossRef]
- Cao, W.; Liu, X.; Bai, T.; Fan, H.; Hong, K.; Song, H.; Han, Y.; Lin, L.; Ruan, L.; Li, T. High-Dose Intravenous Immunoglobulin as a Therapeutic Option for Deteriorating Patients With Coronavirus Disease 2019. Open Forum Infect. Dis. 2020, 7, ofaa102. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Cao, S.; Dong, H.; Li, Q.; Chen, E.; Zhang, W.; Yang, L.; Fu, S.; Wang, R. Effect of regular intravenous immunoglobulin therapy on prognosis of severe pneumonia in patients with COVID-19. J. Infect. 2020, 81, 318–356. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.-G.; Xie, S.-M.; Zhang, J.; Zheng, F.; Jiang, D.-X.; Li, K.-Y.; Zuo, Q.; Yan, Y.-S.; Liu, J.-Y.; Xie, Y.-L.; et al. Short-Term Moderate-Dose Corticosteroid Plus Immunoglobulin Effectively Reverses COVID-19 Patients Who Have Failed Low-Dose Therapy; Preprints, 2020. Available online: https://www.preprints.org/manuscript/202003.0065/v1 (accessed on 17 May 2021).
- Shao, Z.; Feng, Y.; Zhong, L.; Xie, Q.; Lei, M.; Liu, Z.; Wang, C.; Ji, J.; Liu, H.; Gu, Z.; et al. Clinical efficacy of intravenous immunoglobulin therapy in critical ill patients with COVID-19: A multicenter retrospective cohort study. Clin. Transl. Immunol. 2020, 9, e1192. [Google Scholar] [CrossRef]
- Conlon, N.; Keogan, M.; COVID-19 Evidence Review Group. Clinical Evidence for the use of Intravenous Immunoglobulin in the Treatment of COVID-19; National Centre for Pharmacoeconomics: Dublin, Ireland, 2020. [Google Scholar]
- Buda, S.; Riefolo, A.; Biscione, R.; Goretti, E.; Cattabriga, I.; Grillone, G.; Bacchi-Reggiani, L.; Pacini, D. Clinical experience with polyclonal IgM-enriched immunoglobulins in a group of patients affected by sepsis after cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2005, 19, 440–445. [Google Scholar] [CrossRef][Green Version]
- Cavazzuti, I.; Serafini, G.; Busani, S.; Rinaldi, L.; Biagioni, E.; Buoncristiano, M.; Girardis, M. Early therapy with IgM-enriched polyclonal immunoglobulin in patients with septic shock. Intensive Care Med. 2014, 40, 1888–1896. [Google Scholar] [CrossRef]
- Cui, J.; Wei, X.; Lv, H.; Li, Y.; Li, P.; Chen, Z.; Liu, G. The clinical efficacy of intravenous IgM-enriched immunoglobulin (pentaglobin) in sepsis or septic shock: A meta-analysis with trial sequential analysis. Ann. Intensive Care 2019, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Kakoullis, L.; Pantzaris, N.D.; Platanaki, C.; Lagadinou, M.; Papachristodoulou, E.; Velissaris, D. The use of IgM-enriched immunoglobulin in adult patients with sepsis. J. Crit. Care 2018, 47, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Norrby-Teglund, A.; Haque, K.N.; Hammarström, L. Intravenous polyclonal IgM-enriched immunoglobulin therapy in sepsis: A review of clinical efficacy in relation to microbiological aetiology and severity of sepsis. J. Intern. Med. 2006, 260, 509–516. [Google Scholar] [CrossRef]
- Carlone, G.; Torelli, L.; Maestro, A.; Zanon, D.; Barbi, E.; Maximova, N. Pentaglobin ® Efficacy in Reducing the Incidence of Sepsis and Transplant-Related Mortality in Pediatric Patients Undergoing Hematopoietic Stem Cell Transplantation: A Retrospective Study. J. Clin. Med. 2020, 9, 1592. [Google Scholar] [CrossRef]
- Barratt-Due, A.; Sokolov, A.; Gustavsen, A.; Hellerud, B.C.; Egge, K.; Pischke, S.E.; Lindstad, J.K.; Pharo, A.; Castellheim, A.; Thorgersen, E.B.; et al. Polyvalent immunoglobulin significantly attenuated the formation of IL-1β in Escherichia coli-induced sepsis in pigs. Immunobiology 2013, 218, 683–689. [Google Scholar] [CrossRef]
- Poynton, C.H.; Jackson, S.; Fegan, C.; Barnes, R.A.; Whittaker, J.A. Use of IgM enriched intravenous immunoglobulin (Pentaglobin) in bone marrow transplantation. Bone Marrow Transplant. 1992, 9, 451–457. [Google Scholar] [PubMed]
- Tsang, K.; Zhong, N.S. SARS: Pharmacotherapy. Respirology 2003, 8, S25–S30. [Google Scholar] [CrossRef] [PubMed]
- Ho, J.C.; Wu, A.Y.; Lam, B.; Ooi, G.C.; Khong, P.L.; Ho, P.L.; Chan-Yeung, M.; Zhong, N.S.; Ko, C.; Lam, W.K.; et al. Pentaglobin in steroid-resistant severe acute respiratory syndrome. Int. J. Tuberc. Lung Dis. Off. J. Int. Union Against Tuberc. Lung Dis. 2004, 8, 1173–1179. [Google Scholar]
- Wand, S.; Klages, M.; Kirbach, C.; Warszawska, J.; Meybohm, P.; Zacharowski, K.; Koch, A. IgM-Enriched Immunoglobulin Attenuates Systemic Endotoxin Activity in Early Severe Sepsis: A Before-After Cohort Study. PLoS ONE 2016, 11, e0160907. [Google Scholar] [CrossRef]
- Perico, L.; Benigni, A.; Casiraghi, F.; Ng, L.F.P.; Renia, L.; Remuzzi, G. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat. Rev. Nephrol. 2021, 17, 46–64. [Google Scholar] [CrossRef]
- Colantuoni, A.; Martini, R.; Caprari, P.; Ballestri, M.; Capecchi, P.L.; Gnasso, A.; Lo Presti, R.; Marcoccia, A.; Rossi, M.; Caimi, G. COVID-19 Sepsis and Microcirculation Dysfunction. Front. Physiol. 2020, 11, 747. [Google Scholar] [CrossRef]
- Grasselli, G.; Tonetti, T.; Protti, A.; Langer, T.; Girardis, M.; Bellani, G.; Laffey, J.; Carrafiello, G.; Carsana, L.; Rizzuto, C.; et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: A multicentre prospective observational study. Lancet Respir. Med. 2020, 8, 1201–1208. [Google Scholar] [CrossRef]
- Pentaglobin™ SmPC. Available online: https://farmaci.agenziafarmaco.gov.it/aifa/servlet/PdfDownloadServlet?pdfFileName=footer_000752_029021_RCP.pdf&sys=m0b1l3 (accessed on 17 May 2021).
- Ferrari, E.; Taillan, B.; Drai, E.; Morand, P.; Baudouy, M. Investigation of the thoracic aorta in cholesterol embolism by transoesophageal echocardiography. Heart 1998, 79, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Boero, R.; Pignataro, A.; Rollino, C.; Quarello, F. Do corticosteroids improve survival in acute renal failure due to cholesterol atheroembolism? Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transplant. Assoc. Eur. Ren. Assoc. 2000, 15, 441. [Google Scholar] [CrossRef]
- González, E.; Gutiérrez, E.; Galeano, C.; Chevia, C.; de Sequera, P.; Bernis, C.; Parra, E.G.; Delgado, R.; Sanz, M.; Ortiz, M.; et al. Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int. 2008, 73, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Fontana, J.; Vogt, A.; Hohenstein, A.; Vettermann, U.; Doroshenko, E.; Lammer, E.; Yard, B.A.; Hoeger, S. Impact of Steroids on the Inflammatory Response after Ischemic Acute Kidney Injury in Rats. Indian J. Nephrol. 2017, 27, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Shankar-Hari, M.; Spencer, J.; Sewell, W.A.; Rowan, K.M.; Singer, M. Bench-to-bedside review: Immunoglobulin therapy for sepsis—biological plausibility from a critical care perspective. Crit. Care 2012, 16, 206. [Google Scholar] [CrossRef]
- Foltran, F.; Baldi, I.; Bertolini, G.; Merletti, F.; Gregori, D. Monitoring the performance of intensive care units using the variable life-adjusted display: A simulation study to explore its applicability and efficiency. J. Eval. Clin. Pract. 2009, 15, 506–513. [Google Scholar] [CrossRef]
- Le Gall, J.R.; Lemeshow, S.; Saulnier, F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270, 2957–2963. [Google Scholar] [CrossRef] [PubMed]
| Variables | Group A n = 24 | Group B n = 23 | p-Value |
|---|---|---|---|
| Age (yrs.) | 59.5 (57–66) | 61(55–67) | 0.212 |
| SAPS II-score | 45 (38–59) | 46 (38–58) | 0.222 |
| SOFA-score | 9 (7–10) | 8 (5–11) | 0.174 |
| Pre-ICU-LOS (days) | 3 (1–5) | 4 (1–10.5) | 0.620 |
| ICU-LOS (days) | 15.5 (5–15.5) | 9 (5–11) | 0.045 |
| MV-length (days) | 12 (4–15) | 7 (5–9) | 0.045 |
| Urea (mg/dL) | 55 (40–109) | 48 (30–74) | 0.209 |
| Total bilirubin (mg/dL) | 0.9 (0.6–1.9) | 1 (0.8–1.7) | 0.529 |
| Ammonium (mg/dL) | 76 (57–109) | 72 (53–100) | 0.335 |
| Total diuresis (mg/dL) | 1.7 (1.2–2.2) | 1.7 (1.1–2.6) | 0.202 |
| PLT (103/mL) | 110 (75–275) | 105 (86–233) | 0.358 |
| LDH (mg/dL) | 525 (320–705) | 462 (272–563) | 0.478 |
| CPK (mg/dL) | 2239 (1140–2537) | 3467 (2228–4185) | 0.022 |
| D-Dimer μg/mL | 6485 (1400–11.000) | 10.7 (1.200–20.000) | 0.110 |
| IgG-pre (mg/dL) (range 7.5–15.6) | 10 (7–14.5) | 10.6 (6.8–14.6) | 0.233 |
| IgA-pre (mg/dL) (range 0.82–4.53) | 0.8 (0.7–3.1) | 0.9 (0.8–3) | 0.125 |
| IgM-pre (mg/dL) (range 0.46–3.04) | 0.5 (0.4–1.5) | 0.6 (0.4–1.6) | 0.276 |
| Variables | Group A n = 24 | Group B n = 23 | OR (95% CI) | p-Value |
|---|---|---|---|---|
| IDDM/NIDDM | 2 (8.3%) | 2 (8.7%) | 1 (0.2–7.9) | 1 |
| Diabetes | 2 (8.3%) | 2 (8.7%) | 1 (0.2–7.9) | 1 |
| Smoke | 2 (8.3%) | 0 | n.a. | 0.488 |
| COPD and other lung pathologies | 2 (8.3%) | 4 (17.4%) | 0.4 (0.1–2.6) | 0.416 |
| Chronic renal failure | 1 (4.2%) | 0 | n.a. | 1 |
| Chronic liver failure | 0 | 0 | n.a. | n.a. |
| Steroid therapy and immunosuppression | 0 | 2 (8.7%) | n.a. | 0.234 |
| Hypertension | 12 (50%) | 7 (33.3%) | ||
| CAD | 4(16.7%) | 1 (4.3%) | 4.7 (0.5–6.2) | 0.343 |
| Other cardiopathies | 2 (8.3%) | 2 (8.7%) | 0.9 (0.1–7.4) | 1 |
| Cerebral stroke | 1 (4.2%) | 0 | n.a. | 1 |
| Neoplasia | 1 (4.2%) | 0 | n.a. | 1 |
| Treatment | Group A n = 23 | Group B n = 24 | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Antiviral therapy (*) | ||||
| Hydroxychloroquine | 7 (29.2%) | 10 (43.5%) | 0.6 (0.2–1.9) | 0.530 |
| Lopinavir/ritonavir | 6 (25%) | 5 (21.7%) | 1.3 (0.3–5.1) | 1 |
| Steroids | 3 (12.5%) | 10 (43.5%) | 0.2 (0.1–0.9) | 0.043 |
| Azitromycin | 7 (29.2%) | 6 (26.1%) | 1.3 (0.3–4.6) | 1 |
| Event | Group A n = 24 | Group B n = 23 | OR (95% CI) | p-Value |
|---|---|---|---|---|
| Pulmonary embolism | 3 (12.5%) | 6 (26.1%) | 0.4 (0.2–1.8) | 0.277 |
| Acute kidney failure | 10 (41.7%) | 3 (13%) | 5.1 (1.2–23) | 0.043 |
| CRRT | 4 (16.7%) | 1 (4.3%) | 4.9 (0.5–48.4) | 0.185 |
| Acute liver failure | 10 (41.7%) | 5 (21.7) | 2.7 (0.8–10.2) | 0.197 |
| Acute cerebral stroke | 2 (8.3%) | 2 (8.7%) | 0.9 (0.1–7.5) | 1 |
| Sepsis | 5 (20.8%) | 9 (39.1%) | 0.6 (0.1–1.3) | 0.116 |
| Septic shock | 3 (12.5%) | 7 (21.7%) | 0.7 (0.2–5) | 0.045 |
| Deaths | 9 (37.5%) | 13 (56.5%) | 0.6 (0.2–0.8) | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corona, A.; Richini, G.; Simoncini, S.; Zangrandi, M.; Biasini, M.; Russo, G.; Pasqua, M.; Santorsola, C.; Gregorini, C.; Giordano, C. Treating Critically Ill Patients Experiencing SARS-CoV-2 Severe Infection with Ig-M and Ig-A Enriched Ig-G Infusion. Antibiotics 2021, 10, 930. https://doi.org/10.3390/antibiotics10080930
Corona A, Richini G, Simoncini S, Zangrandi M, Biasini M, Russo G, Pasqua M, Santorsola C, Gregorini C, Giordano C. Treating Critically Ill Patients Experiencing SARS-CoV-2 Severe Infection with Ig-M and Ig-A Enriched Ig-G Infusion. Antibiotics. 2021; 10(8):930. https://doi.org/10.3390/antibiotics10080930
Chicago/Turabian StyleCorona, Alberto, Giuseppe Richini, Sara Simoncini, Marta Zangrandi, Monica Biasini, Giuseppe Russo, Mauro Pasqua, Clemente Santorsola, Camilla Gregorini, and Chiara Giordano. 2021. "Treating Critically Ill Patients Experiencing SARS-CoV-2 Severe Infection with Ig-M and Ig-A Enriched Ig-G Infusion" Antibiotics 10, no. 8: 930. https://doi.org/10.3390/antibiotics10080930
APA StyleCorona, A., Richini, G., Simoncini, S., Zangrandi, M., Biasini, M., Russo, G., Pasqua, M., Santorsola, C., Gregorini, C., & Giordano, C. (2021). Treating Critically Ill Patients Experiencing SARS-CoV-2 Severe Infection with Ig-M and Ig-A Enriched Ig-G Infusion. Antibiotics, 10(8), 930. https://doi.org/10.3390/antibiotics10080930






