Abstract
Background: Antibiotic resistance is a worldwide public health problem, leading to longer hospital stays, raising medical costs and mortality levels. As physicians’ attitudes are key factors to antibiotic prescribing, this study sought to explore their differences between primary care and hospital settings. Methods: A survey was conducted between September 2011 and February 2012 in the center region of Portugal in the form of a questionnaire to compare hospital (n = 154) and primary care (n = 421) physicians’ attitudes and knowledge regarding antibiotic prescribing. Results: More than 70% of the attitudes were statistically different (p < 0.05) between hospital physicians (HPs) and primary care physicians (PCPs). When compared to PCPs, HPs showed higher agreement with antibiotic resistances being a public health problem and ascribed more importance to microbiological tests and to the influence of prescription on the development of resistances. On the other hand, PCPs tended to agree more regarding the negative impact of self-medication with antibiotics dispensed without medical prescription and the need for rapid diagnostic tests. Seven out of nine sources of knowledge’s usefulness were statistically different between both settings, with HPs considering most of the knowledge sources to be more useful than PCPs. Conclusions: Besides the efforts made to improve both antibiotic prescribing and use, there are differences in the opinions between physicians working in different settings that might impact the quality of antibiotic prescribing. In the future, these differences must be considered to develop more appropriate interventions.
1. Introduction
Antibiotic resistance is a worldwide public health problem, leading to longer hospital stays and raising medical costs and mortality levels [1,2,3,4,5]. Previous studies highlighted the role of the over-prescription and mis-prescription of antibiotics on the development of resistances [6,7,8,9,10,11]. Hence, promoting interventions to improve the antibiotic prescribing process is a key element to improving antibiotic use and diminishing resistances.
To improve the effectiveness of antimicrobial stewardship interventions, their design should be multifaceted, multidisciplinary and based on the characteristics of each specific setting [12,13,14]. However, prescribing is a complex process, usually affected by economic, demographic, clinical, cultural and social factors beyond evidence-based recommendations [6].
Attitudes are the key factors in the antibiotic prescribing process [13,15,16]. However, an in-depth understanding of how attitudes affect physicians’ clinical practice in different settings is needed. To our knowledge, there are no studies assessing the differences between attitudes and knowledge of hospital physicians (HPs) and primary care physicians (PCPs). Therefore, the aim of this study was to compare both the attitudes and knowledge between PCPs and HPs with regards to antibiotic prescribing.
2. Materials and Methods
2.1. Study Design, Population and Ethics Statement
A survey was conducted in Portugal’s Centre Regional Health Administration (ARS-Centro) (Population in 2011: ~1,737,059 people), from September 2011 to February 2012. Determinants of prescribing were assessed in all PCPs working in the National Health Service facilities of the ARS-Centro and hospital care physicians working in internal medicine departments within the hospitals of the ARS-Centro.
This study was approved by Portugal’s Centre Regional Health Administration (Permit No. 015650/2011), by the hospital’s administration and by the Portuguese Data Protection Authority (Comissão Nacional de Proteção de Dados/CNPD) (Permit No. 2886/2013). The personally addressed, reply-paid self-administered questionnaires were sent by post mail to PCPs up to four times to nonrespondents. In the case of HPs, the questionnaires were hand-delivered to the director of each hospital/medical service, who distributed them among the HPs. The answers were then collected by the administrative services of the department. The respondents did not receive any incentives. Nine hundred and fourteen questionnaires were delivered to PCPs and two hundred and twenty-seven questionnaires to HPs. All the data concerning PCPs’ knowledge and attitudes has been previously published [15].
2.2. Data Collection
All physicians were asked to fill a previously validated (published elsewhere [16,17]), two-page long questionnaire, divided into 5 sections:
- Instructions to complete the questionnaire;
- “Antibiotics and Resistance”: 17 statements regarding the knowledge and attitudes towards antibiotic prescribing, antibiotic use and antimicrobial resistance. To each of these statements, an attitude was attributed;
- “In the treatment of respiratory infections, how would you rate the usefulness of each of these sources of knowledge?”: 9 statements regarding the importance of having several sources of knowledge, which can help comprehend the sources of knowledge underlying antibiotic mis-prescription;
- Sociodemographic and professional data (age, gender, medical specialization, workplace and workflow);
- Open box for additional comments.
The measurement of the agreement with the questions included in Section 2 and Section 3 of the questionnaire was performed through a horizontal, continuous visual analog scale, 8 cm long and unnumbered [16]. Answers were converted into a range from zero (total disagreement) to ten (total agreement). Physicians confidentiality was guaranteed.
2.3. Statistical Analysis
As the variables did not follow a normal distribution, nonparametric tests were conducted. Differences in the results between HPs and PCPs were evaluated using the Mann–Whitney U test. Differences were established as statistically significant at p < 0.05. The statistical analysis was performed using SPSS 25 (SPSS Inc., Armonk, NY, USA) and MS Excel (Microsoft Corporation, Redmond, WA, USA) software.
2.4. Sensitivity Analysis
In order to assess whether the differences observed were influenced by the fact that some physicians reported to work on both settings, a sensitivity analysis was conducted, in which these physicians were excluded.
3. Results
The overall response rate was 47.8%: of the PCPs; 421 answers were obtained, which corresponded to an overall response rate of 46.1%; 124 of the HPs invited accepted to participate in the study, corresponding to an overall response rate of 54.6%.
The process of distributing and collecting the questionnaires is summed up in the Figure 1 below.
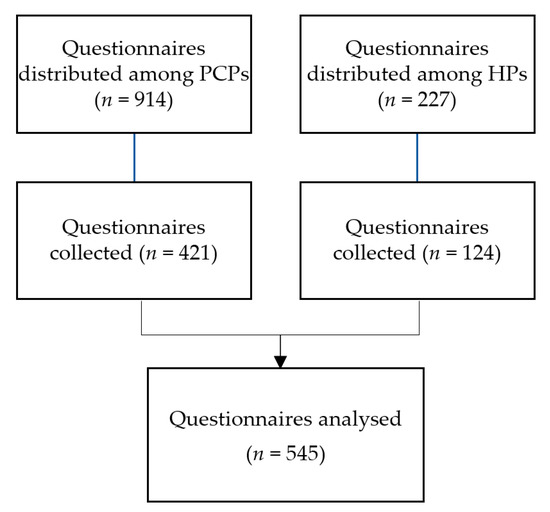
Figure 1.
Questionnaire distribution and collection flowchart.
3.1. Comparison of Sociodemographic and Professional Characteristics
Table 1 presents the comparisons between the sociodemographic characteristics of PCPs and HPs.

Table 1.
Sociodemographic and professional characteristics of both primary care and HPs.
3.2. Comparison of Knowledge and Attitudes towards Antibiotic Prescribing, Antibiotic Use and Antimicrobial Resistance
Table 2 describes and compares the results obtained for the 17 statements concerning antibiotic prescribing and resistances in both PCPs and HPs.

Table 2.
Differences in the attitudes and knowledge regarding antibiotic prescribing between PCPs and HPs (10—completely agree; 0—completely disagree).
Statistically significant results were obtained for the attitudes such as ignorance, responsibility of others, fear, complacency and indifference statements. Regarding ignorance, hospital physicians showed a higher agreement with resistance being a public health problem (S1), the importance of microbiological tests (S2) and the influence of prescriptions on the development of resistances (S4) compared to PCPs.
About the responsibility of others, HPs appear to be less convinced that the development of new antibiotics will solve the resistance problem (S5). On the other hand, PCPs tend to agree more regarding the negative impact of self-medication with antibiotics and dispense without medical prescription (S12 and S13). Furthermore, PCPs expressed a higher agreement about the need of rapid diagnostic tests (S3).
PCPs agreed more with the prescription of antibiotics in situations of fear and uncertainty (S7 and S8), as well as about having a complacent attitude with their patients (S10).
3.3. Comparison of the Usefulness of Different Sources of Knowledge
Table 3 describes and compares the results regarding the usefulness of different sources of knowledge between primary care and HPs.

Table 3.
Differences in the usefulness of sources of knowledge between primary care and HPs (10—completely agree; 0—completely disagree).
The differences found in the usefulness of sources of knowledge were all related to HPs considering some of the sources evaluated more helpful. Differences were found for clinical practice guidelines, documentation from the industry and from medical information officers, continuous educations, contribution of specialists, peers and the internet.
3.4. Sensitivity Analysis
Overall, after the sensitivity analysis, the differences between PCPs and HPs, have remained constant in almost all dimensions. However, the attitudes of fear (S7) and responsibility of others—other professionals (S13) were no longer significant. Furthermore, despite that the distribution remained the same as the one reported in Table 2, the differences between the importance attributed to Continuing Education Courses (S6) were no longer significant.
4. Discussion
This study shows that, besides an overall increasing of both apprehension and knowledge regarding health professionals and patients, there are still differences in the knowledge and attitudes that may be important to tackle in future healthcare interventions [18,19]. Furthermore, and considering that antibiotics can only be prescribed by physicians, these results provide a picture on the discrepancies between HPs and PCPs in terms of attitudes and knowledge concerning antibiotic resistances.
Regarding the attitudes underlying antibiotic prescribing, statistically significant differences were found for the responsibility of others, fear, indifference, complacency and ignorance in 12 of the 17 statements evaluated. These constitute somewhat unsettling results, as it reveals how different the attitudes concerning resistance between both settings can be.
Most HPs and PCPs agreed that antibiotic resistance is an important public health problem in their settings, reflecting the knowledge regarding antibiotic resistance is a distressing worldwide public health problem, increasing medical costs and mortality levels [3,4,5,20,21]. However, significant differences were found between HPs and PCPs, where the HPs showed higher agreement with the statement. This fact might be related with the challenges that HPs are facing to hamper and control the spread of resistant infections and their treatment in their setting. HPs also showed higher knowledge when considering the impact of a prescription to a patient as a factor underlying the possible appearance of resistance. Prior evidence revealed antibiotic prescriptions and use as selective pressure driving at this resistance, both on an individual [22] and community level [23].
The development of new antibiotics is also a point of discordance between PCPs and HPs: the first are more convinced that new antibiotics will be developed, and the literature shows promising lines of research [24]. However, the evidence shows the importance of conserving the molecules already available in practice, namely by using them wisely.
Significantly different answers were also obtained regarding the usefulness of the microbiology results in deciding which treatment to provide and the availability of the diagnostic techniques. The results of blood cultures help to reduce antibiotic use and narrow antibiotic therapy, thus reducing the costs [25], and there are several emerging potential technologies that can address the clinical needs [26]. Nevertheless, the differences found might be related to the availability of diagnostic techniques in time in the hospital setting, contrarywise to what is found in primary care settings, in which widespread testing is not feasible. Yet, in some specific diseases—namely, for pharyngitis—rapid antigen testing is recommended before an antibiotic prescription [27,28,29,30,31].
Differences were also found regarding the responsibility of patients or pharmacies, where PCPs agreed more that patients may manage to obtain antibiotics even without a prescription and/or self-medicate. This difference in physicians’ perceptions might be related to the proximity between primary care and community pharmacy practices. Nevertheless, the evidence is published about the dispense without a prescription [32,33] and self-medication with antibiotics [34], which leads to antibiotic misuse and resistances.
Fear about future bacterial resistances was also an attitude where physicians showed differences. PCPs agreed more about prescribing broad-spectrum antibiotics, in the case of diagnostic uncertainty or the impossibility of following-up patients. This might be explained with the unavailability of diagnostic tools to aid physicians’ diagnosis in primary care settings and is concordant with the previous research [6,35,36,37].
The statistically significant opinions in which physicians showed the least agreement were related to insistence from the patient, patient trust and time constraints. Again, differences were found, and PCPs seem to be more complacent with patients than the HPs. There is data indicating that both physicians consider patient satisfaction is crucial, so it is vital to manage patients’ expectations [9,38], namely with emphasis on precise clarifications. As a patient’s satisfaction is related to their belief of their understanding of their disease, the data shows the success of longer, patient-centered consultations with low antibiotic prescriptions [6,8,9,13,39,40]. Changing primary healthcare setting is hard, but patient empowerment and reinforcement during doctor–patient communication with a realist awareness of the patient’s expectations was reveal to be essential in reducing the antibiotic prescription [41,42].
HPs tended to show higher agreement about the usefulness of the sources of knowledge. With exception to the courses promoted and organized by the pharmaceutical industry and previous clinical practices, all the other sources of knowledge evaluated were considered more useful by HPs. The reasons behind these differences are complex to understand, but the need to be continuously updated in a hospital care context might be associated with the results found. Furthermore, as the HPs tended to be younger, they might feel the need to resort to other sources of knowledge to compensate for a lower clinical practice experience when compared to PCPs, who tend to be older. Perhaps younger doctors rely more on sources of information based on scientific evidence, while older doctors rely on their clinical experience.
Considering the fact that the vast majority of antibiotics are prescribed in primary care [43], the identification of the differences in the attitudes and the underlying behaviors in antibiotic prescribing between settings allows us to tailor antibiotic stewardship interventions. As inadequate antibiotic prescriptions are an important factor for antibiotic resistances development [18,19], and high rates of inadequate antimicrobial prescribing are noted in the context of primary care [44], identifying the dimensions in which PCPs are less aware is an essential strategy toward improving these issues. Furthermore, parallel to the results in this study, in which PCPs tend to attribute more responsibility to others than HPs, and less important than the issue of antibiotic resistances, some studies have shown that PCPs do not only give less importance to the issue of antibiotic resistances but also tend to not consider themselves particularly accountable about their roles in this issue [20,21,44]. Hence, raising awareness among PCPs to tackle antimicrobial resistances should be a priority.
This study is accompanied by some limitations. Despite the statistically significant differences in attitudes, we cannot assure it triggers different antibiotic prescribing practices between settings. Considering the geographical limitations, the low response rate and specific characteristics regarding physicians’ clinical practice and the Portuguese Health System, the extrapolation of the results to other countries might not be adequate, as it can compromise its external validity. Nevertheless, the internal validity has been assured, as the questionnaire has been previously validated [16,45]. The response rates obtained both with primary care and HPs are low when compared to similar studies [46,47,48]. However, low response rates among physicians is a recognized problem in survey research [49,50]. The fact that the questionnaires were sent by post mail to PCPs and hand-delivered to the director of each hospital/service, along with the differences in the geographical dispersion of physicians within the territory, might explain the slight discrepancy between the response rates. Still, the difference in only 8% between response rates constitutes a positive outcome in this study, as it results in a less-biased appraisal between both settings. Furthermore, at the time in which this survey was conducted, there were 4.5 physicians/1000 inhabitants, considering both the public and private sectors [51]. Considering the estimated population of the center region, we estimate that this survey is highly representative of the public sector physician population, as it included almost a third of the physicians of this region. Even though this study was conducted in 2011 to 2012, which can be considered a limitation, the data from this study remains relevant, as the attitudes are stable variables over time [20,21], and it still brings an important contribution to the knowledge on this topic.
5. Conclusions
To conclude, the results of the study revealed that there are differences in opinions between physicians working in hospital and primary care that might impact the quality of antibiotic prescribing. Therefore, interventions to improve the antibiotic prescription quality should be tailored to each setting, especially considering the more evident differences between primary care and HP attitudes (particularly, dimensions of fear, ignorance and responsibility to others) for a more effective tackling of this global concern.
Author Contributions
Conceptualization, A.F., F.R. and M.T.H.; data curation, A.T.R., F.R. and M.T.H.; formal analysis, A.T.R., J.C.F.N., M.E., A.F., F.R. and M.T.H.; funding acquisition, F.R. and M.T.H.; investigation, A.T.R., A.F., F.R. and M.T.H.; methodology, A.T.R., J.C.F.N., M.E., A.F., F.R. and M.T.H.; project administration, M.T.H.; writing—original draft, A.T.R. and writing—review and editing, J.C.F.N., M.E., A.F., F.R. and M.T.H. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the Foundation for Science & Technology (Fundação para a Ciência e Tecnologia—FCT), Institute of Biomedicine-iBiMED (UIDP/04501/2020) grant (UIDB/04501/2020) and by grant PTDC/SAU-ESA/105530/2008, from the Portuguese Ministry of Science & Education, co-financed by FEDER through the COMPETE Program, and by the research project PTDC/SAU-SER/31678/2017, supported by the operational program on competitiveness and internationalization (POCI) in its FEDER/FNR component, POCI-01-0145-FEDER-031678, and by the Foundation for Science and Technology in its state budget component (OE).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by approved by Portugal’s Centre Regional Health Administration (Permit No. 015650/2011), by the hospital’s administration and by the Portuguese Data Protection Authority (Comissão Nacional de Proteção de Dados/CNPD) (Permit No. 2886/2013).
Informed Consent Statement
The participation of the questionnaire was a volunteer and only the participants that agree to participate fulfill the questionnaire.
Acknowledgments
We thank Tânia Magalhães Silva (iBiMED/UA) for her collaboration on the revision of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses or interpretation of the data; in the writing of the manuscript or in the decision to publish the results.
References
- Livermore, D. Minimising antibiotic resistance. Lancet Infect. Dis. 2005, 5, 450–459. [Google Scholar] [CrossRef]
- Yewale, V. Antimicrobial resistance—A ticking bomb! Indian Pediatr. 2014, 51, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H. Inadequate antimicrobial treatment: An Important determinant of outcome for hospitalized patients. Clin. Infect. Dis. 2000, 31, 131–138. [Google Scholar] [CrossRef]
- Kandeel, A.; El-shoubary, W.; Hicks, L.A.; Fattah, M.A.; Dooling, K.L.; Lohiniva, A.L.; Ragab, O.; Galal, R.; Talaat, M. Patient Attitudes and Beliefs and Provider Practices Regarding Antibiotic Use for Acute Respiratory Tract Infections in Minya, Egypt. Antibiotics 2014, 292, 632–644. [Google Scholar] [CrossRef] [PubMed]
- Kollef, M.H. The importance of appropriate initial antibiotic therapy for hospital-acquired infections. Am. J. Med. 2003, 115, 582–584. [Google Scholar] [CrossRef]
- Ackerman, S.; Gonzales, R. The context of antibiotic overuse. Ann. Intern. Med. 2012, 147, 211–212. [Google Scholar] [CrossRef]
- McNulty, C.A.M. European Antibiotic Awareness Day 2012: General practitioners encouraged to TARGET antibiotics through guidance, education and tools. J. Antimicrob. Chemother. 2012, 67, 2543–2546. [Google Scholar] [CrossRef]
- Hart, A.; Pepper, G.; Gonzales, R. Balancing acts: Deciding for or against antibiotics in acute respiratory infections. J. Fam. Pract. 2016, 55, 320–325. [Google Scholar] [CrossRef]
- Ong, S.; Nakase, J.; Moran, G.; Karras, D.; Kuehnert, M.; Talan, D. Antibiotic Use for Emergency Department Patients With Upper Respiratory Infections: Prescribing Practices, Patient Expectations, and Patient Satisfaction. Ann. Emerg. Med. 2007, 50, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Wigton, R.S.; Darr, C.A.; Corbett, K.K.; Nickol, D.R.; Gonzales, R. How do community practitioners decide whether to prescribe antibiotics for acute respiratory tract infections? J. Gen. Intern. Med. 2008, 23, 1615–1620. [Google Scholar] [CrossRef]
- Dallas, A.; Van Driel, M.; Van De Mortel, T.; Magin, P. Antibiotic prescribing for the future: Exploring the attitudes of trainees in general practice. Br. J. Gen. Pract. 2014, 64, e561–e567. [Google Scholar] [CrossRef]
- Roque, F.; Teixeira-Rodrigues, A.; Breitenfeld, L.; Piñeiro-Lamas, M.; Figueiras, A.; Herdeiro, M.T. Decreasing antibiotic use through a joint intervention targeting physicians and pharmacists. Future Microbiol. 2016, 11, 877–886. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Vazquez, P.; Vazquez-Lago, J.M.; Figueiras, A. Misprescription of antibiotics in primary care: A critical systematic review of its determinants. J. Eval. Clin. Pract. 2012, 18, 473–484. [Google Scholar] [CrossRef]
- Arnold, S.; Straus, S. Interventions to improve antibiotic prescribing practices in ambulatory care. Evid.-Based Child Health A Cochrane Rev. J. 2006, 1, 623–690. [Google Scholar] [CrossRef]
- Rodrigues, A.T.; Ferreira, M.; Piñeiro-Lamas, M.; Falcão, A.; Figueiras, A.; Herdeiro, M.T. Determinants of physician antibiotic prescribing behavior: A 3 year cohort study in Portugal. Curr. Med. Res. Opin. 2016, 32, 949–957. [Google Scholar] [CrossRef]
- Teixeira Rodrigues, A.; Ferreira, M.; Roque, F.; Falcão, A.; Ramalheira, E.; Figueiras, A.; Herdeiro, M.T. Physicians’ attitudes and knowledge concerning antibiotic prescription and resistance: Questionnaire development and reliability. BMC Infect. Dis. 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- López-Vázquez, P.; Vázquez-Lago, J.M.; Gonzalez-Gonzalez, C.; Piñeiro-Lamas, M.; López-Durán, A.; Herdeiro, M.T.; Figueiras, A.; GREPHEPI Group. Development and validation of the knowledge and attitudes regarding antibiotics and resistance (KAAR-11) questionnaire for primary care physicians. J. Antimicrob. Chemother. 2016, 71, 2972–2979. [Google Scholar] [CrossRef]
- Zetts, R.M.; Stoesz, A.; Garcia, A.M.; Doctor, J.N.; Gerber, J.S.; Linder, J.A.; Hyun, D.Y. Primary care physicians’ attitudes and perceptions towards antibiotic resistance and outpatient antibiotic stewardship in the USA: A qualitative study. BMJ Open 2020, 10, 34983. [Google Scholar] [CrossRef]
- Zetts, R.M.; Garcia, A.M.; Doctor, J.N.; Gerber, J.S.; Linder, J.A.; Hyun, D.Y. Primary care physicians’ attitudes and perceptions towards antibiotic resistance and antibiotic stewardship: A national survey. Open Forum Infect. Dis. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, R.; Bartlett, J.; Besser, R.; Cooper, R.; Hickner, J.; Hoffman, J.; Sande, M. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: Background, specific aims, and methods. Ann. Intern. Med. 2001, 134, 479–486. [Google Scholar] [CrossRef]
- Lepape, A.; Monnet, D.L. Experience of European intensive care physicians with infections due to antibiotic-resistant bacteria, 2009. Eurosurveillance 2009, 14, 9–11. [Google Scholar] [CrossRef]
- Costelloe, C.; Metcalfe, C.; Lovering, A.; Mant, D.; Hay, A.D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ 2010, 340, 1120. [Google Scholar] [CrossRef] [PubMed]
- Derde, L.P.G.; Cooper, B.S.; Goossens, H.; Malhotra-Kumar, S.; Willems, R.J.L.; Gniadkowski, M.; Hryniewicz, W.; Empel, J.; Dautzenberg, M.J.D.; Annane, D.; et al. Interventions to reduce colonisation and transmission of antimicrobial-resistant bacteria in intensive care units: An interrupted time series study and cluster randomised trial. Lancet Infect. Dis. 2014, 14, 31–39. [Google Scholar] [CrossRef]
- The Pew Charitable Trusts Tracking the Pipeline of Antibiotics in Development. Available online: https://www.pewtrusts.org/en/research-and-analysis/articles/2016/12/tracking-the-pipeline-of-antibiotics-in-development (accessed on 24 May 2021).
- Dowell, S.F.; Marcy, S.M.; Phillips, W.R.; Gerber, M.A.; Schwartz, B. Principles of Judicious Use of Antimicrobial Agents for Pediatric Upper Respiratory tract infections. Pediatrics 1998, 101, 163–165. [Google Scholar] [CrossRef]
- O’Brien, K.L.; Dowell, S.F.; Schwartz, B.; Marcy, S.M.; Phillips, W.R.; Gerber, M.A. Cough illness/bronchitis—Principles of judicious use of antimicrobial agents. Pediatrics 1998, 101, 178–181. [Google Scholar] [CrossRef]
- Fraser, H.; Gallacher, D.; Achana, F.; Court, R.; Taylor-Phillips, S.; Nduka, C.; Stinton, C.; Willans, R.; Gill, P.; Mistry, H. Rapid antigen detection and molecular tests for group a streptococcal infections for acute sore throat: Systematic reviews and economic evaluation. Health Technol. Assess. 2020, 24, 1–232. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.F.; Pauchard, J.Y.; Hjelm, N.; Cohen, R.; Chalumeau, M. Efficacy and safety of rapid tests to guide antibiotic prescriptions for sore throat. Cochrane Database Syst. Rev. 2020, 2020. [Google Scholar] [CrossRef]
- Cohen, J.F.; Bertille, N.; Cohen, R.; Chalumeau, M. Rapid antigen detection test for group A streptococcus in children with pharyngitis. Cochrane Database Syst. Rev. 2016, 2016. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, R. Donowitz Acute Pharyngitis—Symptoms, Diagnosis and Treatment | BMJ Best Practice. Available online: https://bestpractice.bmj.com/topics/en-gb/5 (accessed on 27 January 2020).
- Carvalho, É.; Estrela, M.; Zapata-Cachafeiro, M.; Figueiras, A.; Roque, F.; Herdeiro, M.T. E-Health Tools to Improve Antibiotic Use and Resistances: A Systematic Review. Antibiotics 2020, 9, 505. [Google Scholar] [CrossRef]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Batista, A.D.; Rodrigues, D.A.; Figueiras, A.; Zapata-Cachafeiro, M.; Roque, F.; Herdeiro, M.T. Antibiotic Dispensation without a Prescription Worldwide: A Systematic Review. Antibiotics 2020, 9, 786. [Google Scholar] [CrossRef] [PubMed]
- Rosenstein, N.; Phillips, W.R.; Gerber, M.A.; Marcy, S.M.; Schwartz, B.; Dowell, S.F. The common cold—Principles of judicious use of antimicrobial agents. Pediatrics 1998, 101, 181–184. [Google Scholar]
- Linder, J.A.; Schnipper, J.L.; Tsurikova, R.; Volk, L.A.; Middleton, B. Self-reported familiarity with acute respiratory infection guidelines and antibiotic prescribing in primary care. Int. J. Qual. Health Care 2010, 22, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Lee, T.H.; Wong, J.G.X.; Lye, D.C.B.; Chen, M.I.C.; Loh, V.W.K.; Leo, Y.S.; Lee, L.K.; Chow, A.L.P. Medical and psychosocial factors associated with antibiotic prescribing in primary care: Survey questionnaire and factor analysis. Br. J. Gen. Pract. 2017, 67, e168–e177. [Google Scholar] [CrossRef]
- Allaire, A.-S.; Labrecque, M.; Giguère, A.; Gagnon, M.-P.; Grimshaw, J.; Légaré, F. Barriers and facilitators to the dissemination of DECISION+, a continuing medical education program for optimizing decisions about antibiotics for acute respiratory infections in primary care: A study protocol. Implement. Sci. 2011, 6, 3. [Google Scholar] [CrossRef]
- Pan, D.S.T.; Huang, J.H.; Lee, M.H.M.; Yu, Y.; Chen, M.I.C.; Goh, E.H.; Jiang, L.; Chong, J.W.C.; Leo, Y.S.; Lee, T.H.; et al. Knowledge, attitudes and practices towards antibiotic use in upper respiratory tract infections among patients seeking primary health care in Singapore. BMC Fam. Pract. 2016, 17, 1–9. [Google Scholar] [CrossRef]
- Ikai, H.; Morimoto, T.; Shimbo, T.; Imanaka, Y.; Koike, K. Impact of postgraduate education on physician practice for community-acquired pneumonia. J. Eval. Clin. Pract. 2012, 18, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Linder, J.A.; Singer, D.E. Desire for Antibiotics and Antibiotic Prescribing for Adults with Upper Respiratory Tract Infections. J. Gen. Intern. Med. 2003, 18, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Al-Homaidan, H.T.; Barrimah, I.E. Physicians’ knowledge, expectations, and practice regarding antibiotic use in primary health care. Int. J. Health Sci. 2018, 12, 18–24. [Google Scholar]
- Davey, P.; Pagliari, C.; Hayes, A. The patient’s role in the spread and control of bacterial resistance to antibiotics. Clin. Microbiol. Infect. 2002, 8, 43–68. [Google Scholar] [CrossRef]
- Llor, C.; Bjerrum, L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther. Adv. Drug Saf. 2014, 5, 229–241. [Google Scholar] [CrossRef] [PubMed]
- Shively, N.R.; Buehrle, D.J.; Clancy, C.J.; Decker, B.K. Prevalence of Inappropriate Antibiotic Prescribing in Primary Care Clinics within a Veterans Affairs Health Care System. Antimicrob. Agents Chemother. 2018, 62. [Google Scholar] [CrossRef]
- Terrível, J.; Terrível, J.; Teixeira Rodrigues, A.; Ferreira, M.; Ferreira, M.; Neves, C.; Neves, C.; Roque, F.; Roque, F.; Da Cruz e Silva, O.A.B.; et al. Conhecimento dos médicos relativo à prescrição de antibióticos e à resistência microbiana: Estudo piloto de comparação de questionário online vs papel. Rev. Epidemiol. e Control. Infecção 2014, 3, 93. [Google Scholar] [CrossRef]
- Labi, A.K.; Obeng-Nkrumah, N.; Bjerrum, S.; Aryee, N.A.A.; Ofori-Adjei, Y.A.; Yawson, A.E.; Newman, M.J. Physicians’ knowledge, attitudes, and perceptions concerning antibiotic resistance: A survey in a Ghanaian tertiary care hospital. BMC Health Serv. Res. 2018, 18, 126. [Google Scholar] [CrossRef] [PubMed]
- Wester, C.W.; Durairaj, L.; Evans, A.T.; Schwartz, D.N.; Husain, S.; Martinez, E. Antibiotic resistance: A survey of physician perceptions. Arch. Intern. Med. 2002, 162, 2210–2216. [Google Scholar] [CrossRef] [PubMed]
- Voidăzan, S.; Moldovan, G.; Voidăzan, L.; Zazgyva, A.; Moldovan, H. Knowledge, Attitudes And Practices Regarding The Use Of Antibiotics. Study on The General Population of Mureş County, Romania. Infect. Drug Resist. 2019, 12, 3385–3396. [Google Scholar] [CrossRef] [PubMed]
- Barclay, S.; Todd, C.; Finlay, I.; Grande, G.; Wyatt, P. Not another questionnaire! Maximizing the response rate, predicting non-response and assessing non-response bias in postal questionnaire studies of GPs. Fam. Pract. 2002, 19, 105–111. [Google Scholar] [CrossRef]
- Sibbald, B.; Addington-Hall, J.; Brenneman, D.; Freeling, P. Telephone versus postal surveys of general practitioners: Methodological considerations. Br. J. Gen. Pract. 1994, 44, 297–300. [Google Scholar]
- PORDATA PORDATA—Médicos e Outro Pessoal de Saúde por 100 mil Habitants. Available online: https://www.pordata.pt/Portugal/Médicos+e+outro+pessoal+de+saúde+por+100+mil+habitantes-639 (accessed on 29 April 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).