Adherence to National Antimicrobial Guidelines in Hospitalized Geriatric Patients with Community-Acquired Pneumonia: A Prospective Observational study in a Malaysian Hospital
Abstract
:1. Introduction
2. Results
2.1. Patients’ Baseline Characteristics
2.2. CAP Criteria for Hospital Admission and Patients’ Outcomes
2.3. Empiric Antibiotic Prescribed for CAP Patients
2.4. Patients’ Duration of CAP Hospitalization and Intravenous Antibiotic Use
2.5. Management of Therapeutic Failure
2.6. Criteria for Discharge
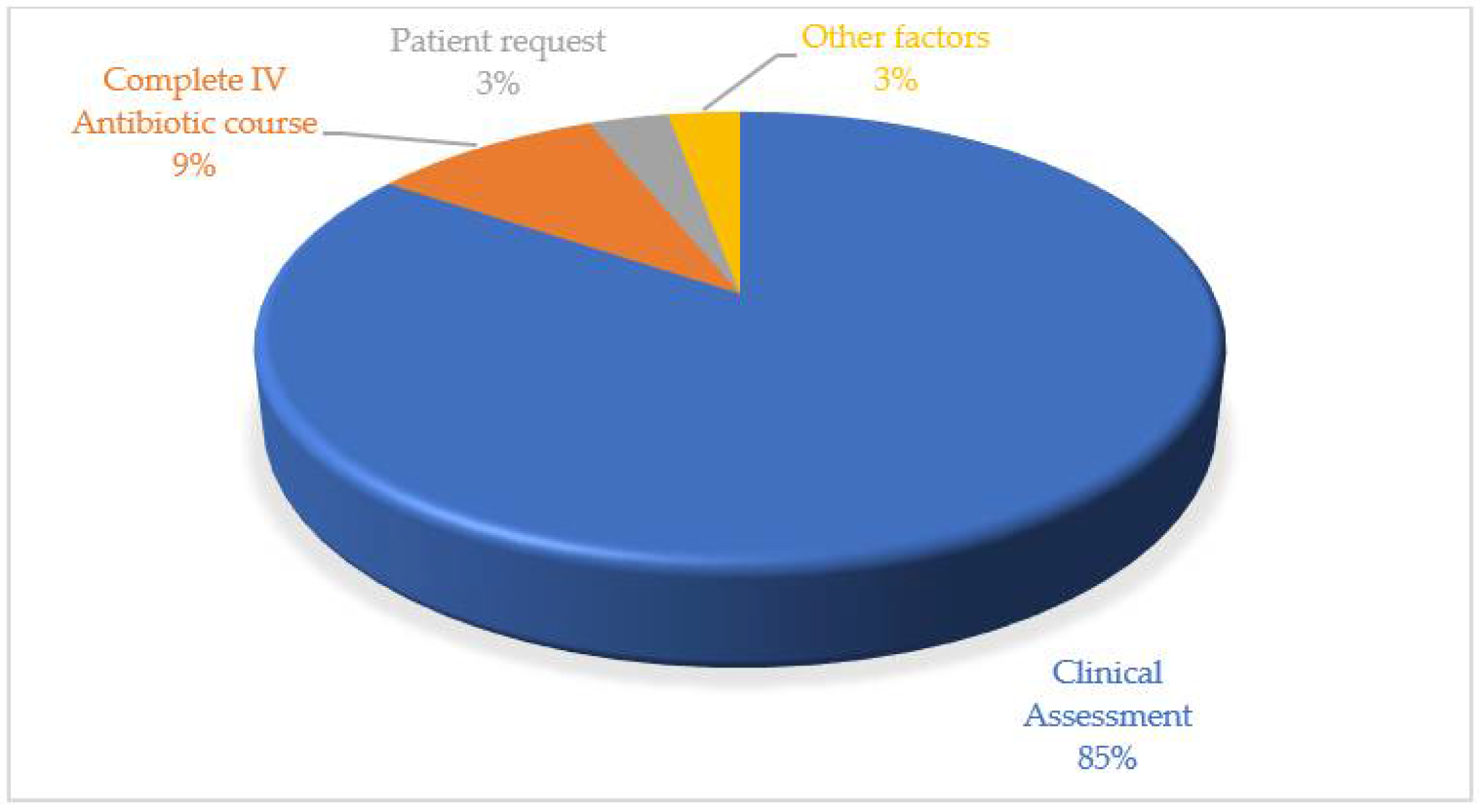
3. Discussion
4. Materials and Methods
4.1. Study Population and Settings
4.2. Instruments and Techniques for Data Collection
4.3. Ethical Consideration
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Oumei, H.; Xuefeng, W.; Jianping, L.; Kunling, S.; Rong, M.; Zhenze, C.; Deng, L.; Zhao, X.; Wei, W.; Hua, X.; et al. Etiology of Community-Acquired Pneumonia in 1500 Hospitalized Children. J. Med. Virol. 2018, 90, 421–428. [Google Scholar] [CrossRef]
- Lopardo, G.D.; Fridman, D.; Raimondo, E.; Albornoz, H.; Lopardo, A.; Bagnulo, H.; Goleniuk, H.; Sanabria, M.; Stamboulian, D. Incidence Rate of Community-Acquired Pneumonia in Adults: A Population-Based Prospective Active Surveillance Study in Three Cities in South America. BMJ Open 2018, 8, e019439. [Google Scholar]
- Su, M.; Wang, Q.; Li, D.; Wang, L.-L.; Wang, C.-Y.; Wang, J.-L.; Zhang, Q.; Du, L.-Y.; Liu, J.-Y.; Xie, G.-C. Prevalence and Clinical Characteristics of Hospitalized Children with Community-Acquired Mycoplasma Pneumoniae Pneumonia during 2017/2018, Chengde, China. Medicine 2021, 100, e23786. [Google Scholar] [CrossRef]
- Nair, G.B.; Niederman, M.S. Updates on Community Acquired Pneumonia Management in the ICU. Pharmacol. Ther. 2020, 217, 107663. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Coimbra, J.; Sarda, C.; Rello, J. Burden of Community-Acquired Pneumonia and Unmet Clinical Needs. Adv. Ther. 2020, 37, 1302–1318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gregersen, M.; Hansen, T.K.; Jørgensen, B.B.; Damsgaard, E.M. Frailty Is Associated with Hospital Readmission in Geriatric Patients: A Prognostic Study. Eur Geriatr. Med. 2020, 11, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.K.; Dang, D.A.; Kim, K.H.; Kartasasmita, C.; Kim, H.M.; Zhang, X.H.; Shafi, F.; Yu, T.W.; Ledesma, E.; Meyer, N. Burden of Hospitalized Childhood Community-Acquired Pneumonia: A Retrospective Cross-Sectional Study in Vietnam, Malaysia, Indonesia and the Republic of Korea. Hum. Vaccin Immunother. 2018, 14, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Xie, H.; Li, J.; Li, R.; Chen, W.; Huang, L.; Li, X.; Yan, P. The Prognostic Value of Geriatric Nutritional Risk Index in Elderly Patients with Severe Community-Acquired Pneumonia: A Retrospective Study. Medicine 2020, 99, e22217. [Google Scholar] [CrossRef] [PubMed]
- Tal, S. Length of Hospital Stay Among Oldest-Old Patients in Acute Geriatric Ward. Arch. Gerontol Geriatr. 2021, 94, 104352. [Google Scholar] [CrossRef] [PubMed]
- Eticha, E.M.; Gemechu, W.D. Adherence to Guidelines for Assessment and Empiric Antibiotics Recommendations for Community-Acquired Pneumonia at Ambo University Referral Hospital: Prospective Observational Study. Patient Prefer. Adherence 2021, 15, 467. [Google Scholar] [CrossRef]
- Li, H.Y.; Guo, Q.; Song, W.D.; Zhou, Y.P.; Li, M.; Chen, X.K.; Liu, H.; Peng, H.L.; Yu, H.Q.; Chen, X.; et al. Modified IDSA/ATS Minor Criteria for Severe Community-Acquired Pneumonia Best Predicted Mortality. Medicine 2015, 94, e1474. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. National Antimicrobial Guideline 2019, 3rd ed.; Selangor, Malaysia; Pharmaceutical Services Programme, Ministry of Health Malaysia: Putrajaya, Malaysia, 2019; Volume 64, pp. 509–519.
- Yavuz, B.G.; Çolak, S.; Guven, R.; Oner, M.; Bayramoglu, B. The Effectiveness of Geriatric Pneumonia Severity Index in Predicting Mortality. Int. J. Gerontol. 2021, 15, 73–77. [Google Scholar]
- Ahn, J.H.; Choi, E.Y. Expanded A-DROP score: A New Scoring System for the Prediction of Mortality in Hospitalized Patients with Community-Acquired Pneumonia. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef]
- Manabe, T.; Kotani, K.; Teraura, H.; Minami, K.; Kohro, T.; Matsumura, M. Characteristic Factors of Aspiration Pneumonia to Distinguish from Community-Acquired Pneumonia Among Oldest-Old Patients in Primary-Care Settings of Japan. Geriatrics 2020, 5, 42. [Google Scholar] [CrossRef]
- Yilmaz, H.E.B. Factors Affecting Mortality In Geriatric Patients Diagnosed With Community-Acquired Pneumonia Treated In Intensive Care Units. Turk. Geriatr. Derg. 2021, 24, 212–219. [Google Scholar] [CrossRef]
- Kolditz, M.; Ewig, S. Community-acquired pneumonia in adults. Dtsch Ärztebl. Int. 2017, 114, 838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Abri, S.S.; Al-Maashani, S.; Memish, Z.A.; Beeching, N.J. An Audit of Inpatient Management of Community-Acquired Pneumonia in Oman: A Comparison with Regional Clinical Guidelines. J. Infect. Public Health 2012, 5, 250–256. [Google Scholar] [CrossRef] [Green Version]
- Brett, J.; Lam, V.; Baysari, M.T.; Milder, T.; Killen, L.; Chau, A.M.; McMullan, B.; Harkness, J.; Marriott, D.; Day, R.O. Pneumonia Severity Scores and Prescribing Antibiotics for Community-Acquired Pneumonia at an Australian Hospital. J. Pharm. Pract. Res. 2013, 43, 97–100. [Google Scholar] [CrossRef]
- Wensing, M.; Grol, R.; Grimshaw, J. Improving Patient Care: The Implementation of Change in Health Care; John Wiley & Sons: Hoboken, NJ, USA, 2020. [Google Scholar]
- Guo, Q.; Li, H.-Y.; Zhou, Y.P.; Li, M.; Chen, X.-K.; Liu, H.; Peng, H.-L.; Yu, H.-Q.; Chen, X.; Liu, N.; et al. Compliance with the CURB-65 Score and the Consequences of Non-implementation. Int J. Tuberc Lung Dis. 2011, 15, 1697–1702. [Google Scholar] [CrossRef] [PubMed]
- Yoon, C.H.; Ritchie, S.R.; Duffy, E.J.; Thomas, M.G.; McBride, S.; Read, K.; Chen, R.; Humphrey, G. Impact of a Smartphone App on Prescriber Adherence to Antibiotic Guidelines in Adult Patients with Community Acquired Pneumonia or Urinary Tract Infections. PLoS ONE 2019, 14, e0211157. [Google Scholar]
- Lee, J.S.; Giesler, D.L.; Gellad, W.F.; Fine, M.J. Antibiotic Therapy for Adults Hospitalized with Community-Acquired Pneumonia: A Systematic Review. JAMA 2016, 315, 593–602. [Google Scholar] [CrossRef]
- Ball, P. The Clinical Development and Launch of Amoxicillin/Clavulanate for the Treatment of a Range of Community-Acquired Infections. Int. J. Antimicrob. Agents 2007, 30, 113–117. [Google Scholar] [CrossRef]
- White, A.R.; Kaye, C.; Poupard, J.; Pypstra, R.; Woodnutt, G.; Wynne, B. Augmentin®(amoxicillin/Clavulanate) in the Treatment of Community-Acquired Respiratory Tract Infection: A Review of the Continuing Development of an Innovative Antimicrobial Agent. J. Antimicrob. Chemother. 2004, 53, i3–i20. [Google Scholar] [CrossRef] [Green Version]
- Simonetti, A.; Garcia-Vidal, C.; Viasus, D.; García-Somoza, D.; Dorca, J.; Gudiol, F.; Carratala, J. Declining Mortality Among Hospitalized Patients with Community-Acquired Pneumonia. Clin. Microbiol Infect. 2016, 22, 567.e1. [Google Scholar] [CrossRef] [Green Version]
- Hariri, G.; Tankovic, J.; Boëlle, P.-Y.; Dubée, V.; Leblanc, G.; Pichereau, C.; Bourcier, S.; Bige, N.; Baudel, J.-L.; Galbois, A.; et al. Are Third-Generation Cephalosporins Unavoidable for Empirical Therapy of Community-Acquired Pneumonia in Adult Patients Who Require ICU Admission? A Retrospective Study. Ann. Intensive Care 2017, 7, 1–8. [Google Scholar] [CrossRef]
- Kollef, M.H.; Betthauser, K.D. New Antibiotics for Community-Acquired Pneumonia. Curr Opin Infect. Dis. 2019, 32, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Shakeel, S.; Iffat, W.; Qamar, A.; Ghuman, F.; Yamin, R.; Ahmad, N.; Ishaq, S.M.; Gajdacs, M.; Patel, I.; Jamshed, S. Pediatricians’ Compliance to the Clinical Management Guidelines for Community-Acquired Pneumonia in Infants and Young Children in Pakistan. Healthcare 2021, 9, 701. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File Jr, T.M.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in Adults. Clin. Infect. Dis. 2007, 44, S27–S72. [Google Scholar] [CrossRef] [PubMed]
- Cillóniz, C.; Rodríguez-Hurtado, D.; Torres, A. Characteristics and management of community-acquired pneumonia in the era of global aging. Med Sci. 2018, 6, 35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wunderink, R.G.; Waterer, G. Advances in the causes and management of community acquired pneumonia in adults. BMJ 2017, 358, j2471. [Google Scholar] [CrossRef] [PubMed]
- Kolditz, M.; Ewig, S.; Klapdor, B.; Schütte, H.; Winning, J.; Rupp, J.; Suttorp, N.; Welte, T.; Rohde, G. Community-Acquired Pneumonia as Medical Emergency: Predictors of Early Deterioration. Thorax 2015, 70, 551–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ito, A.; Ishida, T.; Tokumasu, H.; Washio, Y.; Yamazaki, A.; Ito, Y.; Tachibana, H. Prognostic Factors in Hospitalized Community-Acquired Pneumonia: A Retrospective Study of a Prospective Observational Cohort. BMC Pulm. Med. 2017, 17, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Baseline Characteristics | n (%) | |
|---|---|---|
| Age (years) | ||
| Mean ± SD | 73.5 ± 6.2 | |
| Median | 72 | |
| Range | 64–90 | |
| Height (cm, mean ± SD) | 164 ± 8.8 | |
| Weight (kg, mean ± SD) | 59.7 ± 12.4 | |
| Mean length of stay (days) | 4.5 ± 3.3 | |
| Gender | Male | 73 (60) |
| Female | 48 (40) | |
| Race | Malay | 89 (73) |
| Chinese | 17 (14) | |
| Indian | 15 (12) | |
| Residence | Urban | 56 (46) |
| Rural | 65 (54) | |
| Occupation | Employed | 2 (2) |
| Unemployed | 51 (42) | |
| Retired | 65 (54) | |
| Own business | 3 (2) | |
| Smoker | Yes | 46 (38) |
| No | 75 (62) | |
| Age > 65 years | 111 (91.7) |
| BMI | |
| Underweight | 11 (9) |
| Normal | 96 (79) |
| Overweight | 12 (10) |
| Obese | 2 (2) |
| SBP < 90 mmHg or DBP ≤ 60 mmHg | 27 (22.3) |
| LDH > 230 U/L | 75 (61.9) |
| Urea > 7 mmol/L | 50 (41.3) |
| Platelet count < 100 × 103 /mm3 | 15 (12.3) |
| Albumin < 3.5 g/dl | 57 (47.1) |
| Patients’ outcomes | |
| LOS: mean ± SD (days) | 4.5 ± 3.3 |
| Cure | 62 (51.2) |
| 30-day mortality | 13 (10.7) |
| ICU admission | 45 (37.1) |
| Readmitted within 30 days | 1 (0.8) |
| Scenario | Antibiotic Prescribed | ||
|---|---|---|---|
| Non-Severe Pneumonia | |||
| With no co-morbidities | Beta lactam + beta lactamase inhibitors (BLIs) * | Beta lactam + BLIs plus macrolide ** | Doxycycline |
| 11 (9%) | 3 (2.4%) | 1 (0.8%) | |
| With co-morbidities | Beta lactam+ BLI s plus macrolide | Ceftriaxone plus macrolide | Ceftriaxone |
| 21 (17.3%) | 13 (10.7%) | 8 (6.6%) | |
| Severe Pneumonia | |||
| With no co-morbidities | Beta lactam + BLIs | Beta lactam + BLIs plus macrolide | Beta lactam + BLIs plus doxycycline |
| 4 (3.3%) | 10 (8.2%) | 7 (5.7%) | |
| With co-morbidities | Beta lactam+ BLIs plus macrolide | Ceftriaxone plus macrolide | Ciprofloxacin |
| 26 (21.4%) | 12 (9.9%) | 5 (4.1%) | |
| Length of Hospitalization and IV Use of Antibiotics | No. of Days | Frequency (n; %) |
|---|---|---|
| Duration of hospital stay with non-severe pneumonia | < 3 days | 14 (11.5) |
| 3–5 days | 22 (18.1) | |
| 6–7 days | 5 (4.1) | |
| 8–10 days | 2 (1.6) | |
| Duration of hospital stay with severe pneumonia | < 5 days | 26 (21.4) |
| 6–7 days | 29 (23.9) | |
| 8–10 days | 15 (12.3) | |
| 11–14 days | 8 (6.6) | |
| Duration of IV antibiotics use in patients with severe pneumonia | < 3 days | 13 (10.7) |
| 3–5 days | 20 (16.5) | |
| 6–7 days | 39 (32.2) | |
| 8–10 days | 6 (4.9) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shakeel, S.; Muneswarao, J.; Abdul Aziz, A.; Yeong Le, H.; Abd. Halim, F.S.; Rehman, A.U.; Hussain, R. Adherence to National Antimicrobial Guidelines in Hospitalized Geriatric Patients with Community-Acquired Pneumonia: A Prospective Observational study in a Malaysian Hospital. Antibiotics 2021, 10, 1490. https://doi.org/10.3390/antibiotics10121490
Shakeel S, Muneswarao J, Abdul Aziz A, Yeong Le H, Abd. Halim FS, Rehman AU, Hussain R. Adherence to National Antimicrobial Guidelines in Hospitalized Geriatric Patients with Community-Acquired Pneumonia: A Prospective Observational study in a Malaysian Hospital. Antibiotics. 2021; 10(12):1490. https://doi.org/10.3390/antibiotics10121490
Chicago/Turabian StyleShakeel, Sadia, Jaya Muneswarao, Azrina Abdul Aziz, Heng Yeong Le, Fatin Syazwanni Abd. Halim, Anees Ur Rehman, and Rabia Hussain. 2021. "Adherence to National Antimicrobial Guidelines in Hospitalized Geriatric Patients with Community-Acquired Pneumonia: A Prospective Observational study in a Malaysian Hospital" Antibiotics 10, no. 12: 1490. https://doi.org/10.3390/antibiotics10121490
APA StyleShakeel, S., Muneswarao, J., Abdul Aziz, A., Yeong Le, H., Abd. Halim, F. S., Rehman, A. U., & Hussain, R. (2021). Adherence to National Antimicrobial Guidelines in Hospitalized Geriatric Patients with Community-Acquired Pneumonia: A Prospective Observational study in a Malaysian Hospital. Antibiotics, 10(12), 1490. https://doi.org/10.3390/antibiotics10121490







