Understanding Antimicrobial Resistance from the Perspective of Public Policy: A Multinational Knowledge, Attitude, and Perception Survey to Determine Global Awareness
Abstract
1. Introduction
2. Results
2.1. Participant Characteristics
2.2. Overall Knowledge, Attitude, and Perception Scores
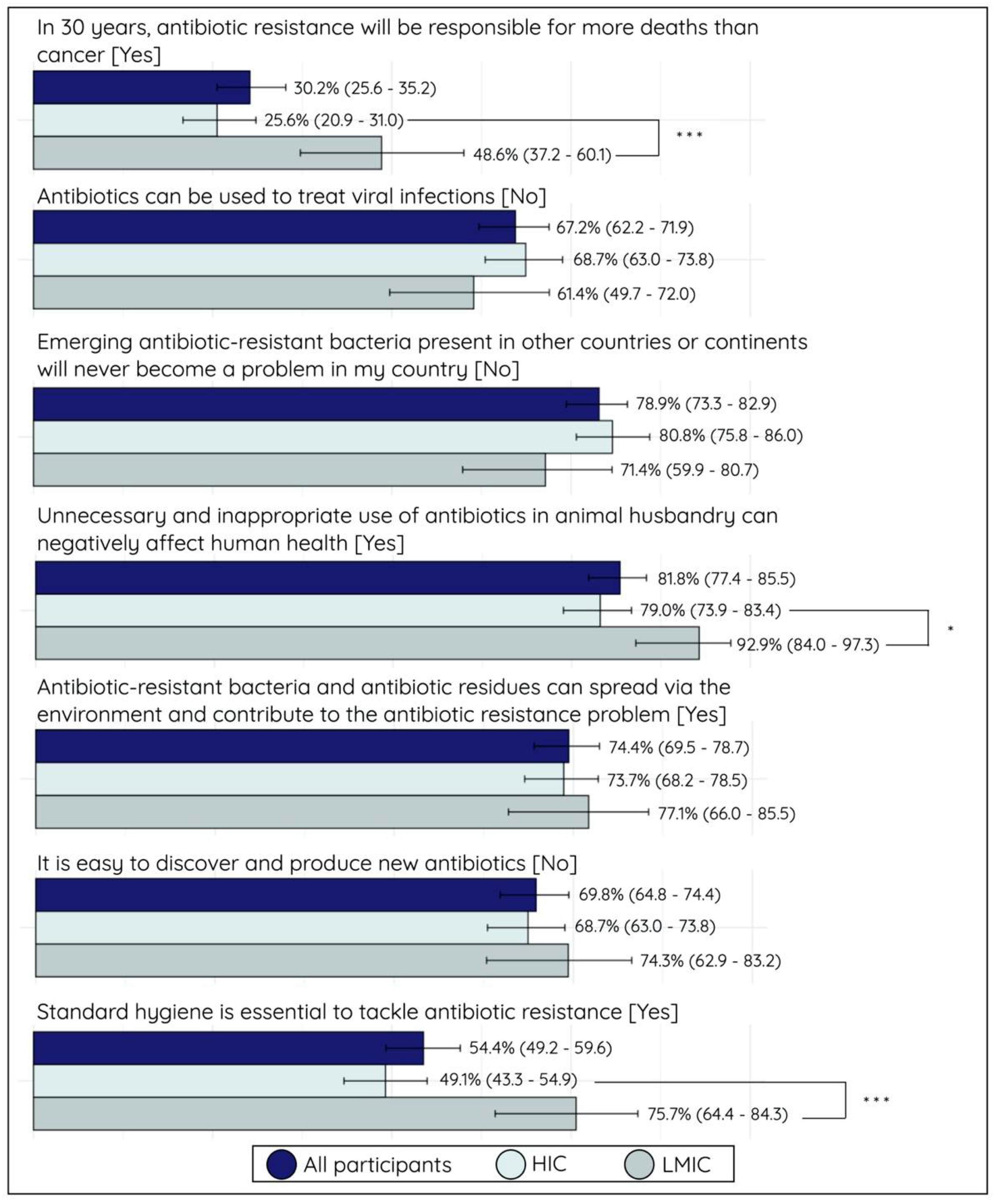
2.3. Knowledge Assessment
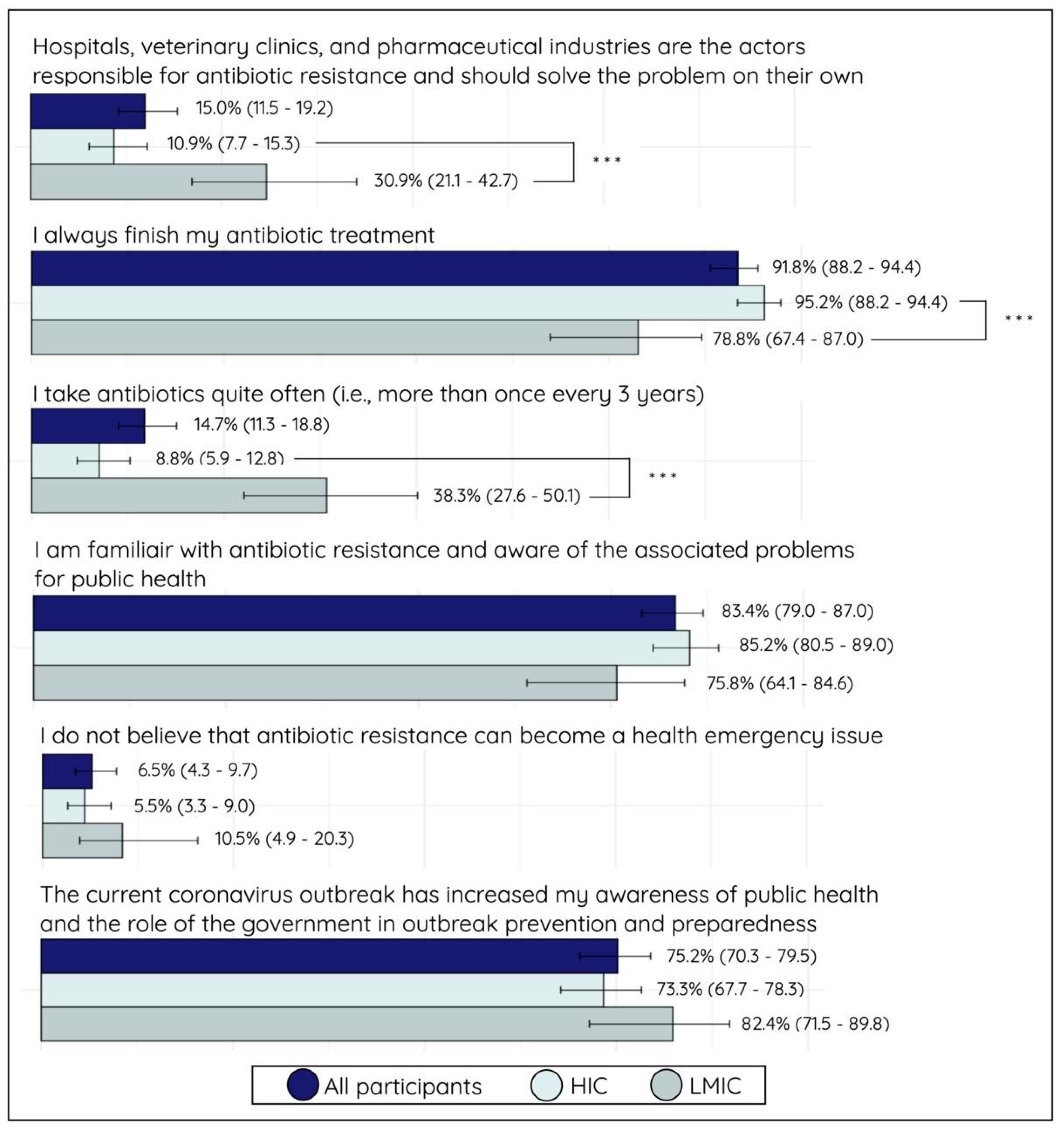
2.4. Attitude and Perception Assessment
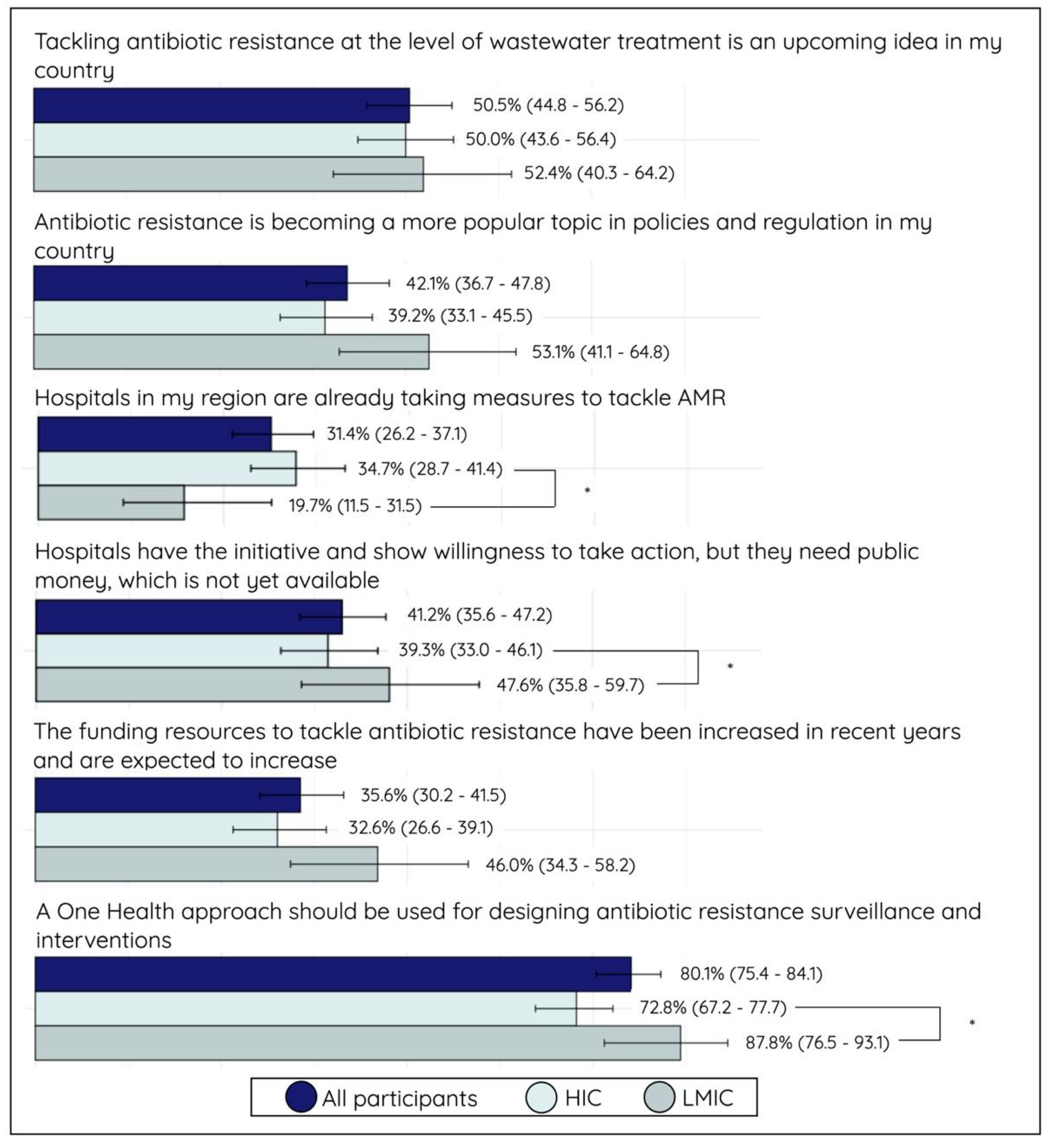
2.5. Political Activity and Involvement
3. Discussion
3.1. Personal Knowledge and Attitude towards Antimicrobial Resistance and Consumption
3.2. Participant’s Perspectives on Political Efforts to Address AMR
3.3. Implications for Public Health Policies
3.4. Remark on Research and Development (R&D)
3.5. Methodological Considerations
4. Materials and Methods
4.1. Design of Survey
4.2. Participant Recruitment
4.3. Data Collection and Transformation
4.4. Scoring System
4.5. Statistical Analysis
4.6. Ethical Statement
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Microbiology Society. Antimicrobial Resistance: The Next Pandemic? 2020. Available online: https://microbiologysociety.org/blog/antimicrobial-resistance-the-next-pandemic.html (accessed on 7 June 2021).
- Hsu, J. How COVID-19 is accelerating the threat of antimicrobial resistance. BMJ 2020, 369, m1983. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, H.; Wu, Y.; Zhang, L.; Yu, Z.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://apps.who.int/iris/handle/10665/193736 (accessed on 30 June 2021).
- World Health Organization; Food and Agriculture Organization of the United Nations (FAO); World Organisation for Animal Health (OIE). Monitoring Global Progress on Antimicrobial Resistance: Tripartite AMR Country Self-Assessment Survey (TRACCS) 2019–2020: Global Analysis Report; WHO Press: Geneva, Switzerland, 2021. [Google Scholar]
- Mendelson, M.; Matsoso, M.P. The World Health Organization Global Action Plan for antimicrobial resistance. S. Afr. Med. J. 2015, 105, 325. [Google Scholar] [CrossRef] [PubMed]
- United Nations. High-Level Interactive Dialogue on Antimicrobial Resistance (29 April 2021)|General Assembly of the United Nations. 2021. Available online: https://www.un.org/pga/75/antimicrobial-resistance/ (accessed on 30 June 2021).
- Lu, J.; Sheldenkar, A.; Lwin, M.O. A decade of antimicrobial resistance research in social science fields: A scientometric review. Antimicrob. Resist. Infect. Control 2020, 9, 178. [Google Scholar] [CrossRef] [PubMed]
- Miethke, M.; Pieroni, M.; Weber, T.; Brönstrup, M.; Hammann, P.; Halby, L.; Arimondo, P.B.; Glaser, P.; Aigle, B.; Bode, H.B.; et al. Towards the sustainable discovery and development of new antibiotics. Nat. Rev. Chem. 2021, 5, 726–749. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.X.; Hubbard-Lucey, V.M.; Tang, J. Immuno-oncology drug development goes global. Nat. Rev. Drug Discov. 2019, 18, 899–900. [Google Scholar] [CrossRef]
- Årdal, C.; Lacotte, Y.; Ploy, M.-C. Financing Pull Mechanisms for Antibiotic-Related Innovation: Opportunities for Europe. Clin. Infect. Dis. 2020, 71, 1994–1999. [Google Scholar] [CrossRef] [PubMed]
- Tangcharoensathien, V.; Sattayawutthipong, W.; Kanjanapimai, S.; Kanpravidth, W.; Brown, R.; Sommanustweechai, A. Antimicrobial resistance: From global agenda to national strategic plan, Thailand. Bull. World Health Organ. 2017, 95, 599–603. [Google Scholar] [CrossRef] [PubMed]
- Oliver, T.R. The politics of public health policy. Annu. Rev. Public Health 2006, 27, 195–233. [Google Scholar] [CrossRef]
- Adolph, C.; Amano, K.; Bang-Jensen, B.; Fullman, N.; Wilkerson, J. Pandemic Politics: Timing State-Level Social Distancing Responses to COVID-19. J. Health Politics-Policy Law 2021, 46, 211–233. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.R.; Chua, A.Q.; Tan, S.T.; Tam, C.C.; Hsu, L.Y.; Legido-Quigley, H. Combating Antimicrobial Resistance in Singapore: A Qualitative Study Exploring the Policy Context, Challenges, Facilitators, and Proposed Strategies. Antibiotics 2019, 8, 201. [Google Scholar] [CrossRef] [PubMed]
- Van Wijk, M.; Naing, S.; Franchy, S.D.; Heslop, R.T.; Lozano, I.N.; Vila, J.; Ballesté-Delpierre, C. Perception and knowledge of the effect of climate change on infectious diseases within the general public: A multinational cross-sectional survey-based study. PLoS ONE 2020, 15, e0241579. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Durrance-Bagale, A.; Mateus, A.; Sultana, Z.; Hasan, R.; Hanefeld, J. What are the barriers to implementing national antimicrobial resistance action plans? A novel mixed-methods policy analysis in Pakistan. Health Policy Plan. 2020, 35, 973–982. [Google Scholar] [CrossRef]
- European Commission; Directorate General for Health; Food Safety; Kantar Public. Special Eurobaromter 478: Anti-Microbial Resistance; LU Publications Office: Brussels, Belgium, 2018; Available online: https://data.europa.eu/doi/10.2875/92205 (accessed on 22 September 2021).
- Belachew, S.A.; Hall, L.; Selvey, L.A. Non-prescription dispensing of antibiotic agents among community drug retail outlets in Sub-Saharan African countries: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control 2021, 10, 1–15. [Google Scholar] [CrossRef]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Hadi, M.A.; Karami, N.A.; Al-Muwalid, A.S.; Al-Otabi, A.; Al-Subahi, E.; Bamomen, A.; Mohamed, M.M.; Elrggal, M.E. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): A cross-sectional survey in Makkah Province, Saudi Arabia. Int. J. Infect. Dis. 2016, 47, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Kamata, K.; Tokuda, Y.; Gu, Y.; Ohmagari, N.; Yanagihara, K. Public knowledge and perception about antimicrobials and antimicrobial resistance in Japan: A national questionnaire survey in 2017. PLoS ONE 2018, 13, e0207017. [Google Scholar] [CrossRef] [PubMed]
- Vallin, M.; Polyzoi, M.; Marrone, G.; Rosales-Klintz, S.; Wisell, K.T.; Lundborg, C.S. Knowledge and Attitudes towards Antibiotic Use and Resistance—A Latent Class Analysis of a Swedish Population-Based Sample. PLoS ONE 2016, 11, e0152160. [Google Scholar] [CrossRef]
- Mazińska, B.; Strużycka, I.; Hryniewicz, W. Surveys of public knowledge and attitudes with regard to antibiotics in Poland: Did the European Antibiotic Awareness Day campaigns change attitudes? PLoS ONE 2017, 12, e0172146. [Google Scholar] [CrossRef]
- Guillemot, D.; Varon, E.; Bernède, C.; Weber, P.; Henriet, L.; Simon, S.; Laurent, C.; Lecoeur, H.; Carbon, C. Reduction of Antibiotic Use in the Community Reduces the Rate of Colonization with Penicillin G--Nonsusceptible Streptococcus pneumoniae. Clin. Infect. Dis. 2005, 41, 930–938. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Santiago, V.H.; Davey, P.G.; Nathwani, D.; Marwick, C.A.; Guthrie, B. Changes in resistance among coliform bacteraemia associated with a primary care antimicrobial stewardship intervention: A population-based interrupted time series study. PLoS Med. 2019, 16, e1002825. [Google Scholar] [CrossRef]
- Van Katwyk, S.R.; Grimshaw, J.M.; Nkangu, M.; Nagi, R.; Mendelson, M.; Taljaard, M.; Hoffman, S.J. Government policy interventions to reduce human antimicrobial use: A systematic review and evidence map. PLoS Med. 2019, 16, e1002819. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC) and Organisation for Economic Cooperation and Development (OECD). Antimicrobial Resistance: Tackling the Burden in the European Union. 2019. Available online: https://www.oecd.org/health/health-systems/AMR-Tackling-the-Burden-in-the-EU-OECD-ECDC-Briefing-Note-2019.pdf (accessed on 10 February 2021).
- Dat, V.Q.; Toan, P.K.; van Doorn, H.R.; Thwaites, C.L.; Nadjm, B. Purchase and use of antimicrobials in the hospital sector of Vietnam, a lower middle-income country with an emerging pharmaceuticals market. PLoS ONE 2020, 15, e0240830. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Library of AMR National Action Plans. 2021. Available online: https://www.who.int/teams/surveillance-prevention-control-AMR/national-action-plan-monitoring-evaluation/library-of-national-action-plans (accessed on 10 February 2021).
- WAAW 2020 Highlights Myanmar. Available online: https://www.who.int/southeastasia/news/events/world-antibiotic-awareness-week-18-24-november-2020/waaw-2020-highlights-myanmar (accessed on 9 October 2021).
- Baekkeskov, E.; Rubin, O.; Munkholm, L.; Zaman, W. Antimicrobial Resistance as a Global Health Crisis. Oxf. Res. Encycl. Politics 2020. [Google Scholar] [CrossRef]


| Complete Dataset % (N) | HICs % (N) | LMICs % (N) | Fisher Exact | |
|---|---|---|---|---|
| Total | 351 | 80.1% (281) | 19.9% (70) | |
| Top 3 nationalities A | NLD 48.7% (171) | NLD 60.9% (171) | MMR 48.6% (34) | |
| ESP 27.6% (97) | ESP 34.5% (97) | IND 15.7% (11) | ||
| MMR 9.7% (34) | AUS 1.4% (4) | NGA 12.9% (9) | ||
| Gender | ||||
| Female | 51.9% (182) | 40.8% (15) | 45.7% (32) | 0.252 |
| Male | 46.4% (163) | 44.5% (125) | 54.3% (38) | |
| Undisclosed | 1.7% (6) | 2.1% (6) | 0.0% (0) | |
| Age | ||||
| Mean ± standard deviation | 49.3 ± 13.3 | 52.2 ± 12.0 | 37.8 ± 12.3 | |
| Median [IQR] | 52.0 [21.5–62.5] | 55 [46.5–63.5] | 33 [23.3–42.8] | |
| Age group | ||||
| <40 | 26.8% (94) | 16.4% (46) | 68.6% (49) | <0.001 *** |
| 40–60 | 51.0% (179) | 57.3% (161) | 25.7% (18) | |
| >60 | 22.2% (78) | 26.3% (74) | 5.7% (4) | |
| Position duration | ||||
| <1 year | 7.7% (27) | 8.2% (23) | 5.7% (4) | <0.001 *** |
| 1–3 years | 30.2% (106) | 33.5% (94) | 17.1% (12) | |
| 3–5 years | 17.1% (60) | 12.5% (35) | 35.7% (25) | |
| 5–10 years | 19.7% (69) | 19.2% (54) | 21.4% (15) | |
| >10 years | 25.4% (89) | 26.7% (75) | 20.0% (14) | |
| Educational background | ||||
| Master/PhD | 44.7% (157) | 39.5% (111) | 65.7% (46) | <0.001 *** |
| Bachelor | 40.7% (143) | 42.7% (120) | 32.9% (23) | |
| Lower levels | 14.0% (49) | 17.1% (48) | 1.4% (1) | |
| Unknown | 0.6% (2) | 0.7% (2) | 0.0% (0) | |
| Expertise | ||||
| Scientific | 46.4% (163) | 42.7% (120) | 61.4% (43) | 0.008 ** |
| Other background | 53.6% (188) | 57.3% (161) | 38.6% (27) | |
| Living condition | ||||
| (Sub)urban | 62.7% (220) | 54.1% (152) | 97.1% (68) | <0.001 *** |
| Rural | 37.0% (130) | 45.6% (128) | 2.9% (2) | |
| Unknown | 0.3% (1) | 0.4% (1) | 0.0% (0) | |
| Role | ||||
| Government | 86.3% (303) | 97.2% (273) | 42.9% (30) | <0.001 *** |
| Non-government | 12.8% (45) | 2.1% (6) | 55.7% (39) | |
| Unknown | 0.9% (3) | 0.7% (2) | 1.4% (1) | |
| Role (detailed) | ||||
| Municipal and regional | 52.1% (183) | 64.1% (180) | 4.3% (3) | <0.001 *** |
| Province | 18.2% (64) | 22.4% (63) | 1.4% (1) | |
| National | 7.1% (25) | 4.6% (13) | 17.1% (12) | |
| Non-government and unknown | 22.5% (79) | 8.9% (25) | 77.1% (54) |
| All Participants | HICs | LMICs | Significance a | |
|---|---|---|---|---|
| Personal knowledge | ||||
| Means ± standard deviation | 5.95 ± 2.82 | 5.81 ± 2.79 | 6.43 ± 3.57 | 0.053 |
| Median [inter quartile range] | 6.43 [3.57] | 6.55 [2.87] | 7.14 [3.57] | 0.044 * |
| Personal attitude and perception (AP) | ||||
| Means ± standard deviation | 6.99 ± 2.55 | 7.31 ± 2.38 | 5.70 ± 2.80 | <0.001 *** |
| Median [inter quartile range] | 7.50 [2.50] | 7.50 [2.50] | 5.83 [4.58] | <0.001 *** |
| Political KAP | ||||
| Means ± standard deviation | 2.88 ± 2.21 | 2.84 ± 2.16 | 3.04 ± 2.14 | 0.529 |
| Median [inter quartile range] | 2.31 [3.08] | 2.31 [3.08] | 2.69 [3.37] | 0.676 |
| Variable | N | Good Score A % (N) | aOR 95% CI | p-Value | Fair Score A % (N) | aOR 95% CI | p-Value |
|---|---|---|---|---|---|---|---|
| 351 | 41.3% (156) | 74.1% (260) | |||||
| Gender B | |||||||
| Female | 182 | 44.0% (88) | ref | 72.5% (132) | ref | ||
| Male | 163 | 44.2% (72) | 1.06 [0.66–1.69] | 0.805 | 69.9% (114) | 0.96 [0.57–1.64] | 0.892 |
| Age group B | |||||||
| <40 | 94 | 41.5% (39) | ref | 71.3% (67) | ref | ||
| 40–60 | 179 | 49.2% (88) | 2.12 [1.11–4.04] | 0.023 | 77.1% (138) | 1.76 [0.85–3.64] | 0.125 |
| >60 | 78 | 37.2% (29) | 2.03 [0.91–4.52] | 0.080 | 60.3% (47) | 1.68 [0.70–4.01] | 0.243 |
| Country class B | |||||||
| HIC | 281 | 42.4% (119) | ref | 70.5% (198) | ref | ||
| LMIC | 70 | 52.9% (37) | 1.97 [0.84–4.62] | 0.117 | 77.1% (54) | 1.47 [0.52–4.10] | 0.467 |
| Nationality C | |||||||
| The Netherlands | 171 | 43.3% (73) | ref | 64.9% (111) | ref | ||
| Spain | 97 | 39.2% (38) | 0.44 [0.23–0.86] | 0.017 | 78.4% (76) | 1.07 [0.51–2.25] | 0.856 |
| Myanmar | 34 | 26.5% (9) | 0.65 [0.22–1.92] | 0.432 | 64.7% (22) | 1.39 [0.42–4.64] | 0.593 |
| Duration B | |||||||
| <3 years | 133 | 45.1% (60) | 71.4% (95) | ref | |||
| 3–10 years | 129 | 44.2% (57) | 0.86 [0.50–1.48] | 0.593 | 72.1% (93) | 0.90 [0.48–1.67] | 0.728 |
| >10 years | 89 | 43.8% (39) | 0.66 [0.35–1.21] | 0.178 | 71.9% (64) | 0.65 [0.32–1.33] | 0.239 |
| Education B | |||||||
| Master and PhD | 157 | 54.8% (86) | ref | 79.6% (125) | ref | ||
| Bachelor | 143 | 41.3% (59) | 0.61 [0.37–0.99] | 0.045 | 75.5% (108) | 0.86 [0.48–1.53] | 0.597 |
| Lower levels | 49 | 22.5% (11) | 0.25 [0.11–0.57] | <0.001 | 38.8% (19) | 0.16 [0.07–0.37] | <0.001 |
| Expertise B | |||||||
| Scientific | 163 | 55.2% (90) | ref | 83.4% (136) | ref | ||
| Other | 188 | 35.1% (66) | 0.49 [0.31–0.79] | 0.004 | 61.7% (116) | 0.34 [0.19–0.56] | <0.001 |
| Living condition B | |||||||
| (Sub)urban | 220 | 48.2% (106) | ref | 75.9% (167) | ref | ||
| Rural | 130 | 37.7% (49) | 0.79 [0.47–1.31] | 0.357 | 64.6% (84) | 0.73 [0.41–1.30] | 0.287 |
| Occupation B | |||||||
| Government | 303 | 37.3% (113) | 71.6% (217) | ref | |||
| Non-government | 45 | 44.4% (20) | 0.56 [0.23–1.34] | 0.190 | 71.1% (32) | 0.52 [0.18–1.46] | 0.213 |
| Role (detailed) D | |||||||
| Regional | 183 | 38.3% (70) | 66.1% (121) | ref | |||
| Province | 64 | 50.0% (32) | 1.27 [0.69–2.36] | 0.441 | 76.6% (49) | 1.28 [0.62–2.68] | 0.504 |
| National | 25 | 56.0% (14) | 1.50 [0.57–3.95] | 0.409 | 80.0% (20) | 1.28 [0.40–4.12] | 0.680 |
| Non-government | 79 | 50.6% (40) | 1.10 [0.51–2.39] | 0.804 | 78.5% (62) | 1.27 [0.47–3.44] | 0.644 |
| Variable | N | Good AP A % (N) | aOR 95% CI | p-Value | Fair AP A % (N) | aOR 95% CI | p-Value |
|---|---|---|---|---|---|---|---|
| 351 | 41.6% (146) | 83.8% (294) | |||||
| Gender B | |||||||
| Female | 182 | 62.1% (113) | ref | 81.3% (148) | ref | ||
| Male | 163 | 55.2% (90) | 0.76 [0.47–1.21] | 0.246 | 85.9% (140) | 1.57 [0.80–3.09] | 0.194 |
| Age group B | |||||||
| <40 | 94 | 45.7% (43) | ref | 71.3% (67) | ref | ||
| 40–60 | 179 | 64.8% (116) | 1.48 [0.78–2.78] | 0.227 | 90.5% (162) | 2.38 [0.96–5.90] | 0.062 |
| >60 | 78 | 59.0% (46) | 1.85 [0.84–4.11] | 0.129 | 83.3% (65) | 2.46 [0.78–7.76] | 0.125 |
| Country class B | |||||||
| HIC | 281 | 63.0% (177) | ref | 88.3% (248) | ref | ||
| LMIC | 70 | 40.0% (28) | 0.33 [0.14–0.75] | 0.009 | 65.7% (46) | 0.19 [0.06–0.60] | 0.005 |
| Nationality C | |||||||
| The Netherlands | 171 | 56.7% (97) | ref | 85.4% (146) | ref | ||
| Spain | 97 | 72.2% (70) | 1.77 [0.90–3.45] | 0.100 | 92.8% (90) | 1.87 [0.63–5.58] | 0.259 |
| Myanmar | 34 | 14.7% (5) | 0.15 [0.05–0.52] | 0.003 | 38.2% (13) | 0.15 [0.04–0.57] | 0.005 |
| Duration B | |||||||
| <3 years | 133 | 60.2% (80) | ref | 82.7% (110) | ref | ||
| 3–10 years | 129 | 55.8% (72) | 1.06 [0.61–1.84] | 0.832 | 83.7% (108) | 1.82 [0.81–4.09] | 0.148 |
| >10 years | 89 | 59.6% (53) | 0.71 [0.38–1.33] | 0.288 | 85.4% (76) | 0.89 [0.36–2.19] | 0.800 |
| Education B | |||||||
| Master/PhD | 157 | 61.2% (96) | ref | 88.5% (139) | ref | ||
| Bachelor | 143 | 59.4% (85) | 0.85 [0.51–1.43] | 0.547 | 82.5% (118) | 0.45 [0.21–0.97] | 0.043 |
| Lower levels | 49 | 49.0% (24) | 0.47 [0.22–0.99] | 0.048 | 75.5% (37) | 0.18 [0.06–0.53] | 0.002 |
| Expertise B | |||||||
| Scientific | 163 | 67.5% (110) | ref | 91.4% (149) | ref | ||
| Other | 188 | 50.5% (95) | 0.37 [0.23–0.62] | <0.001 | 77.1% (145) | 0.23 [0.10–0.50] | <0.001 |
| Living condition B | |||||||
| (Sub)urban | 220 | 59.1% (130) | ref | 82.7% (182) | ref | ||
| Rural | 130 | 57.7% (75) | 0.72 [0.43–1.21] | 0.211 | 85.4% (111) | 0.74 [0.33–1.63] | 0.451 |
| Occupation B | |||||||
| Government | 303 | 61.4% (186) | ref | 86.8% (263) | ref | ||
| Non-government | 45 | 18.0% (40) | 0.73 [0.30–1.75] | 0.483 | 62.2% (28) | 0.43 [0.14–1.27] | 0.127 |
| Role (detailed) D | |||||||
| Regional | 183 | 61.8% (113) | ref | 88.5% (162) | ref | ||
| Province | 64 | 60.9% (39) | 0.79 [0.43–1.48] | 0.453 | 89.1% (57) | 0.54 [0.19–1.50] | 0.237 |
| National | 25 | 60.0% (15) | 1.21 [0.44–3.30] | 0.715 | 88.0% (22) | 0.70 [0.15–3.22] | 0.644 |
| Non-government | 79 | 48.1% (38) | 0.88 [0.38–2.03] | 0.765 | 67.1% (53) | 0.18 [0.05–0.61] | 0.006 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naing, S.; van Wijk, M.; Vila, J.; Ballesté-Delpierre, C. Understanding Antimicrobial Resistance from the Perspective of Public Policy: A Multinational Knowledge, Attitude, and Perception Survey to Determine Global Awareness. Antibiotics 2021, 10, 1486. https://doi.org/10.3390/antibiotics10121486
Naing S, van Wijk M, Vila J, Ballesté-Delpierre C. Understanding Antimicrobial Resistance from the Perspective of Public Policy: A Multinational Knowledge, Attitude, and Perception Survey to Determine Global Awareness. Antibiotics. 2021; 10(12):1486. https://doi.org/10.3390/antibiotics10121486
Chicago/Turabian StyleNaing, SoeYu, Max van Wijk, Jordi Vila, and Clara Ballesté-Delpierre. 2021. "Understanding Antimicrobial Resistance from the Perspective of Public Policy: A Multinational Knowledge, Attitude, and Perception Survey to Determine Global Awareness" Antibiotics 10, no. 12: 1486. https://doi.org/10.3390/antibiotics10121486
APA StyleNaing, S., van Wijk, M., Vila, J., & Ballesté-Delpierre, C. (2021). Understanding Antimicrobial Resistance from the Perspective of Public Policy: A Multinational Knowledge, Attitude, and Perception Survey to Determine Global Awareness. Antibiotics, 10(12), 1486. https://doi.org/10.3390/antibiotics10121486








