Three-Year Trends of Healthcare-Associated Infections and Antibiotic Use in Acute Care Hospitals: Findings from 2016–2018 Point Prevalence Surveys in Sicily, Italy
Abstract
:1. Introduction
2. Results
2.1. Characteristics of Patients
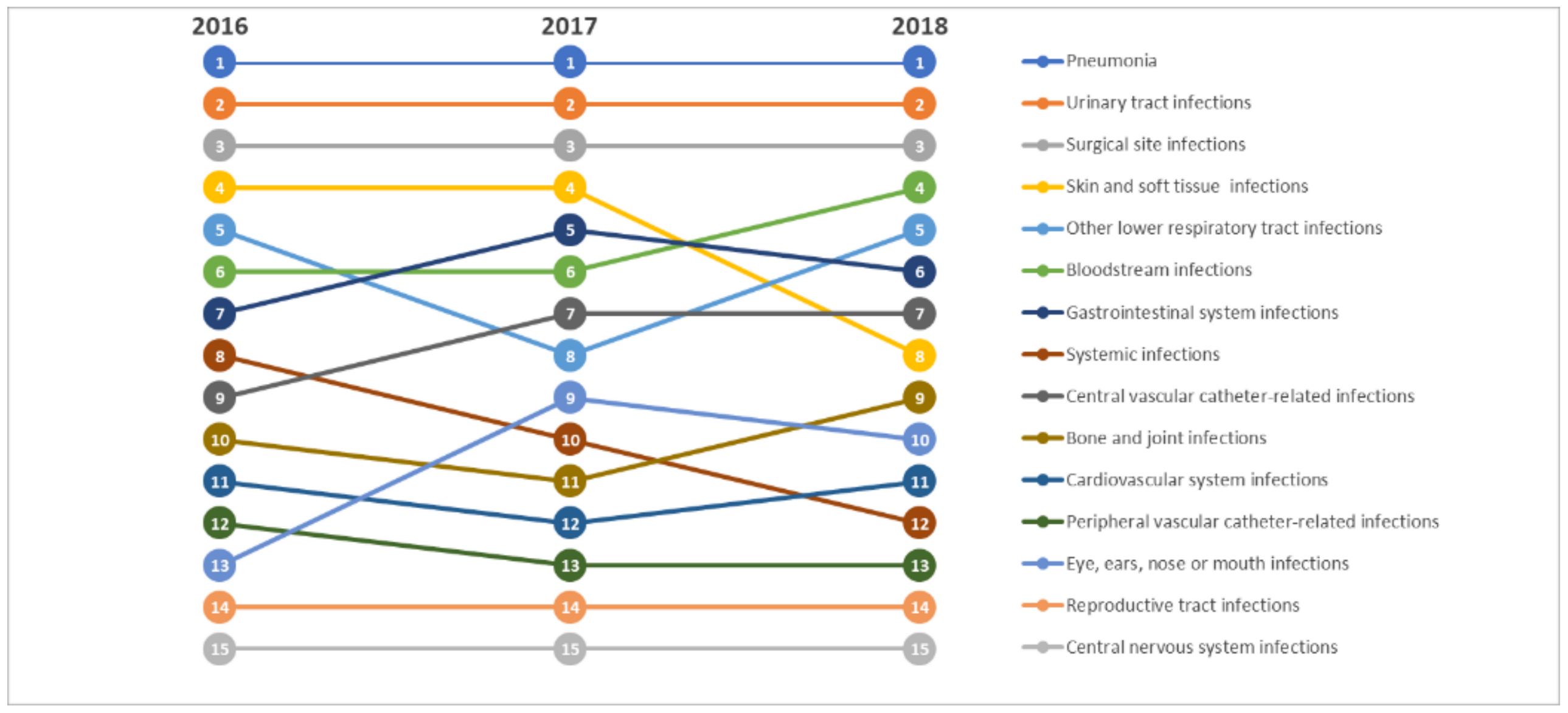
2.2. Prevalence of Healthcare-Associated Infections
2.3. Factors Related to Healthcare-Associated Infections
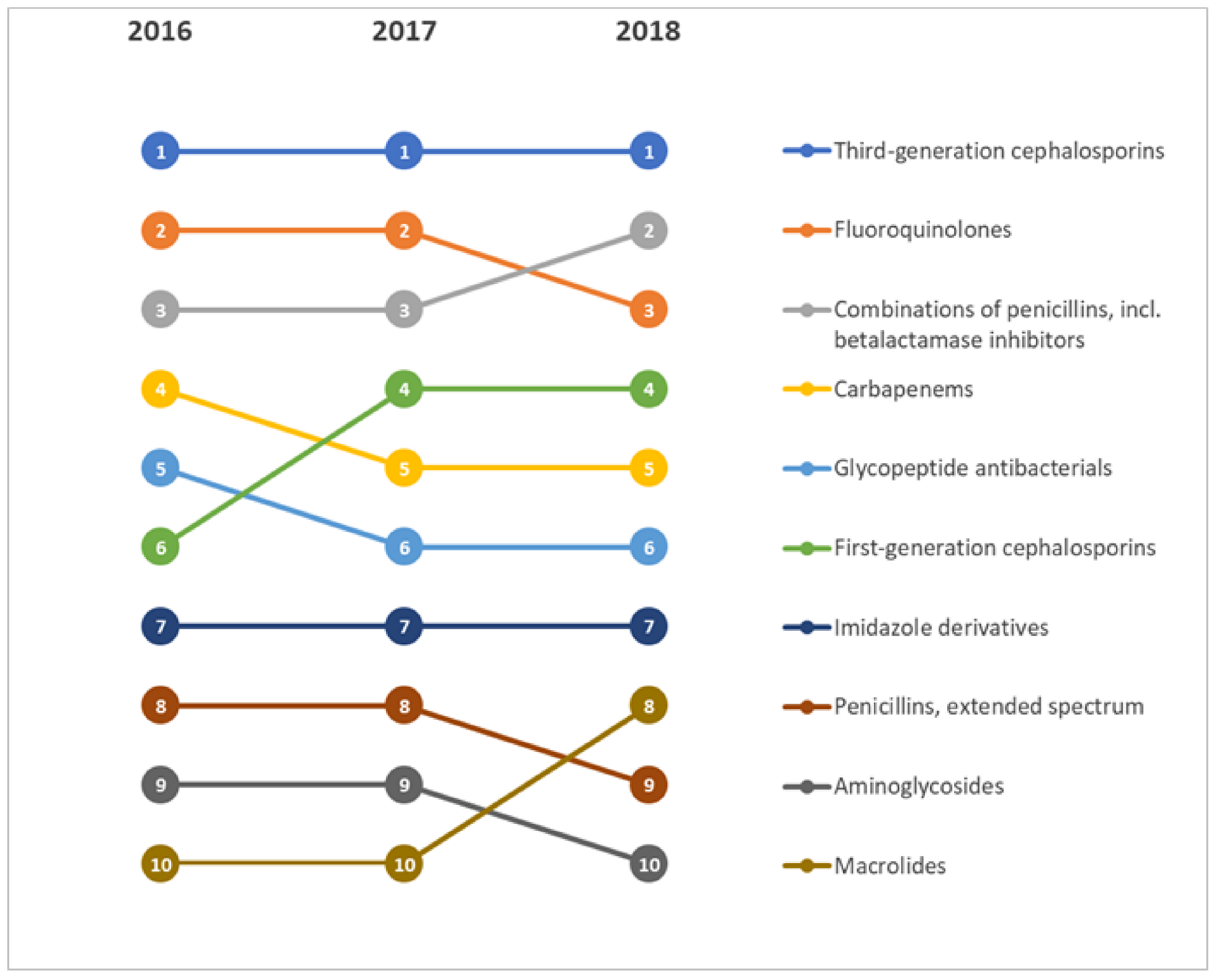
2.4. Prevalence of Antibiotic Use, Indication, and Antimicrobial Agents
3. Discussion
4. Materials and Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alp, E.; Damani, N. Healthcare-associated infections in intensive care units: Epidemiology and infection control in low-to-middle income countries. J. Infect. Dev. Ctries 2015, 9, 1040–1045. [Google Scholar] [CrossRef] [Green Version]
- Haque, M.; Sartelli, M.; McKimm, J.; Abu Bakar, M. Health care-associated infections—An overview. Infect. Drug Resist. 2018, 11, 2321–2333. [Google Scholar] [CrossRef] [Green Version]
- Serra-Burriel, M.; Keys, M.; Campillo-Artero, C.; Agodi, A.; Barchitta, M.; Gikas, A.; Palos, C.; López-Casasnovas, G. Impact of multi-drug resistant bacteria on economic and clinical outcomes of healthcare-associated infections in adults: Systematic review and meta-analysis. PLoS ONE 2020, 15, e0227139. [Google Scholar] [CrossRef]
- Agodi, A.; Barchitta, M.; Auxilia, F.; Brusaferro, S.; D’Errico, M.M.; Montagna, M.T.; Pasquarella, C.; Tardivo, S.; Arrigoni, C.; Fabiani, L.; et al. Epidemiology of intensive care unit-acquired sepsis in Italy: Results of the SPIN-UTI network. Ann. Ig 2018, 30, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.L.; Suetens, C.; Savey, A.; Palomar, M.; Hiesmayr, M.; Morales, I.; Agodi, A.; Frank, U.; Mertens, K.; Schumacher, M.; et al. Clinical outcomes of health-care-associated infections and antimicrobial resistance in patients admitted to European intensive-care units: A cohort study. Lancet Infect. Dis. 2011, 11, 30–38. [Google Scholar] [CrossRef]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals 2011–2012; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2013. [Google Scholar]
- Suetens, C.; Latour, K.; Kärki, T.; Ricchizzi, E.; Kinross, P.; Moro, M.L.; Jans, B.; Hopkins, S.; Hansen, S.; Lyytikäinen, O.; et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: Results from two European point prevalence surveys, 2016 to 2017. Euro Surveill. 2018, 23, 1800516. [Google Scholar] [CrossRef] [Green Version]
- Masia, M.D.; Barchitta, M.; Liperi, G.; Cantù, A.P.; Alliata, E.; Auxilia, F.; Torregrossa, V.; Mura, I.; Agodi, A.; (GISIO), I.S.G.o.H.H. Validation of intensive care unit-acquired infection surveillance in the Italian SPIN-UTI network. J. Hosp. Infect. 2010, 76, 139–142. [Google Scholar] [CrossRef]
- Haley, R.W.; Culver, D.H.; White, J.W.; Morgan, W.M.; Emori, T.G.; Munn, V.P.; Hooton, T.M. The efficacy of infection surveillance and control programs in preventing nosocomial infections in US hospitals. Am. J. Epidemiol 1985, 121, 182–205. [Google Scholar] [CrossRef]
- Haley, R.W.; Quade, D.; Freeman, H.E.; Bennett, J.V. The SENIC Project. Study on the efficacy of nosocomial infection control (SENIC Project). Summary of study design. Am. J. Epidemiol. 1980, 111, 472–485. [Google Scholar] [CrossRef]
- Gastmeier, P.; Sohr, D.; Schwab, F.; Behnke, M.; Zuschneid, I.; Brandt, C.; Dettenkofer, M.; Chaberny, I.F.; Rüden, H.; Geffers, C. Ten years of KISS: The most important requirements for success. J. Hosp. Infect. 2008, 70 (Suppl. 1), 11–16. [Google Scholar] [CrossRef]
- Zingg, W.; Holmes, A.; Dettenkofer, M.; Goetting, T.; Secci, F.; Clack, L.; Allegranzi, B.; Magiorakos, A.P.; Pittet, D. Systematic review and evidence-based guidance on organization of hospital infection control programmes (SIGHT) study group. Hospital organisation, management, and structure for prevention of health-care-associated infection: A systematic review and expert consensus. Lancet Infect. Dis. 2015, 15, 212–224. [Google Scholar] [CrossRef] [PubMed]
- Storr, J.; Twyman, A.; Zingg, W.; Damani, N.; Kilpatrick, C.; Reilly, J.; Price, L.; Egger, M.; Grayson, M.L.; Kelley, E.; et al. Core components for effective infection prevention and control programmes: New WHO evidence-based recommendations. Antimicrob. Resist. Infect. Control. 2017, 6, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mayon-White, R.T.; Ducel, G.; Kereselidze, T.; Tikomirov, E. An international survey of the prevalence of hospital-acquired infection. J. Hosp. Infect. 1988, 11 (Suppl. A), 43–48. [Google Scholar] [CrossRef]
- Barchitta, M.; Matranga, D.; Quattrocchi, A.; Bellocchi, P.; Ruffino, M.; Basile, G.; Agodi, A. Prevalence of surgical site infections before and after the implementation of a multimodal infection control programme. J. Antimicrob. Chemother. 2012, 67, 749–755. [Google Scholar] [CrossRef] [Green Version]
- Pearce, N. Classification of epidemiological study designs. Int. J. Epidemiol. 2012, 41, 393–397. [Google Scholar] [CrossRef] [Green Version]
- Barchitta, M.; Quattrocchi, A.; Maugeri, A.; Rosa, M.C.; Mastra, C.; Basile, G.; Giuffrida, G.; Rinaldi, F.M.; Murolo, G.; Agodi, A. The “Obiettivo Antibiotico” Campaign on Prudent Use of Antibiotics in Sicily, Italy: The Pilot Phase. Int. J. Environ. Res. Public Health 2020, 17. [Google Scholar] [CrossRef]
- Furmenti, M.F.; Rossello, P.; Bianco, S.; Olivero, E.; Thomas, R.; Emelurumonye, I.N.; Zotti, C.M.; Group, H.I.C. Healthcare-associated infections and antimicrobial use in long-term care facilities (HALT3): An overview of the Italian situation. J. Hosp. Infect. 2019, 102, 425–430. [Google Scholar] [CrossRef]
- Tardivo, S.; Moretti, F.; Agodi, A.; Appignanesi, R.; Baldovin, T.; Barchitta, M.; Brusaferro, S.; Canino, R.; Carli, A.; D’Errico, M.M.; et al. Essential strategies in HAI prevention and control: Performance assessment through the implementation of the HAI-CoSIP tool of the GISIO-SItI group. A pilot study in a sample of Italian Organizations. Ann. Ig. 2018, 30, 70–85. [Google Scholar] [CrossRef]
- Brusaferro, S.; Arnoldo, L.; Finzi, G.; Mura, I.; Auxilia, F.; Pasquarella, C.; Agodi, A.; Board Group. Hospital Hygiene and Infection Prevention and Control in Italy: State of the art and perspectives. Ann. Ig. 2018, 30, 1–6. [Google Scholar] [CrossRef]
- Tardivo, S.; Moretti, F.; Nobile, M.; Agodi, A.; Appignanesi, R.; Arrigoni, C.; Baldovin, T.; Brusaferro, S.; Canino, R.; Carli, A.; et al. Definition of criteria and indicators for the prevention of Healthcare-Associated Infections (HAIs) in hospitals for the purposes of Italian institutional accreditation and performance monitoring. Ann. Ig. 2017, 29, 529–547. [Google Scholar] [CrossRef] [PubMed]
- Agodi, A.; Auxilia, F.; Barchitta, M.; Brusaferro, S.; D’Alessandro, D.; Montagna, M.T.; Orsi, G.B.; Pasquarella, C.; Torregrossa, V.; Suetens, C.; et al. Building a benchmark through active surveillance of intensive care unit-acquired infections: The Italian network SPIN-UTI. J. Hosp. Infect. 2010, 74, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Secondo Studio di Prevalenza Italiano Sulle Infezioni Correlate All’assistenza e Sull’uso di Antibiotici Negli Ospedali Per Acuti—Protocollo ECDC.; Dipartimento Scienze Della Salute Pubblica e Pediatriche, Università di Torino. 2018. Available online: http://www.salute.gov.it/imgs/C_17_pubblicazioni_2791_allegato.pdf (accessed on 18 November 2020).
- Arnoldo, L.; Smaniotto, C.; Celotto, D.; Brunelli, L.; Cocconi, R.; Tignonsini, D.; Faruzzo, A.; Brusaferro, S.; Group, F.R.S.C. Monitoring healthcare-associated infections and antimicrobial use at regional level through repeated point prevalence surveys: What can be learnt? J. Hosp. Infect. 2019, 101, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Agodi, A.; Quattrocchi, A.; Barchitta, M.; Adornetto, V.; Cocuzza, A.; Latino, R.; Li Destri, G.; Di Cataldo, A. Risk of surgical site infection in older patients in a cohort survey: Targets for quality improvement in antibiotic prophylaxis. Int. Surg. 2015, 100, 473–479. [Google Scholar] [CrossRef]
- Barchitta, M.; Maugeri, A.; Favara, G.; Riela, P.M.; La Mastra, C.; La Rosa, M.C.; San Lio, R.M.; Gallo, G.; Mura, I.; Agodi, A.; et al. Cluster analysis identifies patients at risk of catheter-associated urinary tract infections in intensive care unit: Findings from the SPIN-UTI network. J. Hosp. Infect. 2020. [Google Scholar] [CrossRef]
- Agodi, A.; Auxilia, F.; Barchitta, M.; Brusaferro, S.; D’Alessandro, D.; Grillo, O.C.; Montagna, M.T.; Pasquarella, C.; Righi, E.; Tardivo, S.; et al. Trends, risk factors and outcomes of healthcare-associated infections within the Italian network SPIN-UTI. J. Hosp. Infect. 2013, 84, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Agodi, A.; Barchitta, M.; Quattrocchi, A.; Spera, E.; Gallo, G.; Auxilia, F.; Brusaferro, S.; D’Errico, M.M.; Montagna, M.T.; Pasquarella, C.; et al. Preventable proportion of intubation-associated pneumonia: Role of adherence to a care bundle. PLoS ONE 2017, 12, e0181170. [Google Scholar] [CrossRef] [Green Version]
- Valencia, C.; Hammami, N.; Agodi, A.; Lepape, A.; Herrejon, E.P.; Blot, S.; Vincent, J.L.; Lambert, M.L. Poor adherence to guidelines for preventing central line-associated bloodstream infections (CLABSI): Results of a worldwide survey. Antimicrob. Resist. Infect. Control. 2016, 5, 49. [Google Scholar] [CrossRef] [Green Version]
- Lambert, M.L.; Silversmit, G.; Savey, A.; Palomar, M.; Hiesmayr, M.; Agodi, A.; Van Rompaye, B.; Mertens, K.; Vansteelandt, S. Preventable proportion of severe infections acquired in intensive care units: Case-mix adjusted estimations from patient-based surveillance data. Infect. Control. Hosp. Epidemiol. 2014, 35, 494–501. [Google Scholar] [CrossRef]
- Lambert, M.L.; Palomar, M.; Agodi, A.; Hiesmayr, M.; Lepape, A.; Ingenbleek, A.; Palencia Herrejon, E.; Blot, S.; Frank, U. Prevention of ventilator-associated pneumonia in intensive care units: An international online survey. Antimicrob. Resist. Infect. Control. 2013, 2, 9. [Google Scholar] [CrossRef] [Green Version]
- Donelli, G.; De Paoli, P.; Fadda, G.; Marone, P.; Nicoletti, G.; Varaldo, P.E.; Group, C.S. A multicenter study on central venous catheter-associated infections in Italy. J. Chemother. 2001, 13 (Suppl. 4), 251–262. [Google Scholar] [CrossRef] [PubMed]
- Barchitta, M.; Quattrocchi, A.; Maugeri, A.; La Rosa, M.C.; La Mastra, C.; Sessa, L.; Cananzi, P.; Murolo, G.; Oteri, A.; Basile, G.; et al. Antibiotic Consumption and Resistance during a 3-Year Period in Sicily, Southern Italy. Int. J. Environ. Res. Public Health 2019, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agodi, A.; Auxilia, F.; Barchitta, M.; Brusaferro, S.; D’Errico, M.M.; Montagna, M.T.; Pasquarella, C.; Tardivo, S.; Mura, I.; SPIN-UTI network of the GISIOWorking Group of the Italian Society of Hygiene, Preventive Medicine and Public Health (SItI). Antibiotic consumption and resistance: Results of the SPIN-UTI project of the GISIO-SItI. Epidemiol. Prev. 2015, 39, 94–98. [Google Scholar] [PubMed]
- Agodi, A.; Barchitta, M.; Quattrocchi, A.; Maugeri, A.; Aldisio, E.; Marchese, A.E.; Mattaliano, A.R.; Tsakris, A. Antibiotic trends of Klebsiella pneumoniae and Acinetobacter baumannii resistance indicators in an intensive care unit of Southern Italy, 2008–2013. Antimicrob. Resist. Infect. Control. 2015, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Agodi, A.; Voulgari, E.; Barchitta, M.; Quattrocchi, A.; Bellocchi, P.; Poulou, A.; Santangelo, C.; Castiglione, G.; Giaquinta, L.; Romeo, M.A.; et al. Spread of a carbapenem- and colistin-resistant Acinetobacter baumannii ST2 clonal strain causing outbreaks in two Sicilian hospitals. J. Hosp. Infect. 2014, 86, 260–266. [Google Scholar] [CrossRef]
- Zarrilli, R.; Di Popolo, A.; Bagattini, M.; Giannouli, M.; Martino, D.; Barchitta, M.; Quattrocchi, A.; Iula, V.D.; de Luca, C.; Scarcella, A.; et al. Clonal spread and patient risk factors for acquisition of extensively drug-resistant Acinetobacter baumannii in a neonatal intensive care unit in Italy. J. Hosp. Infect. 2012, 82, 260–265. [Google Scholar] [CrossRef]
- Stefani, S.; Agodi, A. Molecular epidemiology of antibiotic resistance. Int. J. Antimicrob. Agents 2000, 13, 143–153. [Google Scholar] [CrossRef]
- Plachouras, D.; Kärki, T.; Hansen, S.; Hopkins, S.; Lyytikäinen, O.; Moro, M.L.; Reilly, J.; Zarb, P.; Zingg, W.; Kinross, P.; et al. Antimicrobial use in European acute care hospitals: Results from the second point prevalence survey (PPS) of healthcare-associated infections and antimicrobial use, 2016 to 2017. Euro Surveill. 2018, 23. [Google Scholar] [CrossRef] [Green Version]
- Assessorato della Salute della Regione Siciliana Programma Regionale di Sorveglianza e Controllo Delle ICA. Available online: https://www.qualitasiciliassr.it/?q=infezioni-correlate-assistenza (accessed on 18 November 2020).
- Agodi, A.; Barchitta, M.; Mura, I.; Pasquarella, C.; Torregrossa, M.V.; SItI, G. The commitment of the GISIO-SItI to contrast Healthcare-Associated Infections and the experience of prevalence studies in Sicily. Ann. Ig. 2018, 30, 38–47. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Point Prevalence Survey of Healthcare-Associated Infections and Antimicrobial Use in European Acute Care Hospitals, Protocol version 5.1; European Centre for Disease Prevention and Control: Stockholm, Sweden, 2016. [Google Scholar]


| Characteristics | 2016 (n = 6448) | 2017 (n = 5974) | 2018 (n = 6430) | p-Value a |
|---|---|---|---|---|
| Age, years b | 58.6 (24.7) | 58.5 (25.3) | 62.4 (22.2) | <0.001 |
| Gender (% men) | 50.3% | 51.0% | 50.5% | 0.720 |
| Surgery during admission | ||||
| None | 69.3% | 68.7% | 67.4% | <0.001 |
| NHSN operative procedure | 17.9% | 20.6% | 17.5% | |
| Non-NHSN operative procedure | 12.8% | 10.7% | 10.1% | |
| McCabe score c | ||||
| Non-fatal | 77.0% | 74.6% | 62.6% | <0.001 |
| Fatal | 12.2% | 11.8% | 11.6% | |
| Rapidly fatal | 10.8% | 13.6% | 16.4% | |
| Presence of urinary catheter | 33.5% | 35.5% | 41.2% | <0.001 |
| Presence of intubation | 3.4% | 4.5% | 5.6% | <0.001 |
| Presence of central venous catheter | 8.2% | 9.9% | 11.0% | <0.001 |
| Presence of peripheral venous catheter | 63.1% | 67.6% | 71.0% | <0.001 |
| Characteristics | Univariate Analysis a | Logistic Regression b | |||
|---|---|---|---|---|---|
| Non-Infected | Infected | p-Value | OR | p-Value | |
| Age, years c | 59.6 (24.3) | 63.3 (22.1) | <0.001 | 1.00 (0.99–1.01) | 0.491 |
| Gender (% men) | 50.5% | 53.1% | 0.111 | 0.96 (0.83–1.12) | 0.606 |
| Surgery during admission | |||||
| None | 70.1% | 59.9% | <0.001 | Ref | |
| Non-NHSN | 11.4% | 13.1% | 0.96 (0.76–1.21) | 0.732 | |
| NHSN | 18.5% | 27.0% | 1.04 (0.87–1.24) | 0.682 | |
| McCabe score d | |||||
| Non-fatal | 74.7% | 46.6% | <0.001 | Ref | |
| Fatal | 11.8% | 24.1% | 1.70 (1.39–2.07) | <0.001 | |
| Rapidly fatal | 13.5% | 29.3% | 1.91 (1.57–2.31) | <0.001 | |
| Presence of urinary catheter | 35.7% | 61.2% | <0.001 | 1.16 (0.97–1.38) | 0.101 |
| Presence of intubation | 3.7% | 19.3% | <0.001 | 1.88 (1.49–2.38) | <0.001 |
| Presence of central venous catheter | 8.1% | 38.8% | <0.001 | 3.21 (2.61–3.95) | <0.001 |
| Presence of peripheral venous catheter | 67.4% | 69.9% | 0.976 | 0.99 (0.82–1.21) | 0.951 |
| Antibiotic use prevalence | 51.0% | 96.6% | <0.001 | 18.87 (13.08–27.22) | <0.001 |
| Indication | 2016 (n = 4271) | 2017 (n = 4156) | 2018 (n = 4414) | p-Value a |
|---|---|---|---|---|
| Surgical prophylaxis | 27.0% | 26.7% | 21.5% | <0.001 |
| Treatment of community infection | 22.3% | 22.2% | 24.5% | 0.017 |
| Treatment of hospital infection | 9.9% | 7.3% | 10.1% | <0.001 |
| Treatment of infection acquired in LTCF | 1.5% | 1.9% | 1.6% | 0.330 |
| Medical prophylaxis | 34.1% | 35.6% | 36.4% | 0.073 |
| Other indication/Unknown | 5.2% | 6.3% | 5.8% | 0.092 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barchitta, M.; Maugeri, A.; La Rosa, M.C.; La Mastra, C.; Murolo, G.; Agodi, A. Three-Year Trends of Healthcare-Associated Infections and Antibiotic Use in Acute Care Hospitals: Findings from 2016–2018 Point Prevalence Surveys in Sicily, Italy. Antibiotics 2021, 10, 1. https://doi.org/10.3390/antibiotics10010001
Barchitta M, Maugeri A, La Rosa MC, La Mastra C, Murolo G, Agodi A. Three-Year Trends of Healthcare-Associated Infections and Antibiotic Use in Acute Care Hospitals: Findings from 2016–2018 Point Prevalence Surveys in Sicily, Italy. Antibiotics. 2021; 10(1):1. https://doi.org/10.3390/antibiotics10010001
Chicago/Turabian StyleBarchitta, Martina, Andrea Maugeri, Maria Clara La Rosa, Claudia La Mastra, Giuseppe Murolo, and Antonella Agodi. 2021. "Three-Year Trends of Healthcare-Associated Infections and Antibiotic Use in Acute Care Hospitals: Findings from 2016–2018 Point Prevalence Surveys in Sicily, Italy" Antibiotics 10, no. 1: 1. https://doi.org/10.3390/antibiotics10010001
APA StyleBarchitta, M., Maugeri, A., La Rosa, M. C., La Mastra, C., Murolo, G., & Agodi, A. (2021). Three-Year Trends of Healthcare-Associated Infections and Antibiotic Use in Acute Care Hospitals: Findings from 2016–2018 Point Prevalence Surveys in Sicily, Italy. Antibiotics, 10(1), 1. https://doi.org/10.3390/antibiotics10010001







