Evaluation of Smartphones Equipped with Light Detection and Ranging Technology for Circumferential and Volumetric Measurements in Lower Extremity Lymphedema
Abstract
1. Introduction
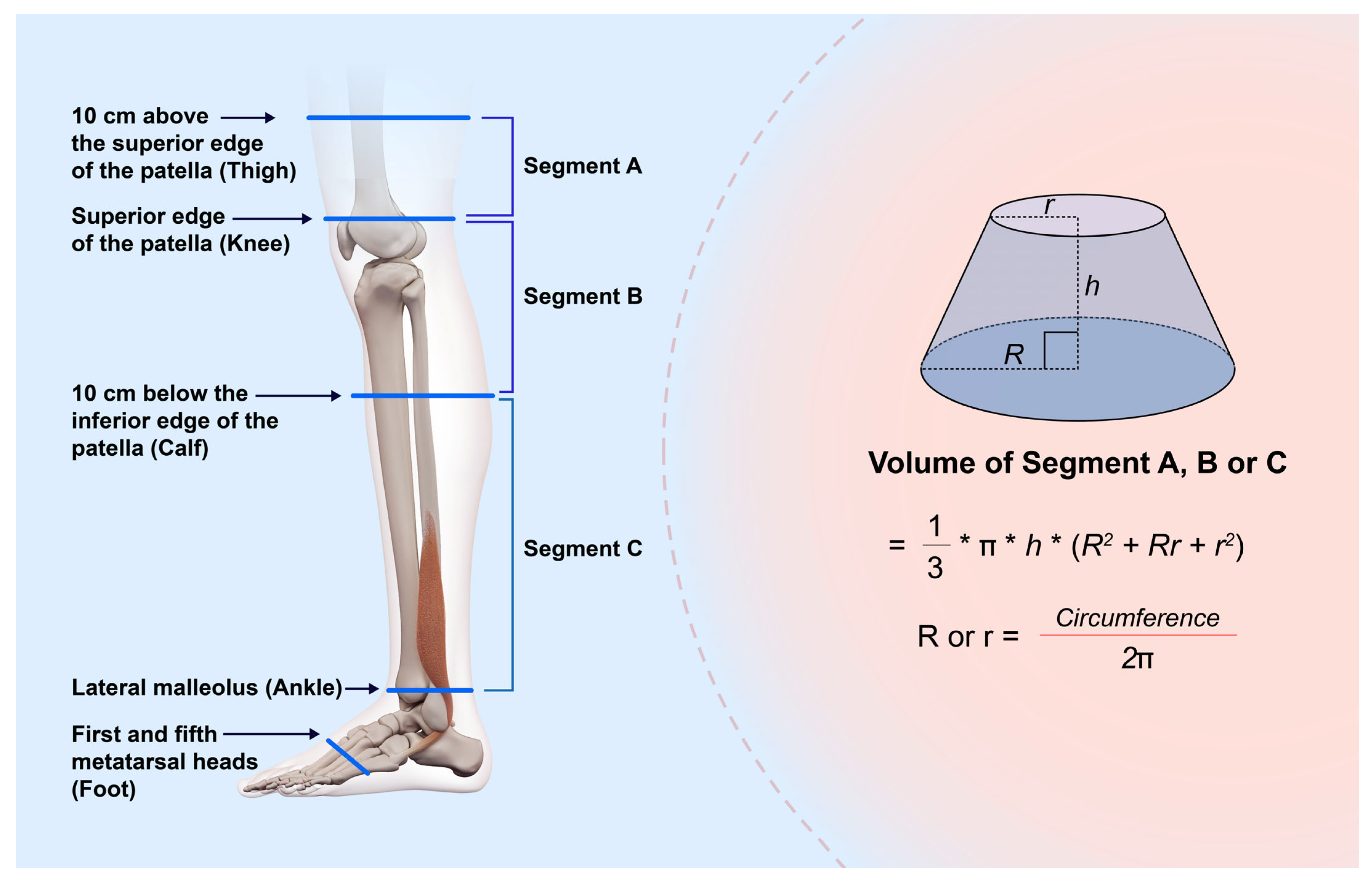
2. Materials and Methods
2.1. Evaluation of the Validity and Reliability of LiDAR in a Healthy Volunteer
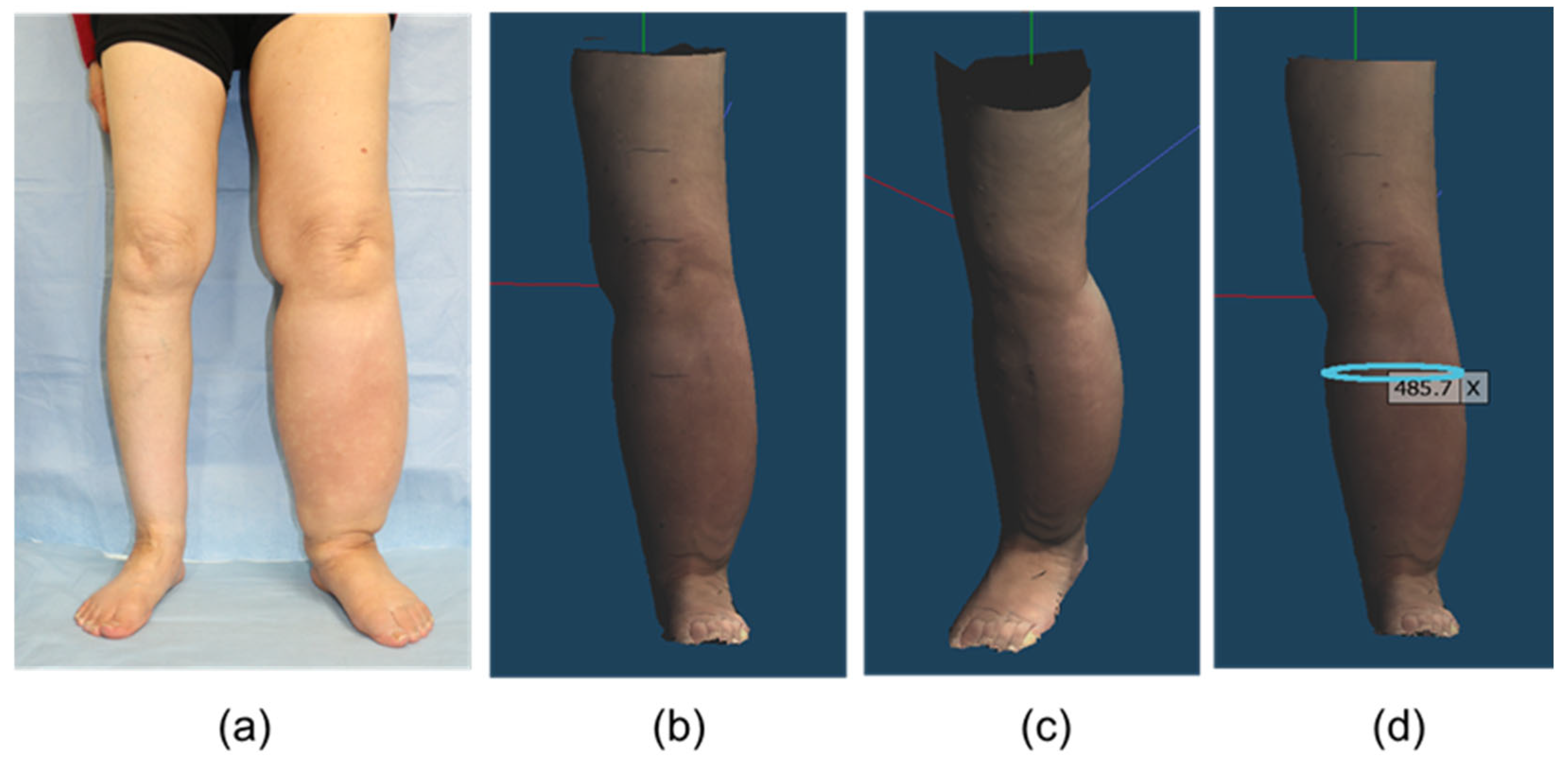
2.2. Agreement and Correlation Between TM and LiDAR in Patients with LEL
2.3. Statistical Analysis
3. Results
3.1. Evaluation of the Validity and Reliability of LiDAR in a Healthy Volunteer
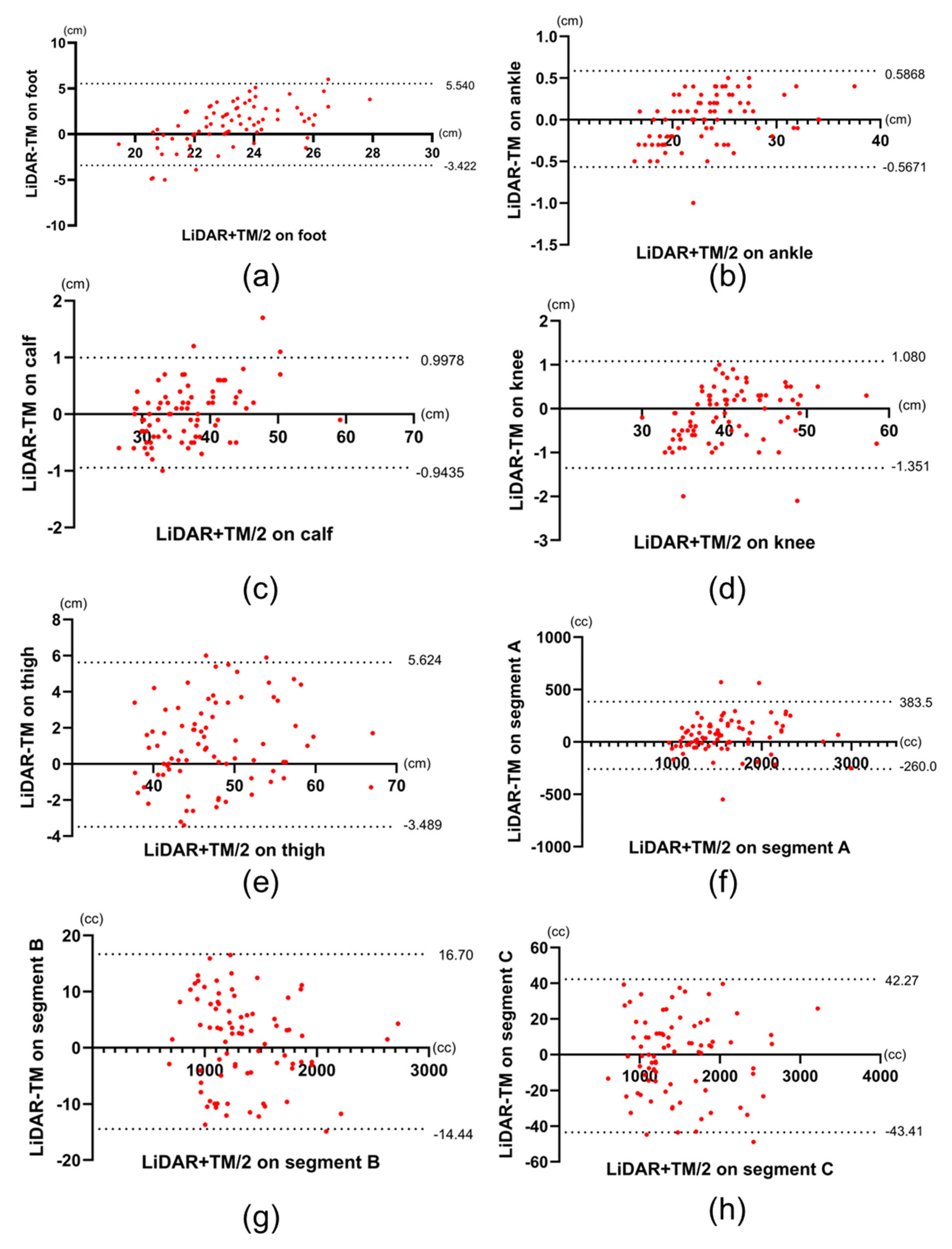
3.2. Agreement and Correlation Between TM and LiDAR in Patients with LEL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TM | Tape measurement |
| LiDAR | Light detection and ranging |
| LOA | Limits of agreement |
| 3D | Three-dimensional |
| BMI | Body mass index |
| ISL | International Society of Lymphology |
| LEL | Lower extremity lymphedema |
| ICC | Intraclass correlation coefficient |
| CI | Confidence interval |
References
- Executive Committee of the International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2020 Consensus Document of the International Society of Lymphology. Lymphology 2020, 53, 3–19. [Google Scholar] [CrossRef]
- Vilán, J.; Caamaño, J.; Cabaleiro, M.; Arias, P.; Riveiro, B. Automatic 3D modelling of metal frame connections from LiDAR data for structural engineering purposes. ISPRS J. Photogramm. Remote. Sens. 2014, 96, 47–56. [Google Scholar] [CrossRef]
- Li, Y.; Ibanez-Guzman, J. Lidar for Autonomous Driving: The Principles, Challenges, and Trends for Automotive Lidar and Perception Systems. IEEE Signal Process. Mag. 2020, 37, 50–61. [Google Scholar] [CrossRef]
- Zhang, X.; Li, J.; Xia, S.; Chen, D.; Wang, R. Geometric Primitives in LiDAR Point Clouds: A Review. IEEE J. Sel. Top. Appl. Earth Obs. Remote. Sens. 2020, 13, 685–707. [Google Scholar] [CrossRef]
- Fineschi, V.; Ciallella, C.; Manetti, A.C.; Maiese, A. The Introduction of a New Diagnostic Tool in Forensic Pathology: LiDAR Sensor for 3D Autopsy Documentation. Biosensors 2022, 12, 132. [Google Scholar] [CrossRef]
- Sader, R.; Beyer, M.; Thieringer, F.M.; Seifert, L.B.; Czok, V.; Aigner, A.; Abazi, S. Comparative Accuracy of Stationary and Smartphone-Based Photogrammetry in Oral and Maxillofacial Surgery: A Clinical Study. J. Clin. Med. 2024, 13, 6678. [Google Scholar] [CrossRef]
- Kwon, H.; Ha, Y.; Kim, J.; Kim, S.; Oh, S.-H.; Song, B.; Song, S.-H. Smartphone-Based LiDAR Application for Easy and Accurate Wound Size Measurement. J. Clin. Med. 2023, 12, 6042. [Google Scholar] [CrossRef]
- iPhone 15 Pro Technical Specifications. Available online: https://support.apple.com/en-us/111829 (accessed on 18 February 2025).
- Charlton, M.E.; Large, A.R.G.; Fuller, I.C. Application of airborne LiDAR in river environments: The River Coquet, Northumberland, UK. Earth Surf. Process. Landf. 2003, 28, 299–306. [Google Scholar] [CrossRef]
- Hill, J.M.; Graham, L.A.; Henry, R.J.; Cotter, D.M.; Young, D. Wide-area topographic mapping and applications using airborne light detection and ranging (LIDAR) technology. Photogramm. Eng. Remote Sens. 2000, 66, 908–914. [Google Scholar]
- Wulder, M.A.; Bater, C.W.; Coops, N.C.; Hilker, T.; White, J.C. The role of LiDAR in sustainable forest management. For. Chron. 2008, 84, 807–826. [Google Scholar] [CrossRef]
- Li, S.; Fan, X.; Wang, H.; Guo, H.; Rao, Q.; Hou, Z.; Qiu, S.; Huang, L. Body Dimension Measurements of Qinchuan Cattle with Transfer Learning from LiDAR Sensing. Sensors 2019, 19, 5046. [Google Scholar] [CrossRef] [PubMed]
- Tezuka, T.; Ishigaki, T.; Kuriyama, M.; Ogata, H.; Kosaka, K.; Yamaji, Y.; Mitsukawa, N.; Akita, S.; Tokumoto, H. Comparison of Vectra three-dimensional stereophotogrammetry measurement and tape measurement in the evaluation of perioperative volume change of the lower abdomen in association with lymphatic microsurgery. Microsurgery 2020, 42, 50–56. [Google Scholar] [CrossRef]
- Deltombe, T.; Jamart, J.; Recloux, S.; Legrand, C.; Vandenbroeck, N.; Theys, S.; Hanson, P. Reliability and limits of agreement of circumferential, water displacement, and optoelectronic volumetry in the measurement of upper limb lymphedema. Lymphology 2007, 40, 26–34. [Google Scholar]
- Saw, R.P.M.; Spillane, A.J.; Byth, K.; Thompson, J.F.; Tucker, M.G.D. Defining Lower Limb Lymphedema After Inguinal or Ilio-Inguinal Dissection in Patients With Melanoma Using Classification and Regression Tree Analysis. Ann. Surg. 2008, 248, 286–293. [Google Scholar] [CrossRef]
- Biehl, J.T.; Andrews, E.G.; Babichenko, D.; Khan, T. A systematic comparison of the accuracy of monocular RGB tracking and LiDAR for neuronavigation. Health Technol. Lett. 2022, 9, 91–101. [Google Scholar] [CrossRef]
- Morgenthal, G.; Tondo, G.R.; Riley, C. Characterization of the iPhone LiDAR-Based Sensing System for Vibration Measurement and Modal Analysis. Sensors 2023, 23, 7832. [Google Scholar] [CrossRef]
- Kroon, A.; Bjørk, A.A.; Luetzenburg, G. Evaluation of the Apple iPhone 12 Pro LiDAR for an Application in Geosciences. Sci. Rep. 2021, 11, 22221. [Google Scholar] [CrossRef]
- D Scanner App. Available online: https://3dscannerapp.com/ (accessed on 20 May 2025).
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Beurskens, C.H.; Hidding, J.T.; van Laarhoven, H.W.; der Sanden, M.W.N.-V.; van der Wees, P.J.; Viehoff, P.B. Measurement Properties of Instruments for Measuring of Lymphedema: Systematic Review. Phys. Ther. 2016, 96, 1965–1981. [Google Scholar] [CrossRef]
- Critchley, L.A.H.; Critchley, J.A.J.H. A Meta-Analysis of Studies Using Bias and Precision Statistics to Compare Cardiac Output Measurement Techniques. J. Clin. Monit. Comput. 1999, 15, 85–91. [Google Scholar] [CrossRef]
- Boonhong, J. Validity and reliability of girth measurement (circumferencemeasurement) for calculating residual limb volumein below-knee amputees. Chulalongkorn Med. J. 2007, 51, 77–88. [Google Scholar] [CrossRef]
- Coutts, F.; Bulley, C.; Tan, C.-W. Measurement of lower limb volume: Agreement between the vertically oriented perometer and a tape measure method. Physiotherapy 2013, 99, 247–251. [Google Scholar] [CrossRef]
- Kuriyama, M.; Tokumoto, H.; Akita, S.; Mitsukawa, N. Utilization of Three-Dimensional Photography (VECTRA) for the Evaluation of Lower Limb Lymphedema in Patients Following Lymphovenous Anastomosis. Lymphat. Res. Biol. 2018, 16, 547–552. [Google Scholar] [CrossRef]
- Hnin, Y.K.; Ong, L.X.; Tsai, C.C.-C.; Ong, S.S.; Yee, S.G.; Choo, B.A.; Low, J.J.H. Does initial routine use of a compression garment reduce the risk of lower limb lymphedema after gynecological cancer treatment? A randomized pilot study in an Asian institution and review of the literature. Lymphology 2018, 51, 174–183. [Google Scholar]
- Partsch, H.; Neumann, H.A.; Flour, M.; Mosti, G. Classification of compression stockings: Report of the meeting of the International Compression Club, Copenhagen. Int. Angiol. 2015, 35, 122–128. [Google Scholar]
- Lucas, C.; E Nieweg, O.; Van Geel, A.N.; De Rooij, J.D.; Horenblas, S.; Aaronson, N.K.; Stuiver, M.M.; Van Beurden, M. No evidence of benefit from class-II compression stockings in the prevention of lower-limb lymphedema after inguinal lymph node dissection: Results of a randomized controlled trial. Lymphology 2013, 46, 120–131. [Google Scholar]
- Kristiansen, M.; Skogh, A.-C.D.; Halle, M.; Pignatti, M. Evaluation and selection of lower limb lymphedema patients for lymphaticovenular anastomosis: A prospective study. Injury 2020, 51, S108–S113. [Google Scholar] [CrossRef]
- Rutks, I.R.; Hillman, Y.J.; Greer, N.L.; Hagel, E.M.; Warshaw, E.M.; MacDonald, R.; Wilt, T.J. Teledermatology for diagnosis and management of skin conditions: A systematic review. J. Am. Acad. Dermatol. 2011, 64, 759-772.e21. [Google Scholar] [CrossRef]
- Down, M.; Czubak, F.; Grsuska, G.; Stacley, S.; Benham, D. Recommended Practices for Replicable Measurement Systems. In Measurement System Analysis, 4th ed.; AIAG: Southfield, MI, USA, 2010; pp. 102–103. [Google Scholar]
- Aerospace Engine Supplier Quality Steering Group. Elements to Consider When Conducting MSA. In RM13003—Measurement Systems Analysis, 2nd ed.; SAE Industry Technologies Consortia: Warrendale, PA, USA, 2022; pp. 14–15. [Google Scholar]



| LiDAR (n = 9) | TM (n = 9) | p Value | |
|---|---|---|---|
| Foot (cm) | 23.9 ± 1.57 | 23.8 ± 0.413 | 0.690 |
| Ankle (cm) | 21.3 ± 1.32 | 21.6 ± 0.371 | 0.623 |
| Calf (cm) | 35.9 ± 0.810 | 36.0 ± 0.534 | 0.756 |
| Knee (cm) | 37.9 ± 0.995 | 37.7 ± 0.296 | 0.626 |
| Thigh (cm) | 44.6 ± 0.596 | 44.7 ± 0.454 | 0.722 |
| Segment A (cc) | 1369.9 ± 30.5 | 1353.4 ± 20.8 | 0.216 |
| Segment B (cc) | 1826.6 ± 42.8 | 1783.7 ± 120.7 | 0.289 |
| Segment C (cc) | 1567.2 ± 54.4 | 1564.7 ± 151.7 | 0.929 |
| Patients (n = 55) | Affected Limbs (n = 81) | ||
|---|---|---|---|
| Age (year) | 64.1 ± 11.4 | - | |
| Causes of lymphedema | Endometrial cancer | 28 | - |
| Ovarian cancer | 12 | - | |
| Cervical Cancer | 10 | - | |
| Primary lymphedema | 2 | - | |
| Others | 3 | - | |
| BMI | 23.8 ± 5.10 | - | |
| ISL classification per limb | 1 | - | 55 |
| 2a | - | 15 | |
| 2b | - | 10 | |
| 3 | - | 1 | |
| Lymphedema duration(month) | - | 56.7 ± 73.6 |
| LiDAR (cm/cc) | TM (cm/cc) | p Value | Correlation Coefficient | p Value | △LOAs (cm/cc) | %△LOAs to the Mean Measurement Made Using LiDAR | |
|---|---|---|---|---|---|---|---|
| Foot | 23.7 ± 2.53 | 22.7 ± 1.40 | <0.0001 | 0.519 | <0.0001 | 8.49 | 35.8 |
| Ankle | 23.2 ± 4.10 | 23.1 ± 3.98 | 0.378 | 0.998 | <0.0001 | 1.09 | 4.70 |
| Calf | 36.2 ± 5.77 | 36.2 ± 5.58 | 0.648 | 0.997 | <0.0001 | 1.88 | 5.19 |
| Knee | 40.3 ± 5.48 | 40.4 ± 5.32 | 0.758 | 0.994 | <0.0001 | 2.38 | 5.90 |
| Thigh | 47.4 ± 6.61 | 46.3 ± 6.31 | <0.0001 | 0.932 | <0.0001 | 9.41 | 19.8 |
| Segment A | 1575 ± 455 | 1523 ± 411 | 0.0020 | 0.925 | <0.0001 | 677 | 42.9 |
| Segment B | 1327 ± 372 | 1326 ± 373 | 0.285 | 0.999 | <0.0001 | 31.9 | 2.40 |
| Segment C | 1461 ± 480 | 1460 ± 483 | 0.625 | 0.998 | <0.0001 | 90.0 | 6.16 |
| LiDAR (cm/cc) | TM (cm/cc) | p Value | Correlation Coefficient | p Value | △LOAs (cm/cc) | %△LOAs to the Mean Measurement Made Using LiDAR | |
|---|---|---|---|---|---|---|---|
| Foot | 23.8 ± 2.57 | 22.7 ± 1.43 | <0.0001 | 0.466 | <0.0001 | 8.96 | 37.6 |
| Ankle | 23.4 ± 4.36 | 23.3 ± 4.24 | 0.763 | 0.998 | <0.0001 | 1.14 | 4.87 |
| Calf | 36.6 ± 6.10 | 36.5 ± 5.87 | 0.623 | 0.997 | <0.0001 | 1.93 | 5.27 |
| Knee | 40.7 ± 5.64 | 40.8 ± 5.50 | 0.0522 | 0.994 | <0.0001 | 2.43 | 5.97 |
| Thigh | 48.0 ± 6.70 | 46.9 ± 6.31 | <0.0001 | 0.937 | <0.0001 | 9.10 | 18.9 |
| Segment A | 1623 ± 442 | 1561 ± 425 | 0.0011 | 0.929 | <0.0001 | 642 | 39.5 |
| Segment B | 1351 ± 393 | 1349 ± 394 | 0.204 | 0.998 | <0.0001 | 31.3 | 2.31 |
| Segment C | 1485 ± 514 | 1486 ± 516 | 0.815 | 0.999 | <0.0001 | 85.6 | 5.76 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsuchiya, M.; Abe, K.; Kubo, S.; Azuma, R. Evaluation of Smartphones Equipped with Light Detection and Ranging Technology for Circumferential and Volumetric Measurements in Lower Extremity Lymphedema. Biosensors 2025, 15, 381. https://doi.org/10.3390/bios15060381
Tsuchiya M, Abe K, Kubo S, Azuma R. Evaluation of Smartphones Equipped with Light Detection and Ranging Technology for Circumferential and Volumetric Measurements in Lower Extremity Lymphedema. Biosensors. 2025; 15(6):381. https://doi.org/10.3390/bios15060381
Chicago/Turabian StyleTsuchiya, Masato, Kanako Abe, Satoshi Kubo, and Ryuichi Azuma. 2025. "Evaluation of Smartphones Equipped with Light Detection and Ranging Technology for Circumferential and Volumetric Measurements in Lower Extremity Lymphedema" Biosensors 15, no. 6: 381. https://doi.org/10.3390/bios15060381
APA StyleTsuchiya, M., Abe, K., Kubo, S., & Azuma, R. (2025). Evaluation of Smartphones Equipped with Light Detection and Ranging Technology for Circumferential and Volumetric Measurements in Lower Extremity Lymphedema. Biosensors, 15(6), 381. https://doi.org/10.3390/bios15060381





