Abstract
The adoption of wearable sensors for precision training has accelerated in recent years, yet most studies and reviews remain device- or feasibility-centric and lack a field-ready decision framework. This review organizes wearable sensing across four monitoring dimensions—physiological, kinematic, biochemical, and dynamic—and maps them onto three training pillars: physical, technical, and tactical. From the perspectives of athletes and coaches, we operationalize quality control, threshold, and feedback loop to translate measurement into action. We critically appraise key limitations, including signal robustness under high-intensity motion, inter-individual variability and limited model generalizability, cross-device data fusion and latency, battery life and wearability, privacy and data ownership, and limited accessibility beyond elite settings. Looking ahead, we advocate a shift from mere multidimensional measurement to a verifiable, reusable, and deployable precision-training ecosystem that delivers actionable metrics and clear decision support for practitioners.
1. Introduction
Accurate multidimensional data acquisition during physical activity is essential for optimizing training, preventing injuries, and enhancing performance. Continuous, real-time monitoring underpins individualized interventions, load evaluation, and early risk detection, aligning with the needs of precision training and rehabilitation [1,2,3]. Recent advances in muscle biology emphasize the plasticity of exercise metabolism and sex-specific adaptations, strengthening the biological rationale for data-driven monitoring [2,3].
Conventional approaches face common limitations: reliance on subjective ratings reduces reliability; laboratory or intermittent tests lack ecologically valid real-time measurements; and single indicators or modalities struggle to capture multiple parameters simultaneously and link them to training-competition contexts, thereby creating a measurement-to-decision bottleneck [4,5].
Wearable sensors help address these issues. Multimodal platforms, including IMUs, EMG, ECG, and sweat and other biofluid biochemical sensing, combined with low-power wireless and analytics, can continuously track internal and external loads with near-real-time feedback, providing a unified data foundation for mechanistic insight and practical optimization [6].
In the current wearable literature and reviews, a substantial proportion still prioritizes feasibility of signal acquisition and validity/reliability testing from device- or system-design perspectives, whereas decision workflows tailored to athletes/coaches remain underdeveloped [7,8,9,10,11]. Meanwhile, recent consensus statements and systematic reviews on training-load management-injury/illness risk and tactical/team spatiotemporal metrics emphasize internal and external load integration and contextualized application, moving wearable data from “signal-available” to “decision-ready” [1,12,13,14]. Accordingly, this review first structures the field into four dimensions: physiological, kinematic, biochemical, and kinetic; it then maps metrics onto three decision lines, conditioning, technical skills, and tactical coordination (as illustrated in Figure 1), and proposes a reusable framework of metric mapping, threshold setting, and feedback implementation to fill the device/validity-centric gap [1,6,12,13,14].
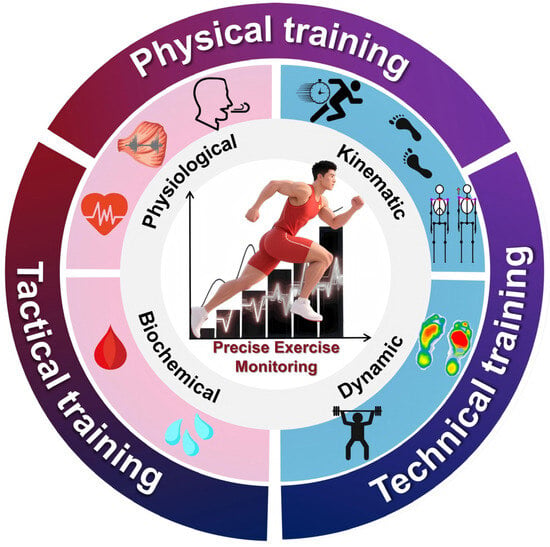
Figure 1.
A diagrammatic overview of the review. The signals commonly used in exercise monitoring and their application scenarios, including physiological signals, biochemical signals, kinematic signals, and dynamic signals. The monitoring of these signals is often applied in physical training, technical training, and tactical training.
2. The Functions of Wearable Sensors in Exercise Monitoring
2.1. Physiological Monitoring
Wearable sensors facilitate real-time monitoring of the athletes’ physiological parameters, providing an efficient and non-invasive approach to evaluating internal physiological responses across different stages of exercise [15,16]. These devices are capable of continuously tracking dynamic changes in key physiological indicators, thereby providing valuable insights into the athlete’s performance status and physical condition. Wrist photoplethysmography (PPG) delivers generally accurate heart rate (HR) (but not energy-expenditure), with proper quality control (QC), such as strap fit, motion-artifact suppression, signal-to-noise ratio (SNR), and signal quality index (SQI),which supports intensity prescription and session monitoring [17]. Standardized heart-rate variability (HRV) reflects autonomic balance for individualized load/recovery [18,19]. Skin/ear temperature fusion aids core-temperature and heat-strain management; electrodermal activity (EDA) is maturing for field stress assessment [20,21,22,23].
The field of physiological monitoring faces the following challenges: (1) High-intensity motion, skin tone/perfusion, strap tension, and posture changes systematically degrade the stability of PPG and HRV; therefore, multi-wavelength/multi-path PPG, motion-adaptive filtering with SQI, fixed posture/time acquisition, and interpretation against a rolling individual baseline should be used to improve the repeatability of training-and-recovery decisions [17,18,19]. (2) Inferring core temperature from skin temperature and assessing stress via EDA are both context-dependent (ambient heat/humidity, sweating and blood-flow redistribution, skin contact, and hydration); thus, multimodal fusion (ear/skin/HR/acceleration) with covariate logging of ambient conditions and contact impedance and scenario-specific validation of thresholds and alerts is required [20,21,22,23].
2.2. Kinematic Monitoring
Kinematic analysis focuses on the temporal and spatial characteristics of human movement, offering critical insights into the mechanical execution and coordination of motion patterns. Through quantifying variables such as velocity, acceleration, displacement, and joint angles, kinematic assessment serves as a foundation for evaluating movement quality, efficiency, and potential asymmetries.
Field IMU kinematics now show increasing concurrent validity and test–retest reliability versus optical systems for running/walking spatiotemporal metrics and joint angles [22,23,24]. The 2024 ISB recommendations standardize frames, alignment, and reporting, while alignment-free and dynamic-calibration methods reduce environmental and placement errors [25,26,27]. Tooling such as OpenSense and personalized musculoskeletal models is facilitating laboratory-to-field deployment [28].
The field of kinematic monitoring faces the following challenges: (1) Integration drift, soft-tissue artifact, and segment-frame misalignment still cap joint-angle accuracy; consequently, functional calibration, short-window integration with constrained sensor fusion, and alignment-free methods should be coupled with cross-task and cross-population validation to ensure generalization [22,23,24,25,26,27]. (2) Methodological heterogeneity, spanning event detection, joint definitions, and reporting conventions, limits comparability and reproducibility; therefore, studies should adopt ISB guidance, publish mappings from raw data to derived metrics and sensor placement protocols, and report uncertainty estimates [24,25,28,29,30,31].
2.3. Biochemical Monitoring
Although wearable biochemical monitoring remains at an early stage, preliminary applications in sport/exercise are promising. Most systems leverage sweat sensing for noninvasive, continuous readouts of internal load and homeostasis, integrated into garments, bands, or patches with minimal motion interference [32,33,34,35]. Recent reviews highlight that coupling flexible microfluidics with electrochemical transduction is improving sensitivity and spatiotemporal resolution [32,36].
Current capabilities and analytes beyond lactate and electrolytes (Na+, K+), cortisol (stress), and glucose (energy metabolism) are emerging targets [34,35,37,38,39,40]. Evidence suggests stronger serum–sweat agreement for cortisol in several studies and reviews, whereas sweat–blood lactate correspondence is conditional and often inconsistent across sweat rates and exercise phases. In parallel, continuous glucose monitoring (CGM) of interstitial fluid is gaining traction in athletes, but benefits and best practices for non-diabetic users are still being defined [37,38,39,40,41,42,43].
The field of biochemical monitoring faces the following challenges: (1) Calibration and stability under dynamics. Exercise induces temperature/humidity swings, motion, and strain that drive baseline drift and noise. Electrochemical readouts are sensitive to reference stability, redox potential, pH, and temperature. Consensus recommendations include in vivo and near-body multi-point calibration, redox buffers, stabilizing conducting polymers, and concurrent temperature and flow sensing to improve reproducibility [32,44]. (2) Inter- and intra-individual and site variability in sweat rate and chemistry. Intensity, environment, heat acclimation, sex, and body site affect sweat rate and [Na+], causing mixing of new and old sweat and local dilution/concentration. Best practice is to report real-time sweat rate, sampling site, and conditions and to use one-way microfluidics and flow metering to mitigate mixing artifacts [32,36,45,46,47,48]. (3) Sweat–blood mapping and lag vary depending on the analyte. Transport mechanisms differ by analyte: ions (Na+, Cl−) and tightly regulated species (e.g., K+) generally do not mirror plasma. Lactate correspondence is phase- and rate-dependent and often nonlinear; cortisol and other passively diffusing small molecules show more reliability between sweat and serum in several reports. Studies should include parallel blood/sweat (or interstitial) sampling, lag reporting, and calibration modeling [32,37,38,39,42,46].
2.4. Dynamics Monitoring
Dynamic monitoring focuses on force-related parameters in sports movements, providing essential biomechanical insights into how the body interacts with external surfaces and equipment during physical activity. By quantifying variables such as ground reaction forces (GRFs), joint loading patterns, and force application timing, dynamic monitoring plays a critical role in performance optimization, technique evaluation, and injury prevention.
In-shoe pressure-sensing systems quantify plantar pressure, partial GRFs, and contact events in the field and show generally good validity and reliability in walking and running, although peak vGRF may be underestimated in high-impact landings with notable device- and task-specific differences [49,50,51]. In endurance and strength contexts, LPT/LVT and IMU devices deliver actionable KPIs for velocity-based training with strong reliability under exercise- and load-specific constraints [52,53]. When force plates are unavailable, IMU-based models with machine learning (ML) can estimate GRFs and impulses; recent SSL approaches improve generalization and data efficiency and are beginning to integrate PINN-style priors [54].
The field of kinematic monitoring faces the following challenges: (1) Robust mapping from pressure to force is particularly challenging in high-impact scenarios (jumping and landing) because insoles primarily capture normal pressure (not shear) and may saturate or underestimate peaks; therefore, individualized calibration, task-specific models, and high-rate event detection are needed to improve peak and loading-rate estimates, alongside explicit definition of usage [49,50,51]. (2) Mechanical outputs are highly sensitive to surface, footwear, and fatigue, and current models often lack transparency; consequently, validation should span surfaces/footwear/athletes with uncertainty reporting, and IMU-based ML or SSL approaches ought to disclose training-data distributions and synchronization references while leveraging PINN/physics priors to curb overfitting and enhance transferability [54].
3. Wearable Sensors Facilitate the Precision Sports Training Systems
The multidimensional data captured in Section 2 (physiological, kinematic, biochemical, and dynamic) are integrated here to enable precision across three pillars of athletic preparation: physical, technical, and tactical training. We explicitly link each sensor stream to decision rules (zones, thresholds, and feedback) and appraise technology readiness levels (TRLs) and remaining barriers to adoption (as illustrated in Table 1).
We cautiously adapt TRLs to use-case units (“sensor × application”) in sport and compute an indicative 1–9 score using five dimensions with gate caps and a conservative synthesis:
Dimensions (A–E): A validity/reliability (agreement vs. reference, test–retest, field replication); B robustness/transfer (across speed/environment/skin tone/placement; failure modes and SQI); C standards/guidelines (e.g., ISB, FIFA EPTS, third-party testing); D workflow and closed-loop (QC–threshold–feedback, latency, minimal KPI set); E scale and compliance (multicenter deployment, quality/regulatory alignment).
Gate caps: no field reference—TRL ≤ 5; lack of standards/certification/guidance ⇒ TRL ≤ 7; no actionable thresholds or real-time feedback —TRL ≤ 6.
Synthesis: weighted average (A, B, D = 0.25; C, E = 0.125), floor to the lower bound and apply gates; report uncertainty ranges.
We anchor this approach in ISO-16290 while aligning with digital-health DiMe V3/V3+ and NICE ESF evidence expectations; FIFA EPTS performance testing serves as an external benchmark for high-TRL tracking use-casess [55,56,57,58,59].
3.1. Physical Training
Physical fitness training within sports conditioning constitutes a process centered on systematic load stimulation. Its primary objective is to specifically enhance the athletes’ physical attributes, namely, strength, endurance, speed, agility, and flexibility, through the scientific modulation of training intensity, volume, frequency, and recovery periods. Its core goal is to induce adaptive physiological and biomechanical remodeling of the body to optimize specific competitive performance and enhance exercise tolerance. During implementation, training plans must be dynamically adjusted according to the athletes’ individual characteristics, specific requirements, and training phases, adhering to the principles of individualization and periodization.
Physical conditioning is driven by systematic modulation of intensity, volume, frequency, and recovery. Wrist photoplethysmography (PPG) provides generally accurate heart rate (HR) for zone-based prescription, whereas energy-expenditure estimates are unreliable at higher intensities. Standardized heart-rate variability (HRV) reflects autonomic balance and recovery status, and inertial measurement units (IMUs) provide spatiotemporal gait and running metrics (cadence, stride length, contact time) that flag fatigue-related technique drift and asymmetry. Fusing HR/HRV with IMU outputs constrains training zones more robustly, minimizing cumulative injury risk while improving adaptation specificity [17,18,19,39,42,60,61,62,63].
Using an ISO/NASA 1–9 TRL frame: PPG-HR is high-TRL (≈8–9) with multi-brand field validation; HRV in sport is mid-to-high TRL (≈6–7) but hinges on strict standardization (posture, time-of-day, breathing, sleep) to ensure repeatability; IMU spatiotemporal running metrics are high-TRL (≈7–8) with solid concurrent validity and test–retest reliability; by contrast, sweat lactate for real-time load regulation remains prototypical (low TRL ≈ 3–4) due to sweat-rate variability and uncertain sweat–blood mapping, so it should currently augment—not drive—training decisions. Key adoption barriers include motion/phenotype effects on PPG/HRV, IMU placement/alignment consistency across sessions, and context-specific calibration/thresholding for sweat analytics [17,18,19,39,42,60,61,62,63].
3.2. Technical Training
Technical training in sports constitutes a systematic process aimed at optimizing the accuracy, consistency, and biomechanical efficiency of movements through quantitative analysis and targeted correction of critical components within specific sport skills (e.g., kinematic sequences, force transmission pathways, and temporal coordination patterns). Its primary objective is to establish movement patterns that conform to the mechanical principles governing the human kinetic chain. In practice, training plans need to be dynamically adjusted in combination with athletes’ individual movement characteristics and specific technical standards.
Technical training aims to optimize accuracy, consistency, and mechanical efficiency via quantitative analysis and targeted correction. IMUs provide joint/segment timing and angles; in-shoe pressure systems deliver plantar-pressure maps and contact events as surrogates for ground reaction forces (GRFs); together they enable rapid, field-based feedback for high-speed, highly coordinated skills. Evidence from judged and cyclic sports shows feasibility across take-off, flight, and landing phases with actionable feedback loops [24,64,65,66,67,68,69,70,71,72,73].
A pelvis and bilateral thigh IMU configuration (sagittal angular kinematics) combined with bilateral in-shoe pressure sensors (contact onset, peak pressure, force–time surrogates) can quantify on-track: (i) reaction time (start signal synchronized to first plantar-pressure rise/hand release; audio trigger if instrumented blocks are unavailable); (ii) push-off and block-exit asymmetry (bilateral peak pressure and impulse ratios); and (iii) early-step spatiotemporal metrics (step length/time for the first two steps) and pelvic tilt, which relate to initial horizontal velocity. These metrics align with known determinants of start performance (propulsive block forces, first-stance contact time, angular-momentum control) and have been benchmarked against force plates/instrumented blocks or laser + IMU references, enabling concrete corrections such as shortening block contact, constraining excessive anterior pelvic tilt, reducing bilateral force asymmetry, and optimizing hip timing at touchdown [24,64,65,66,67,68,69,70,71,72,73].
IMU step-to-step kinematics in high-speed running show validated agreement with optical/laser/force-plate references (mid-to-high TRL ≈ 6–8). Pressure insoles yield reliable vGRF trends and contact events but may underestimate peak loads in high-impact phases (mid-to-high TRL ≈ 6–7). Adoption barriers include multi-device synchronization and time alignment, sampling-rate demands, context-specific pressure-to-force mapping, and integration into coaching workflows (real-time visualization, minimal KPI sets) [24,64,65,66,67,68,69,70,71,72,73].
3.3. Tactical Training
Tactical training in sports training refers to a training process that, based on specific competitive rules and opponent characteristics, systematically designs offensive and defensive strategies, positional coordination patterns, and dynamic response plans to optimize the decision-making efficiency and execution consistency of teams or individuals in competition scenarios. Its core goal is to establish a tactical cognition and behavioral coordination system that meets the needs of competitive situations. Through training that simulates strategy implementation, role collaboration, and situational transitions under competitive pressure, it improves the accuracy, adaptability of tactical execution, and the overall effectiveness of the team. In practice, training plans need to be dynamically adjusted in combination with opponent analysis, venue characteristics, and the individual tactical roles of athletes.
In team sports (e.g., football/soccer, basketball, rugby), GPS, LPS, and IMU plus HR form multi-level position, velocity, and load databases that quantify collective behaviors, namely, team centroid, surface area/convex hull, stretch index, and synchrony, across pressing, transitions, and compactness, while integrating external and internal load for contextualized decisions [14,50,74].
Wearable position/velocity tracking has standardized performance evaluation within FIFA’s Electronic Performance and Tracking Systems (EPTS) program and is high-TRL (≈8–9). However, collective tactical metrics show context-dependent reliability/sensitivity (sampling rate, algorithms, occlusion/indoor conditions), placing them mid-to-high TRL (≈6–7). Barriers include cross-system comparability, position errors under crowding/indoor conditions, and limited translation from metrics to coaching decision rules (e.g., thresholding for formation compactness or pressing triggers) [14,50,68,74].

Table 1.
Mapping of sensor–application units to outputs, validation, standards alignment, gates, and indicative TRL.
Table 1.
Mapping of sensor–application units to outputs, validation, standards alignment, gates, and indicative TRL.
| Sens × Use-case | Primary Outputs | Validation Anchors (Refs) | V3/ESF Alignment | Gates Triggered | Indicative TRL (Range) | Notes |
|---|---|---|---|---|---|---|
| Wrist * PPG → HR zone prescription | HR, HR zones | ECG/chest-strap comparisons [17,60,61] | * V✓/A✓/C△ | * — | 8–9 | Field-validated across sports; energy-expenditure (* EE) estimates not used for decisions. |
| * IMU (pelvis/thigh)→ sprint start profiling | Step time/length, pelvic tilt | Force-plate/laser + IMU [24,64,65,66] | * V✓/A✓/C△ | * — | 6–8 | Requires high sampling and precise synchronization; align sensor frames consistently. |
| In-shoe pressure → * vGRF trend and contacts | Plantar pressure, contact events | Force-plate comparisons [50] | * V✓/A✓/C△ | Peak underestimation → cap | 6–7 | Peaks may be underestimated in high-impact tasks; task-/shoe-specific calibration recommended. |
| Sweat lactate → real-time load regulation | [Lac], sweat rate | Sweat–blood mapping studies [39,62] | * V△/A△/C△ | No actionable thresholds → cap | 3–4 | High inter-/intra-subject variability; use as adjunct signal, not primary driver. |
| CGM (interstitial) → fueling/pacing support | Glucose dynamics | Athlete reviews/pilot studies [42] | * V✓/A✓/C△ | * — | 5–6 | Cautious use in non-diabetic athletes; interpret with nutrition/medical oversight. |
| GPS/LPS/* IMU (tactical) → formation compactness | Position, velocity; centroid/surface/stretch index | FIFA EPTS; positional-data reviews [14,68,74] | * V✓/A✓/C△ | Collective metric sensitivity/context dependence → cap | 8–9 (tracking); 6–7 (collective metrics) | Cross-system comparability issues; indoor/occlusion errors may increase. |
* Abbreviations: PPG, photoplethysmography; IMU, inertial measurement unit; vGRF, vertical ground reaction force. V/A/C, DiMe V3 layers (Verification/Analytical/Clinical); “✓” indicates being basically in place; “△” indicates insufficient evidence or being contextualized ESF, NICE Evidence Standards Framework; EE, energy expenditure. “—“ indicates “not applicable”. Notes: Gate caps applied: no field reference—TRL ≤ 5; lack of standards/guidance—TRL ≤ 7; no actionable thresholds/real-time feedback—TRL ≤ 6.
4. Limitations and Practical Barriers
4.1. Sensor Accuracy and Robustness in Intense, Dynamic Movement (Signal Noise and Motion Artifacts)
During intense, dynamic movement, optical and inertial signals are vulnerable to motion artifacts, soft-tissue oscillations, and sensor micro-slippage. Wrist-PPG HR errors grow with vigorous arm swing and at high intensities; energy-expenditure estimates are particularly unreliable across brands [17,18,60]. Lower-limb IMU step-to-step metrics generally agree with optical/laser/force-plate references but are sensitive to placement/alignment, magnetic disturbance, and sampling-rate limits [64,68]. In-shoe pressure systems capture contact events and vGRF trends yet may underestimate peaks during high-impact tasks, requiring task- and shoe-specific calibration [50,62].Limited by the aforementioned factors, there are often few options for the placement of wearable devices (as illustrated in Figure 2).
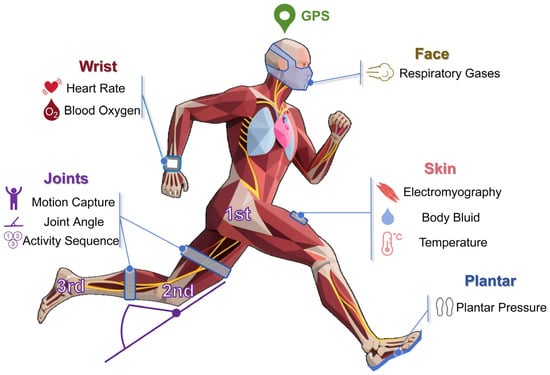
Figure 2.
Common body parts and metrics for training monitoring. The rapid development of related technologies has enabled wearable sensors to find numerous applications in fields such as healthcare, energy, and the environment. However, the types of sensors used in the training monitoring field are relatively limited. Due to the complexity of sports training movements, wearable sensors must minimize their impact on athletes as much as possible.
4.2. Inter-Individual Variability and Model Generalization
Marked inter-individual and regional variability exists: HR/PPG depends on skin tone and perfusion [17,60]; HRV requires strict standardization and individual baselines to be interpretable [19,61]; sweat analytics are shaped by sweat rate and site, with unstable sweat–blood mapping that impedes threshold transfer [24,65,66]. Hence, one-size-fits-all models are brittle; personalized or hierarchical modeling with multi-site datasets is needed.
4.3. Data Fusion and Threshold Transfer (Bridging Measurement to Decision)
Multi-sensor fusion often degrades in the wild due to latency, synchronization, packet loss, and cross-system algorithmic differences, with collective tactical metrics particularly sensitive to sampling-rate and context (indoor/occlusion/crowding) [14,68]. Emerging biomarkers (e.g., sweat lactate) still lack actionable thresholds and on-field feedback workflows [65,66].
4.4. Energy Consumption, Battery Life, and Wearability
High-rate sensing and wireless streaming strain battery life; energy density and form factor limit 24/7 capture. Some epidermal/adhesive systems cause irritation, discomfort, or detachment, hurting compliance and continuity [6,75]. Energy optimization and harvesting are advancing, yet self-powered operation without sacrificing signal quality/rate remains challenging [6,75].
4.5. Data Security, Privacy, and Ownership of Athlete Biometrics
Athlete biometrics are sensitive personal data. Lawful processing requires compliance with GDPR and robust privacy-information management; in sport, charters such as the FIFPRO Player Data Rights emphasize transparency, consent, access/erasure, portability, and secondary-use limits [76,77]. Ownership and sharing across teams and vendors remain unsettled, posing ethical and compliance risks.
4.6. User Compliance, Comfort, and Accessibility (Cost and Equity)
Comfort, minimal interference, and esthetics determine long-term adherence [6,75]. Device/service/infrastructure costs constrain grassroots adoption; for some technologies (e.g., CGM in non-diabetic athletes), evidence and regulation are evolving, limiting access and equity [5,6,67].
5. Summary and Outlook
Biosensors and bioelectronic devices show substantial promise for exercise monitoring. Current systems integrate multidimensional biosignal sensors—such as electromyography (EMG), blood oxygen saturation (SpO2), heart rate variability (HRV), and lactate measurement—into wearable platforms to capture athletes’ physiological and kinematic status in real time. These platforms acquire comprehensive, high-resolution data reflecting internal and external training loads, providing an evidence base for designing and continuously optimizing personalized programs and for the early detection and prevention of sport-related injuries. By delivering real-time feedback on physiological thresholds and biomechanical parameters, athletes and coaches can implement evidence-based adjustments that improve training efficacy and safety.
In parallel, the adoption of advanced materials, such as flexible electronic skins, textile-integrated sensors, and smart sportswear, has markedly improved the comfort, stability, and noninvasiveness of data acquisition during dynamic activity. These innovations support prolonged wear and continuous monitoring under complex movement conditions without disrupting natural biomechanics. Consequently, long-term tracking of training adaptations, fatigue accumulation, and recovery progression has become more feasible and acceptable in both professional and recreational sport settings. Therefore, innovations in fields such as materials and algorithms can effectively drive the development of wearable sensors in the field of motion detection (as illustrated in Figure 3).
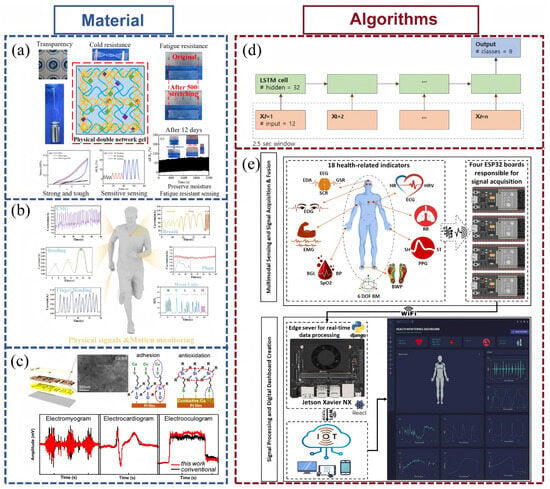
Figure 3.
Advanced technologies for wearable sensors applied to exercise monitoring. (a) The PHA/Agar/EG hydrogel-based flexible sensor monitors different human motions and physiological activities [78]. (b) A multifunctional, integrated, flexible sensing platform based on biocompatible graphene/bacterial cellulose bioaerogel can be used for real-time monitoring of human health characteristic [79], and is reprinted (adapted) with permission from [19], Copyright 2023 Elsevier. (c) Nanophotonic-Sintered Copper Membrane with Ultrahigh Conductivity for Electrodes of Wearable Flexible Sensors [80]. (d) A “many-to-one” Long Short-Term Memory architecture for the classification of 9 types of human activities [81]. (e) An intelligent, IoT-enabled wearable multi-modal biosensing device [82] reprinted (adapted) with permission from [22], Copyright 2025 Elsevier.
Looking forward, the field is poised to advance in precision, intelligence, and system integration. On the one hand, breakthroughs in materials science, especially pressure-sensitive materials [78], biodegradable substrates [79], and biocompatible conductive polymers [80], will enable further miniaturization, higher sensitivity, greater flexibility, and long-term skin compatibility. These gains can mitigate current limitations such as signal instability, motion artifacts, and adherence issues, supporting robust, unobtrusive data capture across varied training environments.
On the other hand, the deep integration of multimodal data fusion algorithms with artificial intelligence (AI) and machine learning (ML) frameworks will transform wearable systems from passive data collectors into active decision-support platforms [81,82]. By interpreting large-scale, heterogeneous biosignals, such systems can deliver real-time, personalized training recommendations, injury-risk estimates, and recovery guidance. Furthermore, establishing closed-loop systems that span data acquisition and preprocessing through adaptive feedback and automatic adjustment of training prescriptions will markedly improve the autonomy and responsiveness of digital training support platforms.
Materials and AI co-design will shift wearables from “measurable” to “actionable.” Conductive hydrogels provide a skin-sensor interface with high conductivity, strong adhesion, self-healing, and all-weather stability, preserving contact under large strain and cold to suppress motion artifacts. Coupled with lightweight on-device intelligence for context recognition, multimodal fusion, and personalized self-calibration, cleaner signals can be converted into low-latency, actionable training cues. This synergy targets long-term stability, comfort, and in-field calibration, accelerating deployment across the physical, technical, and tactical pillars [83,84].
This review contributes by mapping four wearable data domains, physiological, kinematic, biochemical, and dynamic, onto three training pillars: physical, technical, and tactical, thereby turning “what we can measure” into “what we can do,” quantified with use-case TRLs and operationalized through a quality control (QC), threshold, and feedback loop. The three pillars target load appropriateness (physical), movement economy (technical), and team coordination (tactical), aligning with core training objectives. For athletes, wearables should be light, stable, low latency, and provide concise cues anchored to personal baselines, with transparent privacy and data ownership; for coaches and teams, outputs should condense into on-screen thresholds and prescription suggestions with robust QC, cross-context reliability, and workflow compatibility. Future work should prioritize threshold-driven intervention trials, multi-site personalized and hierarchical modeling, and regularly updated use-case TRL assessments, advancing wearables from signal availability to true decision utility.
Author Contributions
Writing—original draft preparation, B.S. (Bo Su), F.L., B.S. (Bingtian Su); Writing—review and editing, B.S. (Bo Su), F.L., B.S. (Bingtian Su). All authors have read and agreed to the published version of the manuscript.
Funding
This work is supported by the National Natural Science Foundation of China (22474049) and the National Key R&D Program of China (2023YFC2414504).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study.
Acknowledgments
During the preparation of this manuscript, the authors used ChatGPT (OpenAI; model: GPT-5 Thinking; accessed October 2025) to assist language polishing (grammar, style, punctuation), punctuation normalization, and reference formatting in ACS style. All AI-assisted text was reviewed and edited by the authors, who take full responsibility for the content.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Bourdon, P.C.; Cardinale, M.; Murray, A.; Gastin, P.; Kellmann, M.; Varley, M.C.; Gabbett, T.J.; Coutts, A.J.; Burgess, D.J.; Gregson, W.; et al. Monitoring Athlete Training Loads: Consensus Statement. Int. J. Sports Physiol. Perform. 2017, 12, S2-161–S2-170. [Google Scholar] [CrossRef]
- Smith, J.A.B.; Murach, K.A.; Dyar, K.A.; Zierath, J.R. Exercise metabolism and adaptation in skeletal muscle. Nat. Rev. Mol. Cell Biol. 2023, 24, 607–632. [Google Scholar] [CrossRef] [PubMed]
- Landen, S.; Hiam, D.; Voisin, S.; Jacques, M.; Lamon, S.; Eynon, N. Physiological and molecular sex differences in human skeletal muscle in response to exercise training. J. Physiol. 2021, 601, 419–434. [Google Scholar] [CrossRef] [PubMed]
- Eline, V.D.K.; Reijne., M.M. Accuracy of human motion capture systems for sport applications; state-of-the-art review. Eur. J. Sport Sci. 2018, 18, 806–819. [Google Scholar]
- Halson, S.L. Monitoring training load to understand fatigue in athletes. Sports Med. 2014, 44 (Suppl. S2), 139–147. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the internal and external workload of the athlete. npj Digit. Med. 2019, 2, 71. [Google Scholar] [CrossRef]
- Adesida, Y.; Papi, E.; McGregor, A.H. Exploring the Role of Wearable Technology in Sport Kinematics and Kinetics: A Systematic Review. Sensors 2019, 19, 1597. [Google Scholar] [CrossRef]
- Aroganam, G.; Manivannan, N.; Harrison, D. Review on Wearable Technology Sensors Used in Consumer Sport Applications. Sensors 2019, 19, 1983. [Google Scholar] [CrossRef] [PubMed]
- Fuller, D.; Colwell, E.; Low, J.; Orychock, K.; Tobin, M.A.; Simango, B.; Buote, R.; Van Heerden, D.; Luan, H.; Cullen, K.; et al. Reliability and Validity of Commercially Available Wearable Devices for Measuring Steps, Energy Expenditure, and Heart Rate: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e18694. [Google Scholar] [CrossRef]
- Doherty, C.; Baldwin, M.; Keogh, A.; Caulfield, B.; Argent, R. Keeping Pace with Wearables: A Living Umbrella Review of Systematic Reviews Evaluating the Accuracy of Consumer Wearable Technologies in Health Measurement. Sports Med. 2024, 54, 2907–2926. [Google Scholar] [CrossRef]
- Scataglini, S.; Abts, E.; Van Bocxlaer, C.; Bussche, M.V.D.; Meletani, S.; Truijen, S. Accuracy, Validity, and Reliability of Markerless Camera-Based 3D Motion Capture Systems versus Marker-Based 3D Motion Capture Systems in Gait Analysis: A Systematic Review and Meta-Analysis. Sensors 2024, 24, 3686. [Google Scholar] [CrossRef] [PubMed]
- Soligard, T.; Schwellnus, M.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, F.M.; Marcora, S.M.; Coutts, A.J. Internal and External Training Load: 15 Years On. Int. J. Sports Physiol. Perform. 2019, 14, 270–273. [Google Scholar] [CrossRef]
- Teixeira, J.E.; Forte, P.; Ferraz, R.; Branquinho, L.; Silva, A.J.; Monteiro, A.M.; Barbosa, T.M. Integrating physical and tactical factors in football using positional data: A systematic review. PeerJ 2022, 10, e14381. [Google Scholar] [CrossRef]
- Mahato, K.; Saha, T.; Ding, S.; Sandhu, S.S.; Chang, A.-Y.; Wang, J. Hybrid multimodal wearable sensors for comprehensive health monitoring. Nat. Electron. 2024, 7, 735–750. [Google Scholar] [CrossRef]
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Rose, S.M.S.-F.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLOS Biol. 2017, 15, e2001402. [Google Scholar] [CrossRef]
- Shcherbina, A.; Mattsson, C.M.; Waggott, D.; Salisbury, H.; Christle, J.W.; Hastie, T.; Wheeler, M.T.; Ashley, E.A. Accuracy in Wrist-Worn, Sensor-Based Measurements of Heart Rate and Energy Expenditure in a Diverse Cohort. J. Pers. Med. 2017, 7, 3. [Google Scholar] [CrossRef]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef]
- Plews, D.J.; Laursen, P.B.; Stanley, J.; Kilding, A.E.; Buchheit, M. Training Adaptation and Heart Rate Variability in Elite Endurance Athletes: Opening the Door to Effective Monitoring. Sports Med. 2013, 43, 773–781. [Google Scholar] [CrossRef]
- Dolson, C.M.; Harlow, E.R.; Phelan, D.M.; Gabbett, T.J.; Gaal, B.; McMellen, C.; Geletka, B.J.; Calcei, J.G.; Voos, J.E.; Seshadri, D.R. Wearable Sensor Technology to Predict Core Body Temperature: A Systematic Review. Sensors 2022, 22, 7639. [Google Scholar] [CrossRef]
- Kato, I.; Watanabe, H.; Nagashima, K. Evaluation of newly developed wearable ear canal thermometer, mimicking the application to activities on sports and labor fields. J. Physiol. Sci. 2023, 73, 15–19. [Google Scholar] [CrossRef]
- Klimek, A.; Mannheim, I.; Schouten, G.; Wouters, E.J.M.; Peeters, M.W.H. Wearables measuring electrodermal activity to assess perceived stress in care: A scoping review. Acta Neuropsychiatr. 2023, 37, e19. [Google Scholar] [CrossRef]
- Almadhor, A.; Sampedro, G.A.; Abisado, M.; Abbas, S.; Kim, Y.-J.; Khan, M.A.; Baili, J.; Cha, J.-H. Wrist-Based Electrodermal Activity Monitoring for Stress Detection Using Federated Learning. Sensors 2023, 23, 3984. [Google Scholar] [CrossRef] [PubMed]
- Zeng, Z.; Liu, Y.; Hu, X.; Tang, M.; Wang, L. Validity and Reliability of Inertial Measurement Units on Lower Extremity Kinematics During Running: A Systematic Review and Meta-Analysis. Sports Med.-Open 2022, 8, 86. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.; Pearson, L.T.; Barry, G.; Young, F.; Lennon, O.; Godfrey, A.; Stuart, S. Wearables for Running Gait Analysis: A Systematic Review. Sports Med. 2023, 53, 241–268. [Google Scholar] [CrossRef]
- Mason, R.; Barry, G.; Robinson, H.; O’cAllaghan, B.; Lennon, O.; Godfrey, A.; Stuart, S. Validity and reliability of the DANU sports system for walking and running gait assessment. Physiol. Meas. 2023, 44, 115001. [Google Scholar] [CrossRef]
- Cereatti, A.; Gurchiek, R.; Mündermann, A.; Fantozzi, S.; Horak, F.; Delp, S.; Aminian, K. ISB recommendations on the definition, estimation, and reporting of joint kinematics in human motion analysis applications using wearable inertial measurement technology. J. Biomech. 2024, 173, 112225. [Google Scholar] [CrossRef]
- Rhudy, M.B.; Mahoney, J.M.; Altman-Singles, A.R. Knee Angle Estimation with Dynamic Calibration Using Inertial Measurement Units for Running. Sensors 2024, 24, 695. [Google Scholar] [CrossRef]
- Chen, H.; Schall, M.C.; Martin, S.M.; Fethke, N.B. Drift-Free Joint Angle Calculation Using Inertial Measurement Units without Magnetometers: An Exploration of Sensor Fusion Methods for the Elbow and Wrist. Sensors 2023, 23, 7053. [Google Scholar] [CrossRef]
- Uhlenberg, L.; Amft, O. Where to mount the IMU? Validation of joint angle kinematics and sensor selection for activities of daily living. Front. Comput. Sci. 2024, 6, 1347424. [Google Scholar] [CrossRef]
- Baker, L.B. Sweating Rate and Sweat Sodium Concentration in Athletes: A Review of Methodology and Intra/Interindividual Variability. Sports Med. 2017, 47, 111–128. [Google Scholar] [CrossRef]
- Gao, F.; Liu, C.; Zhang, L.; Liu, T.; Wang, Z.; Song, Z.; Cai, H.; Fang, Z.; Chen, J.; Wang, J.; et al. Wearable and flexible electrochemical sensors for sweat analysis: A review. Microsyst. Nanoeng. 2023, 9, 1. [Google Scholar] [CrossRef] [PubMed]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the physiological and biochemical profile of the athlete. npj Digit. Med. 2019, 2, 72. [Google Scholar] [CrossRef]
- Jalal, N.R.; Madrakian, T.; Ahmadi, M.; Afkhami, A.; Khalili, S.; Bahrami, M.; Roshanaei, M. Wireless wearable potentiometric sensor for simultaneous determination of pH, sodium and potassium in human sweat. Sci. Rep. 2024, 14, 11526. [Google Scholar] [CrossRef]
- Bariya, M.; Nyein, H.Y.Y.; Javey, A. Wearable sweat sensors. Nat. Electron. 2018, 1, 160–171. [Google Scholar] [CrossRef]
- Chung, M.; Fortunato, G.; Radacsi, N. Wearable flexible sweat sensors for healthcare monitoring: A review. J. R. Soc. Interface 2019, 16, 20190217. [Google Scholar] [CrossRef]
- Torrente-Rodríguez, R.M.; Tu, J.; Yang, Y.; Min, J.; Wang, M.; Song, Y.; Yu, Y.; Xu, C.; Ye, C.; IsHak, W.W.; et al. Investigation of Cortisol Dynamics in Human Sweat Using a Graphene-Based Wireless mHealth System. Matter 2020, 2, 921–937. [Google Scholar] [CrossRef] [PubMed]
- Vignesh, V.; Castro-Dominguez, B.; James, T.D.; Gamble-Turner, J.M.; Lightman, S.; Reis, N.M. Advancements in Cortisol Detection: From Conventional Methods to Next-Generation Technologies for Enhanced Hormone Monitoring. ACS Sensors 2024, 9, 1666–1681. [Google Scholar] [CrossRef]
- Messina, L.; Giardi, M.T. Recent Status on Lactate Monitoring in Sweat Using Biosensors: Can This Approach Be an Alternative to Blood Detection? Biosensors 2024, 15, 3. [Google Scholar] [CrossRef]
- Bowler, A.-L.M.; Whitfield, J.; Marshall, L.; Coffey, V.G.; Burke, L.M.; Cox, G.R. The Use of Continuous Glucose Monitors in Sport: Possible Applications and Considerations. Int. J. Sport Nutr. Exerc. Metab. 2023, 33, 121–132. [Google Scholar] [CrossRef] [PubMed]
- Takei, N.; Inaba, T.; Morita, Y.; Kakinoki, K.; Hatta, H.; Kitaoka, Y. Differential patterns of sweat and blood lactate concentration response during incremental exercise in varied ambient temperatures: A pilot study. Temperature 2024, 11, 247–253. [Google Scholar] [CrossRef]
- Childs, A.; Mayol, B.; Lasalde-Ramírez, J.A.; Song, Y.; Sempionatto, J.R.; Gao, W. Diving into Sweat: Advances, Challenges, and Future Directions in Wearable Sweat Sensing. ACS Nano 2024, 18, 24605–24616. [Google Scholar] [CrossRef]
- Flockhart, M.; Larsen, F.J. Continuous Glucose Monitoring in Endurance Athletes: Interpretation and Relevance of Measurements for Improving Performance and Health. Sports Med. 2023, 54, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Bauhaus, H.; Erdogan, P.; Braun, H.; Thevis, M. Continuous Glucose Monitoring (CGM) in Sports—A Comparison between a CGM Device and Lab-Based Glucose Analyser under Resting and Exercising Conditions in Athletes. Int. J. Environ. Res. Public Heal. 2023, 20, 6440. [Google Scholar] [CrossRef]
- Lara, B.; Gallo-Salazar, C.; Puente, C.; Areces, F.; Salinero, J.J.; Del Coso, J. Interindividual variability in sweat electrolyte concentration in marathoners. J. Int. Soc. Sports Nutr. 2016, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.; Heikenfeld, J.; Milla, C.; Javey, A. The challenges and promise of sweat sensing. Nat. Biotechnol. 2024, 42, 860–871. [Google Scholar] [CrossRef]
- Ghaffari, R.; Yang, D.S.; Kim, J.; Mansour, A.; Wright, J.A.; Model, J.B.; Wright, D.E.; Rogers, J.A.; Ray, T.R. State of Sweat: Emerging Wearable Systems for Real-Time, Noninvasive Sweat Sensing and Analytics. ACS Sens. 2021, 6, 2787–2801. [Google Scholar] [CrossRef]
- Ibrahim, N.F.A.; Sabani, N.; Johari, S.; Manaf, A.A.; Wahab, A.A.; Zakaria, Z.; Noor, A.M. A Comprehensive Review of the Recent Developments in Wearable Sweat-Sensing Devices. Sensors 2022, 22, 7670. [Google Scholar] [CrossRef]
- Renner, K.E.; Williams, D.B.; Queen, R.M. The Reliability and Validity of the Loadsol® under Various Walking and Running Conditions. Sensors 2019, 19, 265. [Google Scholar] [CrossRef]
- Cudejko, T.; Button, K.; Al-Amri, M. Wireless pressure insoles for measuring ground reaction forces and trajectories of the centre of pressure during functional activities. Sci. Rep. 2023, 13, 14946. [Google Scholar] [CrossRef]
- Brindle, R.A.; Bleakley, C.M.; Taylor, J.B.; Queen, R.M.; Ford, K.R. Validity of estimating center of pressure during walking and running with plantar load from a three-sensor wireless insole. Wearable Technol. 2022, 3, e8. [Google Scholar] [CrossRef]
- Martínez-Cava, A.; Hernández-Belmonte, A.; Courel-Ibáñez, J.; Morán-Navarro, R.; González-Badillo, J.J.; Pallarés, J.G. Correction: Reliability of technologies to measure the barbell velocity: Implications for monitoring resistance training. PLoS ONE 2020, 15, e0236073. [Google Scholar] [CrossRef]
- Weakley, J.; Morrison, M.; García-Ramos, A.; Johnston, R.; James, L.; Cole, M.H. The Validity and Reliability of Commercially Available Resistance Training Monitoring Devices: A Systematic Review. Sports Med. 2021, 51, 443–502. [Google Scholar] [CrossRef]
- Tan, T.; Shull, P.B.; Hicks, J.L.; Uhlrich, S.D.; Chaudhari, A.S. Self-Supervised Learning Improves Accuracy and Data Efficiency for IMU-Based Ground Reaction Force Estimation. IEEE Trans. Biomed. Eng. 2024, 71, 2095–2104. [Google Scholar] [CrossRef]
- ISO 16290:2013; Space Systems—Definition of the Technology Readiness Levels (TRLs) and Their Criteria of Assessment. ISO: Geneva, Switzerland, 2013.
- Goldsack, J.C.; Dowling, A.V.; Samuelson, D.; Patrick-Lake, B.; Clay, I. Verification, analytical validation, and clinical validation (V3): The foundation of determining fit-for-purpose for Biometric Monitoring Technologies (BioMeTs). npj Digit. Med. 2020, 3, 55. [Google Scholar] [CrossRef]
- Bakker, J.P.; Barge, R.; Centra, J.; Cobb, B.; Cota, C.; Guo, C.C.; Hartog, B.; Horowicz-Mehler, N.; Izmailova, E.S.; Manyakov, N.V.; et al. V3+ extends the V3 framework to ensure user-centricity and scalability of sensor-based digital health technologies. npj Digit. Med. 2025, 8, 51. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Evidence Standards Framework for Digital Health Technologies (ESF); National Institute for Health and Care Excellence: Manchester, UK, 2022. [Google Scholar]
- Fédération Internationale de Football Association. EPTS Testing Process—FIFA Quality Programme for Electronic Performance & Tracking Systems; FIFA: Zurich, Switzerland, 2025. [Google Scholar]
- Wang, R.; Blackburn, G.; Desai, M.; Phelan, D.; Gillinov, L.; Houghtaling, P.; Gillinov, M. Accuracy of Wrist-Worn Heart Rate Monitors. JAMA Cardiol. 2017, 2, 104–106. [Google Scholar] [CrossRef]
- Düking, P.; Giessing, L.; Frenkel, M.O.; Koehler, K.; Holmberg, H.-C.; Sperlich, B. Wrist-Worn Wearables for Monitoring Heart Rate and Energy Expenditure While Sitting or Performing Light-to-Vigorous Physical Activity: Validation Study. JMIR mHealth uHealth 2020, 8, e16716. [Google Scholar] [CrossRef] [PubMed]
- Van Hoovels, K.; Xuan, X.; Cuartero, M.; Gijssel, M.; Swarén, M.; Crespo, G.A. Can Wearable Sweat Lactate Sensors Contribute to Sports Physiology? ACS Sens. 2021, 6, 3496–3508. [Google Scholar] [CrossRef] [PubMed]
- Baker, L.B.; Ungaro, C.T.; Sopeña, B.C.; Nuccio, R.P.; Reimel, A.J.; Carter, J.M.; Stofan, J.R.; Barnes, K.A. Body map of regional vs. whole body sweating rate and sweat electrolyte concentrations in men and women during moderate exercise-heat stress. J. Appl. Physiol. 2018, 124, 1304–1318. [Google Scholar] [CrossRef] [PubMed]
- Tillaar, R.v.D.; Nagahara, R.; Gleadhill, S.; Jiménez-Reyes, P. Step-to-Step Kinematic Validation between an Inertial Measurement Unit (IMU) 3D System, a Combined Laser+IMU System and Force Plates during a 50 M Sprint in a Cohort of Sprinters. Sensors 2021, 21, 6560. [Google Scholar] [CrossRef]
- Bezodis, N.E.; Willwacher, S.; Salo, A.I.T. The Biomechanics of the Track and Field Sprint Start: A Narrative Review. Sports Med. 2019, 49, 1345–1364. [Google Scholar] [CrossRef]
- Pain, M.T.G.; Hibbs, A. Sprint starts and the minimum auditory reaction time. J. Sports Sci. 2007, 25, 79–86. [Google Scholar] [CrossRef]
- Slawinski, J.; Bonnefoy, A.; Levêque, J.-M.; Ontanon, G.; Riquet, A.; Dumas, R.; Chèze, L. Kinematic and Kinetic Comparisons of Elite and Well-Trained Sprinters During Sprint Start. J. Strength Cond. Res. 2010, 24, 896–905. [Google Scholar] [CrossRef]
- Linke, D.; Lames, M. Validation of electronic performance and tracking systems EPTS under field conditions. PLoS ONE 2018, 13, e0199519. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, J.; Zhang, Y.; Zhu, R. A wearable motion capture device able to detect dynamic motion of human limbs. Nat. Commun. 2020, 11, 5615. [Google Scholar] [CrossRef]
- Liu, S.Q.; Zhang, J.C.; Li, G.-Z.; Zhu, R. A Wearable Flow-MIMU Device for Monitoring Human Dynamic Motion. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 637–645. [Google Scholar] [CrossRef]
- Li, G.-Z.; Zhao, S.; Zhu, R. Wearable Anemometer With Multi-Sensing of Wind Absolute Orientation, Wind Speed, Attitude, and Heading. IEEE Sens. J. 2018, 19, 297–303. [Google Scholar] [CrossRef]
- Schümperlin, D.; Schärer, C.; Kalberer, L.; Ferguson, S.J.; Lorenzetti, S.R. Pilot study: Validity and reliability of textile insoles used to measure the characteristics of landing tasks during rehabilitation and artistic gymnastics. BMC Res. Notes 2023, 16, 59. [Google Scholar] [CrossRef] [PubMed]
- Willwacher, S.; Herrmann, V.; Heinrich, K.; Funken, J.; Strutzenberger, G.; Goldmann, J.-P.; Braunstein, B.; Brazil, A.; Irwin, G.; Potthast, W.; et al. Sprint Start Kinetics of Amputee and Non-Amputee Sprinters. PLoS ONE 2016, 11, e0166219. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rico-González, M.; Ortega, J.; Nakamura, F.; Moura, F.; Arcos, A. Identification, Computational Examination, Critical Assessment and Future Considerations of Spatial Tactical Variables to Assess the Use of Space in Team Sports by Positional Data: A Systematic Review. J. Hum. Kinet. 2021, 77, 205–221. [Google Scholar] [CrossRef]
- Stoppa, M.; Chiolerio, A. Wearable Electronics and Smart Textiles: A Critical Review. Sensors 2014, 14, 11957–11992. [Google Scholar] [CrossRef]
- Regulation, Protection. Regulation (EU) 2016/679 of the European Parliament and of the Council. Off. J. Eur. Union 2016, 679, 10–13. [Google Scholar]
- Fifpro. Charter of Player Data Rights. Available online: https://fifpro.org/en/supporting-players/competitions-innovation-and-growth/player-performance-data/charter-of-player-data-rights-launched-for-professional-footballers (accessed on 30 July 2025).
- Yang, J.; Kang, Q.; Zhang, B.; Fang, X.; Liu, S.; Qin, G.; Chen, Q. Strong, tough, anti-freezing, non-drying and sensitive ionic sensor based on fully physical cross-linked double network hydrogel. Mater. Sci. Eng. C 2021, 130, 112452. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Xiu, K.; Wang, Z.; Hu, N.; Zhao, L.; Zhu, H.; Kong, F.; Xiao, J.; Cheng, L.; Bi, X. Multifunctional wearable humidity and pressure sensors based on biocompatible graphene/bacterial cellulose bioaerogel for wireless monitoring and early warning of sleep apnea syndrome. Nano Energy 2023, 108, 108215. [Google Scholar] [CrossRef]
- Kwon, Y.-T.; Kim, Y.-S.; Lee, Y.; Kwon, S.; Lim, M.; Song, Y.; Choa, Y.-H.; Yeo, W.-H. Ultrahigh Conductivity and Superior Interfacial Adhesion of a Nanostructured, Photonic-Sintered Copper Membrane for Printed Flexible Hybrid Electronics. ACS Appl. Mater. Interfaces 2018, 10, 44071–44079. [Google Scholar] [CrossRef]
- Chung, S.; Lim, J.; Noh, K.J.; Kim, G.; Jeong, H. Sensor Data Acquisition and Multimodal Sensor Fusion for Human Activity Recognition Using Deep Learning. Sensors 2019, 19, 1716. [Google Scholar] [CrossRef] [PubMed]
- Assaad, R.H.; Mohammadi, M.; Poudel, O. Developing an Intelligent IoT-enabled Wearable Multimodal Biosensing Device and Cloud-Based Digital Dashboard for Real-Time and Comprehensive Health, Physiological, Emotional, and Cognitive Monitoring Using Multi-Sensor Fusion Technologies. Sens. Actuators A Phys. 2024, 381, 116074. [Google Scholar] [CrossRef]
- Han, F.; Chen, S.; Wang, F.; Liu, M.; Li, J.; Liu, H.; Yang, Y.; Zhang, H.; Liu, D.; He, R.; et al. High-Conductivity, Self-Healing, and Adhesive Ionic Hydrogels for Health Monitoring and Human-Machine Interactions Under Extreme Cold Conditions. Adv. Sci. 2025, 12, e2412726. [Google Scholar] [CrossRef]
- Wu, J.; Hong, J.; Gao, X.; Wang, Y.; Wang, W.; Zhang, H.; Park, J.; Shi, W.; Guo, W. Recent Progress in Flexible Wearable Sensors Utilizing Conductive Hydrogels for Sports Applications: Characteristics, Mechanisms, and Modification Strategies. Gels 2025, 11, 589. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).