Development of a Multiplex HIV/TB Diagnostic Assay Based on the Microarray Technology
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
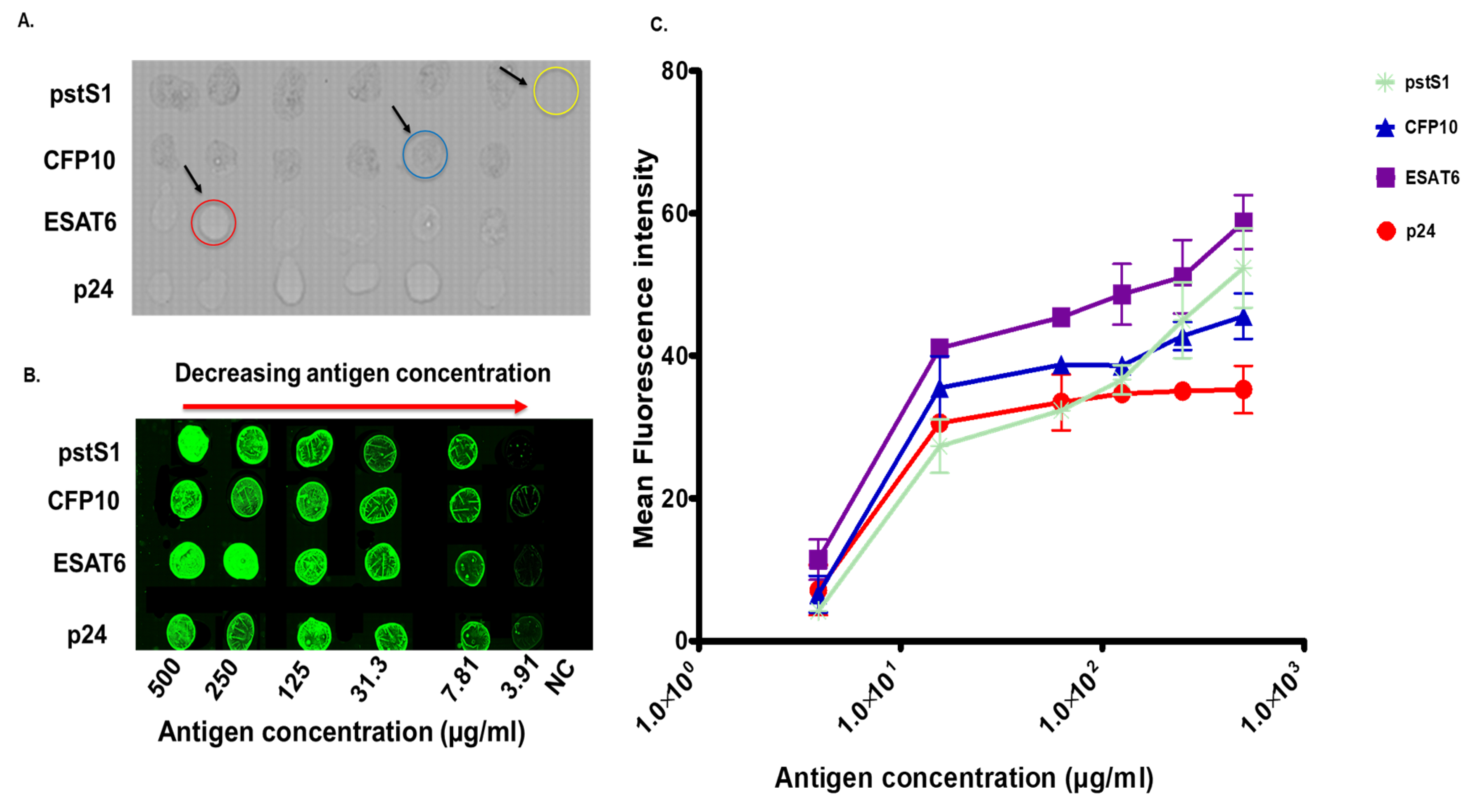
2.2. Immobilization of HIV-1 p24 as Well as M.tb CFP10 ESAT6 and pstS1 Antigens on Epoxy-Coated Glass Slides
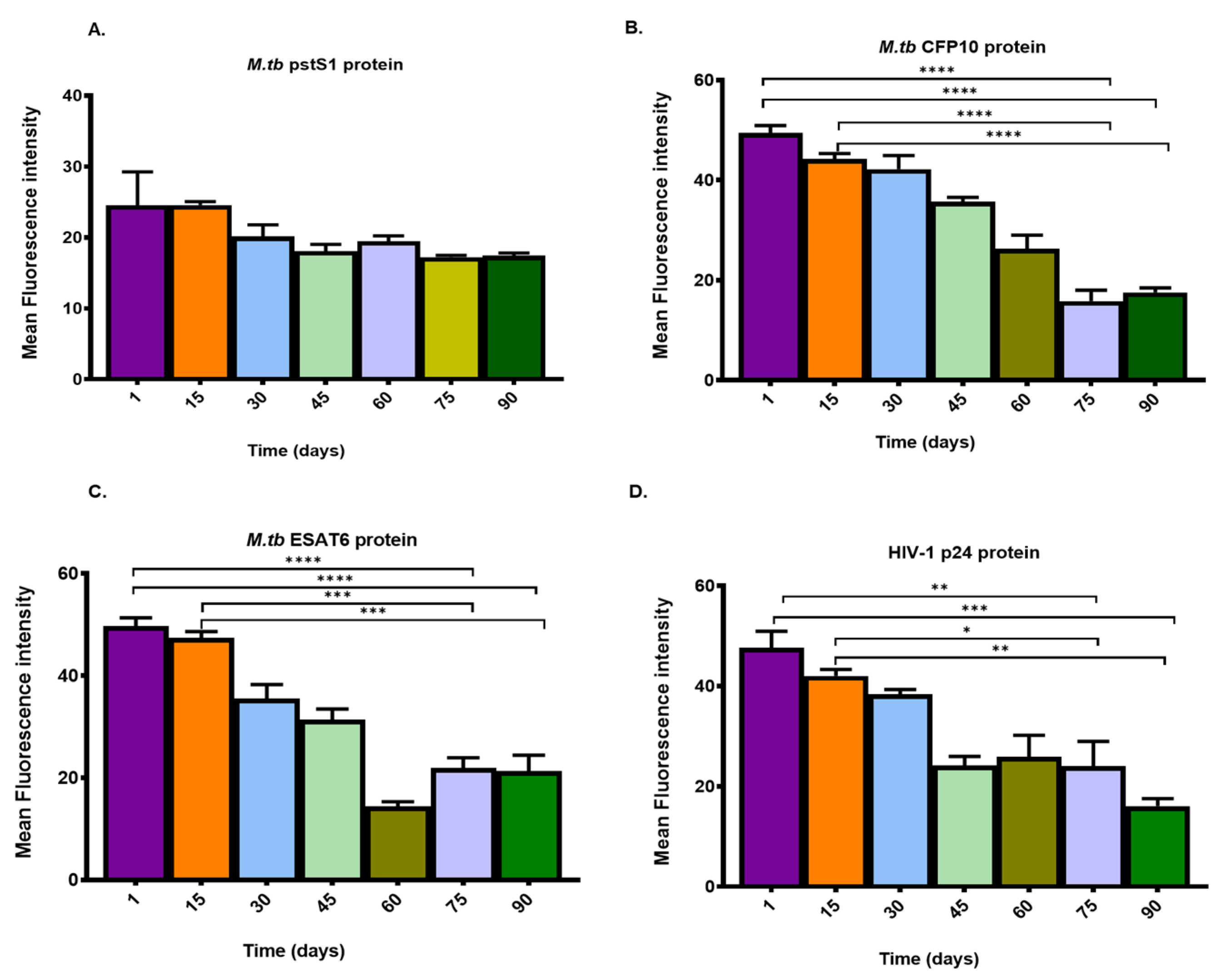
2.3. Determination of the Optimal Buffer pH, Storage Condition, Temperature and Shelf-Life of Immobilized HIV and TB Antigens
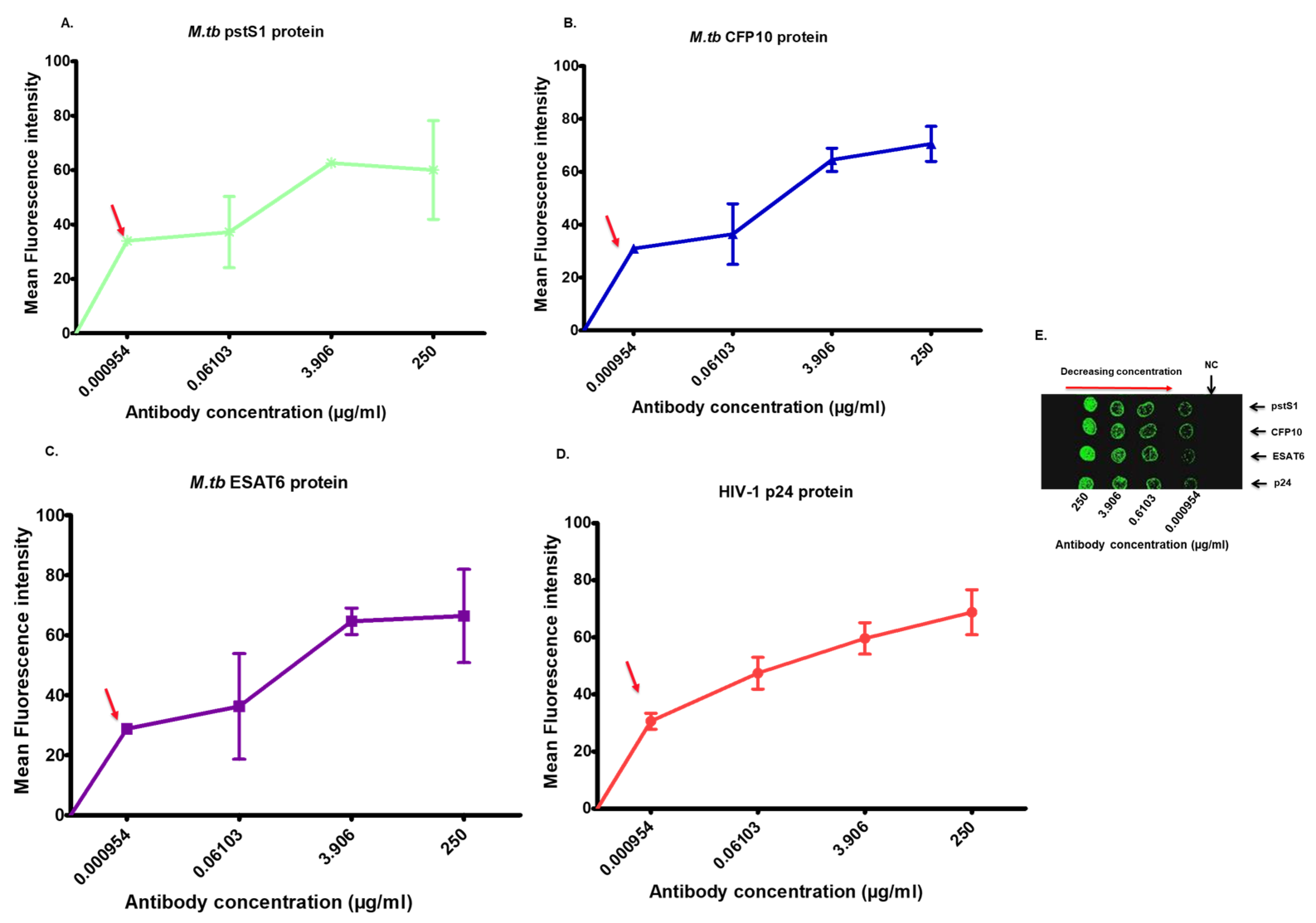
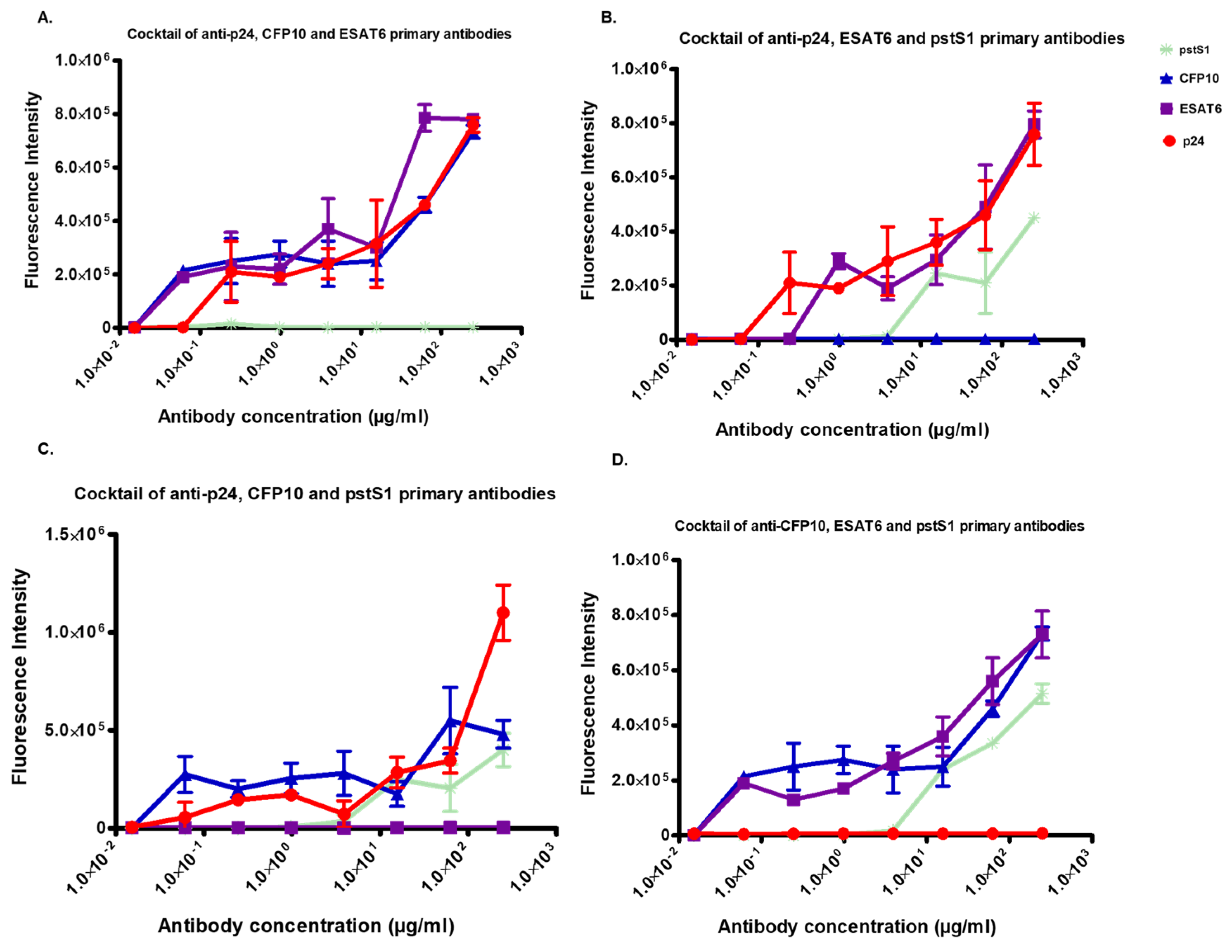
2.4. In Vitro Specificity and Sensitivity of the Microarray-Based Detection System for HIV and M.tb Antibodies
2.5. Statistical Analysis
3. Results
3.1. Immobilization of Antigens on Epoxy-Coated Glass Slides
3.2. Investigation of the Stability of Immobilized Antigens on the Epoxy-Coated Glass Slides
3.3. Comparison of the Antigen–Antibody Reactions between the Microarray Epoxy-Coated Slide Platform and the Protein Polystyrene High-Binding Plates
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A


| Method | Used Material | Target Matrix | Limit of Detection (LOD) |
|---|---|---|---|
| Multiplex HIV/TB microarray technology | -CFP10, ESAT6, pstS1 and p24 antigens and primary antibodies -Alexa fluor-conjugated secondary antibodies for fluorescence detection | -Human serum | -CFP10, ESAT6, pstS1 and p24 antibodies LOD of 0.000954 µg/mL |
| Electrochemical impedimetric ESAT-6 immunosensor [52] | -ESAT6 proteins and monoclonal antibodies -Label free (uses Ultrasensitive electrochemical immunosensors) | -Mice serum samples | -ESAT 6 protein LOD of 7.0 × 10−6 µg/ml |
| Gold Nanoparticle (AuNps)-based Lateral flow TB immunoassay [53] | -ESAT6 and CFP10 antibodies and antigens -AuNps-conjugated antibodies for colorimetric labelling | -Non-sputum samples | -ESAT6 antigen LOD of 0.0000625 µg/mL -CFP10 antigen LOD of 0.00769 µg/ml |
| HIV p24 detection using combined immunoprecipitation and digital ELISA [54] | -p24 antigen and p24 monoclonal antibodies -Biotin-labelled anti-p24 antibody | -Cell lysate | -p24 protein LOD of 5.0 × 10−9 µg/mL |
References
- UNIAIDS. Global HIV & AIDS Statistics—Fact Sheet. 2021, pp. 1–7. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 20 September 2022).
- Antony, B.; Tiewsoh, J.B.A.; Boloor, R. HIV-TB co-infection with clinical presentation, diagnosis, treatment, outcome and its relation to CD4 count, a cross-sectional study in a tertiary care hospital in coastal Karnataka. J. Fam. Med. Prim. Care 2020, 9, 1160–1165. [Google Scholar] [CrossRef]
- Ríos-Hincapié, C.Y.; Rojas, M.; López, M.; Porras, A.; Luque, R.; Pelissari, D.M.; López, L.; Rueda, Z.V. Delays in HIV and TB diagnosis and treatment initiation in co-infected patients in Colombia. Int. J. STD AIDS 2020, 31, 410–419. [Google Scholar] [CrossRef]
- Dewan, R.; Anuradha, S.; Khanna, A.; Garg, S.; Singla, S.; Ish, P.; Agarwal, S.; Narayana, H.A.; Hanif, M.; Singh, H.; et al. Role of cartridge-based nucleic acid amplification test (CBNAAT) for early diagnosis of pulmonary tuberculosis in HIV. Indian Acad. Clin. Med. 2015, 16, 114–117. [Google Scholar]
- Scott, L.; da Silva, P.; Boehme, C.C.; Stevens, W.; Gilpin, C. Diagnosis of opportunistic infections: HIV co-infections-tuberculosis. Curr. Opin. Hiv Aids 2017, 12, 129–138. [Google Scholar] [CrossRef]
- Cheon, S.A.; Cho, H.H.; Kim, J.; Lee, J.; Kim, H.-J.; Park, T.J. Recent tuberculosis diagnosis toward the end TB strategy. J. Microbiol. Methods 2016, 123, 51–61. [Google Scholar] [CrossRef]
- Gina, P.; Randall, P.J.; Muchinga, T.E.; Pooran, A.; Meldau, R.; Peter, J.G.; Dheda, K. Early morning urine collection to improve urinary lateral flow LAM assay sensitivity in hospitalised patients with HIV-TB co-infection. BMC Infect. Dis. 2017, 17, 339. [Google Scholar] [CrossRef]
- Ryu, Y.J. Diagnosis of Pulmonary Tuberculosis: Recent Advances and Diagnostic Algorithms. Tuberc. Respir. Dis. 2015, 78, 64–71. [Google Scholar] [CrossRef]
- Liu, H.; Schittny, V.; Nash, M.A. Removal of a Conserved Disulfide Bond Does Not Compromise Mechanical Stability of a VHH Antibody Complex. Nano Lett. 2019, 19, 5524–5529. [Google Scholar] [CrossRef]
- Sauer, U. Analytical Protein Microarrays: Advancements Towards Clinical Applications. Sensors 2017, 17, 256. [Google Scholar] [CrossRef]
- Sutandy, F.X.R.; Qian, J.; Chen, C.-S.; Zhu, H. Overview of Protein Microarrays. Curr. Protoc. Protein Sci. 2013, 72, 27.1.1–27.1.16. [Google Scholar] [CrossRef]
- Templin, M.F.; Stoll, D.; Schrenk, M.; Traub, P.C.; Vöhringer, C.F.; Joos, T.O. Protein microarray technology. Drug Discov. Today 2002, 7, 815–822. [Google Scholar] [CrossRef]
- Haab, B.B. Antibody Arrays in Cancer Research. Mol. Cell. Proteom. 2005, 4, 377–383. [Google Scholar] [CrossRef]
- Seidel, M.; Niessner, R. Automated analytical microarrays: A critical review. Anal. Bioanal. Chem. 2008, 391, 1521–1544. [Google Scholar] [CrossRef]
- Chen, Z.-A.; Sun, Y.-F.; Wang, Q.-X.; Ma, H.-H.; Ma, Z.-Z.; Yang, C.-J. Integrated Analysis of Multiple Microarray Studies to Identify Novel Gene Signatures in Ulcerative Colitis. Front. Genet. 2021, 12, 697514. [Google Scholar] [CrossRef]
- Govarthanan, K.; Gupta, P.K.; Ramasamy, D.; Kumar, P.; Mahadevan, S.; Verma, R.S. DNA methylation microarray uncovers a permissive methylome for cardiomyocyte differentiation in human mesenchymal stem cells. Genomics 2019, 112, 1384–1395. [Google Scholar] [CrossRef]
- Lin, X.M.; Chen, Y.H. Identification of Potentially Functional CircRNA-miRNA-mRNA Regulatory Network in Hepatocellular Carcinoma by Integrated Microarray Analysis. Med. Sci. Monit. Basic Res. 2018, 24, 70–78. [Google Scholar] [CrossRef]
- Wang, S.; Yan, R.; Wang, B.; Meng, P.; Tan, W.; Guo, X. The Functional Analysis of Selenium-Related Genes and Magnesium-Related Genes in the Gene Expression Profile Microarray in the Peripheral Blood Mononuclear Cells of Keshan Disease. Biol. Trace Elem. Res. 2019, 192, 3–9. [Google Scholar] [CrossRef]
- Zhang, H.; Klose, A.M.; Miller, B.L. Label-Free, Multiplex Glycan Microarray Biosensor for Influenza Virus Detection. Bioconjugate Chem. 2021, 32, 533–540. [Google Scholar] [CrossRef]
- Zhang, H.; Liu, X.; Zhang, C.; Xu, Y.; Su, J.; Lu, X.; Shi, J.; Wang, L.; Landry, M.P.; Zhu, Y.; et al. A DNA tetrahedral structure-mediated ultrasensitive fluorescent microarray platform for nucleic acid test. Sens. Actuators B Chem. 2020, 321, 128538. [Google Scholar] [CrossRef]
- Wu, T.; Li, Y.; Liang, X.; Liu, X.; Tang, M. Identification of potential circRNA-miRNA-mRNA regulatory networks in response to graphene quantum dots in microglia by microarray analysis. Ecotoxicol. Environ. Saf. 2021, 208, 111672. [Google Scholar] [CrossRef]
- Ruano-Gallego, D.; García-Villadangos, M.; Moreno-Paz, M.; Gómez-Elvira, J.; Postigo, M.; Simón-Sacristán, M.; Reyburn, H.T.; Carolis, C.; Rodrigo, N.; Codeseira, Y.B. A multiplex antigen microarray for simultaneous IgG and IgM detection against SARS-CoV-2 reveals higher seroprevalence than reported. Microb. Biotechnol. 2021, 14, 1228–1236. [Google Scholar] [CrossRef]
- Khan, S.; Nakajima, R.; Jain, A.; De Assis, R.R.; Jasinskas, A.; Obiero, J.M.; Adenaiye, O.; Tai, S.; Hong, F.; Milton, D.K. Analysis of Serologic Cross-Reactivity Between Common Human Coronaviruses and SARS-CoV-2 Using Coronavirus Antigen Microarray. bioRxiv 2020. [Google Scholar] [CrossRef]
- Pohlmann, C.; Elssner, T. Multiplex Immunoassay Techniques for On-Site Detection of Security Sensitive Toxins. Toxins 2020, 12, 727. [Google Scholar] [CrossRef]
- Fan, Y.; Duan, X.; Zhao, M.; Wei, X.; Wu, J.; Chen, W.; Liu, P.; Cheng, W.; Cheng, Q.; Ding, S. High-sensitive and multiplex biosensing assay of NSCLC-derived exosomes via different recognition sites based on SPRi array. Biosens. Bioelectron. 2020, 154, 112066. [Google Scholar] [CrossRef]
- Cohen, L.; Walt, D.R. Highly Sensitive and Multiplexed Protein Measurements. Chem. Rev. 2018, 119, 293–321. [Google Scholar] [CrossRef]
- Rusmini, F.; Zhong, Z.; Feijen, J. Protein Immobilization Strategies for Protein Biochips. Biomacromolecules 2007, 8, 1775–1789. [Google Scholar] [CrossRef]
- Jian, M.; Zhang, H.; Li, X.; Wang, Z. Profiling of multiple matrix metalloproteinases activities in the progression of osteosarcoma by peptide microarray-based fluorescence assay on polymer brush coated zinc oxide nanorod substrate. Sens. Actuators B Chem. 2021, 330, 129361. [Google Scholar] [CrossRef]
- Shlyapnikov, Y.M.; Malakhova, E.A.; Shlyapnikova, E.A. Improving Immunoassay Performance with Cleavable Blocking of Microarrays. Anal. Chem. 2020, 93, 1126–1134. [Google Scholar] [CrossRef]
- Yousefi, H.; Su, H.-M.; Ali, M.; Filipe, C.D.M.; Didar, T.F. Producing Covalent Microarrays of Amine-Conjugated DNA Probes on Various Functional Surfaces to Create Stable and Reliable Biosensors. Adv. Mater. Interfaces 2018, 5, 1800659. [Google Scholar] [CrossRef]
- Zhu, C.; Zhu, X.; Landry, J.P.; Cui, Z.; Li, Q.; Dang, Y.; Mi, L.; Zheng, F.; Fei, Y. Developing an Efficient and General Strategy for Immobilization of Small Molecules onto Microarrays Using Isocyanate Chemistry. Sensors 2016, 16, 378. [Google Scholar] [CrossRef]
- Davidow, A.; Kanaujia, G.V.; Shi, L.; Kaviar, J.; Guo, X.; Sung, N.; Kaplan, G.; Menzies, D.; Gennaro, M.L. Antibody Profiles Characteristic of Mycobacterium tuberculosis Infection State. Infect. Immun. 2005, 73, 6846–6851. [Google Scholar] [CrossRef] [PubMed]
- de Araujo, L.S.; da Silva, N.D.B.M.; Leung, J.A.M.; Mello, F.C.Q.; Saad, M.H.F. IgG subclasses’ response to a set of mycobacterial antigens in different stages of Mycobacterium tuberculosis infection. Tuberculosis 2018, 108, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, S.; Khalid, R.; Afzal, M.; Waheed Akhtar, M. Truncation of PstS1 antigen of Mycobacterium tuberculosis improves diagnostic efficiency. Tuberculosis 2013, 93, 654–659. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.; Li, H.; Ma, B.; Weiss, R.; Bendayan, D.; Abramovitz, L.; Ben-Shalom, N.; Mor, M.; Pinko, E.; Bar Oz, M.; et al. Human antibodies targeting a Mycobacterium transporter protein mediate protection against tuberculosis. Nat. Commun. 2021, 12, 602. [Google Scholar] [CrossRef]
- Jørgensen, M.M.; Sloth, J.K.; Bæk, R. Optimization of High-Throughput Multiplexed Phenotyping of Extracellular Vesicles Performed in 96-Well Microtiter Plates. Polymers 2021, 13, 2368. [Google Scholar] [CrossRef]
- Tsougeni, K.; Ellinas, K.; Koukouvinos, G.; Petrou, P.S.; Tserepi, A.; Kakabakos, S.E.; Gogolides, E. Three-dimensional (3D) plasma micro-nanotextured slides for high performance biomolecule microarrays: Comparison with epoxy-silane coated glass slides. Colloids Surf. B Biointerfaces 2018, 165, 270–277. [Google Scholar] [CrossRef]
- Mujawar, L.H.; Moers, A.; Norde, W.; van Amerongen, A. Rapid mastitis detection assay on porous nitrocellulose membrane slides. Anal. Bioanal. Chem. 2013, 405, 7469–7476. [Google Scholar] [CrossRef]
- Raux, M.; Finkielsztejn, L.; Salmon-Ceron, D.; Bouchez, H.; Excler, J.; Dulioust, E.; Grouin, J.; Sicard, D.; Blondeau, C.; Mestecky, J.; et al. Comparison of the Distribution of IgG and IgA Antibodies in Serum and Various Mucosal Fluids of HIV Type 1-Infected Subjects. AIDS Res. Hum. Retroviruses 1999, 15, 1365–1376. [Google Scholar] [CrossRef]
- Kimuda, S.G.; Andia-Biraro, I.; Egesa, M.; Bagaya, B.S.; Raynes, J.G.; Levin, J.; Elliott, A.M.; Cose, S. Use of QuantiFERON(R)-TB Gold in-tube culture supernatants for measurement of antibody responses. PLoS ONE 2017, 12, e0188396. [Google Scholar] [CrossRef]
- Viitala, S.M.; Jääskeläinen, A.J.; Kelo, E.; Sirola, H.; Moilanen, K.; Suni, J.; Vaheri, A.; Vapalahti, O.; Närvänen, A. Surface-activated microtiter-plate microarray for simultaneous CRP quantification and viral antibody detection. Diagn. Microbiol. Infect. Dis. 2012, 75, 174–179. [Google Scholar] [CrossRef]
- Yeung, D.; Ciotti, S.; Purushothama, S.; Gharakhani, E.; Kuesters, G.; Schlain, B.; Shen, C.; Donaldson, D.; Mikulskis, A. Evaluation of highly sensitive immunoassay technologies for quantitative measurements of sub-pg/mL levels of cytokines in human serum. J. Immunol. Methods 2016, 437, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Zhou, H.; Lin, H.; Roy, S.; Shaler, T.A.; Hill, L.R.; Norton, S.; Kumar, P.; Anderle, M.; Becker, C.H. Quantification of Proteins and Metabolites by Mass Spectrometry without Isotopic Labeling or Spiked Standards. Anal. Chem. 2003, 75, 4818–4826. [Google Scholar] [CrossRef] [PubMed]
- Toedter, G.; Hayden, K.; Wagner, C.; Brodmerkel, C. Simultaneous Detection of Eight Analytes in Human Serum by Two Commercially Available Platforms for Multiplex Cytokine Analysis. Clin. Vaccine Immunol. 2008, 15, 42–48. [Google Scholar] [CrossRef]
- Bhakta, S.A.; Evans, E.; Benavidez, T.E.; Garcia, C.D. Protein adsorption onto nanomaterials for the development of biosensors and analytical devices: A review. Anal. Chim. Acta 2015, 872, 7–25. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Rong, C.; Lu, T.; Hu, H. Identifying Strong Covalent Interactions with Pauli Energy. J. Phys. Chem. A 2018, 122, 3087–3095. [Google Scholar] [CrossRef]
- Mallinson, P.R.; Smith, G.T.; Wilson, C.C.; Grech, E.; Wozniak, K. From Weak Interactions to Covalent Bonds: A Continuum in the Complexes of 1,8-Bis(dimethylamino)naphthalene. J. Am. Chem. Soc. 2003, 125, 4259–4270. [Google Scholar] [CrossRef] [PubMed]
- Kapingidza, A.B.; Kowal, K.; Chruszcz, M. Antigen-Antibody Complexes. Subcell Biochem. 2020, 94, 465–497. [Google Scholar]
- Cervia, C.; Nilsson, J.; Zurbuchen, Y.; Valaperti, A.; Schreiner, J.; Wolfensberger, A.; Raeber, M.E.; Adamo, S.; Weigang, S.; Emmenegger, M. Systemic and mucosal antibody responses specific to SARS-CoV-2 during mild versus severe COVID-19. J. Allergy Clin. Immunol. 2021, 147, 545–557.e9. [Google Scholar] [CrossRef]
- Van Regenmortel, M.H. Specificity, polyspecificity, and heterospecificity of antibody-antigen recognition. J. Mol. Recognit. 2014, 27, 627–639. [Google Scholar] [CrossRef]
- Koukouvinos, G.; Karachaliou, C.-E.; Kanioura, A.; Tsougeni, K.; Livaniou, E.; Kakabakos, S.E.; Petrou, P.S. Fluorescence Enhancement on Silver-Plated Plasma Micro-Nanostructured 3D Polymeric Microarray Substrates for Multiplex Mycotoxin Detection. Processes 2021, 9, 392. [Google Scholar] [CrossRef]
- Xia, Y.; Zhu, H.; Liu, R.; Li, X.; Xie, X.; Zhao, J.; Li, J.; Jiao, X.; Yang, Z.; Chen, X. Picogram level electrochemical impedimetric immunosensor for monitoring Mycobacterium tuberculosis based on specific and sensitive ESAT-6 monoclonal antibody. Talanta 2023, 253, 124052. [Google Scholar] [CrossRef]
- Seele, P.P.; Dyan, B.; Skepu, A.; Maserumule, C.; Sibuyi, N.R.S. Development of Gold-Nanoparticle-Based Lateral Flow Immunoassays for Rapid Detection of TB ESAT-6 and CFP-10. Biosensors 2023, 13, 354. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Cheney, C.; Huang, Q.; Hazuda, D.J.; Howell, B.J.; Zuck, P. Improved Detection of HIV Gag p24 Protein Using a Combined Immunoprecipitation and Digital ELISA Method. Front. Microbiol. 2021, 12, 636703. [Google Scholar] [CrossRef] [PubMed]
- Ellington, A.A.; Kullo, I.J.; Bailey, K.R.; Klee, G.G. Antibody-Based Protein Multiplex Platforms: Technical and Operational Challenges. Clin. Chem. 2010, 56, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Ndlovu, Z.; Fajardo, E.; Mbofana, E.; Maparo, T.; Garone, D.; Metcalf, C.; Bygrave, H.; Kao, K.; Zinyowera, S. Multidisease testing for HIV and TB using the GeneXpert platform: A feasibility study in rural Zimbabwe. PLoS ONE 2018, 13, e0193577. [Google Scholar] [CrossRef]
- Shah, M.; Variava, E.; Holmes, C.B.; Coppin, A.; Golub, J.E.; McCallum, J.; Wong, M.; Luke, B.; Martin, D.J.; Chaisson, R.E.; et al. Diagnostic Accuracy of a Urine Lipoarabinomannan Test for Tuberculosis in Hospitalized Patients in a High HIV Prevalence Setting. J. Acquir. Immune Defic. Syndr. 2009, 52, 145–151. [Google Scholar] [CrossRef]
- Lawn, S.D.; Brooks, S.V.; Kranzer, K.; Nicol, M.P.; Whitelaw, A.; Vogt, M.; Bekker, L.-G.; Wood, R. Screening for HIV-Associated Tuberculosis and Rifampicin Resistance before Antiretroviral Therapy Using the Xpert MTB/RIF Assay: A Prospective Study. PLoS Med. 2011, 8, e1001067. [Google Scholar] [CrossRef]
- Kellum, J.A. Determinants of blood pH in health and disease. Crit. Care 2000, 4, 6–14. [Google Scholar] [CrossRef][Green Version]
- Brunskill, S.; Thomas, S.; Whitmore, E.; McDonald, C.P.; Dorée, C.; Hopewell, S.; Staves, J.; Cardigan, R.; Murphy, M.F. What Is the Maximum Time That a Unit of Red Blood Cells Can Be Safely Left Out of Controlled Temperature Storage? Transfus. Med. Rev. 2012, 26, 209–223. [Google Scholar] [CrossRef]
- Parsons, L.M.; Somoskövi, A.; Gutierrez, C.; Lee, E.; Paramasivan, C.N.; Abimiku, A.; Spector, S.; Roscigno, G.; Nkengasong, J. Laboratory Diagnosis of Tuberculosis in Resource-Poor Countries: Challenges and Opportunities. Clin. Microbiol. Rev. 2011, 24, 314–350. [Google Scholar] [CrossRef]
- Karim, S.S.A.; Churchyard, G.J.; Karim, Q.A.; Lawn, S.D. Health in South Africa 3 HIV infection and tuberculosis in South Africa: An urgent need to escalate the public health response. Lancet 2009, 374, 921–933. [Google Scholar] [CrossRef]
- Krizkova, S.; Heger, Z.; Zalewska, M.; Moulick, A.; Adam, V.; Kizek, R.; Zhang, T.-X.; Zhu, G.-Y.; Lu, B.-Y.; Zhang, C.-L.; et al. Nanotechnologies in protein microarrays. Nanomedicine 2015, 10, 2743–2755. [Google Scholar] [CrossRef]
- Pultar, J.; Sauer, U.; Domnanich, P.; Preininger, C. Aptamer–antibody on-chip sandwich immunoassay for detection of CRP in spiked serum. Biosens. Bioelectron. 2009, 24, 1456–1461. [Google Scholar] [CrossRef]
- Mytych, D.T.; La, S.; Barger, T.; Ferbas, J.; Swanson, S.J. The development and validation of a sensitive, dual-flow cell, SPR-based biosensor immunoassay for the detection, semi-quantitation, and characterization of antibodies to darbepoetin alfa and epoetin alfa in human serum. J. Pharm. Biomed. Anal. 2009, 49, 415–426. [Google Scholar] [CrossRef]
- Mohammadi, S.; Salimi, A.; Hamd-Ghadareh, S.; Fathi, F.; Soleimani, F. A FRET immunosensor for sensitive detection of CA 15-3 tumor marker in human serum sample and breast cancer cells using antibody functionalized luminescent carbon-dots and AuNPs-dendrimer aptamer as donor-acceptor pair. Anal. Biochem. 2018, 557, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Maple, L.; Lathrop, R.; Bozich, S.; Harman, W.; Tacey, R.; Kelley, M.; Danilkovitch-Miagkova, A. Development and validation of ELISA for Herceptin detection in human serum. J. Immunol. Methods 2004, 295, 169–182. [Google Scholar] [CrossRef] [PubMed]
- Albrecht, C.; Kaeppel, N.; Gauglitz, G. Two immunoassay formats for fully automated CRP detection in human serum. Anal. Bioanal. Chem. 2008, 391, 1845–1852. [Google Scholar] [CrossRef] [PubMed]





| Primary Antibody | Limit of Detection Concentration (µg/mL) | |||
|---|---|---|---|---|
| Primary Antibodies Diluted in PBS | Primary Antibodies Diluted in Human Serum | |||
| Epoxy-Coated Glass Slides | Polystyrene High-Binding Microtiter Plates | Epoxy-Coated Glass Slides | Polystyrene High-Binding Microtiter Plates | |
| Anti-p24 | 0.000954 | 0.061 | 0.000954 | 0.9765 |
| Anti-ESAT6 | 0.000954 | 0.06138 | 0.000954 | 0.9765 |
| Anti-CFP10 | 0.000954 | 0.06138 | 0.000954 | 0.9765 |
| Anti-pstS1 | 0.000954 | 15.62 | 0.000954 | 15.62 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malatji, K.; Singh, A.; Thobakgale, C.; Alexandre, K. Development of a Multiplex HIV/TB Diagnostic Assay Based on the Microarray Technology. Biosensors 2023, 13, 894. https://doi.org/10.3390/bios13090894
Malatji K, Singh A, Thobakgale C, Alexandre K. Development of a Multiplex HIV/TB Diagnostic Assay Based on the Microarray Technology. Biosensors. 2023; 13(9):894. https://doi.org/10.3390/bios13090894
Chicago/Turabian StyleMalatji, Kanyane, Advaita Singh, Christina Thobakgale, and Kabamba Alexandre. 2023. "Development of a Multiplex HIV/TB Diagnostic Assay Based on the Microarray Technology" Biosensors 13, no. 9: 894. https://doi.org/10.3390/bios13090894
APA StyleMalatji, K., Singh, A., Thobakgale, C., & Alexandre, K. (2023). Development of a Multiplex HIV/TB Diagnostic Assay Based on the Microarray Technology. Biosensors, 13(9), 894. https://doi.org/10.3390/bios13090894





