Fluoropolymer Functionalization of Organ-on-Chip Platform Increases Detection Sensitivity for Cannabinoids
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals
2.2. PDMS-Based Microfluidic Channel Fabrication
2.3. Coating Flat PDMS Surfaces and Microchannels with Teflon AF 2400
2.4. Water Contact Angle (WCA) Measurement
2.5. Attenuated Total Reflection-Fourier Transform Infrared Spectroscopy (ATR-FTIR)
2.6. X-ray Photoelectron Spectroscopy (XPS)
2.7. CBD Incubation on Flat PDMS and Inside Microfluidic Channels
2.8. CBD Derivatization and LC-MS/MS Analysis
2.9. hCMEC/D3 Cell Culture in Microchannels Coated with and without Teflon AF 2400
2.10. Cell Staining
2.11. Data Analysis
3. Results and Discussion
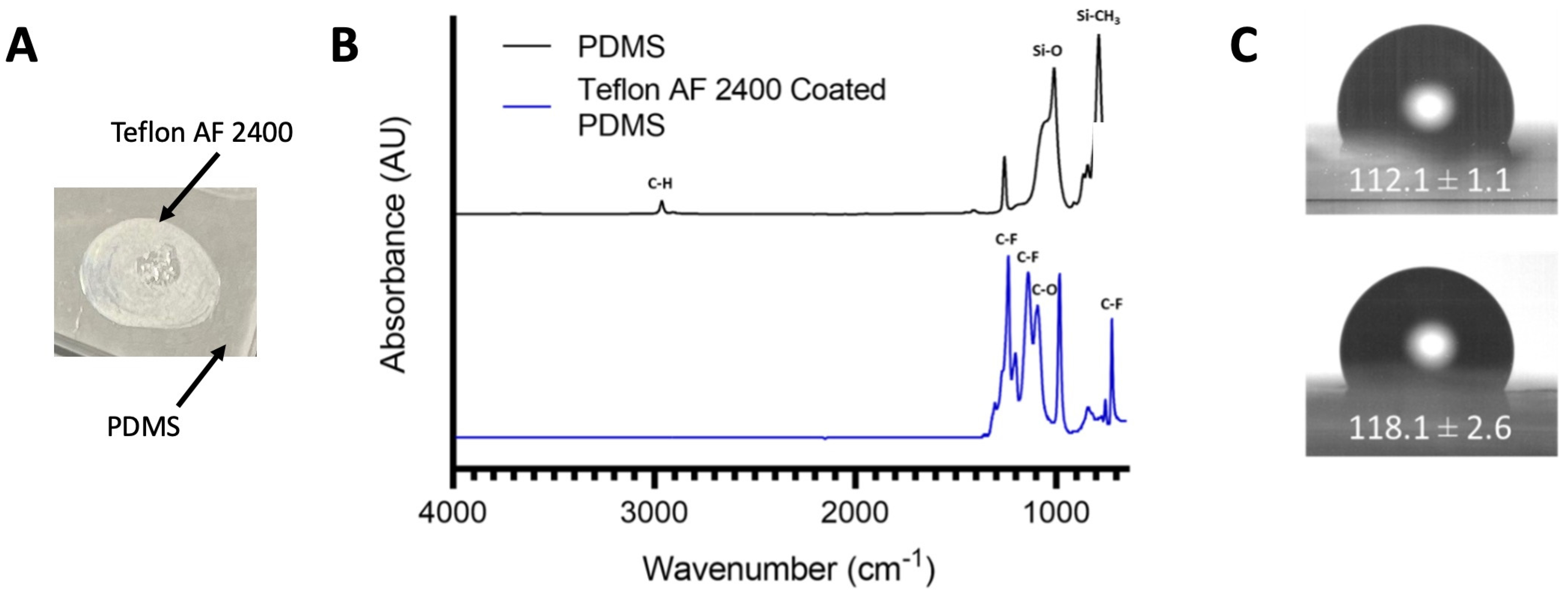
3.1. Surface Characterizations Confirm the Coating of Teflon AF 2400 on PDMS Surface
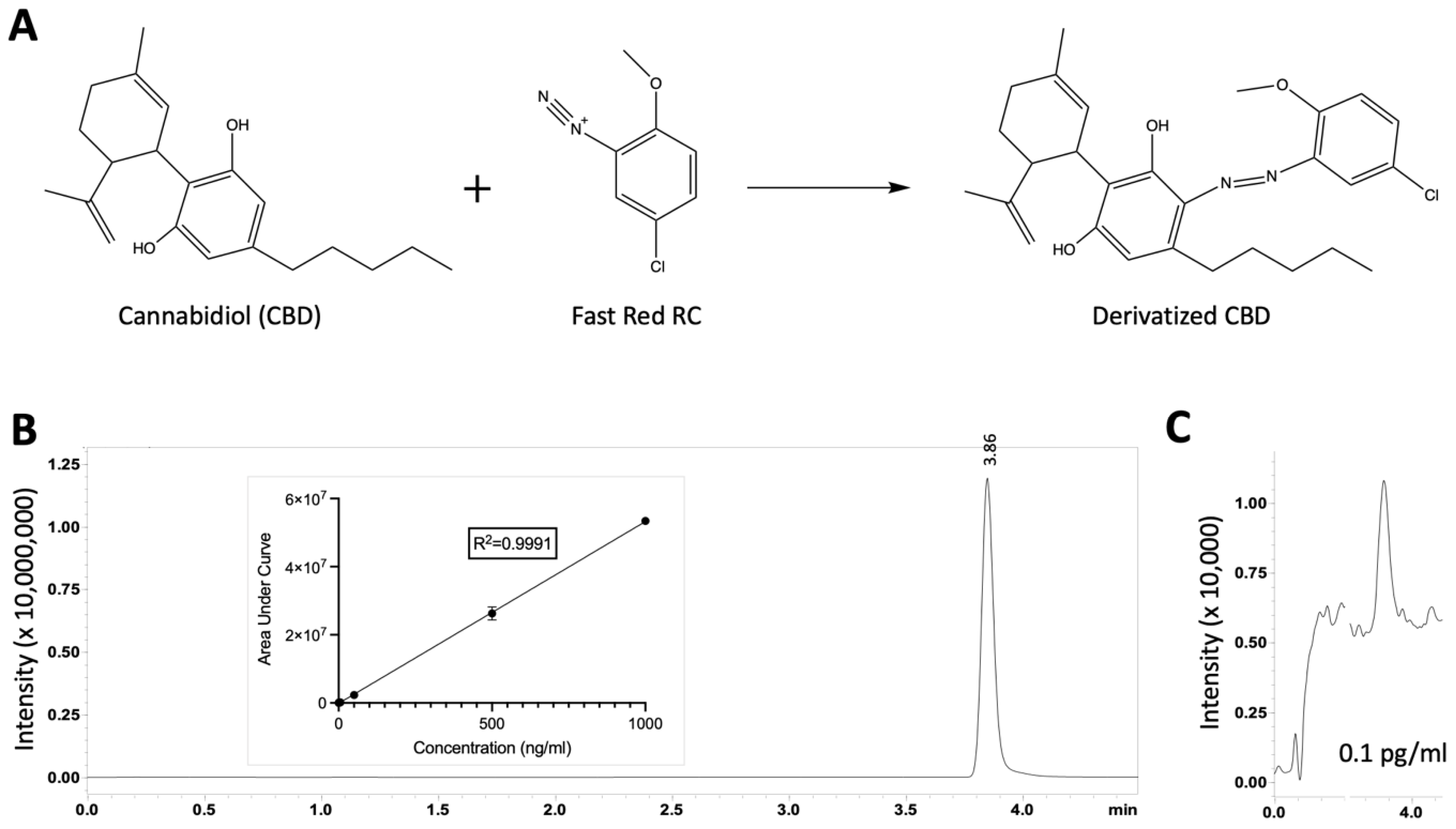
3.2. Azo Coupling Derivatization Method Increased the Limit of Quantification of CBD
3.3. Flat PDMS Surface Functionalized via Teflon AF 2400 Reduced CBD Absorption
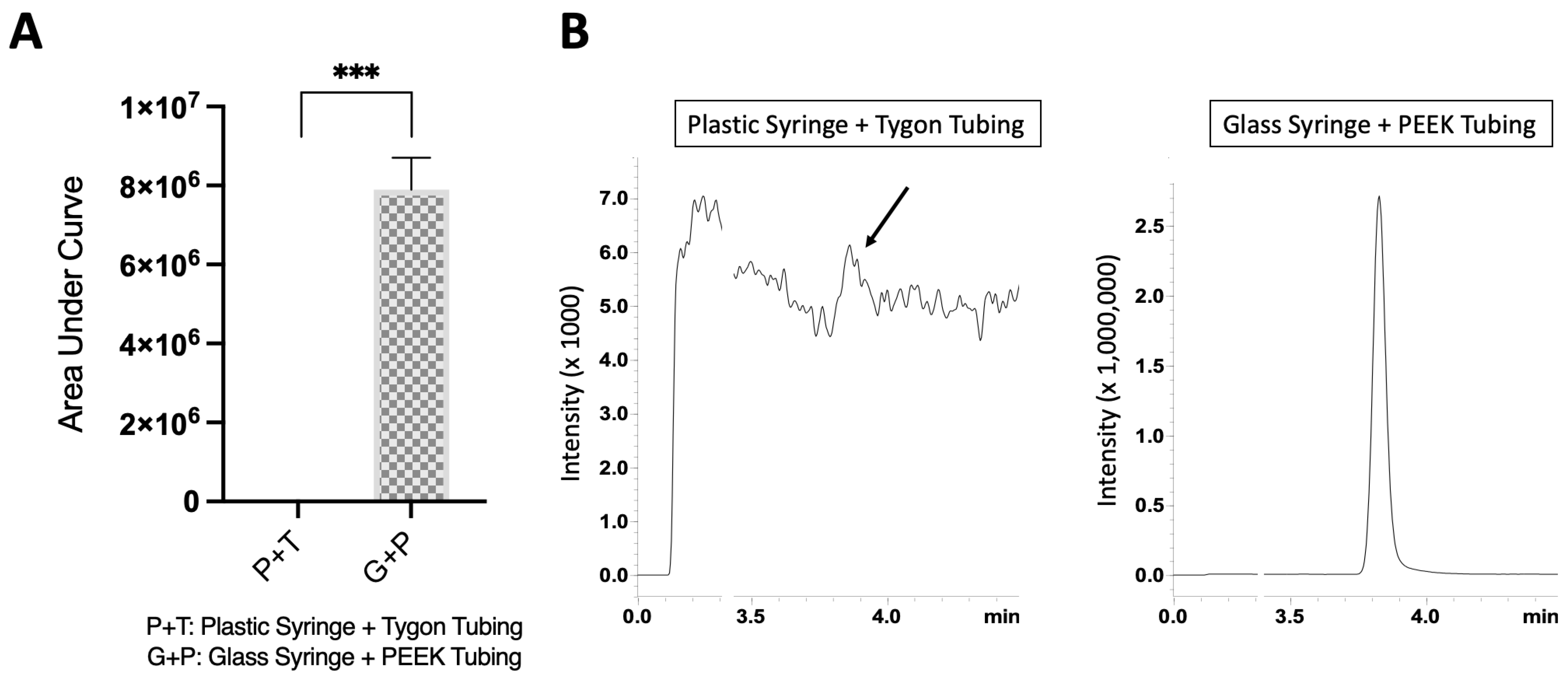
3.4. Glass Syringe and PEEK Tubing Combination Increased the CBD Recovery in Flow Conditions
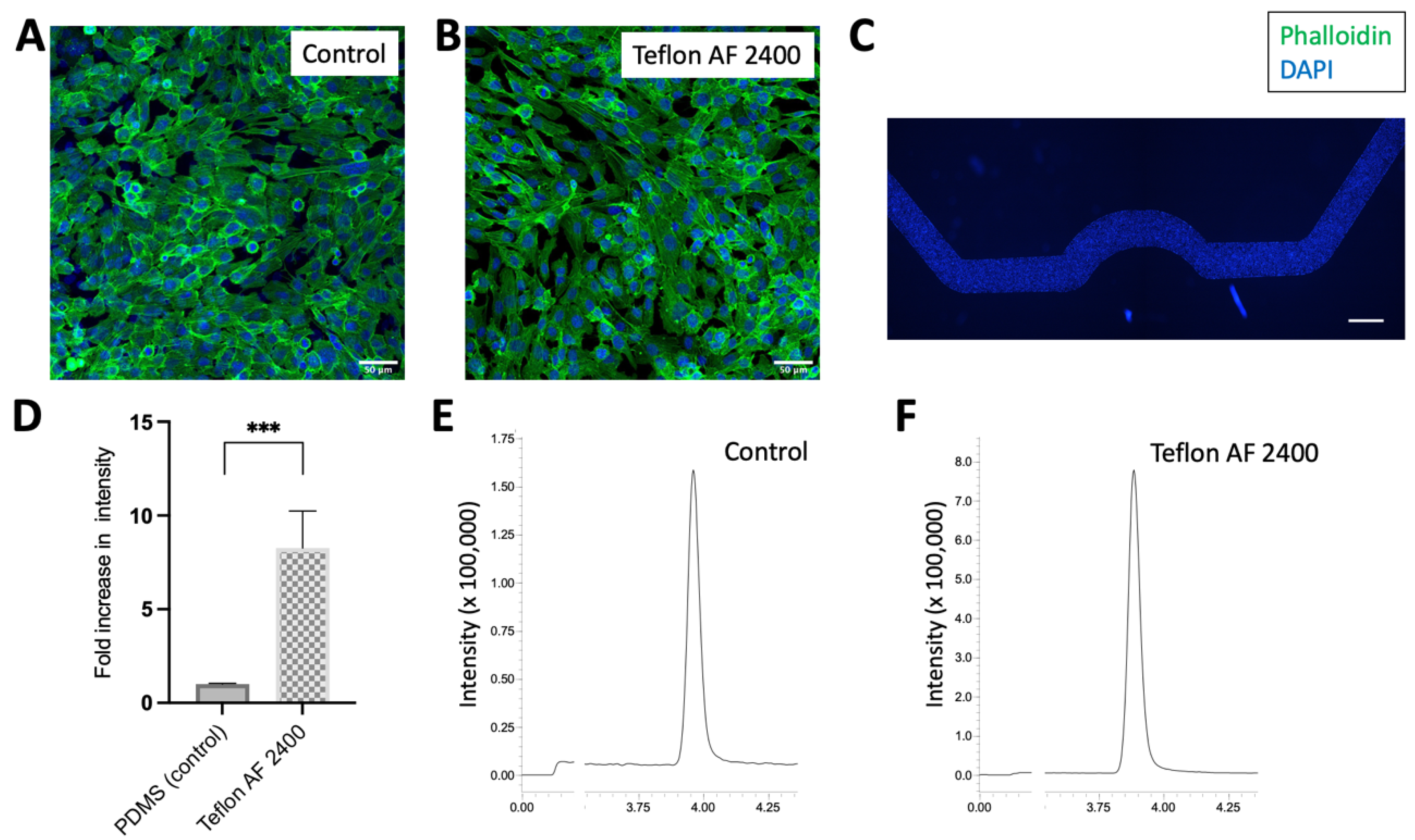
3.5. Microfluidic Channels Functionalized via Teflon AF 2400 Improved CBD Recovery
3.6. Microfluidic Surface Functionalized with Teflon AF 2400 Is Suitable for Cell Experiment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Koyilot, M.C.; Natarajan, P.; Hunt, C.R.; Sivarajkumar, S.; Roy, R.; Joglekar, S.; Pandita, S.; Tong, C.W.; Marakkar, S.; Subramanian, L.; et al. Breakthroughs and Applications of Organ-on-a-Chip Technology. Cells 2022, 11, 1828. [Google Scholar] [CrossRef] [PubMed]
- Mathur, A.; Loskill, P.; Shao, K.; Huebsch, N.; Hong, S.; Marcus, S.G.; Marks, N.; Mandegar, M.; Conklin, B.R.; Lee, L.P.; et al. Human iPSC-based Cardiac Microphysiological System For Drug Screening Applications. Sci. Rep. 2015, 5, 8883. [Google Scholar] [CrossRef] [PubMed]
- Legendre, A.; Baudoin, R.; Alberto, G.; Paullier, P.; Naudot, M.; Bricks, T.; Brocheton, J.; Jacques, S.; Cotton, J.; Leclerc, E. Metabolic characterization of primary rat hepatocytes cultivated in parallel microfluidic biochips. J. Pharm. Sci. 2013, 102, 3264–3276. [Google Scholar] [CrossRef]
- Sutterby, E.; Thurgood, P.; Baratchi, S.; Khoshmanesh, K.; Pirogova, E. Microfluidic Skin-on-a-Chip Models: Toward Biomimetic Artificial Skin. Small 2020, 16, e2002515. [Google Scholar] [CrossRef]
- Musah, S.; Dimitrakakis, N.; Camacho, D.M.; Church, G.M.; Ingber, D.E. Directed differentiation of human induced pluripotent stem cells into mature kidney podocytes and establishment of a Glomerulus Chip. Nat. Protoc. 2018, 13, 1662–1685. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, J.; Razavi Bazaz, S.; Aboulkheyr Es, H.; Yaghobian Azari, D.; Thierry, B.; Ebrahimi Warkiani, M.; Ghadiri, M. Lung-on-a-chip: The future of respiratory disease models and pharmacological studies. Crit. Rev. Biotechnol. 2020, 40, 213–230. [Google Scholar] [CrossRef]
- Kim, H.J.; Ingber, D.E. Gut-on-a-Chip microenvironment induces human intestinal cells to undergo villus differentiation. Integr. Biol. 2013, 5, 1130–1140. [Google Scholar] [CrossRef]
- Ragelle, H.; Goncalves, A.; Kustermann, S.; Antonetti, D.A.; Jayagopal, A. Organ-On-A-Chip Technologies for Advanced Blood-Retinal Barrier Models. J. Ocul. Pharmacol. Ther. 2020, 36, 30–41. [Google Scholar] [CrossRef]
- Kimura, H.; Sakai, Y.; Fujii, T. Organ/body-on-a-chip based on microfluidic technology for drug discovery. Drug Metab. Pharmacokinet. 2018, 33, 43–48. [Google Scholar] [CrossRef]
- Maschmeyer, I.; Lorenz, A.K.; Schimek, K.; Hasenberg, T.; Ramme, A.P.; Hübner, J.; Lindner, M.; Drewell, C.; Bauer, S.; Thomas, A.; et al. A four-organ-chip for interconnected long-term co-culture of human intestine, liver, skin and kidney equivalents. Lab Chip 2015, 15, 2688–2699. [Google Scholar] [CrossRef]
- Sung, J.H.; Shuler, M.L. A micro cell culture analog (microCCA) with 3-D hydrogel culture of multiple cell lines to assess metabolism-dependent cytotoxicity of anti-cancer drugs. Lab Chip 2009, 9, 1385–1394. [Google Scholar] [CrossRef]
- Peng, B.; Hao, S.; Tong, Z.; Bai, H.; Pan, S.; Lim, K.-L.; Li, L.; Voelcker, N.H.; Huang, W. Blood–brain barrier (BBB)-on-a-chip: A promising breakthrough in brain disease research. Lab Chip 2022, 22, 3579–3602. [Google Scholar] [CrossRef] [PubMed]
- Cherusseri, J.; Savio, C.M.; Khalid, M.; Chaudhary, V.; Numan, A.; Varma, S.J.; Menon, A.; Kaushik, A. SARS-CoV-2-on-Chip for Long COVID Management. Biosensors 2022, 12, 890. [Google Scholar] [CrossRef]
- Zhang, B.; Radisic, M. Organ-on-a-chip devices advance to market. Lab Chip 2017, 17, 2395–2420. [Google Scholar] [CrossRef]
- Campbell, S.B.; Wu, Q.; Yazbeck, J.; Liu, C.; Okhovatian, S.; Radisic, M. Beyond Polydimethylsiloxane: Alternative Materials for Fabrication of Organ-on-a-Chip Devices and Microphysiological Systems. ACS Biomater. Sci. Eng. 2021, 7, 2880–2899. [Google Scholar] [CrossRef] [PubMed]
- Cameron, T.C.; Randhawa, A.; Grist, S.M.; Bennet, T.; Hua, J.; Alde, L.G.; Caffrey, T.M.; Wellington, C.L.; Cheung, K.C. PDMS Organ-On-Chip Design and Fabrication: Strategies for Improving Fluidic Integration and Chip Robustness of Rapidly Prototyped Microfluidic In Vitro Models. Micromachines 2022, 13, 1573. [Google Scholar] [CrossRef]
- Regehr, K.J.; Domenech, M.; Koepsel, J.T.; Carver, K.C.; Ellison-Zelski, S.J.; Murphy, W.L.; Schuler, L.A.; Alarid, E.T.; Beebe, D.J. Biological implications of polydimethylsiloxane-based microfluidic cell culture. Lab Chip 2009, 9, 2132–2139. [Google Scholar] [CrossRef]
- Gokaltun, A.; Yarmush, M.L.; Asatekin, A.; Usta, O.B. Recent advances in nonbiofouling PDMS surface modification strategies applicable to microfluidic technology. Technology 2017, 05, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Khetani, S.; Yong, K.W.; Ozhukil Kollath, V.; Eastick, E.; Azarmanesh, M.; Karan, K.; Sen, A.; Sanati-Nezhad, A. Engineering Shelf-Stable Coating for Microfluidic Organ-on-a-Chip Using Bioinspired Catecholamine Polymers. ACS Appl. Mater. Interfaces 2020, 12, 6910–6923. [Google Scholar] [CrossRef] [PubMed]
- Tu, Q.; Wang, J.-C.; Zhang, Y.; Liu, R.; Liu, W.; Ren, L.; Shen, S.; Xu, J.; Zhao, L.; Wang, J. Surface modification of poly(dimethylsiloxane) and its applications in microfluidics-based biological analysis. Rev. Anal. Chem. 2012, 31, 177–192. [Google Scholar] [CrossRef]
- Tan, S.H.; Nguyen, N.T.; Chua, Y.C.; Kang, T.G. Oxygen plasma treatment for reducing hydrophobicity of a sealed polydimethylsiloxane microchannel. Biomicrofluidics 2010, 4, 32204. [Google Scholar] [CrossRef]
- Hellmich, W.; Regtmeier, J.; Duong, T.T.; Ros, R.; Anselmetti, D.; Ros, A. Poly(oxyethylene) Based Surface Coatings for Poly(dimethylsiloxane) Microchannels. Langmuir 2005, 21, 7551–7557. [Google Scholar] [CrossRef] [PubMed]
- Chuah, Y.J.; Kuddannaya, S.; Lee, M.H.; Zhang, Y.; Kang, Y. The effects of poly(dimethylsiloxane) surface silanization on the mesenchymal stem cell fate. Biomater. Sci. 2015, 3, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Radisic, M.; Loskill, P. Beyond PDMS and Membranes: New Materials for Organ-on-a-Chip Devices. ACS Biomater. Sci. Eng. 2021, 7, 2861–2863. [Google Scholar] [CrossRef]
- Ren, K.; Dai, W.; Zhou, J.; Su, J.; Wu, H. Whole-Teflon microfluidic chips. Proc. Natl. Acad. Sci. USA 2011, 108, 8162–8166. [Google Scholar] [CrossRef] [PubMed]
- Doherty, G.J.; de Paula, B.H.R. Cannabinoids in glioblastoma multiforme-hype or hope? Br. J. Cancer 2021, 124, 1341–1343. [Google Scholar] [CrossRef] [PubMed]
- Zhelyazkova, M.; Kirilov, B.; Momekov, G. The pharmacological basis for application of cannabidiol in cancer chemotherapy. Pharmacia 2020, 67, 239–252. [Google Scholar] [CrossRef]
- Jhawar, N.; Schoenberg, E.; Wang, J.V.; Saedi, N. The growing trend of cannabidiol in skincare products. Clin. Dermatol. 2019, 37, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K.; Talukder, M. Cannabinoids for skin diseases and hair regrowth. J. Cosmet. Dermatol. 2021, 20, 2703–2711. [Google Scholar] [CrossRef]
- Navarrete, F.; Gasparyan, A.; Manzanares, J. CBD-mediated regulation of heroin withdrawal-induced behavioural and molecular changes in mice. Addict. Biol. 2022, 27, e13150. [Google Scholar] [CrossRef]
- Zieba, J.; Sinclair, D.; Sebree, T.; Bonn-Miller, M.; Gutterman, D.; Siegel, S.; Karl, T. Cannabidiol (CBD) reduces anxiety-related behavior in mice via an FMRP-independent mechanism. Pharmacol. Biochem. Behav. 2019, 181, 93–100. [Google Scholar] [CrossRef]
- Verrico, C.D.; Wesson, S.; Konduri, V.; Hofferek, C.J.; Vazquez-Perez, J.; Blair, E.; Dunner, K., Jr.; Salimpour, P.; Decker, W.K.; Halpert, M.M. A randomized, double-blind, placebo-controlled study of daily cannabidiol for the treatment of canine osteoarthritis pain. Pain 2020, 161, 2191–2202. [Google Scholar] [CrossRef]
- Alhamoruni, A.; Lee, A.C.; Wright, K.L.; Larvin, M.; O’Sullivan, S.E. Pharmacological effects of cannabinoids on the Caco-2 cell culture model of intestinal permeability. J. Pharmacol. Exp. Ther. 2010, 335, 92–102. [Google Scholar] [CrossRef]
- Mangal, N.; Erridge, S.; Habib, N.; Sadanandam, A.; Reebye, V.; Sodergren, M.H. Cannabinoids in the landscape of cancer. J. Cancer Res. Clin. Oncol. 2021, 147, 2507–2534. [Google Scholar] [CrossRef] [PubMed]
- Delon, L.C.; Nilghaz, A.; Cheah, E.; Prestidge, C.; Thierry, B. Unlocking the Potential of Organ-on-Chip Models through Pumpless and Tubeless Microfluidics. Adv. Healthc. Mater. 2020, 9, 1901784. [Google Scholar] [CrossRef] [PubMed]
- ul Ahmad, A.; Liang, H.; Ali, S.; Abbas, Q.; Farid, A.; Ali, A.; Iqbal, M.; Ahmad khan, I.; Pan, L.; Abbas, A.; et al. Cheap, reliable, reusable, thermally and chemically stable fluorinated hexagonal boron nitride nanosheets coated Au nanoparticles substrate for surface enhanced Raman spectroscopy. Sens. Actuators B Chem. 2020, 304, 127394. [Google Scholar] [CrossRef]
- Akther, F.; Yakob, S.B.; Nguyen, N.T.; Ta, H.T. Surface Modification Techniques for Endothelial Cell Seeding in PDMS Microfluidic Devices. Biosensors 2020, 10, 182. [Google Scholar] [CrossRef]
- Atakan, Z. Cannabis, a complex plant: Different compounds and different effects on individuals. Ther. Adv. Psychopharmacol. 2012, 2, 241–254. [Google Scholar] [CrossRef]
- Kaarj, K.; Yoon, J.Y. Methods of Delivering Mechanical Stimuli to Organ-on-a-Chip. Micromachines 2019, 10, 700. [Google Scholar] [CrossRef]
- Malysheva, A.; Ivask, A.; Hager, C.; Brunetti, G.; Marzouk, E.R.; Lombi, E.; Voelcker, N.H. Sorption of silver nanoparticles to laboratory plastic during (eco)toxicological testing. Nanotoxicology 2016, 10, 385–390. [Google Scholar] [CrossRef]
- Fedi, A.; Vitale, C.; Fato, M.; Scaglione, S. A Human Ovarian Tumor & Liver Organ-on-Chip for Simultaneous and More Predictive Toxo-Efficacy Assays. Bioengineering 2023, 10, 270. [Google Scholar] [PubMed]
- Brown, T.D.; Nowak, M.; Bayles, A.V.; Prabhakarpandian, B.; Karande, P.; Lahann, J.; Helgeson, M.E.; Mitragotri, S. A microfluidic model of human brain (μHuB) for assessment of blood brain barrier. Bioeng. Transl. Med. 2019, 4, e10126. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, H.L.; Nath, P.; Huang, J.H. Multistep Fluidic Control Network toward the Automated Generation of Organ-on-a-Chip. ACS Biomater. Sci. Eng. 2019, 5, 4852–4860. [Google Scholar] [CrossRef] [PubMed]



| PDMS (Atomic%) | PDMS Coated with Teflon AF 2400 (Atomic%) | |
|---|---|---|
| F | 0.0 ± 0.0 | 55.1 ± 0.1 |
| O | 26.9 ± 0.1 | 11.7 ± 0.1 |
| C total | 48.4 ± 0.1 | 32.8 ± 0.2 |
| C1 | 41.2 ± 0.0 | 0.6 ± 0.2 |
| C2 | 6.9 ± 0.2 | 0.3 ± 0.1 |
| C3 | 0.2 ± 0.0 | 0.3 ± 0.0 |
| C4 | 0.1 ± 0.0 | 0.4 ± 0.0 |
| C5 | 0.0 ± 0.0 | 1.5 ± 0.0 |
| C6 | 0.0 ± 0.0 | 9.0 ± 0.1 |
| C7 | 0.0 ± 0.0 | 8.9 ± 0.0 |
| C8 | 0.0 ± 0.0 | 11.7 ± 0.0 |
| Si | 24.7 ± 0.2 | 0.5 ± 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tong, Z.; Esser, L.; Galettis, P.; Rudd, D.; Easton, C.D.; Nilghaz, A.; Peng, B.; Zhu, D.; Thissen, H.; Martin, J.H.; et al. Fluoropolymer Functionalization of Organ-on-Chip Platform Increases Detection Sensitivity for Cannabinoids. Biosensors 2023, 13, 779. https://doi.org/10.3390/bios13080779
Tong Z, Esser L, Galettis P, Rudd D, Easton CD, Nilghaz A, Peng B, Zhu D, Thissen H, Martin JH, et al. Fluoropolymer Functionalization of Organ-on-Chip Platform Increases Detection Sensitivity for Cannabinoids. Biosensors. 2023; 13(8):779. https://doi.org/10.3390/bios13080779
Chicago/Turabian StyleTong, Ziqiu, Lars Esser, Peter Galettis, David Rudd, Christopher D. Easton, Azadeh Nilghaz, Bo Peng, Douer Zhu, Helmut Thissen, Jennifer H. Martin, and et al. 2023. "Fluoropolymer Functionalization of Organ-on-Chip Platform Increases Detection Sensitivity for Cannabinoids" Biosensors 13, no. 8: 779. https://doi.org/10.3390/bios13080779
APA StyleTong, Z., Esser, L., Galettis, P., Rudd, D., Easton, C. D., Nilghaz, A., Peng, B., Zhu, D., Thissen, H., Martin, J. H., & Voelcker, N. H. (2023). Fluoropolymer Functionalization of Organ-on-Chip Platform Increases Detection Sensitivity for Cannabinoids. Biosensors, 13(8), 779. https://doi.org/10.3390/bios13080779







