Microfluidic Sliding Paper-Based Device for Point-of-Care Determination of Albumin-to-Creatine Ratio in Human Urine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Control Samples and Reagents
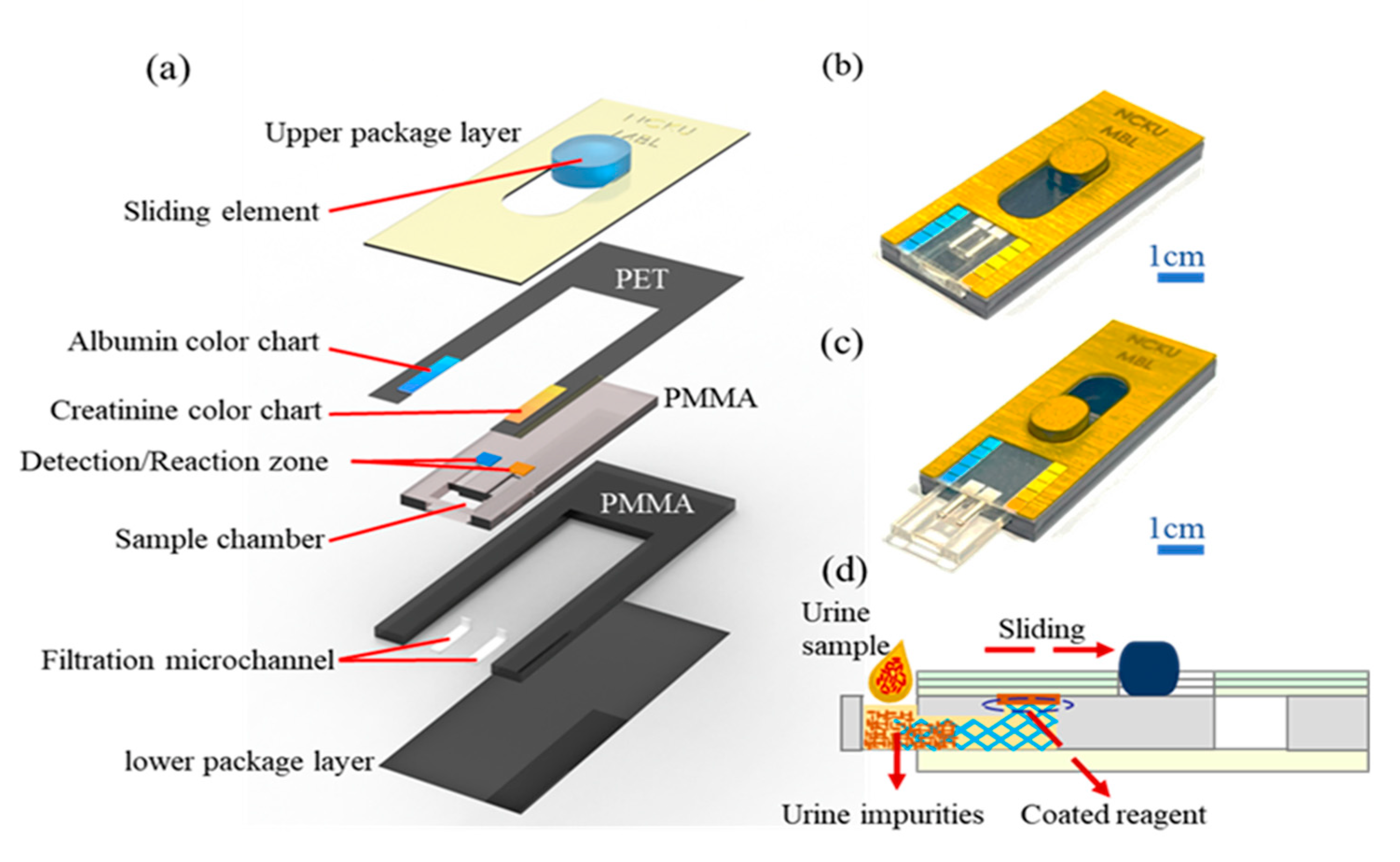
2.2. Manufacture of Sliding Microfluidic Double-Track Paper-Based Chip
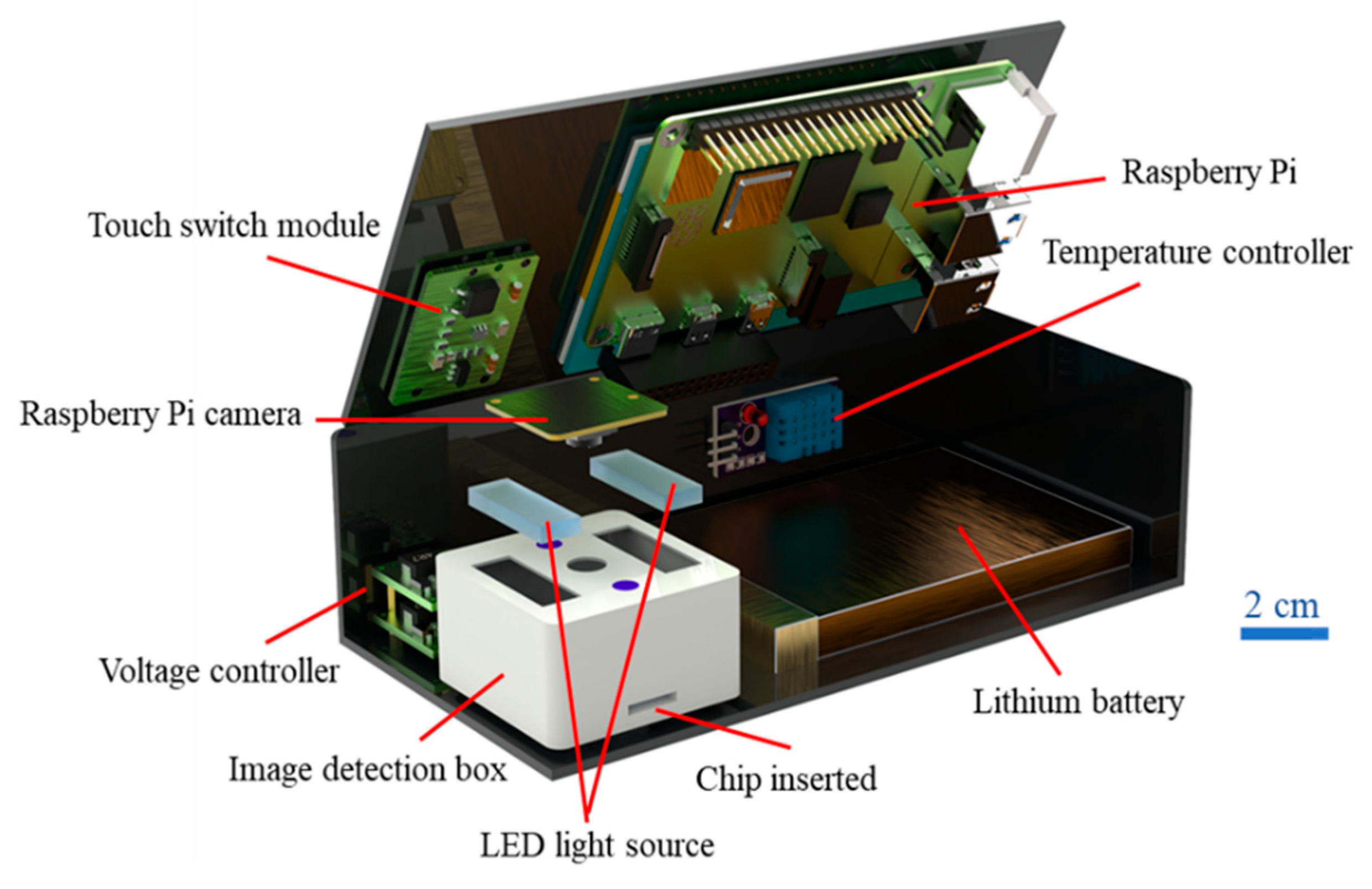
2.3. Hand-Held Detection System
2.4. ALB and CRE Concentrations Detection Process
3. Results and Discussion
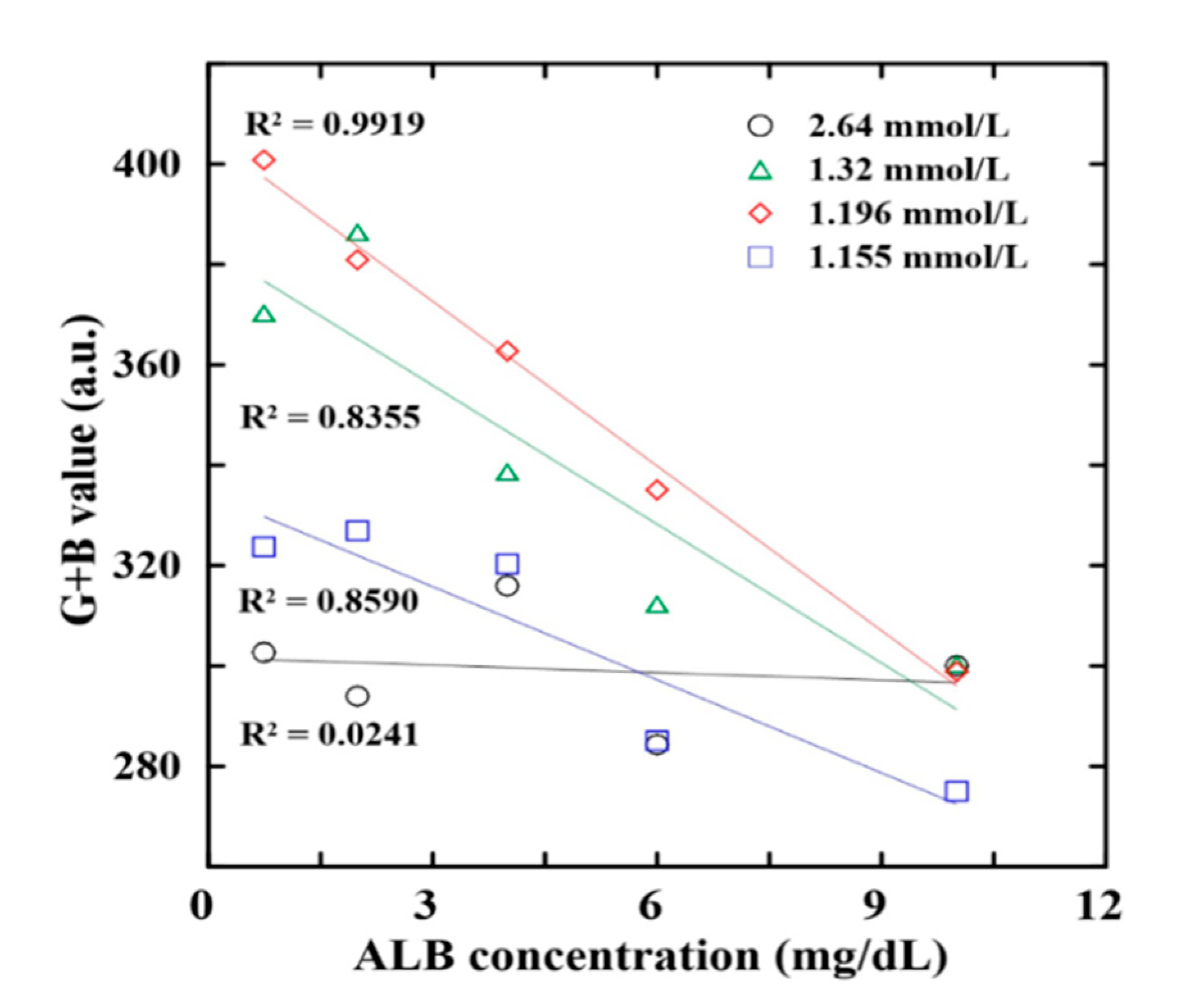
3.1. Optimization of ALB and CRE Reaction Conditions
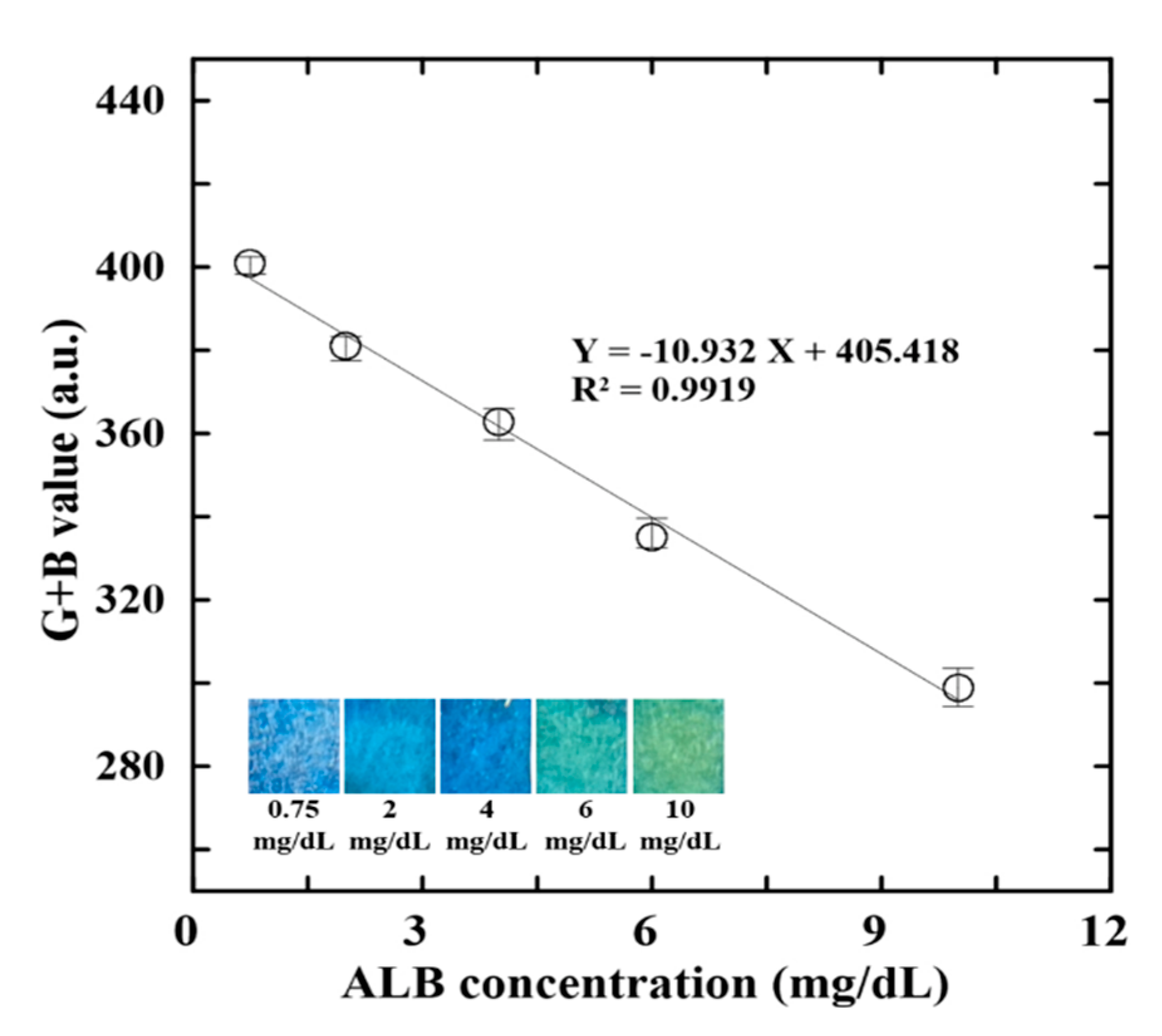
3.2. Calibration Equations for ALB and CRE Detection
3.3. Application of Proposed Assay Platform to Real-World Urine Samples
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jha, V.; Garcia-Garcia, G.; Iseki, K.; Li, Z.; Naicker, S.; Plattner, B.; Saran, R.; Wang, A.Y.-M.; Yang, C.-W. Chronic kidney disease: Global dimension and perspectives. Lancet 2013, 382, 260–272. [Google Scholar] [CrossRef]
- Ndrepepa, G. Uric acid and cardiovascular disease. Clin. Chim. Acta 2018, 484, 150–163. [Google Scholar] [CrossRef]
- Zhang, G.; Yu, Y.; Guo, M.; Lin, B.; Zhang, L. A sensitive determination of albumin in urine by molecularly imprinted electrochemical biosensor based on dual-signal strategy. Sens. Actuators B 2019, 288, 564–570. [Google Scholar] [CrossRef]
- Tseng, C.-C.; Ko, C.-H.; Lu, S.-Y.; Yang, C.-E.; Fu, L.-M.; Li, C.-Y. Rapid electrochemical-biosensor microchip platform for determination of microalbuminuria in CKD patients. Anal. Chim. Acta 2021, 1146, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, D.; Bergman, H.; Burgess, S.; Assimes, T.L.; Bhalla, V.; Ingelsson, E. Urinary albumin, sodium, and potassium and cardiovascular outcomes in the UK biobank: Observational and Mendelian randomization analyses. Hypertens 2020, 75, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Veeralingam, S.; Sahatiya, P.; Badhulika, S. Low cost, flexible and disposable SnSe2 based photoresponsive ammonia sensor for detection of ammonia in urine samples. Sens. Actuators B 2019, 297, 126725. [Google Scholar] [CrossRef]
- Tai, W.-C.; Chang, Y.-C.; Chou, D.; Fu, L.-M. Lab-on-Paper Devices for Diagnosis of Human Diseases Using Urine Samples—A Review. Biosensors 2021, 11, 260. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.-C.; Chen, S.-J.; Lu, S.-Y.; Ko, C.-H.; Wang, J.-M.; Fu, L.-M.; Liu, Y.-H. Novel sliding hybrid microchip detection system for determination of whole blood phosphorus concentration. Chem. Eng. J. 2021, 419, 129592. [Google Scholar]
- Randall, D.; Naidoo, V. Urine: The liquid gold of wastewater. J. Environ. Chem. Eng. 2018, 6, 2627–2635. [Google Scholar] [CrossRef]
- Sung, K.C.; Ryu, S.; Lee, J.Y.; Lee, S.H.; Cheong, E.; Hyun, Y.Y.; Lee, K.B.; Kim, H.; Byrne, C.D. Urine albumin/creatinine ratio below 30 mg/g is a predictor of incident hypertension and cardiovascular mortality. J. Am. Heart Assoc. 2016, 5, e003245. [Google Scholar] [CrossRef] [Green Version]
- Yeom, G.S.; Song, I.-h.; Warkad, S.D.; Shinde, P.B.; Kim, T.; Park, S.-m.; Nimse, S.B. Development of a Novel Benzimidazole-Based Probe and Portable Fluorimeter for the Detection of Cysteine in Human Urine. Biosensors 2021, 11, 420. [Google Scholar] [CrossRef]
- Lindqvist, H.M.; Rådjursöga, M.; Torstensson, T.; Jansson, L.; Ellegård, L.; Winkvist, A. Urine metabolite profiles and nutrient intake based on 4-day weighed food diary in habitual vegans, vegetarians, and omnivores. J. Nutr. 2021, 151, 30–39. [Google Scholar] [CrossRef]
- Hsi, R.S.; Sanford, T.; Goldfarb, D.S.; Stoller, M.L. The role of the 24-hour urine collection in the prevention of kidney stone recurrence. J. Urol. 2017, 197, 1084–1089. [Google Scholar] [CrossRef] [Green Version]
- Yang, J.; Huang, J.; Wei, S.; Zhou, X.; Nong, Y.; Sun, J.; Zhai, Z.; Li, W.; Lu, W. Urine Albumin-Creatinine ratio is associated with prognosis in patients with diabetic foot osteomyelitis. Diabetes Res. Clin. Pract. 2021, 180, 109043. [Google Scholar] [CrossRef]
- Sumida, K.; Nadkarni, G.N.; Grams, M.E.; Sang, Y.; Ballew, S.H.; Coresh, J.; Matsushita, K.; Surapaneni, A.; Brunskill, N.; Chadban, S.J. Conversion of urine protein–creatinine ratio or urine dipstick protein to urine albumin–creatinine ratio for use in chronic kidney disease screening and prognosis: An individual participant–based meta-analysis. Ann. Intern. Med. 2020, 173, 426–435. [Google Scholar] [CrossRef]
- Jain, R.B.; Ducatman, A. Perfluoroalkyl acids serum concentrations and their relationship to biomarkers of renal failure: Serum and urine albumin, creatinine, and albumin creatinine ratios across the spectrum of glomerular function among US adults. Environ. Res. 2019, 174, 143–151. [Google Scholar] [CrossRef]
- Romero-Aroca, P.; Baget-Bernaldiz, M.; Navarro-Gil, R.; Moreno-Ribas, A.; Valls-Mateu, A.; Sagarra-Alamo, R.; Mundet-Tuduri, X. Glomerular filtration rate and/or ratio of urine albumin to creatinine as markers for diabetic retinopathy: A ten-year follow-up study. J. Diabetes Res. 2018, 2018, 5637130. [Google Scholar] [CrossRef]
- Weaver, R.G.; James, M.T.; Ravani, P.; Weaver, C.G.; Lamb, E.J.; Tonelli, M.; Manns, B.J.; Quinn, R.R.; Jun, M.; Hemmelgarn, B.R. Estimating urine albumin-to-creatinine ratio from protein-to-creatinine ratio: Development of equations using same-day measurements. J. Am. Soc. Nephrol. 2020, 31, 591–601. [Google Scholar] [CrossRef]
- Shah, A.; Leslie, S.W.; Ramakrishnan, S. Hyperoxaluria. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Lin, C.-T.; Chiang, Y.-J.; Liu, K.-L.; Lin, K.-J.; Chu, S.-H.; Wang, H.-H. Urine albumin creatinine ratio may predict graft function after kidney transplant. Transplant. Proc. 2019, 51, 1331–1336. [Google Scholar] [CrossRef]
- Chaiyo, S.; Kalcher, K.; Apilux, A.; Chailapakul, O.; Siangproh, W. A novel paper-based colorimetry device for the determination of the albumin to creatinine ratio. Analyst 2018, 143, 5453–5460. [Google Scholar] [CrossRef]
- Wang, M.; Zi, G.; Liu, J.; Song, Y.; Zhao, X.; Wang, Q.; Zhao, T. Self-Powered Biosensor for Specifically Detecting Creatinine in Real Time Based on the Piezo-Enzymatic-Reaction Effect of Enzyme-Modified ZnO Nanowires. Biosensors 2021, 11, 342. [Google Scholar] [CrossRef]
- Chang, T.-H.; Tung, K.-H.; Gu, P.-W.; Yen, T.-H.; Cheng, C.-M. Rapid Simultaneous Determination of Paraquat and Creatinine in Human Serum Using a Piece of Paper. Micromachines 2018, 9, 586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tseng, C.-C.; Yang, R.-J.; Ju, W.-J.; Fu, L.-M. Microfluidic paper-based platform for whole blood creatinine detection. Chem. Eng. J. 2018, 348, 117–124. [Google Scholar] [CrossRef]
- Wang, S.; Chen, H.; Sun, B. Recent progress in food flavor analysis using gas chromatography–ion mobility spectrometry (GC–IMS). Food Chem. 2020, 315, 126158. [Google Scholar] [CrossRef] [PubMed]
- Špánik, I.; Machyňáková, A. Recent applications of gas chromatography with high-resolution mass spectrometry. J. Sep. Sci. 2018, 41, 163–179. [Google Scholar] [CrossRef] [PubMed]
- Chiu, H.-H.; Kuo, C.-H. Gas chromatography-mass spectrometry-based analytical strategies for fatty acid analysis in biological samples. J. Food Drug Anal. 2020, 28, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Mertins, P.; Tang, L.C.; Krug, K.; Clark, D.J.; Gritsenko, M.A.; Chen, L.; Clauser, K.R.; Clauss, T.R.; Shah, P.; Gillette, M.A. Reproducible workflow for multiplexed deep-scale proteome and phosphoproteome analysis of tumor tissues by liquid chromatography–mass spectrometry. Nat. Protoc. 2018, 13, 1632–1661. [Google Scholar] [CrossRef]
- Guo, J.; Huan, T. Comparison of full-scan, data-dependent, and data-independent acquisition modes in liquid chromatography–mass spectrometry based untargeted metabolomics. Anal. Chem. 2020, 92, 8072–8080. [Google Scholar] [CrossRef]
- Zheng, F.; Zhao, X.; Zeng, Z.; Wang, L.; Lv, W.; Wang, Q.; Xu, G. Development of a plasma pseudotargeted metabolomics method based on ultra-high-performance liquid chromatography–mass spectrometry. Nat. Protoc. 2020, 15, 2519–2537. [Google Scholar] [CrossRef]
- Passos, M.L.; Saraiva, M.L.M. Detection in UV-visible spectrophotometry: Detectors, detection systems, and detection strategies. Measurement 2019, 135, 896–904. [Google Scholar] [CrossRef]
- Khan, S.; Newport, D.; Le Calvé, S. Gas detection using portable deep-UV absorption spectrophotometry: A review. Sensors 2019, 19, 5210. [Google Scholar] [CrossRef] [Green Version]
- Karimi-Maleh, H.; Karimi, F.; Alizadeh, M.; Sanati, A.L. Electrochemical sensors, a bright future in the fabrication of portable kits in analytical systems. Chem. Rec. 2020, 20, 682–692. [Google Scholar] [CrossRef]
- Cardoso, R.M.; Kalinke, C.; Rocha, R.G.; Dos Santos, P.L.; Rocha, D.P.; Oliveira, P.R.; Janegitz, B.C.; Bonacin, J.A.; Richter, E.M.; Munoz, R.A. Additive-manufactured (3D-printed) electrochemical sensors: A critical review. Anal. Chim. Acta 2020, 1118, 73–91. [Google Scholar] [CrossRef]
- Yang, R.-J.; Tseng, C.-C.; Ju, W.-J.; Fu, L.-M.; Syu, M.-P. Integrated microfluidic paper-based system for determination of whole blood albumin. Sens. Actuators B 2018, 273, 1091–1097. [Google Scholar] [CrossRef]
- Yang, R.-J.; Tseng, C.-C.; Ju, W.-J.; Wang, H.-L.; Fu, L.-M. A rapid paper-based detection system for determination of human serum albumin concentration. Chem. Eng. J. 2018, 352, 241–246. [Google Scholar] [CrossRef]
- Chankvetadze, B. Recent trends in preparation, investigation and application of polysaccharide-based chiral stationary phases for separation of enantiomers in high-performance liquid chromatography. TrAC Trends Anal. Chem. 2020, 122, 115709. [Google Scholar] [CrossRef]
- Źuvela, P.; Skoczylas, M.; Jay Liu, J.; Baçzek, T.; Kaliszan, R.; Wong, M.W.; Buszewski, B. Column characterization and selection systems in reversed-phase high-performance liquid chromatography. Chem. Rev. 2019, 119, 3674–3729. [Google Scholar]
- Bernardo-Bermejo, S.; Sánchez-López, E.; Castro-Puyana, M.; Marina, M.L. Chiral capillary electrophoresis. TrAC Trends Anal. Chem. 2020, 124, 115807. [Google Scholar] [CrossRef]
- Stolz, A.; Jooß, K.; Höcker, O.; Römer, J.; Schlecht, J.; Neusüß, C. Recent advances in capillary electrophoresis-mass spectrometry: Instrumentation, methodology and applications. Electrophorresis 2019, 40, 79–112. [Google Scholar] [CrossRef] [Green Version]
- Molaei, M.J. A review on nanostructured carbon quantum dots and their applications in biotechnology, sensors, and chemiluminescence. Talanta 2019, 196, 456–478. [Google Scholar] [CrossRef]
- Huang, J.; Pu, K. Activatable molecular probes for second near-infrared fluorescence, chemiluminescence, and photoacoustic imaging. Angew. Chem. Int. Ed. 2020, 59, 11717–11731. [Google Scholar] [CrossRef]
- Hoferichter, M.; Hoid, B.-L.; Kubis, B.; Leupold, S.; Schneider, S.P. Dispersion relation for hadronic light-by-light scattering: Pion pole. J. High Energy Phys. 2018, 2018, 141. [Google Scholar] [CrossRef] [Green Version]
- Wang, C.; Liu, M.; Wang, Z.; Li, S.; Deng, Y.; He, N. Point-of-care diagnostics for infectious diseases: From methods to devices. Nano Today 2021, 37, 101092. [Google Scholar] [CrossRef]
- Jain, S.; Nehra, M.; Kumar, R.; Dilbaghi, N.; Hu, T.; Kumar, S.; Kaushik, A.; Li, C.-Z. Internet of medical things (IoMT)-integrated biosensors for point-of-care testing of infectious diseases. Biosens. Bioelectron. 2021, 179, 113074. [Google Scholar] [CrossRef]
- Cai, Y.; Niu, J.C.; Du, X.L.; Fang, F.; Wu, Z.Y. Novel field amplification for sensitive colorimetric detection of microalbuminuria on a paper-based analytical device. Anal. Chim. Acta 2019, 1080, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Niu, J.C.; Liu, Y.Q.; Du, X.L.; Wu, Z.Y. Online sample clean-up and enrichment of proteins from salty media with dynamic double gradients on a paper fluidic channel. Anal. Chim. Acta 2020, 1100, 149–155. [Google Scholar] [CrossRef]
- Mathaweesansurn, A.; Thongrod, S.; Khongkaew, P.; Phechkrajang, C.M.; Wilairat, P.; Choengchan, N. Simple and fast fabrication of microfluidic paper-based analytical device by contact stamping for multiple-point standard addition assay: Application to direct analysis of urinary creatinine. Talanta 2020, 210, 120675. [Google Scholar] [CrossRef] [PubMed]
- Shojaeifard, Z.; Bordbar, M.M.; Aseman, M.D.; Nabavizadeh, S.M.; Hemmateenejad, B. Collaboration of cyclometalated platinum complexes and metallic nanoclusters for rapid discrimination and detection of biogenic amines through a fluorometric paper-based sensor array. Sens. Actuators B Chem. 2021, 334, 129582. [Google Scholar] [CrossRef]
- Hiraoka, R.; Kuwahara, K.; Wen, Y.C.; Yen, T.H.; Hiruta, Y.; Cheng, C.M.; Citterio, D. Paper-based Device for Naked Eye Urinary Albumin/Creatinine Ratio Evaluation. ACS Sen. 2020, 5, 1110–1118. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.-C.; Tsai, Y.-H.; Shen, C.-F.; He, M.-Y.; Fu, Y.-C.; Sang, C.-Y.; Lee, Y.-T.; Cheng, C.-M. Turntable Paper-Based Device to Detect Escherichia coli. Micromachines 2021, 12, 194. [Google Scholar] [CrossRef] [PubMed]
- Bordbar, M.M.; Sheini, A.; Hashemi, P.; Hajian, A.; Bagheri, H. Disposable Paper-Based Biosensors for the Point-of-Care Detection of Hazardous Contaminations—A Review. Biosensors 2021, 11, 316. [Google Scholar] [CrossRef]
- Colozza, N.; Caratelli, V.; Moscone, D.; Arduini, F. Origami Paper-Based Electrochemical (Bio)Sensors: State of the Art and Perspective. Biosensors 2021, 11, 328. [Google Scholar] [CrossRef]
- Rahbar, M.; Zou, S.; Baharfar, M.; Liu, G. A Customized Microfluidic Paper-Based Platform for Colorimetric Immunosensing: Demonstrated via hCG Assay for Pregnancy Test. Biosensors 2021, 11, 474. [Google Scholar] [CrossRef]
- Hou, C.-Y.; Fu, L.-M.; Ju, W.-J.; Wu, P.-Y. Microfluidic colorimetric system for nitrite detection in foods. Chem. Eng. J. 2020, 398, 125573. [Google Scholar] [CrossRef]
- Ko, C.-H.; Liu, C.-C.; Chen, K.-H.; Sheu, F.; Fu, L.-M.; Chen, S.-J. Microfluidic colorimetric analysis system for sodium benzoate detection in foods. Food Chem. 2021, 345, 128773. [Google Scholar] [CrossRef]
- Chen, K.-H.; Liu, C.-C.; Lu, S.-Y.; Chen, S.-J.; Sheu, F.; Fu, L.-M. Rapid microfluidic analysis detection system for sodium dehydroacetate in foods. Chem. Eng. J. 2022, 427, 131530. [Google Scholar] [CrossRef]
- Kim, T.H.; Hahn, Y.K.; Kim, M.S. Recent Advances of Fluid Manipulation Technologies in Microfluidic Paper-Based Analytical Devices (μPADs) toward Multi-Step Assays. Micromachines 2020, 11, 269. [Google Scholar] [CrossRef] [Green Version]
- Fu, L.-M.; Shih, M.-K.; Hsieh, C.-W.; Ju, W.-J.; Tain, Y.-L.; Cheng, K.-C.; Hsu, J.-H.; Chen, Y.-W.; Hou, C.-Y. Design of an Integrated Microfluidic Paper-Based Chip and Inspection Machine for the Detection of Mercury in Food with Silver Nanoparticles. Biosensors 2021, 11, 491. [Google Scholar] [CrossRef]
- Costa-Rama, E.; Fernández-Abedul, M.T. Paper-Based Screen-Printed Electrodes: A New Generation of Low-Cost Electroanalytical Platforms. Biosensors 2021, 11, 51. [Google Scholar] [CrossRef]
- Laurenciano, C.J.D.; Tseng, C.-C.; Chen, S.-J.; Lu, S.-Y.; Tayo, L.L.; Fu, L.-M. Microfluidic colorimetric detection platform with sliding hybrid PMMA/paper microchip for human urine and blood sample analysis. Talanta 2021, 231, 122362. [Google Scholar] [CrossRef]
- Tseng, C.-C.; Kung, C.-T.; Chen, R.-F.; Tsai, M.-H.; Chao, H.-R.; Wang, Y.-N.; Fu, L.-M. Recent advances in microfluidic paper-based assay devices for diagnosis of human diseases using saliva, tears and sweat samples. Sens. Actuators B 2021, 342, 130078. [Google Scholar] [CrossRef]
- Ortiz-Martínez, M.; Flores-DelaToba, R.; González-González, M.; Rito-Palomares, M. Current Challenges and Future Trends of Enzymatic Paper-Based Point-of-Care Testing for Diabetes Mellitus Type 2. Biosensors 2021, 11, 482. [Google Scholar] [CrossRef] [PubMed]
- Tang, R.H.; Liu, L.N.; Zhang, S.F.; He, X.C.; Li, X.J.; Xu, F.; Ni, Y.H.; Li, F. A review on advances in methods for modification of paper supports for use in point-of-care testing. Microchim. Acta 2019, 186, 1–25. [Google Scholar] [CrossRef]
- Hasan, M.N.; An, R.; Akkus, A.; Akkaynak, D.; Minerick, A.R.; Kharangate, C.R.; Gurkan, U.A. Dynamic pH and Thermal Analysis of Paper-Based Microchip Electrophoresis. Micromachines 2021, 12, 1433. [Google Scholar] [CrossRef] [PubMed]
- Pomili, T.; Donati, P.; Pompa, P.P. Paper-Based Multiplexed Colorimetric Device for the Simultaneous Detection of Salivary Biomarkers. Biosensors 2021, 11, 443. [Google Scholar] [CrossRef]
- Antiochia, R. Paper-Based Biosensors: Frontiers in Point-of-Care Detection of COVID-19 Disease. Biosensors 2021, 11, 110. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.C.; Hsu, J.L.; Tseng, C.C.; Lee, G.B. An integrated microfluidic system for the determination of microalbuminuria by measuring the albumin-to-creatinine ratio. Microfluid. Nanofluidics 2011, 10, 1055–1067. [Google Scholar] [CrossRef]
- Siangproh, W.; Teshima, N.; Sakai, T.; Katoh, S.; Chailapakul, O. Alternative method for measurement of albumin/creatinine ratio using spectrophotometric sequential injection analysis. Talanta 2009, 79, 1111–1117. [Google Scholar] [CrossRef]
- Jia, Y.; Liu, G.; Xu, G.; Li, X.; Shi, Z.; Cheng, C.; Liu, Q. Battery-free and wireless tag for in situ sensing of urinary albumin/creatinine ratio (ACR) for the assessment of albuminuria. Sens. Actuators B Chem. 2022, 367, 32050. [Google Scholar] [CrossRef]



| Gender | Age | Number | <10 mg/dL | 10–300 mg/dL | >300 mg/dL |
|---|---|---|---|---|---|
| Male | All | 19 | 4 | 8 | 7 |
| <40 | 3 | 0 | 2 | 1 | |
| 40-60 | 3 | 1 | 1 | 1 | |
| >60 | 13 | 3 | 5 | 5 | |
| Female | All | 4 | 1 | 1 | 2 |
| <40 | 2 | 1 | 0 | 1 | |
| 40-60 | 1 | 0 | 1 | 0 | |
| >60 | 1 | 0 | 0 | 1 |
| Sequential Injection Analysis [69] | Smartphone EC Method [70] | Microfluidic Chip Method [68] | Paper-Based Colorimetry [21] | Current Platform | |
|---|---|---|---|---|---|
| Sample type | Urine | Artificial urine | Urine | Urine | Urine |
| Detection method | SP-metric | EC | Optical detection | Colorimetric | Colorimetric |
| Sample consumption | 100 μL | 100 mL | 6 μL | 2 μL | 50 μL |
| Analysis time | 1 min | 3 min | 1 min | 30 s | 3 min |
| Detection range | 2–20 mg/L (ALB) | 10–2000 μg/mL (ALB) | 5–220 mg/L (ALB) | 10–350 mg/dL (ALB) | 0.75–10 mg/d (ALB) |
| 5–100 mg/L (CRE) | 10–300 μg/mL (CRE) | 1–100 mg/L (CRE) | 10–400 mg/dL (CRE) | 10–300 mg/dL (CRE) | |
| Operating temperature | NA | NA | 37 °C | NA (ALB) | 40 °C |
| 50 °C (CRE) | |||||
| Reagent or medium | Eosin Y | BSA | Non | BCG, | BCG, |
| Picric acid | Picric acid | immunological fluorescent | Picric acid | Picric acid | |
| Price device | High | High | High | Low | Low |
| Instrument size | Benchtop | Hand-held | Benchtop | Hand-held | Hand-held |
| LOD | 0.06 mg/dL (ALB) | 6.3 mg/dL (ALB) | 0.14 mg/dL (ALB) | 7.1 mg/dL (ALB) | 0.5 mg/dL (ALB) |
| 3.5 mg/dL (CRE) | 9.3 mg/dL (CRE) | 0.4 mg/dL (CRE) | 5.4 mg/dL (CRE) | 5 mg/dL (CRE) | |
| Real sample | 39 | 0 | 40 | 0 | 23 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, S.-J.; Tseng, C.-C.; Huang, K.-H.; Chang, Y.-C.; Fu, L.-M. Microfluidic Sliding Paper-Based Device for Point-of-Care Determination of Albumin-to-Creatine Ratio in Human Urine. Biosensors 2022, 12, 496. https://doi.org/10.3390/bios12070496
Chen S-J, Tseng C-C, Huang K-H, Chang Y-C, Fu L-M. Microfluidic Sliding Paper-Based Device for Point-of-Care Determination of Albumin-to-Creatine Ratio in Human Urine. Biosensors. 2022; 12(7):496. https://doi.org/10.3390/bios12070496
Chicago/Turabian StyleChen, Szu-Jui, Chin-Chung Tseng, Kuan-Hsun Huang, Yu-Chi Chang, and Lung-Ming Fu. 2022. "Microfluidic Sliding Paper-Based Device for Point-of-Care Determination of Albumin-to-Creatine Ratio in Human Urine" Biosensors 12, no. 7: 496. https://doi.org/10.3390/bios12070496
APA StyleChen, S.-J., Tseng, C.-C., Huang, K.-H., Chang, Y.-C., & Fu, L.-M. (2022). Microfluidic Sliding Paper-Based Device for Point-of-Care Determination of Albumin-to-Creatine Ratio in Human Urine. Biosensors, 12(7), 496. https://doi.org/10.3390/bios12070496






