Wearable Devices for Physical Monitoring of Heart: A Review
Abstract
:1. Introduction
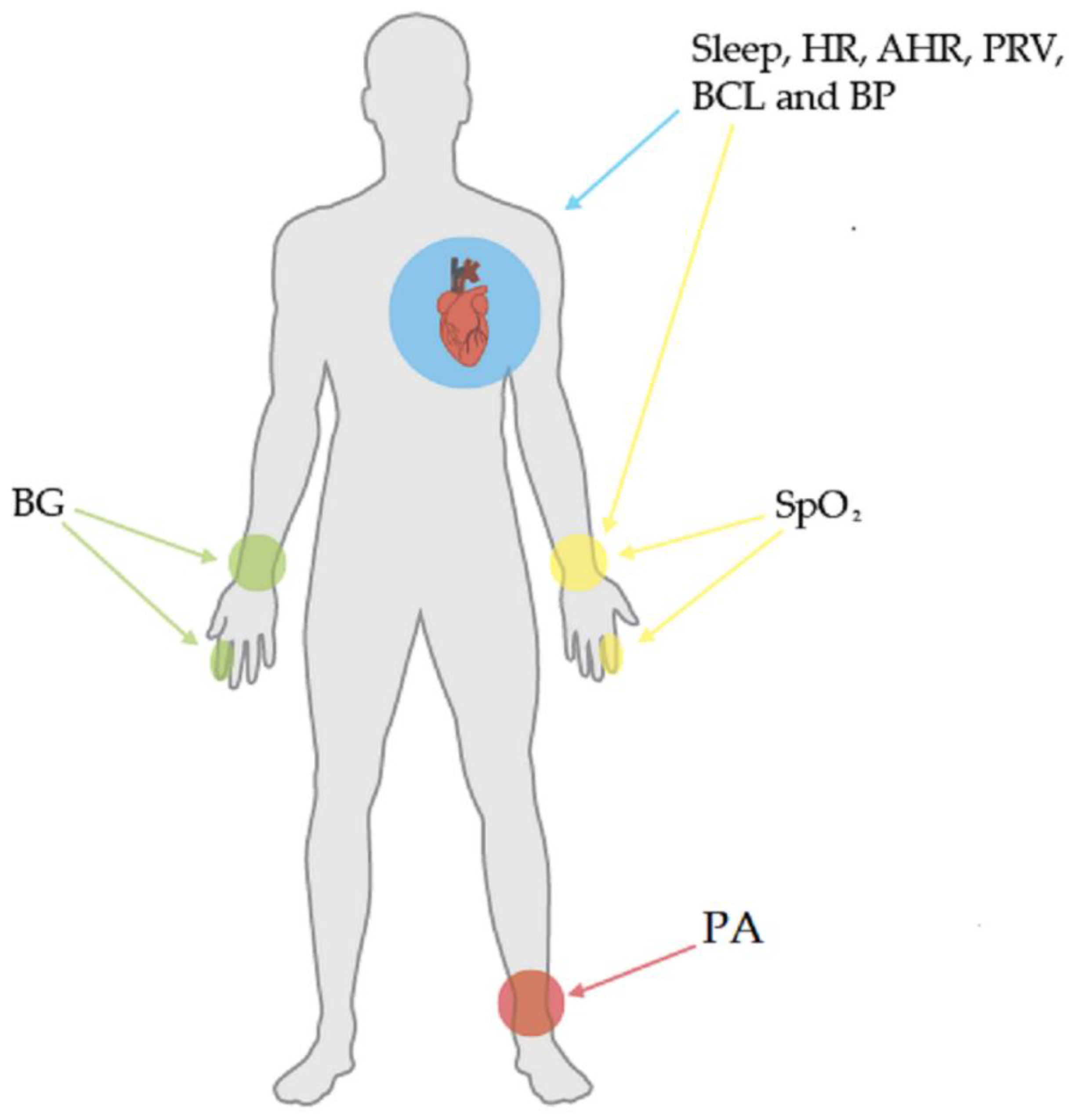
2. Biomedical Variables in CVDs
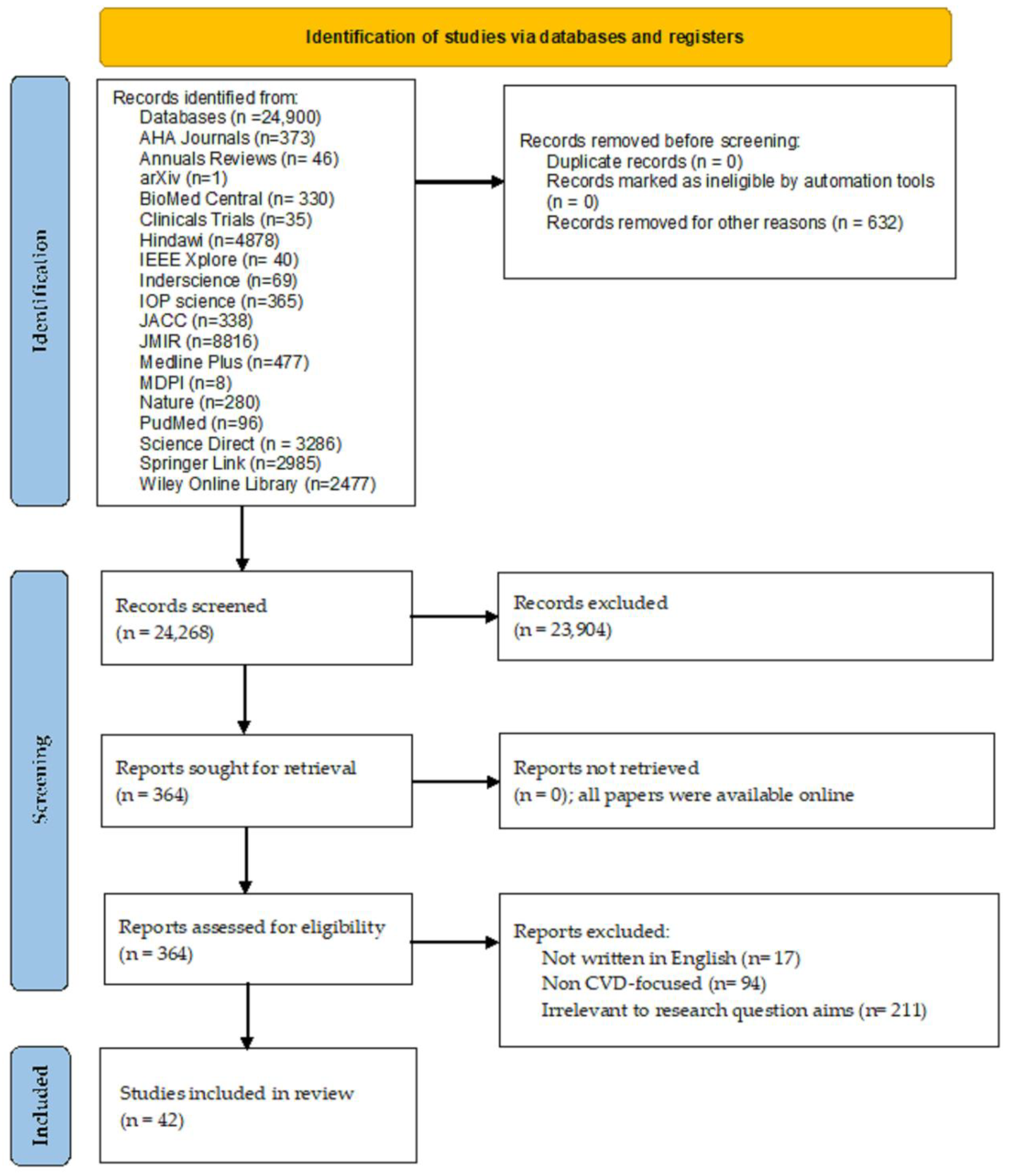
3. Methods
- Main CVDs worldwide.
- Biomedical variables of diagnosed CVDs.
- Wearable devices used to measure these biomedical variables.
- Sensor-based wearable devices available in the market.
- Commercial and noncommercial wearable devices for CVD monitoring.
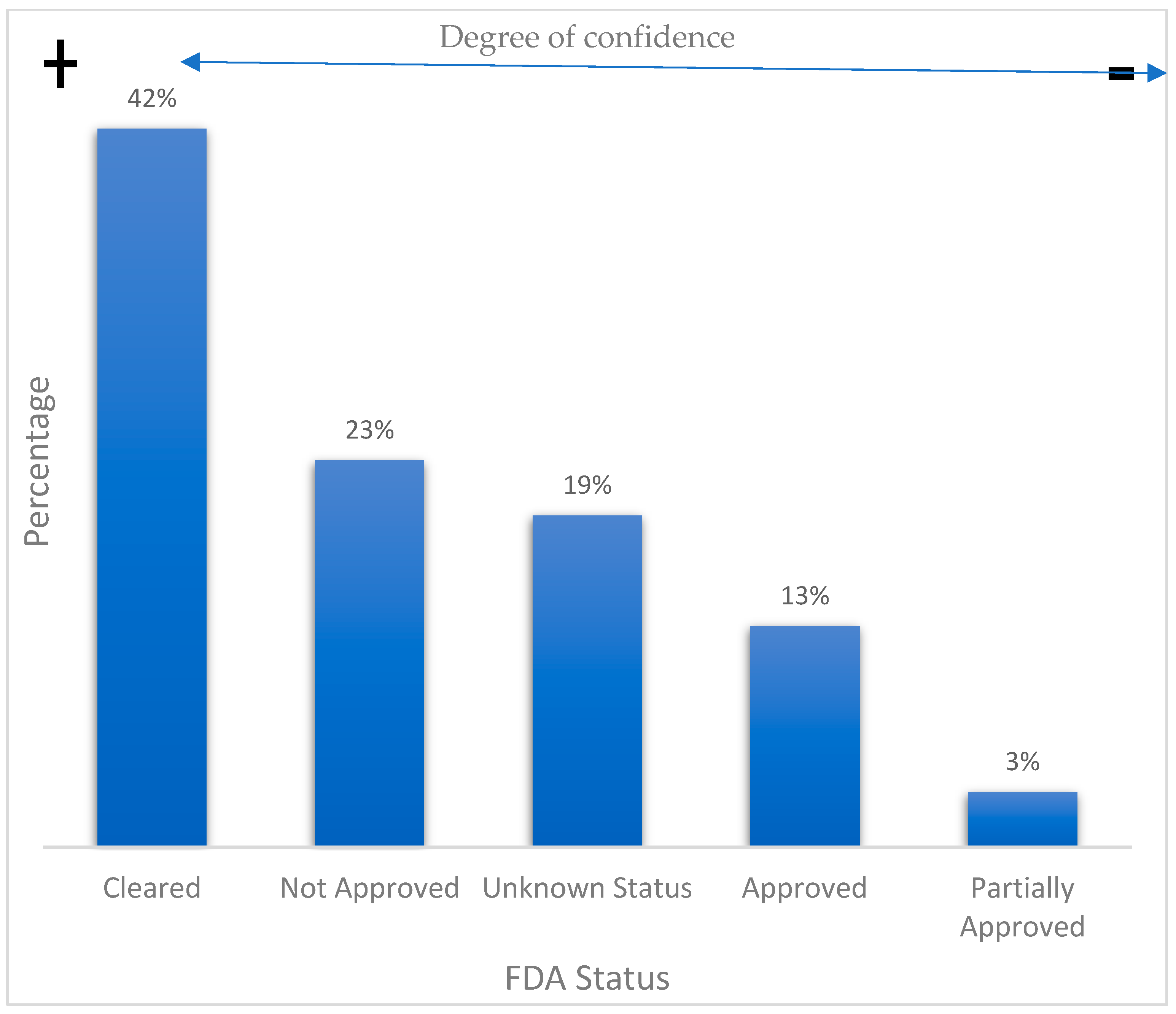
- FDA-approved commercial wearable devices.
4. Results
4.1. Study Selection
4.2. Study Characteristics
5. Commercial Wearable Devices
6. Noncommercial Wearable Devices
- Research year of publication.
- Type of CVD that can be monitored.
- Type of wearable device (e.g., smartwatch and wristband).
- Brief description of the research contribution.
- Sensors or technology used for CVD monitoring.
- Device real-time monitoring capabilities.
7. Discussion
7.1. Challenges and Trends
7.2. Emerging Solutions
7.3. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Noncommunicable Diseases (Who.Int). Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 17 January 2022).
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Cardiovascular Diseases-PAHO/WHO | Pan American Health Organization. Available online: https://www.paho.org/en/topics/cardiovascular-diseases (accessed on 17 January 2022).
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Elshazly, M.B. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Syaifudin, Y.W.; Funabiki, N.; Kuribayashi, M.; Kao, W.C. A proposal of Advanced Widgets learning topic for interactive application in Android programming learning assistance system. SN Comput. Sci. 2021, 2, 172. [Google Scholar] [CrossRef]
- Sarkar, A.; Goyal, A.; Hicks, D.; Sarkar, D.; Hazra, S. Android Application Development: A brief Overview of Android Platforms and Evolution of Security Systems. In Proceedings of the 2019 Third International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud) (I-SMAC) IEEE, Palladam, India, 12–14 December 2019; pp. 73–79. [Google Scholar]
- Cruz-Ramos, N.A.; Alor-Hernández, G.; Colombo-Mendoza, L.O.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L.; Guarneros-Nolasco, L.R. mHealth Apps for Self-Management of Cardiovascular Diseases: A Scoping Review. Healthcare 2022, 10, 322. [Google Scholar] [CrossRef]
- Lobelo, F.; Kelli, H.M.; Tejedor, S.C.; Pratt, M.; McConnell, M.V.; Martin, S.S.; Welk, G.J. The wild wild west: A framework to integrate mHealth software applications and wearables to support physical activity assessment, counseling and interventions for cardiovascular disease risk reduction. Prog. Cardiovasc. Dis. 2016, 58, 584–594. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pevnick, J.M.; Birkeland, K.; Zimmer, R.; Elad, Y.; Kedan, I. Wearable technology for cardiology: An update and framework for the future. Trends Cardiovasc. Med. 2018, 28, 144–150. [Google Scholar] [CrossRef]
- Akinosun, A.S.; Polson, R.; Diaz-Skeete, Y.; De Kock, J.H.; Carragher, L.; Leslie, S.; Gorely, T. Digital Technology Interventions for Risk Factor Modification in Patients with Cardiovascular Disease: Systematic Review and Meta-analysis. JMIR mHealth uHealth 2021, 9, e21061. [Google Scholar] [CrossRef]
- Ji, N.; Xiang, T.; Bonato, P.; Lovell, N.H.; Ooi, S.Y.; Clifton, D.A.; Zhang, Y.T. Recommendation to Use Wearable-Based mHealth in Closed-Loop Management of Acute Cardiovascular Disease Patients During the COVID-19 Pandemic. IEEE J. Biomed. Health Inform. 2021, 25, 903–908. [Google Scholar] [CrossRef]
- Hong, Y.J.; Jeong, H.; Cho, K.W.; Lu, N.; Kim, D.H. Wearable and implantable devices for cardiovascular healthcare: From monitoring to therapy based on flexible and stretchable electronics. Adv. Funct. Mater. 2019, 29, 1808247. [Google Scholar] [CrossRef]
- Lin, J.; Fu, R.; Zhong, X.; Yu, P.; Tan, G.; Li, W.; Ning, C. Wearable sensors and devices for real-time cardiovascular disease monitoring. Cell Rep. Phys. Sci. 2021, 2, 100541. [Google Scholar] [CrossRef]
- Sana, F.; Isselbacher, E.M.; Singh, J.P.; Heist, E.K.; Pathik, B.; Armoundas, A.A. Wearable devices for ambulatory cardiac monitoring: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020, 75, 1582–1592. [Google Scholar] [CrossRef] [PubMed]
- Dagher, L.; Shi, H.; Zhao, Y.; Marrouche, N.F. Wearables in cardiology: Here to stay. Heart Rhythm 2020, 17, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Cho, K.W.; Lee, W.H.; Kim, B.S.; Kim, D.H. Sensors in heart-on-a-chip: A review on recent progress. Talanta 2020, 219, 121269. [Google Scholar] [CrossRef] [PubMed]
- Promphet, N.; Ummartyotin, S.; Ngeontae, W.; Puthongkham, P.; Rodthongkum, N. Non-invasive wearable chemical sensors in real-life applications. Anal. Chim. Acta 2021, 1179, 338643. [Google Scholar] [CrossRef]
- Nasiri, S.; Khosravani, M.R. Progress and challenges in fabrication of wearable sensors for health monitoring. Sens. Actuators A Phys. 2020, 312, 112105. [Google Scholar] [CrossRef]
- Duncker, D.; Ding, W.Y.; Etheridge, S.; Noseworthy, P.A.; Veltmann, C.; Yao, X.; Gupta, D. Smart wearables for cardiac monitoring—Real-world use beyond atrial fibrillation. Sensors 2021, 21, 2539. [Google Scholar] [CrossRef]
- Kinast, B.; Lutz, M.; Schreiweis, B. Telemonitoring of Real-World Health Data in Cardiology: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 9070. [Google Scholar] [CrossRef]
- Chen, S.; Qi, J.; Fan, S.; Qiao, Z.; Yeo, J.C.; Lim, C.T. Flexible wearable sensors for cardiovascular health monitoring. Adv. Healthc. Mater. 2021, 10, 2100116. [Google Scholar] [CrossRef]
- Khan, Y.; Ostfeld, A.E.; Lochner, C.M.; Pierre, A.; Arias, A.C. Monitoring of vital signs with flexible and wearable medical devices. Adv. Mater. 2016, 28, 4373–4395. [Google Scholar] [CrossRef]
- Wang, P.; Lin, Z.; Yan, X.; Chen, Z.; Ding, M.; Song, Y.; Meng, L. A wearable ECG monitor for deep learning based real-time cardiovascular disease detection. arXiv 2022, arXiv:2201.10083. [Google Scholar]
- Scrugli, M.A.; Loi, D.; Raffo, L.; Meloni, P. An adaptive cognitive sensor node for ECG monitoring in the Internet of Medical Things. IEEE Access 2021, 10, 1688–1705. [Google Scholar] [CrossRef]
- Ramasamy, M.; Varadan, V. Wireless Wearable and Implantable Monitoring and Therapeutic Systems for Cardiac Diseases and Neurological Disorders. In The Electrochemical Society Meeting Abstracts; Keynote; IOP Publishing: Bristol, UK, 2018; p. 2037. [Google Scholar]
- Rai, P.; Oh, S.; Shyamkumar, P.; Ramasamy, M.; Harbaugh, R.E.; Varadan, V.K. Nano-bio-textile sensors with mobile wireless platform for wearable health monitoring of neurological and cardiovascular disorders. J. Electrochem. Soc. 2013, 161, B3116. [Google Scholar] [CrossRef]
- Hannan, A.L.; Harders, M.P.; Hing, W.; Climstein, M.; Coombes, J.S.; Furness, J. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: Systematic review and meta-analysis. BMC Sports Sci. Med. Rehabil. 2019, 11, 14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joe, A.; Coronel, B.D.; Coakes, C.E.; Mainous, A., III. Is there a benefit to patients using wearable devices such as Fitbit or health apps on mobiles? A systematic review. Am. J. Med. 2019, 132, 1394–1400. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, A.; Changolkar, S.; Patel, M.S. Wearable Devices to Monitor and Reduce the Risk of Cardiovascular Disease: Evidence and Opportunities. Annu. Rev. Med. 2021, 72, 459–471. [Google Scholar] [CrossRef]
- Rens, N.; Gandhi, N.; Mak, J.; Paul, J.; Bent, D.; Liu, S.; Aalami, O. Activity data from wearables as an indicator of functional capacity in patients with cardiovascular disease. PLoS ONE 2021, 16, e0247834. [Google Scholar] [CrossRef]
- Hammond-Haley, M.; Allen, C.; Han, J.; Patterson, T.; Marber, M.; Redwood, S. Utility of wearable physical activity monitors in cardiovascular disease: A systematic review of 11,464 patients and recommendations for optimal use. Eur. Heart J. Digit. Health 2021, 2, 231–243. [Google Scholar] [CrossRef]
- Xie, Y.; Lu, L.; Gao, F.; He, S.J.; Zhao, H.J.; Fang, Y.; Dong, Z. Integration of Artificial Intelligence, Blockchain, and Wearable Technology for Chronic Disease Management: A New Paradigm in Smart Healthcare. Curr. Med. Sci. 2021, 41, 1123–1133. [Google Scholar] [CrossRef]
- Ferguson, C.; Hickman, L.D.; Turkmani, S.; Breen, P.; Gargiulo, G.; Inglis, S.C. “Wearables only work on patients that wear them”: Barriers and facilitators to the adoption of wearable cardiac monitoring technologies. Cardiovasc. Digit. Health J. 2021, 2, 137–147. [Google Scholar] [CrossRef]
- Tobin, S.Y.; Williams, P.G.; Baron, K.G.; Halliday, T.M.; Depner, C.M. Challenges and Opportunities for Applying Wearable Technology to Sleep. Sleep Med. Clin. 2021, 16, 607–618. [Google Scholar] [CrossRef]
- Nuvvula, S.; Ding, E.Y.; Saleeba, C.; Shi, Q.; Wang, Z.; Kapoor, A.; McManus, D.D. NExUS-Heart: Novel examinations using smart technologies for heart health—Data sharing from commercial wearable devices and telehealth engagement in participants with or at risk of atrial fibrillation. Cardiovasc. Digit. Health J. 2021, 2, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, N.P.; Adusumalli, S.; Small, D.S.; Morris, A.; Feingold, J.; Ha, Y.P.; Patel, M.S. Loss-framed financial incentives and personalized goal-setting to increase physical activity among ischemic heart disease patients using wearable devices: The ACTIVE REWARD randomized trial. J. Am. Heart Assoc. 2018, 7, e009173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castaneda, D.; Esparza, A.; Ghamari, M.; Soltanpur, C.; Nazeran, H. A review on wearable photoplethysmography sensors and their potential future applications in health care. Int. J. Biosens. Bioelectron. 2018, 4, 195. [Google Scholar] [PubMed] [Green Version]
- Shabaan, M.; Arshid, K.; Yaqub, M.; Jinchao, F.; Zia, M.S.; Bojja, G.R.; Munir, R. Survey: Smartphone-based assessment of cardiovascular diseases using ECG and PPG analysis. BMC Med. Inform. Decis. Mak. 2020, 20, 177. [Google Scholar] [CrossRef]
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 2020, 140, 100523. [Google Scholar] [CrossRef]
- Guo, Y.; Liu, X.; Peng, S.; Jiang, X.; Xu, K.; Chen, C.; Chen, W. A review of wearable and unobtrusive sensing technologies for chronic disease management. Comput. Biol. Med. 2021, 129, 104163. [Google Scholar] [CrossRef]
- Tandon, A.; De Ferranti, S.D. Wearable Biosensors in Pediatric Cardiovascular Disease: Promises and Pitfalls Toward Generating Actionable Insights. Circulation 2019, 140, 350–352. [Google Scholar] [CrossRef]
- Nahavandi, D.; Alizadehsani, R.; Khosravi, A.; Acharya, U.R. Application of artificial intelligence in wearable devices: Opportunities and challenges. Comput. Methods Programs Biomed. 2022, 213, 106541. [Google Scholar] [CrossRef]
- Reda, A.; El-Safty, S.A.; Selim, M.M.; Shenashen, M.A. Optical glucose biosensor built-in disposable strips and wearable electronic devices. Biosens. Bioelectron. 2021, 185, 113237. [Google Scholar] [CrossRef]
- Surantha, N.; Atmaja, P.; Wicaksono, M. A Review of Wearable Internet-of-Things Device for Healthcare. Procedia Comput. Sci. 2021, 179, 936–943. [Google Scholar] [CrossRef]
- Khoshmanesh, F.; Thurgood, P.; Pirogova, E.; Nahavandi, S.; Baratchi, S. Wearable sensors: At the frontier of personalised health monitoring, smart prosthetics and assistive technologies. Biosens. Bioelectron. 2021, 176, 112946. [Google Scholar] [CrossRef] [PubMed]
- Santo, K.; Redfern, J. Digital health innovations to improve cardiovascular disease care. Curr. Atheroscler. Rep. 2020, 22, 71. [Google Scholar] [CrossRef] [PubMed]
- DeVore, A.D.; Wosik, J.; Hernandez, A.F. The future of wearables in heart failure patients. JACC Heart Fail. 2019, 7, 922–932. [Google Scholar] [CrossRef]
- Burnham, J.P.; Lu, C.; Yaeger, L.H.; Bailey, T.C.; Kollef, M.H. Using wearable technology to predict health outcomes: A literature review. J. Am. Med. Inform. Assoc. 2018, 25, 1221–1227. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heart Information Center: Heart Disease Risk Factors | Texas Heart Institute. Available online: http://www.texasheart.org/heart-health/heart-information-center/topics/heart-disease-risk-factors/ (accessed on 6 November 2021).
- Kristoffersson, A.; Lindén, M. A Systematic Review of Wearable Sensors for Monitoring Physical Activity. Sensors 2022, 22, 573. [Google Scholar] [CrossRef] [PubMed]
- Imtiaz, S.A. A systematic review of sensing technologies for wearable sleep staging. Sensors 2021, 21, 1562. [Google Scholar] [CrossRef]
- Draghici, A.E.; Taylor, J.A. The physiological basis and measurement of heart rate variability in humans. J. Physiol. Anthropol. 2016, 35, 22. [Google Scholar] [CrossRef] [Green Version]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Zhang, X.; Zhao, L.; Liu, F.; Chen, X.; Yao, Y.; Li, J. Signal quality assessment and lightweight QRS detection for wearable ECG SmartVest system. IEEE Internet Things J. 2018, 6, 1363–1374. [Google Scholar] [CrossRef]
- Pan, J.; Tompkins, W.J. A real-time QRS detection algorithm. IEEE Trans. Biomed. Eng. 1985, 3, 230–236. [Google Scholar] [CrossRef]
- Biswas, D.; Simões-Capela, N.; Van Hoof, C.; Van Helleputte, N. Heart rate estimation from wrist-worn photoplethysmography: A review. IEEE Sens. J. 2019, 19, 6560–6570. [Google Scholar] [CrossRef]
- Acharya, U.R.; Joseph, K.P.; Kannathal, N.; Lim, C.M.; Suri, J.S. Heart rate variability: A review. Med. Biol. Eng. Comput. 2006, 44, 1031–1051. [Google Scholar] [CrossRef] [PubMed]
- Dodds, K.L.; Miller, C.B.; Kyle, S.D.; Marshall, N.S.; Gordon, C.J. Heart rate variability in insomnia patients: A critical review of the literature. Sleep Med. Rev. 2017, 33, 88–100. [Google Scholar] [CrossRef]
- Perpetuini, D.; Di Credico, A.; Filippini, C.; Izzicupo, P.; Cardone, D.; Chiacchiaretta, P.; Merla, A. Is It Possible to Estimate Average Heart Rate from Facial Thermal Imaging? Eng. Proc. 2021, 8, 10. [Google Scholar]
- Yuda, E.; Shibata, M.; Ogata, Y.; Ueda, N.; Yambe, T.; Yoshizawa, M.; Hayano, J. Pulse rate variability: A new biomarker, not a surrogate for heart rate variability. J. Physiol. Anthropol. 2020, 39, 21. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Das, R. Comparing heart rate variability with polar H10 sensor and pulse rate variability with LYFAS: A novel study. J. Biomed. Eng. Technol. 2021, 9, 1–9. [Google Scholar] [CrossRef]
- Miao, F.; Fu, N.; Zhang, Y.T.; Ding, X.R.; Hong, X.; He, Q.; Li, Y. A novel continuous blood pressure estimation approach based on data mining techniques. IEEE J. Biomed. Health Inform. 2017, 21, 1730–1740. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.A.; Rudenski, A.; Gibson, J.; Howard, L.; O’Driscoll, R. Relating oxygen partial pressure, saturation and content: The haemoglobin–oxygen dissociation curve. Breathe 2015, 11, 194–201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almarshad, M.A.; Islam, M.S.; Al-Ahmadi, S.; BaHammam, A.S. Diagnostic Features and Potential Applications of PPG Signal in Healthcare: A Systematic Review. Healthcare 2022, 10, 547. [Google Scholar] [CrossRef]
- Zarich, S.W. Treating the diabetic patient: Appropriate care for glycemic control and cardiovascular disease risk factors. Rev. Cardiovasc. Med. 2003, 4, 19–28. [Google Scholar]
- Siddiqui, S.A.; Zhang, Y.; Lloret, J.; Song, H.; Obradovic, Z. Pain-free blood glucose monitoring using wearable sensors: Recent advancements and future prospects. IEEE Rev. Biomed. Eng. 2018, 11, 21–35. [Google Scholar] [CrossRef] [PubMed]
- Hina, A.; Saadeh, W. A noninvasive glucose monitoring SoC based on single wavelength photoplethysmography. IEEE Trans. Biomed. Circuits Syst. 2020, 14, 504–515. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Mei, Z.; Zhang, Y.; Ma, X.; Lo, B.; Chen, D.; Zhang, Y. A noninvasive blood glucose monitoring system based on smartphone PPG signal processing and machine learning. IEEE Trans. Ind. Inform. 2020, 16, 7209–7218. [Google Scholar] [CrossRef]
- Kim, J.; Campbell, A.S.; Wang, J. Wearable non-invasive epidermal glucose sensors: A review. Talanta 2018, 177, 163–170. [Google Scholar] [CrossRef]
- Soliman, G.A. Dietary cholesterol and the lack of evidence in cardiovascular disease. Nutrients 2018, 10, 780. [Google Scholar] [CrossRef] [Green Version]
- Yadav, H.M.; Park, J.D.; Kang, H.C.; Lee, J.J. Recent development in nanomaterial-based electrochemical sensors for cholesterol detection. Chemosensors 2021, 9, 98. [Google Scholar] [CrossRef]
- Zhazykbayeva, S.; Pabel, S.; Mügge, A.; Sossalla, S.; Hamdani, N. The molecular mechanisms associated with the physiological responses to inflammation and oxidative stress in cardiovascular diseases. Biophys. Rev. 2020, 12, 947–968. [Google Scholar] [CrossRef]
- D’Oria, R.; Schipani, R.; Leonardini, A.; Natalicchio, A.; Perrini, S.; Cignarelli, A.; Giorgino, F. The role of oxidative stress in cardiac disease: From physiological response to injury factor. Oxidative Med. Cell. Longev. 2020, 2020, 5732956. [Google Scholar] [CrossRef]
- Wheeler-Jones, C.P. Cell signalling in the cardiovascular system: An overview. Heart 2005, 91, 1366–1374. [Google Scholar] [CrossRef] [Green Version]
- Sutanto, H.; Lyon, A.; Lumens, J.; Schotten, U.; Dobrev, D.; Heijman, J. Cardiomyocyte calcium handling in health and disease: Insights from in vitro and in silico studies. Prog. Biophys. Mol. Biol. 2020, 157, 54–75. [Google Scholar] [CrossRef]
- Manolis, A.S.; Manolis, A.A.; Manolis, T.A.; Apostolaki, N.E.; Apostolopoulos, E.J.; Melita, H.; Katsiki, N. Mitochondrial dysfunction in cardiovascular disease: Current status of translational research/clinical and therapeutic implications. Med. Res. Rev. 2021, 41, 275–313. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Moher, D. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef] [PubMed]
- ECG Monitor & Activity Watch-Move ECG | Withings. Available online: https://www.withings.com/ca/en/move-ecg (accessed on 1 November 2021).
- Fitbit Versa 2™ Smartwatch | Shop. Available online: https://www.fitbit.com/global/us/products/smartwatches/versa?sku=507BKBK (accessed on 9 January 2022).
- Omron Healthcare Wellness & Healthcare Products. Available online: http://www.omronhealthcare.com (accessed on 8 November 2021).
- Apple Watch Series 7-Apple (MX). Available online: https://www.apple.com/mx/apple-watch-series-7/ (accessed on 1 November 2021).
- HUAWEI WATCH GT, 2-Week Battery-Life, Built-in GPS Smartwatch ∣ HUAWEI United. Available online: https://consumer.huawei.com/us/wearables/watch-gt/ (accessed on 9 January 2022).
- MOCACuff (mocacare.com). Available online: http://www.mocacare.com/mocacuff/ (accessed on 1 November 2021).
- Fitbit Charge 4™ & Charge 3™ Classic Accessory Bands | Shop. Available online: www.fitbit.com/global/us/products/accessories/charge3-classic?sku=168ABBKS (accessed on 9 January 2022).
- Armband HRM | Shop Biostrap. Available online: http://shop.biostrap.com/collections/accessories/products/biostrap-armband-hrm (accessed on 1 November 2021).
- Mi Smart Band 6-No.1 Wearable Band Brand in the World-Xiaomi Global Official. Available online: https://www.mi.com/global/product/mi-smart-band-6/ (accessed on 9 January 2022).
- Heart HEALBE GoBe3. Available online: http://www.healbe.com (accessed on 8 November 2021).
- Home-Sotera Wireless. Available online: http://www.soterawireless.com (accessed on 9 January 2021).
- Oxitone 1000M-Oxitone. Available online: https://www.oxitone.com/oxitone-1000m/ (accessed on 8 November 2021).
- Patient Monitoring System | Wireless Health Monitoring System |Wearables Technology in Healthcare. Available online: https://www.vincense.com (accessed on 8 November 2021).
- ZOLL LifeVest Wearable Defibrillator | ZOLL Medical Corporation. Available online: https://lifevest.zoll.com/ (accessed on 1 November 2021).
- Hexoskin Smart Shirts-Cardiac, Respiratory, Sleep & Activity Metrics. Available online: https://www.hexoskin.com (accessed on 1 November 2021).
- Owlet Smart Sock 3 Baby Monitor. Available online: http://www.sleeplay.com/products/owlet-smart-sock-2-baby-monitor (accessed on 1 November 2021).
- Technology (spirehealth.com). Available online: http://www.spirehealth.com/technology (accessed on 1 November 2021).
- Vivometrics, Inc. LifeShirt System to Be Used in Study Examining Human Attention in Real World Settings | BioSpace. Available online: https://www.biospace.com/article/releases/vivometrics-inc-lifeshirt-system-to-be-used-in-study-examining-human-attention-in-real-world-settings-/ (accessed on 12 October 2021).
- Master Caution® Smart Garments by HealthWatch Technologies. Available online: http://healthwatchtech.com/mastercaution/ (accessed on 8 November 2021).
- HxM | Zephyr™ Performance Systems. Available online: https://www.zephyranywhere.com/system/hxm (accessed on 8 November 2021).
- Uninterrupted Ambulatory Cardiac Monitoring. Available online: https://www.irhythmtech.com/ (accessed on 1 November 2021).
- LISTENS TO THE BEAT-Preventice Solutions. Available online: https://www.preventicesolutions.com/patients/body-guardian-heart (accessed on 1 November 2021).
- MCOT Patch-BioTelemetry, a Philips Company (gobio.com). Available online: http://www.gobio.com/heart-monitoring1/stroke/ (accessed on 9 January 2022).
- Wellysis. Available online: http://www.wellysis.com (accessed on 1 November 2021).
- Home-VitalConnect. Available online: http://www.vitalconnect.com (accessed on 8 November 2021).
- KardiaMobile | AliveCor. Available online: https://www.alivecor.es/kardiamobile (accessed on 1 November 2021).
- PAI Health. Available online: http://www.paihealth.com (accessed on 1 November 2021).
- Ōura Ring: Accurate Health Information Accessible to Everyone. Available online: https://ouraring.com/ (accessed on 1 November 2021).
- iHealth Fingertip Pulse Oximeter (Wired)-iHealth Labs Inc. Available online: http://ihealthlabs.com/products/ihealth-fingertip-pulse-oximeter-wired (accessed on 1 November 2021).
- FreeWavz. Available online: http://www.freewavz.com/store/freewavz-blue/ (accessed on 8 November 2021).
- iHealth Track le Tensiomètre Connecté le Plus Abordable. Available online: http://www.ihealthlabs.eu/fr/24-hypertension (accessed on 8 November 2021).
- Lown, M.; Brown, M.; Brown, C.; Yue, A.M.; Shah, B.N.; Corbett, S.J.; Little, P. Machine learning detection of Atrial Fibrillation using wearable technology. PLoS ONE 2020, 15, e0227401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kwon, S.; Hong, J.; Choi, E.K.; Lee, B.; Baik, C.; Lee, E.; Yi, Y. Detection of atrial fibrillation using a ring-type wearable device (CardioTracker) and deep learning analysis of photoplethysmography signals: Prospective observational proof-of-concept study. J. Med. Internet Res. 2020, 22, e16443. [Google Scholar] [CrossRef] [PubMed]
- Rajakariar, K.; Koshy, A.N.; Sajeev, J.K.; Nair, S.; Roberts, L.; Teh, A.W. Accuracy of a smartwatch based single-lead electrocardiogram device in detection of atrial fibrillation. Heart 2020, 106, 665–670. [Google Scholar] [CrossRef]
- Raja, J.M.; Elsakr, C.; Roman, S.; Cave, B.; Pour-Ghaz, I.; Nanda, A.; Khouzam, R.N. Apple watch, wearables, and heart rhythm: Where do we stand? Ann. Transl. Med. 2019, 7, 417. [Google Scholar] [CrossRef]
- Fukuma, N.; Hasumi, E.; Fujiu, K.; Waki, K.; Toyooka, T.; Komuro, I.; Ohe, K. Feasibility of a T-shirt-type wearable electrocardiography monitor for detection of covert atrial fibrillation in young healthy adults. Sci. Rep. 2019, 9, 11768. [Google Scholar] [CrossRef] [Green Version]
- Tajrishi, F.Z.; Chitsazan, M.; Chitsazan, M.; Shojaei, F.; Gunnam, V.; Chi, G. Smartwatch for the detection of atrial fibrillation. Crit. Pathw. Cardiol. 2019, 18, 176–184. [Google Scholar] [CrossRef]
- Wasserlauf, J.; You, C.; Patel, R.; Valys, A.; Albert, D.; Passman, R. Smartwatch performance for the detection and quantification of atrial fibrillation. Circ. Arrhythm. Electrophysiol. 2019, 12, e006834. [Google Scholar] [CrossRef]
- Shen, Y.; Voisin, M.; Aliamiri, A.; Avati, A.; Hannun, A.; Ng, A. Ambulatory Atrial FIBRILLATION monitoring Using Wearable Photoplethysmography with Deep Learning. In Proceedings of the 25th ACM SIGKDD International Conference on Knowledge Discovery & Data Mining, Washington, DC, USA, 14–18 August 2022; pp. 1909–1916. [Google Scholar]
- Marsili, I.A.; Biasiolli, L.; Masè, M.; Adami, A.; Andrighetti, A.O.; Ravelli, F.; Nollo, G. Implementation and validation of real-time algorithms for atrial fibrillation detection on a wearable ECG device. Comput. Biol. Med. 2020, 116, 103540. [Google Scholar] [CrossRef]
- Sološenko, A.; Petrėnas, A.; Paliakaitė, B.; Sörnmo, L.; Marozas, V. Detection of atrial fibrillation using a wrist-worn device. Physiol. Meas. 2019, 40, 025003. [Google Scholar] [CrossRef] [PubMed]
- Bumgarner, J.M.; Lambert, C.T.; Hussein, A.A.; Cantillon, D.J.; Baranowski, B.; Wolski, K.; Tarakji, K.G. Smartwatch algorithm for automated detection of atrial fibrillation. J. Am. Coll. Cardiol. 2018, 71, 2381–2388. [Google Scholar] [CrossRef]
- Steinhubl, S.R.; Waalen, J.; Edwards, A.M.; Ariniello, L.M.; Mehta, R.R.; Ebner, G.S.; Topol, E.J. Effect of a home-based wearable continuous ECG monitoring patch on detection of undiagnosed atrial fibrillation: The mSToPS randomized clinical trial. JAMA 2018, 320, 146–155. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gotlibovych, I.; Crawford, S.; Goyal, D.; Liu, J.; Kerem, Y.; Benaron, D.; Li, Y. End-to-end deep learning from raw sensor data: Atrial fibrillation detection using wearables. arXiv 2018, arXiv:1807.10707. [Google Scholar]
- Cheung, C.C.; Krahn, A.D.; Andrade, J.G. The emerging role of wearable technologies in arrhythmia detection. Can. J. Cardiol. 2018, 34, 1083–1087. [Google Scholar] [CrossRef] [PubMed]
- Shashikumar, S.P.; Shah, A.J.; Li, Q.; Clifford, G.D.; Nemati, S. A Deep Learning Approach to Monitoring and Detecting Atrial Fibrillation Using Wearable Technology. In Proceedings of the 2017 IEEE EMBS International Conference on Biomedical & Health Informatics (BHI), Orlando, FL, USA, 16–19 February 2017; pp. 141–144. [Google Scholar]
- Kelly, J.P.; Sharma, A. Accelerating the Use of Wearable Devices in Heart Failure. Heart Fail. 2021, 9, 836–838. [Google Scholar] [CrossRef] [PubMed]
- Anchouche, K.; Elharram, M.; Oulousian, E.; Razaghizad, A.; Avram, R.; Marquis-Gravel, G.; Sharma, A. Use of actigraphy (wearable digital sensors to monitor activity) in heart failure randomized clinical trials: A scoping review. Can. J. Cardiol. 2021, 37, 1438–1449. [Google Scholar] [CrossRef]
- Shah, A.J.; Isakadze, N.; Levantsevych, O.; Vest, A.; Clifford, G.; Nemati, S. Detecting heart failure using wearables: A pilot study. Physiol. Meas. 2020, 41, 044001. [Google Scholar] [CrossRef]
- Singhal, A.; Cowie, M.R. The role of wearables in heart failure. Curr. Heart Fail. Rep. 2020, 17, 125–132. [Google Scholar] [CrossRef]
- Kao, A.C.; Krause, S.W.; Handa, R.; Karia, D.; Reyes, G.; Bianco, N.R.; Szymkiewicz, S.J. Wearable defibrillator use in heart failure (WIF): Results of a prospective registry. BMC Cardiovasc. Disord. 2012, 12, 123. [Google Scholar] [CrossRef] [Green Version]
- Stehlik, J.; Schmalfuss, C.; Bozkurt, B.; Nativi-Nicolau, J.; Wohlfahrt, P.; Wegerich, S.; Pham, M. Continuous wearable monitoring analytics predict heart failure hospitalization: The LINK-HF multicenter study. Circ. Heart Fail. 2020, 13, e006513. [Google Scholar] [CrossRef] [PubMed]
- Fisher, R.; Smailagic, A.; Sokos, G. Monitoring Health Changes in Congestive Heart Failure Patients Using Wearables and Clinical Data. In Proceedings of the 2017 16th IEEE International Conference on Machine Learning and Applications (ICMLA), Cancun, Mexico, 18–21 December 2017; pp. 1061–1064. [Google Scholar]
- Alharbi, M.; Straiton, N.; Gallagher, R. Harnessing the potential of wearable activity trackers for heart failure self-care. Curr. Heart Fail. Rep. 2017, 14, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Barsheshet, A.; Kutyifa, V.; Vamvouris, T.; Moss, A.J.; Biton, Y.; Chen, L.; Goldenberg, I. Study of the wearable cardioverter defibrillator in advanced heart-failure patients (SWIFT). J. Cardiovasc. Electrophysiol. 2017, 28, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Sajeev, J.K.; Koshy, A.N.; Teh, A.W. Wearable devices for cardiac arrhythmia detection: A new contender? Intern. Med. J. 2019, 49, 570–573. [Google Scholar] [CrossRef] [PubMed]
- Clark, N.; Sandor, E.; Walden, C.; Ahn, I.S.; Lu, Y. A Wearable ECG Monitoring System for Real-Time Arrhythmia Detection. In Proceedings of the 2018 IEEE 61st International Midwest Symposium on Circuits and Systems (MWSCAS), Windsor, ON, Canada, 5–8 August 2018; pp. 787–790. [Google Scholar]
- Sadrawi, M.; Lin, C.H.; Lin, Y.T.; Hsieh, Y.; Kuo, C.C.; Chien, J.C.; Shieh, J.S. Arrhythmia evaluation in wearable ECG devices. Sensors 2017, 17, 2445. [Google Scholar] [CrossRef]
- Cheung, C.C.; Olgin, J.E.; Lee, B.K. Wearable cardioverter-defibrillators: A review of evidence and indications. Trends Cardiovasc. Med. 2021, 31, 196–201. [Google Scholar] [CrossRef]
- Duncker, D.; Veltmann, C. Role of the wearable defibrillator in newly diagnosed heart failure. Curr. Heart Fail. Rep. 2018, 15, 368–375. [Google Scholar] [CrossRef] [Green Version]
- Lee, S.; Squillace, G.; Smeets, C.; Vandecasteele, M.; Grieten, L.; de Francisco, R.; Van Hoof, C. Congestive heart failure patient monitoring using wearable Bio-impedance sensor technology. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 438–441. [Google Scholar]



| Device Type | Device Brand | Device Model | Monitoring Features | Sensors Used | FDA Status/Year/AP (AP: Accuracy Percentage) | Android Compatibility |
|---|---|---|---|---|---|---|
| Smartwatch | Withings | Move ECG [78] | Records ECG readings with or without a phone nearby, as the data can be stored on the watch until the next sync. | ECG with 3 electrodes, altimeter, and accelerometer. | Cleared/2021/98.1% | Yes |
| Fitbit | Versa 2™ [79] | Monitors and records patient physical activity. Analyzes sleep phases, SpO2, variation of skin temperature, respiratory rate, quality of sleep. Records burned calories, menstrual health, stress, moods, guided breathing sessions, HR and resting HR, and cardiovascular fitness. | Three-axis accelerometer, optical HR monitor, infrared, and red-light sensors for SpO2 monitoring, altimeter, vibration motor, NFC, ambient light sensor, Wi-Fi antenna (802.11 b/g/n), microphone, device temperature sensor (detection of variations in skin temperature only available for Premium users). | Cleared/2020/ 50% (for steps counter) | Yes | |
| OMRON | Heart Guide [80] | It is a portable BP monitor. | Accelerometer, PPG HR, oscillometric BP monitor. | Approved/2019/ 94% | Yes | |
| Apple | Watch Series 7 [81] | Reads blood oxygen levels. Monitors HR and PA. Records sleep hours, among others. | Blood oxygen sensors, electric HR sensor, optical HR sensor, S7 SiP Dual Core Chip, digital crown with haptic feedback, GPS, compass, altimeter, horn, and microphone. | ECG approved/2018, oximeter not approved/ 98% (for ECG) | No | |
| Huawei | Band 6 [82] | Monitors HR 24/7, day and night SpO2. Tracks menstrual cycle, sleep, and stress. | Accelerometer sensor, gyroscope sensor, optical heart rate sensor. | Not approved/not applicable/ not available | Yes | |
| Smart Bracelet | MOCACARE | MOCACuff [83] | Monitors HR and BP. Categorizes BP levels with a color-coded indicator system that correspond to the American Heart Association (AHA) categories. | Information not available. | Approved/2017/ 95% (for HR and BP) | Yes |
| Fitbit | Charge 4 [84] | Monitors and records patient physical activity. Analyzes sleep phases, SpO2, variation of skin temperature, respiratory rate, quality of sleep. Records burned calories, menstrual health, stress, moods, guided breathing sessions, HR and resting HR, and cardiovascular fitness. | Three-axis accelerometer, optical HR monitor, GPS + GLONASS, infrared and red-light sensors for SpO2 monitoring, device temperature sensor (detection of variations in skin temperature available in the Fitbit app), vibration motor, NFC (near field communication) chip, altimeter. | Not approved/not applicable/ 50% (for steps counter) | Yes | |
| BIOSTRAP | Armband HRM [85] | Provides biometric information, such as HR and deep sleep through a clinical grade pulse oximeter. | Armband heart rate sensor–optical HR technology that accurately measures HR, burned calories, traveled distance, speed, and pace. | Not approved/not applicable/ not available | Yes | |
| Xiaomi | Mi Smart Band 5 [86] | Monitors HR (full-day HR, manual HR, resting HR, and HR curve) and sleep (seep sleep, light sleep, rapid eye movement (REM), naps). Tracks women’s health (provides recordings and reminders of menstrual cycle and ovulation phases). Monitors stress (breathing exercises, inactivity alerts, step counter, goal setting). | Six-axis sensors: 3-axis low-power accelerometer and 3-axis gyroscope, PPG heart rate sensor, and microphone. | Unknown/ not applicable/ 70% (for sleep tracking) | Yes | |
| Smart Band | HEALBE | GoBe3 [87] | Monitors HR and arterial BP. automatically tracks calorie intake, body hydration, and stress levels. | Bioimpedance sensor, accelerometer, piezoelectric sensor, and galvanic skin response sensor. | Unknown/ not applicable/ not available | Yes |
| ViSi Mobile | The ViSi Mobile System [88] | Monitors HR, pulse rate, respiratory rate, BP, SpO2, body temperature. Detects arrhythmia, falls, and posture. | Information not available. | Approved/2013 /not available | Yes | |
| Wrist-Sensor | Oxitone | Oxitone 1000M [89] | Measures SpO2, skin temperature, pulse rate variability, respiratory rate. Detects falls, steps, and motion. | Skin temperature sensor. | Cleared/2017/97% (for SpO2) | No |
| VinCense | Wireless Health Monitoring System (whms) [90] | It is a wireless health monitoring system for pulse rate, SpO2, respiratory rate, and skin temperature. | Information not available. | Unknown/ not applicable/ 99% (for skin temperature) | Yes | |
| Smart Clothes | Zoll® (Vest) | LifeVest® [91] | Portable automatic defibrillator that stabilizes heart rhythms through an electrical discharge in the chest (in the heart) of the patient. | Garment, electrode belt, and monitor. | Approved/2019/ 92% | No |
| Hexoskin (Smart Shirt) | Astroskin [92] | Performs continuous monitoring (48 h) of BP, blood oxygenation, 3-track ECG, breathing rate, skin temperature and physical activity. | ECG, accelerometer, temperature sensor. | Not approved/not applicable/ not available | Yes | |
| Sleeplay (Smart Sock) | Owlet Smart Sock 3 Baby Monitor [93] | Monitors the baby’s HR and oxygen level during sleep. It is tracked wirelessly via Bluetooth. | Optical HR sensor. | Not approved/ not applicable/ 89% (for oxygen level) | Yes | |
| Spire Health Tag | Spire [94] | Monitors stress levels, sleep, HR, and breathing patterns. It can be placed on clothes; it is hypoallergenic and water resistant. | Capnographer, ECG and accelerometers. | Not approved/ not applicable/ not available | Yes | |
| Vivometrics (Smart Shirt) | The LifeShirt system [95] | Records BP and HR to later send the records to a health professional for medical diagnosis. | Monitor respiration, activity and posture, ECG. | Cleared/2005/ not available | Yes | |
| HealthWatch Technologies (Smart Garment) | Master Caution® [96] | Monitors cardiac ischemia, arrhythmias, respiration, vital signs. Detects falls, inactivity, and skin temperature. Can be used both inside and outside hospital settings. | 3–15 lead ECG monitoring. The garment is the sensor. | Cleared/2015/ not available | Yes | |
| Medtronic (Strap Chest) | Zephyr [97] | Monitors HR. | ECG. | Cleared/2010/ not available | Yes | |
| Patch | iRhythm | Zio® [98] | Records ECG data as the patch is attached to the chest. Records up to 14 days of electrical activity of the heart during daily activities. Once the monitoring is complete, the patch is sent to the treating physician to extract and value the recorded data. The patch can also detect irregular heart rhythms, such as arrhythmia. | ECG. | Cleared/2021/ 99% (for arrhythmia) | Yes |
| Preventice | BodyGuardian® Heart [99] | Small wireless heart activity monitor that adheres to the chest via a disposable strip. The strip can be repositioned as needed thanks to its medical-grade adhesive and electrode gel and should be replaced periodically during the monitoring period. The monitor is returned to the service provider. | Accelerometer, ECG. | Cleared/2012/ not available | No | |
| BioTelemetry | BioTel Heart’s MCOT Patch MCOT: Mobile Cardiac Outpatient Telemetry [100] | Monitors, detects, and transmits abnormal heart rhythms wirelessly. It has been shown to detect atrial fibrillation (≥30 s) with a sensitivity and positive prediction of 100%. | Accelerometer, ECG. | Cleared/2016/ 100% (for atrial fibrillation) | No | |
| Wellysis | S-Patch Cardio [101] | Records ECG data to assess supraventricular and ventricular arrhythmias. | Accelerometer, ECG. | Unknown/ not applicable/ 95% | Yes | |
| VitalConnect | Vital Patch [102] | Monitors cardiac function. Sends patient data to a secure cloud for real-time monitoring of different cardiac arrhythmias. | Accelerometer, ECG, thermistor. | Cleared/2017/ 59.2% | Yes | |
| Phone Attachment | AliveCor® | KardiaMobile [103] | It can associate cardiac and respiratory symptoms (atrial fibrillation, sinus bradycardia, sinus tachycardia, and arrhythmia) through its ECG patterns. | Mobile electrode with a built-in ECG. | Cleared/2014/ 94% (for arrhythmia) | Yes |
| PAI (personal activity intelligence) | PAI Health [104] | The PAI software records the patient HR to optimally manage their health. | Information not available. | Unknown/ not applicable/ not available | No | |
| Finger Ring | Oura | Oura Ring [105] | Based on body temperature, HR, and HR variability (HRV), it records relevant data on monthly menstrual periods, physical activity, and sleep periods. | Body temperature sensor, optical, infrared sensors, and a 3D accelerometer and gyroscope. | Not approved/ not applicable/ 99.9% (for HR) and 98.4% (for HRV) | Yes |
| Fingertip | iHealth | Pulse Oximeter iHealth Fingertip [106] | Offers an affordable, reliable, and accurate way to check pulse and SpO2 levels. | Optical sensor: red light (wavelength is 660 nm, 6.65 mW), infrared (wavelength is 880 nm, 6.75 mW). | Cleared/2013/ 99% | Yes |
| Smart Earphones | FreeWavz | FreeWavz-Blue [107] | Wireless smart earphones with built-in sensors for HR and fitness monitoring. | Three-axis accelerometer, two electret condenser microphones on each side, pulse oximeter. | Unknown/ not applicable/ not available | No |
| Tensioning Band on the Arm. | iHealth | Tensiometer Bras iHealth Track (KN-550BT) [108] | Monitors Pulse and BP. | BP sensor. | Cleared/2016/ not available | Yes |
| Biomedical Variables | FDA Devices | Non-FDA Devices | Total |
|---|---|---|---|
| HR | 9 | 9 | 18 |
| SpO2 | 7 | 8 | 15 |
| ECG | 9 | 2 | 11 |
| Sleep | 3 | 7 | 10 |
| Physical Activity | 2 | 5 | 7 |
| Skin Temperature | 5 | 2 | 7 |
| Menstrual Health | 1 | 4 | 5 |
| Stress | 1 | 4 | 5 |
| Respiratory Rate | 0 | 4 | 4 |
| Burned Calories | 2 | 1 | 3 |
| Pulse Rate | 2 | 1 | 3 |
| HRV | 2 | 0 | 2 |
| Portable Cardioverter-Defibrillator | 1 | 0 | 1 |
| CVD Type | Device Type | Research Description | Sensors or Technology Used | Real-Time Monitoring |
|---|---|---|---|---|
| Atrial fibrillation | Massachusetts Institute of Technology (MIT)–Beth Israel Hospital (BIH) Atrial Fibrillation database and the MIT–BIH Arrhythmia database were used as training data and verified the algorithm performance. (2020) | Evaluates an inexpensive heart rate monitor (i.e., a chest patch) with a machine learning algorithm (MLA) capable of accurately detecting AF. The monitor can also transmit ECG data that could be used to confirm AF [109]. | Detection algorithm using a decorrelated Lorenz plot. | No |
| Ring and pulse oximeter (2020) | Evaluates the performance of a wearable ring-type device for detecting AF using deep learning analysis of PPG signals obtained from the patient [110]. | PPG and deep learning. | Yes | |
| Smartwatch (2019) | Evaluates the ability of a commercial smartwatch, the AliveCor KardiaBand (KB), to detect atrial fibrillation (AF) or sinus rhythm in comparison with the 12-track electrocardiogram (ECG), obtaining results that demonstrate a moderate diagnostic accuracy [111]. | ECG. | Yes | |
| Smart watchband (2019) | Evaluates the accuracy of PPG technology in heart rate monitoring for diagnosing AF in comparison with conventional electrocardiography [112]. | PPG. | Yes | |
| T-shirt (2019) | Discusses the development of a portable device for community screening of asymptomatic AF using a wireless ECG worn on a T-shirt [113]. | ECG. | Yes | |
| Smartwatch (2019) | Discusses evidence on the performance smartwatches in terms of AF detection, concluding that it is still premature to consider them as a first option; however, the future certainly looks encouraging [114]. | PPG and ECG. | Yes | |
| Smartwatch (2019) | Compares the accuracy between recordings from an insertable cardiac monitor (ICM; Reveal LINQ) and a watch with AF detection (AFSW; Apple Watch with Kardia Band), concluding that an AFSW is sensitive in detecting AF, is an inexpensive option, and is not invasive therapy in the long-term follow-up and treatment of AF [115]. | Smart Rhythm 2.0, a convolutional neural network. | Yes | |
| Algorithm (2019) | Discusses the development of an algorithm that accurately detects AF using the PPG technique when the patient performs daily activities [116]. | PPG. | Yes | |
| Chest electrodes (2019) | Discusses the development of a high-precision portable ECG device optimized for AF detection [117]. | Prototype ECG. | Yes | |
| Wrist-worn device (2018) | Proposes an AF detection algorithm using the PPG technique implemented in a self-designed wrist-worn device [118]. | PPG. | Yes | |
| Smartwatch (2018) | Evaluates the accuracy of the AliveCor KardiaBand (KB) with respect to a 12-lead ECG in detecting AF from sinus arrhythmia [119]. | ECG. | Yes | |
| Patch (2018) | Evaluates a patch with an integrated ECG for AF detection, concluding that individuals monitored by this means had an opportunity to receive care earlier if AF was detected, if compared with unmonitored controls [120]. | ECG. | Yes | |
| Wrist-worn prototype fitness tracker device (2018) | Evaluates a convolutional recurrent neural network with applications in PPG-based AF diagnosis [121]. | Convolutional–recurrent neural network architecture and PPG. | Yes | |
| Smart watchband (2018) | Reviews available portable technologies to determine their potential advantages and disadvantages in AF detection [122]. | PPG and MLAs. | Yes | |
| Wrist-worn Device (2017) | Discusses the development of a deep neural network to accurately classify AF using the PPG technique on the patient’s wrist [123]. | PPG, accelerometer, and single-lead ECG. | Yes | |
| Heart failure | Smart fitness trackers (2021) | Analyzes the physical activity of 70 patients with stable symptoms of heart failure through actigraphy [124]. | Pedometer and accelerometer. | Yes |
| Smart fitness trackers (2021) | Analyzes the current use of actigraphy in randomized controlled trials (RCTs) of patients with heart failure [125]. | Pedometer and accelerometer. | Yes | |
| Wristband (2020) | Examines wristband technologies that can facilitate more accurate bedside testing, due to the difficulty of heart failure diagnosis by physical examination alone. The research concludes that wristbands can be used as a complementary tool in the bedside diagnostic evaluation and not as the only option [126]. | PPG, accelerometer, and ECG. | Yes | |
| Smart watchband and chest patch-vest (2020) | Analyzes the use of sensors in wearable devices that measure biomedical variable signals (noninvasively) for use in patients suffering from heart failure [127]. | PPG, accelerometer, and ECG. | Yes | |
| Chest vest (2020) | Evaluates the efficacy of early defibrillation with a WCD on the incidence of sudden cardiac death [128]. | Cardioverter defibrillator. | Yes | |
| Patch (2020) | Evaluates remote and noninvasive monitoring and predicts rehospitalization for heart failure [129]. | ECG and 3-axis accelerometer. | Yes | |
| Smart watchband and chest patch (2019) | Analyzes the applications and future of wearable devices in HF detection [48]. | PPG, accelerometer, and ECG. | Yes | |
| Smartwatches–fitness trackers (2018) | Reviews current developments and challenges in portable monitoring technologies based on the PPG technique [37]. | PPG. | Yes | |
| Smart watchband and the Multiparameter Intelligent Monitoring in Intensive Care II (MIMIC II) dataset (2017) | Reviews the performance (with respect to cost and diagnostic accuracy) of current health monitoring systems targeting patients with congestive heart failure (CHF) [130]. | PPG and ECG. | Yes | |
| Smart watchband (2017) | Evaluates PA trackers to promote self-care in PA performed by patients with HF [131]. | Pedometer and accelerometer. | Yes | |
| Vest (2017) | Proposes a safe WCD management strategy to avoid implantable cardioverter defibrillator (ICD) implantation in high-risk patients with advanced heart failure [132]. | Cardioverter defibrillator. | Yes | |
| Arrhythmia | Smart watchband (2019) | Discusses the feasibility of a regulatory framework to standardize and incorporate into medical practice the data generated by smart device management platforms [133]. | PPG, accelerometer, and single-lead ECG. | Yes |
| Electronic platform (2018) | Discusses the development of a portable medical system integrating a three-lead ECG sensor for real-time arrhythmia detection [134]. | Texas Instruments TMS320C5515 and Raspberry Pi 3 Model B. | Yes | |
| Four databases from PhysioNet (2017) | Evaluates the precision of portable ECG devices for arrhythmia detection, achieving good results when compared to other previous studies [135]. | ECG. | Yes | |
| Ventricular fibrillation and sudden cardiac death (SCD) | Vest (2021) | Summarizes the literature on wearable cardioverter defibrillators (WCDs) [136]. | Cardioverter-defibrillator. | Not applicable |
| Vest (2018) | Reviews current data on WCD in newly diagnosed cardiomyopathy [137]. | Cardioverter defibrillator. | Not applicable | |
| Congestive heart failure (CHF) | Electrodes (2015) | The researchers discuss a clinical trial where they propose a technique to monitor the fluid status of patients with congestive heart failure in the hospital [138]. | ECG, 3-axis accelerometer, and bioimpedance Z (BioZ). | Yes |
| CVD Type | Real-Time Monitoring | Distribution |
|---|---|---|
| Atrial fibrillation | Yes | 95% |
| No | 5% | |
| Heart failure | Yes | 92% |
| No | 8% |
| CVD Type | Sensor/Technology Used | No. Used | % |
|---|---|---|---|
| Atrial fibrillation | ECG | 10 | 38% |
| PPG | 9 | 35% | |
| Algorithm | 5 | 19% | |
| Accelerometer | 2 | 8% | |
| Heart failure | Accelerometer | 8 | 30% |
| ECG | 6 | 22% | |
| PPG | 5 | 19% | |
| Cardioverter defibrillator | 4 | 15% | |
| Pedometer | 3 | 11% | |
| Bioimpedance Z | 1 | 4% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prieto-Avalos, G.; Cruz-Ramos, N.A.; Alor-Hernández, G.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L.; Guarneros-Nolasco, L.R. Wearable Devices for Physical Monitoring of Heart: A Review. Biosensors 2022, 12, 292. https://doi.org/10.3390/bios12050292
Prieto-Avalos G, Cruz-Ramos NA, Alor-Hernández G, Sánchez-Cervantes JL, Rodríguez-Mazahua L, Guarneros-Nolasco LR. Wearable Devices for Physical Monitoring of Heart: A Review. Biosensors. 2022; 12(5):292. https://doi.org/10.3390/bios12050292
Chicago/Turabian StylePrieto-Avalos, Guillermo, Nancy Aracely Cruz-Ramos, Giner Alor-Hernández, José Luis Sánchez-Cervantes, Lisbeth Rodríguez-Mazahua, and Luis Rolando Guarneros-Nolasco. 2022. "Wearable Devices for Physical Monitoring of Heart: A Review" Biosensors 12, no. 5: 292. https://doi.org/10.3390/bios12050292
APA StylePrieto-Avalos, G., Cruz-Ramos, N. A., Alor-Hernández, G., Sánchez-Cervantes, J. L., Rodríguez-Mazahua, L., & Guarneros-Nolasco, L. R. (2022). Wearable Devices for Physical Monitoring of Heart: A Review. Biosensors, 12(5), 292. https://doi.org/10.3390/bios12050292









