A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy
Abstract
1. Introduction
2. Materials and Methods
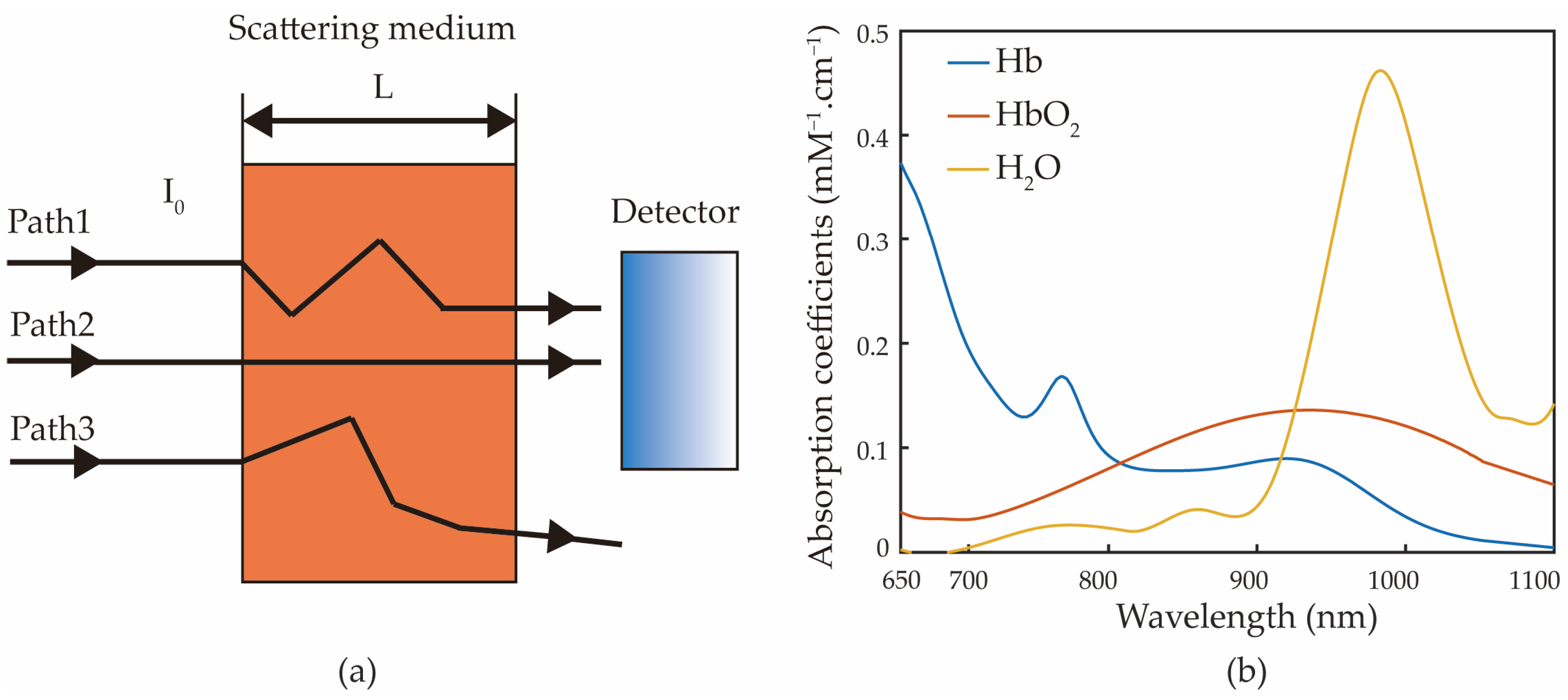
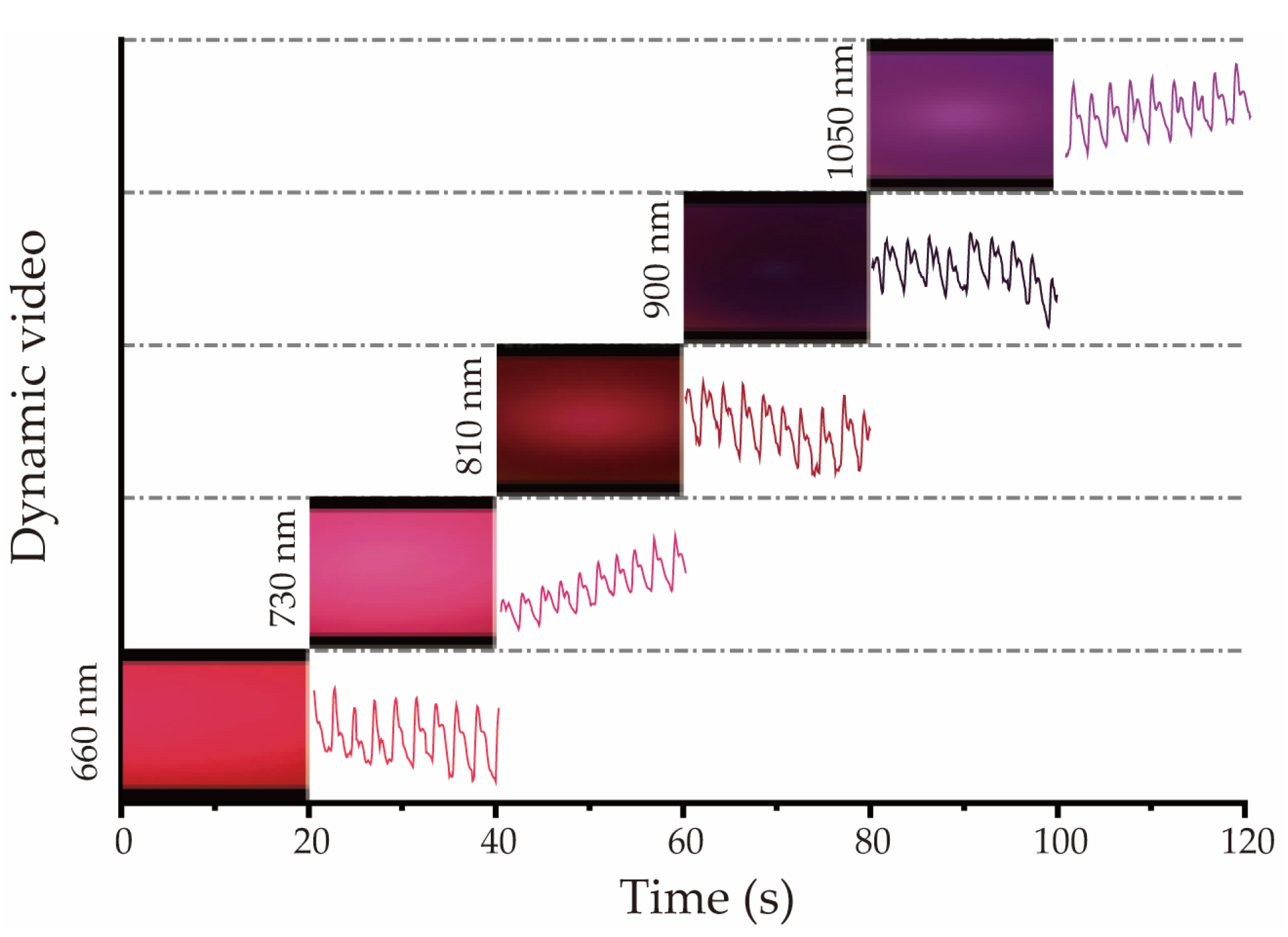
2.1. Modified Beer–Lambert Law and Multiwavelength Selection
2.2. Smartphone Measurement Device
2.3. Data Collection
2.4. Color Space Transformation
2.5. Data Analysis
3. Results
3.1. Comparison of RGB and L*a*b* Color Spaces Results
3.2. Prediction Results of Hemoglobin Concentration
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kamruzzaman, M.; Rabbani, M.G.; Saw, A.; Sayem, M.A.; Hossain, M.G. Differentials in the prevalence of anemia among non-pregnant, ever-married women in Bangladesh: Multilevel logistic regression analysis of data from the 2011 Bangladesh Demographic and Health Survey. BMC Womens Health 2015, 15, 54. [Google Scholar] [CrossRef] [PubMed]
- Karakochuk, C.D.; Hess, S.Y.; Moorthy, D.; Namaste, S.; Parker, M.E.; Rappaport, A.I.; Wegmuller, R.; Dary, O.; Group, H.E.M.W. Measurement and interpretation of hemoglobin concentration in clinical and field settings: A narrative review. Ann. N. Y. Acad. Sci. 2019, 1450, 126–146. [Google Scholar] [CrossRef] [PubMed]
- Causey, M.W.; Miller, S.; Foster, A.; Beekley, A.; Zenger, D.; Martin, M. Validation of noninvasive hemoglobin measurements using the Masimo Radical-7 SpHb Station. Am. J. Surg. 2011, 201, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Kumar, D.; Simmons, S. Systematic review and meta-analysis of method comparison studies of Masimo pulse co-oximeters (Radical-7™ or Pronto-7™) and HemoCue® absorption spectrometers (B-Hemoglobin or 201+) with laboratory haemoglobin estimation. Anaesth. Intensive Care 2015, 43, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.H.; Lee, J.H.; Song, H.G.; Byon, H.J.; Kim, H.S.; Kim, J.T. The accuracy of noninvasive hemoglobin monitoring using the radical-7 pulse CO-Oximeter in children undergoing neurosurgery. Anesth. Analg. 2012, 115, 1302–1307. [Google Scholar] [CrossRef] [PubMed]
- Feiner, J.R.; Bickler, P.E.; Mannheimer, P.D. Accuracy of methemoglobin detection by pulse CO-oximetry during hypoxia. Anesth. Analg. 2010, 111, 143–148. [Google Scholar] [CrossRef]
- Riess, M.L.; Pagel, P.S. Noninvasively Measured Hemoglobin Concentration Reflects Arterial Hemoglobin Concentration Before but Not after Cardiopulmonary Bypass in Patients Undergoing Coronary Artery or Valve Surgery. J. Cardiothorac. Vasc. Anesth. 2016, 30, 1167–1171. [Google Scholar] [CrossRef]
- Song, J.; Pandian, V.; Mauk, M.G.; Bau, H.H.; Cherry, S.; Tisi, L.C.; Liu, C. Smartphone-Based Mobile Detection Platform for Molecular Diagnostics and Spatiotemporal Disease Mapping. Anal. Chem. 2018, 90, 4823–4831. [Google Scholar] [CrossRef]
- Hussain, S.; Chen, X.; Wang, C.; Hao, Y.; Tian, X.; He, Y.; Li, J.; Shahid, M.; Iyer, P.K.; Gao, R. Aggregation and Binding-Directed FRET Modulation of Conjugated Polymer Materials for Selective and Point-of-Care Monitoring of Serum Albumins. Anal. Chem. 2022, 94, 10685–10694. [Google Scholar] [CrossRef]
- Muthuraj, B.; Hussain, S.; Iyer, P.K. A rapid and sensitive detection of ferritin at a nanomolar level and disruption of amyloid β fibrils using fluorescent conjugated polymer. Polym. Chem. 2013, 4, 5096–5107. [Google Scholar] [CrossRef]
- Pal, A.; Sinha, A.; Dutta Choudhury, A.; Chattopadyay, T.; Visvanathan, A. A robust heart rate detection using smart-phone video. In Proceedings of the 3rd ACM MobiHoc Workshop on Pervasive Wireless Healthcare, Bangalore, India, 29 July 2013; ACM: New York, NY, USA, 2013; pp. 43–48. [Google Scholar]
- Pal, A.; Visvanathan, A.; Choudhury, A.D.; Sinha, A. Improved heart rate detection using smart phone. In Proceedings of the 29th Annual ACM Symposium on Applied Computing, Gyeongju, Korea, 24–28 March 2014; ACM: New York, NY, USA, 2014; pp. 8–13. [Google Scholar]
- Gaoan, G.; Zhenmin, Z. Heart rate measurement via smart phone acceleration sensor. In Proceedings of the 2014 International Conference on Smart Computing, Hong Kong, China, 3–5 November 2014; pp. 295–300. [Google Scholar]
- Bui, N.; Nguyen, A.; Nguyen, P.; Truong, H.; Ashok, A.; Dinh, T.; Deterding, R.; Vu, T. PhO2. In Proceedings of the 15th ACM Conference on Embedded Network Sensor Systems, Delft, The Netherlands, 6–8 November 2017; ACM: New York, NY, USA, 2017; pp. 1–14. [Google Scholar]
- Fang, D.; Hu, J.; Wei, X.; Shao, H.; Luo, Y. A Smart Phone Healthcare Monitoring System for Oxygen Saturation and Heart Rate. In Proceedings of the 2014 International Conference on Cyber-Enabled Distributed Computing and Knowledge Discovery, Shanghai, China, 13–15 October 2014; pp. 245–247. [Google Scholar]
- Nemcova, A.; Jordanova, I.; Varecka, M.; Smisek, R.; Marsanova, L.; Smital, L.; Vitek, M. Monitoring of heart rate, blood oxygen saturation, and blood pressure using a smartphone. Biomed. Signal Process. Control 2020, 59, 101928. [Google Scholar] [CrossRef]
- Charlton, P.H.; Birrenkott, D.A.; Bonnici, T.; Pimentel, M.A.F.; Johnson, A.E.W.; Alastruey, J.; Tarassenko, L.; Watkinson, P.J.; Beale, R.; Clifton, D.A. Breathing Rate Estimation from the Electrocardiogram and Photoplethysmogram: A Review. IEEE Rev. Biomed. Eng. 2018, 11, 2–20. [Google Scholar] [CrossRef]
- Karlen, W.; Garde, A.; Myers, D.; Scheffer, C.; Ansermino, J.M.; Dumont, G.A. Estimation of respiratory rate from photoplethysmographic imaging videos compared to pulse oximetry. IEEE J. Biomed. Health Inform. 2015, 19, 1331–1338. [Google Scholar] [CrossRef]
- Batsis, J.A.; Boateng, G.G.; Seo, L.M.; Petersen, C.L.; Fortuna, K.L.; Wechsler, E.V.; Peterson, R.J.; Cook, S.B.; Pidgeon, D.; Dokko, R.S.; et al. Development and Usability Assessment of a Connected Resistance Exercise Band Application for Strength-Monitoring. World Acad. Sci. Eng. Technol. 2019, 13, 340–348. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.J.; Li, W.; Hawkins, D.; Gernsheimer, T.; Norby-Slycord, C.; Patel, S.N. HemaApp. In Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing, Heidelberg, Germany, 12–16 September 2016; ACM: New York, NY, USA, 2016; pp. 593–604. [Google Scholar]
- Ghatpande, N.S.; Apte, P.P.; Joshi, B.N.; Naik, S.S.; Bodas, D.; Sande, V.; Uttarwar, P.; Kulkarni, P.P. Development of a novel smartphone-based application for accurate and sensitive on-field hemoglobin measurement. RSC Adv. 2016, 6, 104067–104072. [Google Scholar] [CrossRef]
- Swinehart, D.F. The beer-lambert law. J. Chem. Educ. 1962, 39, 333. [Google Scholar] [CrossRef]
- Maikala, R.V. Modified Beer’s Law—Historical perspectives and relevance in near-infrared monitoring of optical properties of human tissue. Int. J. Ind. Ergon. 2010, 40, 125–134. [Google Scholar] [CrossRef]
- Pellicer, A.; Bravo Mdel, C. Near-infrared spectroscopy: A methodology-focused review. Semin. Fetal Neonatal Med. 2011, 16, 42–49. [Google Scholar] [CrossRef]
- Duncan, A.; Meek, J.H.; Clemence, M.; Elwell, C.E.; Tyszczuk, L.; Cope, M.; Delpy, D. Optical pathlength measurements on adult head, calf and forearm and the head of the newborn infant using phase resolved optical spectroscopy. Phys. Med. Biol. 1995, 40, 295. [Google Scholar] [CrossRef]
- Zee, P.; Cope, M.; Arridge, S.; Essenpreis, M.; Potter, L.; Edwards, A.; Wyatt, J.; McCormick, D.; Roth, S.; Reynolds, E. Experimentally measured optical pathlengths for the adult head, calf and forearm and the head of the newborn infant as a function of inter optode spacing. In Oxygen Transport to Tissue XIII; Springer: Berlin/Heidelberg, Germany, 1992; pp. 143–153. [Google Scholar]
- Wray, S.; Cope, M.; Delpy, D.T.; Wyatt, J.S.; Reynolds, E.O.R. Characterization of the near infrared absorption spectra of cytochrome aa3 and haemoglobin for the non-invasive monitoring of cerebral oxygenation. Biochim. Biophys. Acta (BBA)-Bioenerg. 1988, 933, 184–192. [Google Scholar] [CrossRef]
- Matcher, S.; Elwell, C.; Cooper, C.; Cope, M.; Delpy, D. Performance comparison of several published tissue near-infrared spectroscopy algorithms. Anal. Biochem. 1995, 227, 54–68. [Google Scholar] [CrossRef] [PubMed]
- Timm, U.; Leen, G.; Lewis, E.; McGrath, D.; Kraitl, J.; Ewald, H. Non-invasive optical real-time measurement of total hemoglobin content. Procedia Eng. 2010, 5, 488–491. [Google Scholar] [CrossRef][Green Version]
- Jeon, K.J.; Kim, S.J.; Park, K.K.; Kim, J.W.; Yoon, G. Noninvasive total hemoglobin measurement. J. Biomed. Opt. 2002, 7, 45–50. [Google Scholar] [CrossRef]
- Aziz, M.H.; Hasan, M.K.; Mahmood, A.; Love, R.R.; Ahamed, S.I. Automated Cardiac Pulse Cycle Analysis from Photoplethysmogram (PPG) Signals Generated from Fingertip Videos Captured Using a Smartphone to Measure Blood Hemoglobin Levels. IEEE J. Biomed. Health Inform. 2021, 25, 1385–1396. [Google Scholar] [CrossRef]
- Yi, X.; Li, G.; Lin, L. Noninvasive hemoglobin measurement using dynamic spectrum. Rev. Sci. Instrum. 2017, 88, 083109. [Google Scholar] [CrossRef] [PubMed]
- Kuru, K. Optimization and enhancement of H&E stained microscopical images by applying bilinear interpolation method on lab color mode. Theor. Biol. Med. Model. 2014, 11, 9. [Google Scholar] [CrossRef]
- Stamatas, G.N.; Zmudzka, B.Z.; Kollias, N.; Beer, J.Z. Non-invasive measurements of skin pigmentation in situ. Pigment Cell Res. 2004, 17, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.R.; Mahadevappa, M.; Goswami, D. Low cost point of care estimation of Hemoglobin levels. In Proceedings of the 2014 International Conference on Medical Imaging, m-Health and Emerging Communication Systems (MedCom), Greater Noida, India, 7–8 November 2014; pp. 216–221. [Google Scholar]
- Biswas, S.K.; Chatterjee, S.; Bandyopadhyay, S.; Kar, S.; Som, N.K.; Saha, S.; Chakraborty, S. Smartphone-Enabled Paper-Based Hemoglobin Sensor for Extreme Point-of-Care Diagnostics. ACS Sens. 2021, 6, 1077–1085. [Google Scholar] [CrossRef]
- Lee, J.; Song, J.; Choi, J.H.; Kim, S.; Kim, U.; Nguyen, V.T.; Lee, J.S.; Joo, C. A Portable Smartphone-linked Device for Direct, Rapid and Chemical-Free Hemoglobin Assay. Sci. Rep. 2020, 10, 8606. [Google Scholar] [CrossRef]





| Model | Color Space | R2 | Adjusted R2 | RMSE | MAPE | Durbin–Watson Test |
| a (L*a*b) | 0.91 | 0.88 | 9.04 | 0.068 | 1.77 | |
| R (RGB) | 0.87 | 0.83 | 10.70 | 0.091 | 2.41 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, Z.; Zhou, Y.; Zhai, H.; Wang, Q.; He, H. A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy. Biosensors 2022, 12, 781. https://doi.org/10.3390/bios12100781
Fan Z, Zhou Y, Zhai H, Wang Q, He H. A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy. Biosensors. 2022; 12(10):781. https://doi.org/10.3390/bios12100781
Chicago/Turabian StyleFan, Zhipeng, Yong Zhou, Haoyu Zhai, Qi Wang, and Honghui He. 2022. "A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy" Biosensors 12, no. 10: 781. https://doi.org/10.3390/bios12100781
APA StyleFan, Z., Zhou, Y., Zhai, H., Wang, Q., & He, H. (2022). A Smartphone-Based Biosensor for Non-Invasive Monitoring of Total Hemoglobin Concentration in Humans with High Accuracy. Biosensors, 12(10), 781. https://doi.org/10.3390/bios12100781





