An Optimized Method for Evaluating the Potential Gd-Nanoparticle Dose Enhancement Produced by Electronic Brachytherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. EBT3 Radiochromic Film Processing and Reading
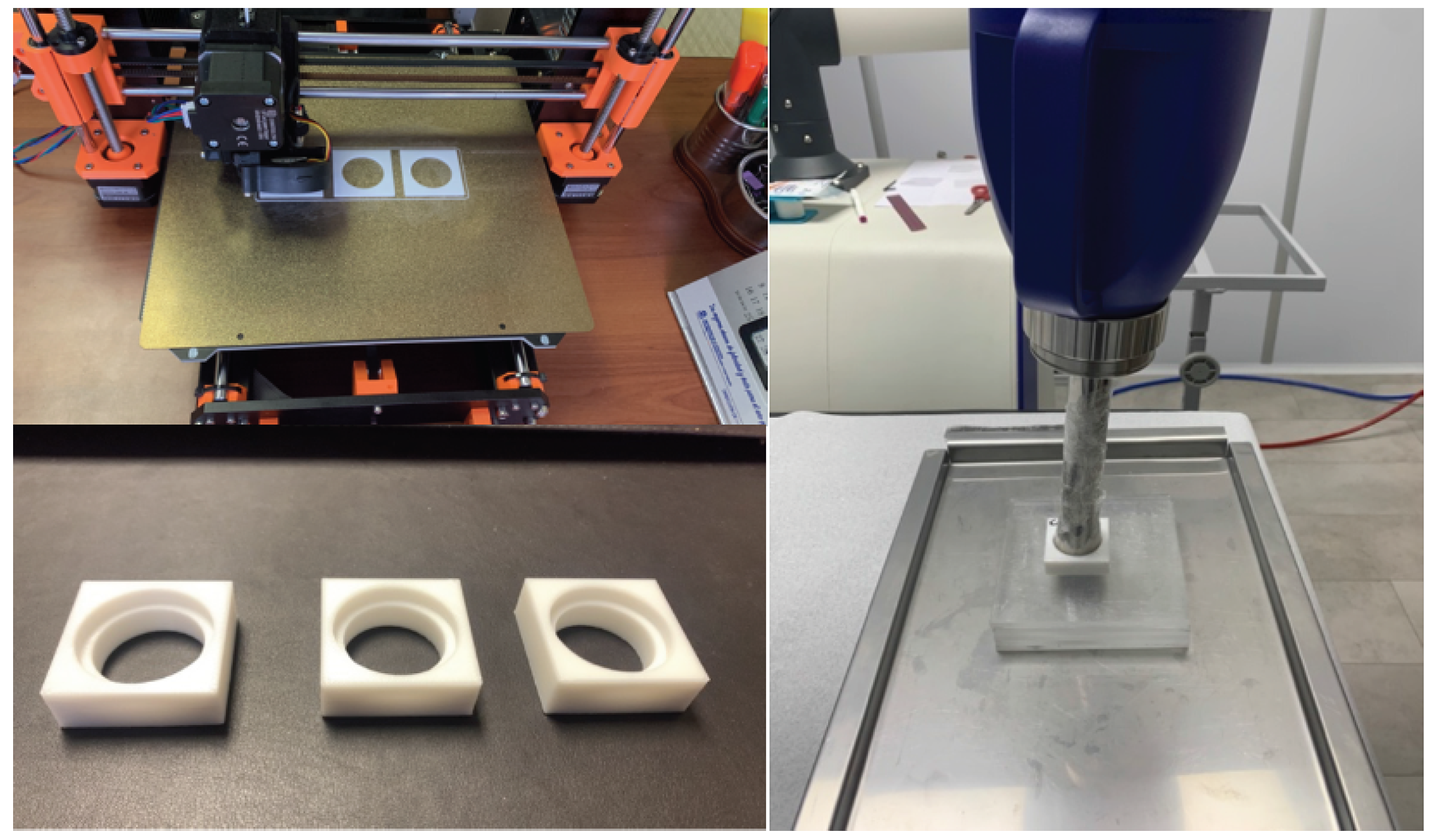
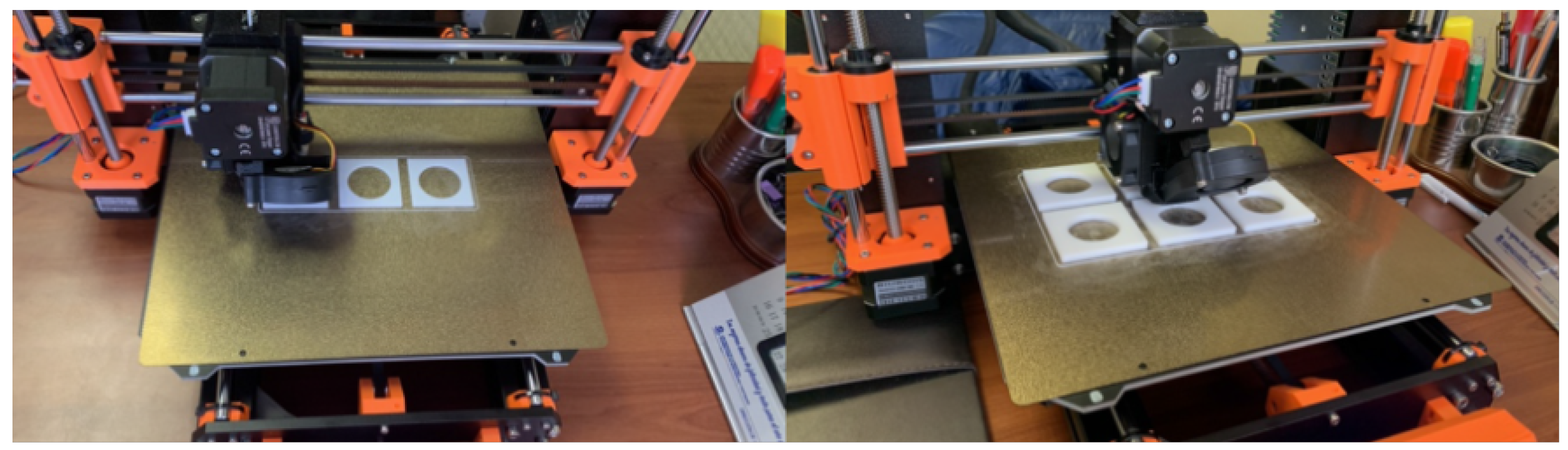
2.2. PMMA Phantom Manufacturing and Setup
2.3. Irradiation System
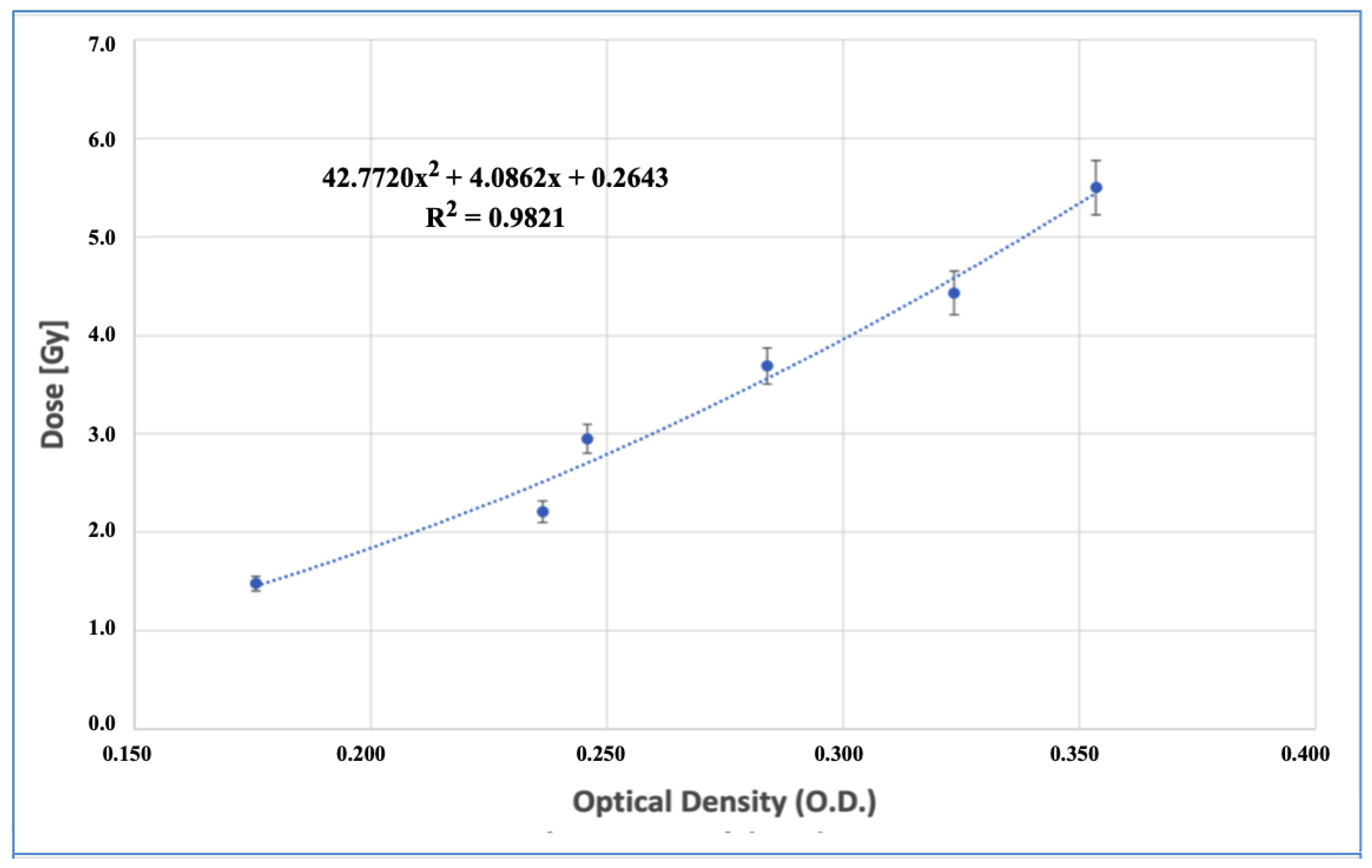
2.4. EBT3 Film Calibration Curve
2.5. Dose Enhancement Evaluation
3. Results
3.1. PMMA Phantom Manufacturing and Evaluation
3.2. Dose Enhancement Measurements
3.2.1. Calibration Curve
3.2.2. Dose Enhancement Evaluation as a Function of Beam Quality
3.2.3. Dose Enhancement Evaluation as a Function of Gd Concentration for the Most Energetic Clinical Beam Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Penninckx, S.; Heuskin, A.-C.; Michiels, C.; Lucas, S. Gold Nanoparticles as a Potent Radiosensitizer: A Transdisciplinary Approach from Physics to Patient. Cancers 2020, 12, 2021. [Google Scholar] [CrossRef] [PubMed]
- Siddique, S.; Chow, J.C.L. Application of Nanomaterials in Biomedical Imaging and Cancer Therapy. Nanomaterials 2020, 10, 1700. [Google Scholar] [CrossRef] [PubMed]
- Kakade, N.R.; Kumar, R.; Sharma, S.D.; Datta, D. Equivalence of silver and gold nanoparticles for dose enhancement in nanoparticle-aided brachytherapy. Biomed. Phys. Eng. Express 2019, 5, 055015. [Google Scholar] [CrossRef]
- Santibáñez, M.; Saavedra, R.; Vedelago, J.; Malano, F.; Valente, M. Optimized EDXRF system for simultaneous detection of gold and silver nanoparticles in tumor phantom. Rad. Phys. Chem. 2019, 165, 108415. [Google Scholar] [CrossRef]
- Rasouli, F.S.; Masoudi, S.F. Monte Carlo investigation of the effect of gold nanoparticles’ distribution on cellular dose enhancement. Rad. Phys. Chem. 2019, 158, 6–12. [Google Scholar] [CrossRef]
- Hainfeld, J.F.; Smilowitz, H.M.; O’Connor, M.J.; Dilmanian, F.A.; Slatkin, D.N. Gold nanoparticle imaging and radiotherapy of brain tumors in mice. Nanomedicine 2013, 8, 1601–1609. [Google Scholar] [CrossRef]
- Ngwa, W.; Kumar, R.; Sridhar, S.; Korideck, H.; Zygmanski, P.; Cormack, R.A.; Berbeco, R.; Makrigiorgos, G.M. Targeted radiotherapy with gold nanoparticles: Current status and future perspectives. Nanomedicine 2014, 9, 1063–1082. [Google Scholar] [CrossRef]
- Shahhoseini, E.; Ramachandran, P.; Patterson, W.R.; Geso, M. Determination of dose enhancement caused by AuNPs with Xoft® Axxent® Electronic (eBx™) and conventional brachytherapy: In vitro study. Int. J. Nanomed. 2018, 13, 5733–5741. [Google Scholar] [CrossRef]
- Mesbahi, A.; Rajabpour, S.; Smilowitz, H.M.; Hainfeld, J.F. Accelerated brachytherapy with the Xoft electronic source used in association with iodine, gold, bismuth, gadolinium, and hafnium nano-radioenhancers. Brachytherapy 2022, 21, 968–978. [Google Scholar] [CrossRef]
- Cifter, G.; Chin, J.; Cifter, F.; Altundal, Y.; Sinha, N.; Sajo, E.; Ngwa, W. Targeted radiotherapy enhancement during electronic brachytherapy of accelerated partial breast irradiation (APBI) using controlled release of gold nanoparticles. Phys. Med. 2015, 31, 1070–1074. [Google Scholar] [CrossRef]
- Alyani Nezhad, Z.; Geraily, G.; Hataminia, F.; Parwaie, W.; Ghanbari, H.; Gholami, S. Bismuth oxide nanoparticles as agents of radiation dose enhancement in intraoperative radiotherapy. Med. Phys. 2021, 48, 1417–1426. [Google Scholar] [CrossRef] [PubMed]
- Baghani, H.R.; Nasrollahi, S. Efficacy of various nanoparticle types in dose enhancement during low energy X-ray IORT: A Monte Carlo simulation study. Rad. Phys. Chem. 2021, 183, 109432. [Google Scholar] [CrossRef]
- Moradi, F.; Sani, S.A.; Khandaker, M.U.; Sulieman, A.; Bradley, D.A. Dosimetric evaluation of gold nanoparticle aided intraoperative radiotherapy with the Intrabeam system using Monte Carlo simulations. Rad. Phys. Chem. 2021, 178, 108864. [Google Scholar] [CrossRef]
- Abd Rahman, W.N.W. Gold Nanoparticles: Novel Radiobiological Dose Enhancement Studies for Radiation Therapy, Synchrotron Based Microbeam and Stereotactic Radiotherapy. Ph.D. Thesis, RMIT University, Melbourne, VIC, Australia, 2010. [Google Scholar]
- Kim, S.R.; Kim, E.H. Gold nanoparticles as dose-enhancement agent for kilovoltage X-ray therapy of melanoma. Int. J. Radiat. Biol. 2017, 93, 517–526. [Google Scholar] [CrossRef]
- Garcia-Martinez, T.; Chan, J.P.; Perez-Calatayud, J.; Ballester, F. Dosimetric characteristics of a new unit for electronic skin brachytherapy. J. Contemp. Brachyther. 2014, 6, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Dickler, A.; Dowlatshahi, K. Xoft Axxent electronic brachytherapy™. Expert Rev. Med. Devices 2009, 6, 27–31. [Google Scholar] [CrossRef] [PubMed]
- Bromma, K.; Rieck, K.; Kulkarni, J.; O’Sullivan, C.; Sung, W.; Cullis, P.; Schuemann, J.; Chithrani, D.B. Use of a lipid nanoparticle system as a Trojan horse in delivery of gold nanoparticles to human breast cancer cells for improved outcomes in radiation therapy. Cancer Nanotechnol. 2019, 10, 1–17. [Google Scholar] [CrossRef]
- Yang, C.; Bromma, K.; Di Ciano-Oliveira, C.; Zafarana, G.; Van Prooijen, M.; Chithrani, D.B. Gold nanoparticle mediated combined cancer therapy. Cancer Nanotechnol. 2018, 9, 1–14. [Google Scholar] [CrossRef]
- Albertini, B.; Mathieu, V.; Iraci, N.; Van Woensel, M.; Schoubben, A.; Donnadio, A.; Greco, S.M.; Ricci, M.; Temperini, A.; Wauthoz, N.; et al. Tumor targeting by peptide-decorated gold nanoparticles. Mol. Pharm. 2019, 16, 2430–2444. [Google Scholar] [CrossRef]
- Chen, G.; Xie, Y.; Peltier, R.; Lei, H.; Wang, P.; Chen, J.; Hu, Y.; Wang, F.; Yao, X.; Sun, H. Peptide-decorated gold nanoparticles as functional nano-capping agent of mesoporous silica container for targeting drug delivery. ACS Appl. Mater. Interfaces 2016, 8, 11204–11209. [Google Scholar] [CrossRef]
- Grüner, F.; Blumendorf, F.; Schmutzler, O.; Staufer, T.; Bradbury, M.; Wiesner, U.; Rosentreter, T.; Loers, G.; Lutz, D.; Hoeschen, C.; et al. Localising functionalised gold-nanoparticles in murine spinal cords by X-ray fluorescence imaging and background-reduction through spatial filtering for human-sized objects. Sci. Rep. 2019, 8, 16561. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Peng, Q. Protein-gold nanoparticle interactions and their possible impact on biomedical applications. Acta Biomater. 2017, 55, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Wangoo, N.; Bhasin, K.K.; Mehta, S.K.; Suri, C.R. Synthesis and capping of water-dispersed gold nanoparticles by an amino acid: Bioconjugation and binding studies. J. Colloid Interface Sci. 2008, 323, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Reuveni, T.; Motiei, M.; Romman, Z.; Popovtzer, A.; Popovtzer, R. Targeted gold nanoparticles enable molecular CT imaging of cancer: An in vivo study. Int. J. Nanomed. 2011, 6, 2859–2864. [Google Scholar]
- Hainfeld, J.F.; O’Connor, M.J.; Dilmanian, F.A.; Slatkin, D.N.; Adams, D.J.; Smilowitz, H.M. Micro-CT enables microlocalisation and quantification of Her2-targeted gold nanoparticles within tumour regions. Br. J. Radiol. 2011, 84, 526–533. [Google Scholar] [CrossRef]
- Ahn, S.; Jung, S.Y.; Lee, S.J. Gold Nanoparticle Contrast Agents in Advanced X-ray Imaging Technologies. Molecules 2013, 18, 5858–5890. [Google Scholar] [CrossRef] [PubMed]
- Hainfeld, J.F.; Slatkin, D.N.; Focella, T.M.; Smilowitz, H.M. Gold nanoparticles: A new X-ray contrast agent. Br. J. Radiol. 2006, 79, 248–253. [Google Scholar] [CrossRef]
- Delorme, R.; Taupin, F.; Flaender, M.; Ravanat, J.L.; Champion, C.; Agelou, M.; Elleaume, H. Comparison of gadolinium nanoparticles and molecular contrast agents for radiation therapy-enhancement. Med. Phys. 2017, 44, 5949–5960. [Google Scholar] [CrossRef]
- Miladi, I.; Aloy, M.T.; Armandy, E.; Mowat, P.; Kryza, D.; Magné, N.; Tillement, O.; Lux, F.; Billotey, C.; Janier, M.; et al. Combining ultrasmall gadolinium-based nanoparticles with photon irradiation overcomes radioresistance of head and neck squamous cell carcinoma. Nanomed. Nanotechnol. Biol. Med. 2015, 11, 247–257. [Google Scholar] [CrossRef]
- Prezado, Y.; Fois, G.; Le Duc, G.; Bravin, A. Gadolinium dose enhancement studies in microbeam radiation therapy. Med. Phys. 2009, 36, 3568–3574. [Google Scholar] [CrossRef]
- Zhang, D.G.; Feygelman, V.; Moros, E.G.; Latifi, K.; Zhang, G.G. Monte Carlo study of radiation dose enhancement by gadolinium in megavoltage and high dose rate radiotherapy. PLoS ONE 2014, 9, e109389. [Google Scholar] [CrossRef]
- Verry, C.; Dufort, S.; Barbier, E.L.; Montigon, O.; Peoc’h, M.; Chartier, P.; Lux, F.; Balosso, J.; Tillement, O.; Sancey, L.; et al. MRI-guided clinical 6-MV radiosensitization of glioma using a unique gadolinium-based nanoparticles injection. Nanomedicine 2016, 11, 2405–2417. [Google Scholar] [CrossRef] [PubMed]
- Bort, G.; Lux, F.; Dufort, S.; Crémillieux, Y.; Verry, C.; Tillement, O. EPR-mediated tumor targeting using ultrasmall-hybrid nanoparticles: From animal to human with theranostic AGuIX nanoparticles. Theranostics 2020, 10, 319–1331. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.J. XCOM: Photon cross sections database. NIST 1998, 8, 3587. Available online: https://physics.nist.gov/PhysRefData/Xcom/html/xcom1.html (accessed on 18 July 2023).
- Rahman, W.N.; Corde, S.; Yagi, N.; Abdul Aziz, S.A.; Annabell, N.; Geso, M. Optimal energy for cell radiosensitivity enhancement by gold nanoparticles using synchrotron-based monoenergetic photon beams. Int. J. Nanomed. 2014, 19, 22459–22467. [Google Scholar] [CrossRef] [PubMed]
- Zygmanski, P.; Liu, B.; Tsiamas, P.; Cifter, F.; Petersheim, M.; Hesser, J.; Sajo, E. A stochastic model of cell survival for high-Z nanoparticle radiotherapy. Phys. Med. Biol. 2013, 58, 7961–7977. [Google Scholar] [CrossRef] [PubMed]
- Spiga, J.; Pellicioli, P.; Manger, S.P.; Duffy, J.A.; Bravin, A. Experimental benchmarking of Monte Carlo simulations for radiotherapy dosimetry using monochromatic X-ray beams in the presence of metal-based compounds. Phys. Med. 2019, 66, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Sisin, N.N.T.; Rashid, R.A.; Abdullah, R.; Razak, K.A.; Geso, M.; Akasaka, H.; Sasaki, R.; Tominaga, T.; Miura, H.; Nishi, M.; et al. Gafchromic™ EBT3 Film Measurements of Dose Enhancement Effects by Metallic Nanoparticles for 192Ir Brachytherapy, Proton, Photon and Electron Radiotherapy. Radiation 2022, 2, 130–148. [Google Scholar] [CrossRef]
- Santibáñez, M.; Fuentealba, M. Experimental determination of Gd dose enhancement and Gd dose sparing by 192Ir brachytherapy source with Gafchromic EBT3 dosimeter. Appl. Radiat. Isot. 2021, 175, 5109787. [Google Scholar] [CrossRef]
- Santibáñez, M.; Fuentealba, M.; Torres, F.; Vargas, A. Experimental determination of the gadolinium dose enhancement in phantom irradiated with low energy X-ray sources by a spectrophotometer-Gafchromic-EBT3 dosimetry system. Appl. Radiat. Isot. 2019, 154, 108857. [Google Scholar] [CrossRef]
- Cho, J.; Gonzalez-Lepera, C.; Manohar, N.; Kerr, M.; Krishnan, S.; Cho, S.H. Quantitative investigation of physical factors contributing to gold nanoparticle-mediated proton dose enhancement. Phys. Med. Biol. 2016, 61, 562–2581. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, R.; Royle, G.; Lourenço, A.; Schwarz, M.; Fracchiolla, F.; Ricketts, K. Investigation into the effects of high-Z nano materials in proton therapy. Phys. Med. Biol. 2016, 61, 4537–4550. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.Y.P.; Chun, S.L.; Yu, K.N. Quality assurance of alpha-particle dosimetry using peeled-off Gafchromic EBT3® film. Rad. Phys. Chem. 2016, 125, 176–179. [Google Scholar] [CrossRef]
- Kakade, N.R.; Das, A.; Kumar, R.; Sharma, S.D.; Chadha, R.; Maiti, N.; Kapoor, S. Application of unlaminated EBT3 film dosimeter for quantification of dose enhancement using silver nanoparticle-embedded alginate film. Biomed. Phys. Eng. Express 2022, 8, 035014. [Google Scholar] [CrossRef]
- Yuri, Y.; Narumi, K.; Yuyama, T. Characterization of a Gafchromic film for the two-dimensional profile measurement of low-energy heavy-ion beams. Nucl. Instrum. Methods Phys. Res. Sect. A Accel. Spectrometers Detect. Assoc. Equip. 2016, 828, 515–521. [Google Scholar] [CrossRef]
- Fuentealba, M.; Santibañez, M.; Bodineau, C. Gadolinium dose enhancement determination by unlaminated EBT3 films irradiated with 192Ir brachytherapy source. Rad. Phys. Chem. 2023, 212, 111103. [Google Scholar] [CrossRef]
- Ma, C.M.; Coffey, C.W.; DeWerd, L.A.; Liu, C.; Nath, R.; Seltzer, S.M.; Seuntjens, J.P. AAPM protocol for 40–300 kV X-ray beam dosimetry in radiotherapy and radiobiology. Med. Phys. 2001, 28, 868–893. [Google Scholar] [CrossRef]
- Williams, M.; Metcalfe, P. Radiochromic film dosimetry and its applications in radiotherapy. In Proceedings of the AIP Conference, Wollongong, Australia, 15–18 September 2010; Volume 1345, pp. 75–99. [Google Scholar]
- Das, I.J. 3. Physics and characteristic of radiochromic films: 3.6 Dose response. In Radiochromic Film: Role and Applications in Radiation Dosimetry; Das, I.J., Ed.; CRC Press: Boca Raton, FL, USA, 2017; pp. 41–44. [Google Scholar]


| Medium | 50 kVp | 70 kVp | ||
|---|---|---|---|---|
| Dose (Gy) | DEF | Dose (Gy) | DEF | |
| Water | 3.00 | – | 3.00 | – |
| 10 mg/mL | 2.84 ± 0.12 | −5 ± 4% | 3.16 ± 0.18 | +6 ± 6% |
| 20 mg/mL | 2.32 ± 0.18 | −23 ± 6% | 3.67 ± 0.21 | +22 ± 7% |
| Concentration (mg/mL Gd) | Prescribed Dose (Gy) | Measured Dose (Gy) | DEF (%) |
|---|---|---|---|
| 10 | 3.00 | 3.17 ± 0.17 | +6.0 ± 6% |
| 20 | 3.00 | 3.67 ± 0.22 | +22.0 ± 7% |
| 30 | 3.00 | 3.26 ± 0.20 | +9.0 ± 7% |
| Concentration (mg/mL Gd) | Prescribed Dose (Gy) | Measured Dose with a 12 m Film (Gy) | Measured Dose with a 2.5 m Film (Gy) | Relative DEF (%) 2.5 m/12 m |
|---|---|---|---|---|
| 20 | 3.00 | 2.84 ± 0.15 | 3.67 ± 0.22 | +29.0 ± 7% |
| 30 | 3.00 | 2.43 ± 0.18 | 3.26 ± 0.20 | +34.0 ± 7% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuentealba, M.; Ferreira, A.; Salgado, A.; Vergara, C.; Díez, S.; Santibáñez, M. An Optimized Method for Evaluating the Potential Gd-Nanoparticle Dose Enhancement Produced by Electronic Brachytherapy. Nanomaterials 2024, 14, 430. https://doi.org/10.3390/nano14050430
Fuentealba M, Ferreira A, Salgado A, Vergara C, Díez S, Santibáñez M. An Optimized Method for Evaluating the Potential Gd-Nanoparticle Dose Enhancement Produced by Electronic Brachytherapy. Nanomaterials. 2024; 14(5):430. https://doi.org/10.3390/nano14050430
Chicago/Turabian StyleFuentealba, Melani, Alejandro Ferreira, Apolo Salgado, Christopher Vergara, Sergio Díez, and Mauricio Santibáñez. 2024. "An Optimized Method for Evaluating the Potential Gd-Nanoparticle Dose Enhancement Produced by Electronic Brachytherapy" Nanomaterials 14, no. 5: 430. https://doi.org/10.3390/nano14050430
APA StyleFuentealba, M., Ferreira, A., Salgado, A., Vergara, C., Díez, S., & Santibáñez, M. (2024). An Optimized Method for Evaluating the Potential Gd-Nanoparticle Dose Enhancement Produced by Electronic Brachytherapy. Nanomaterials, 14(5), 430. https://doi.org/10.3390/nano14050430






