Influence of Clinical Decontamination Techniques on the Surface Characteristics of SLA Titanium Implant
Abstract
1. Introduction
2. Materials and Methods
2.1. Titanium Disc Preparation
2.2. Implant Surface Treatment
2.3. Surface Characterization of Titanium Discs
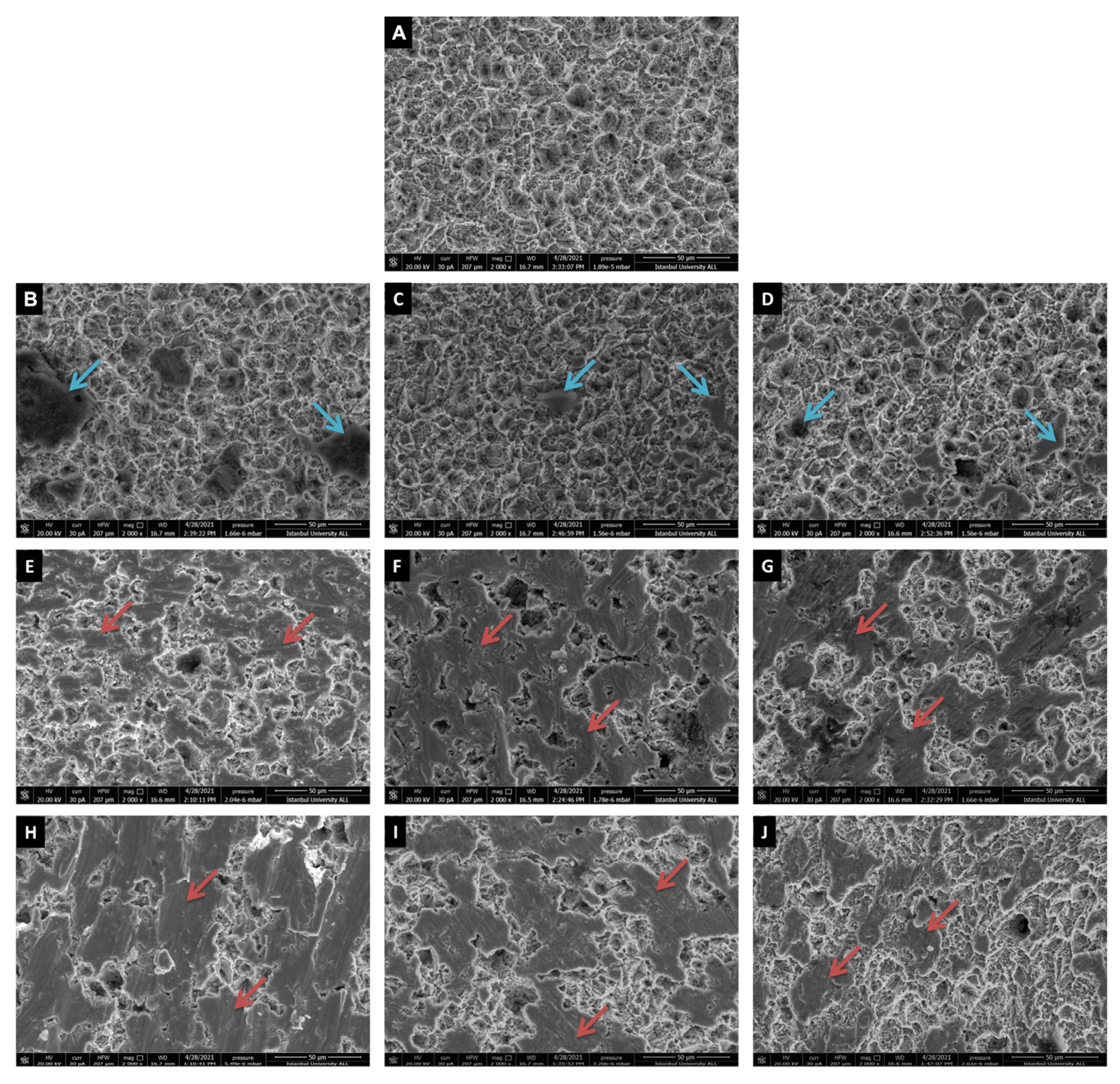
2.3.1. Scanning Electron Microscopy (SEM)
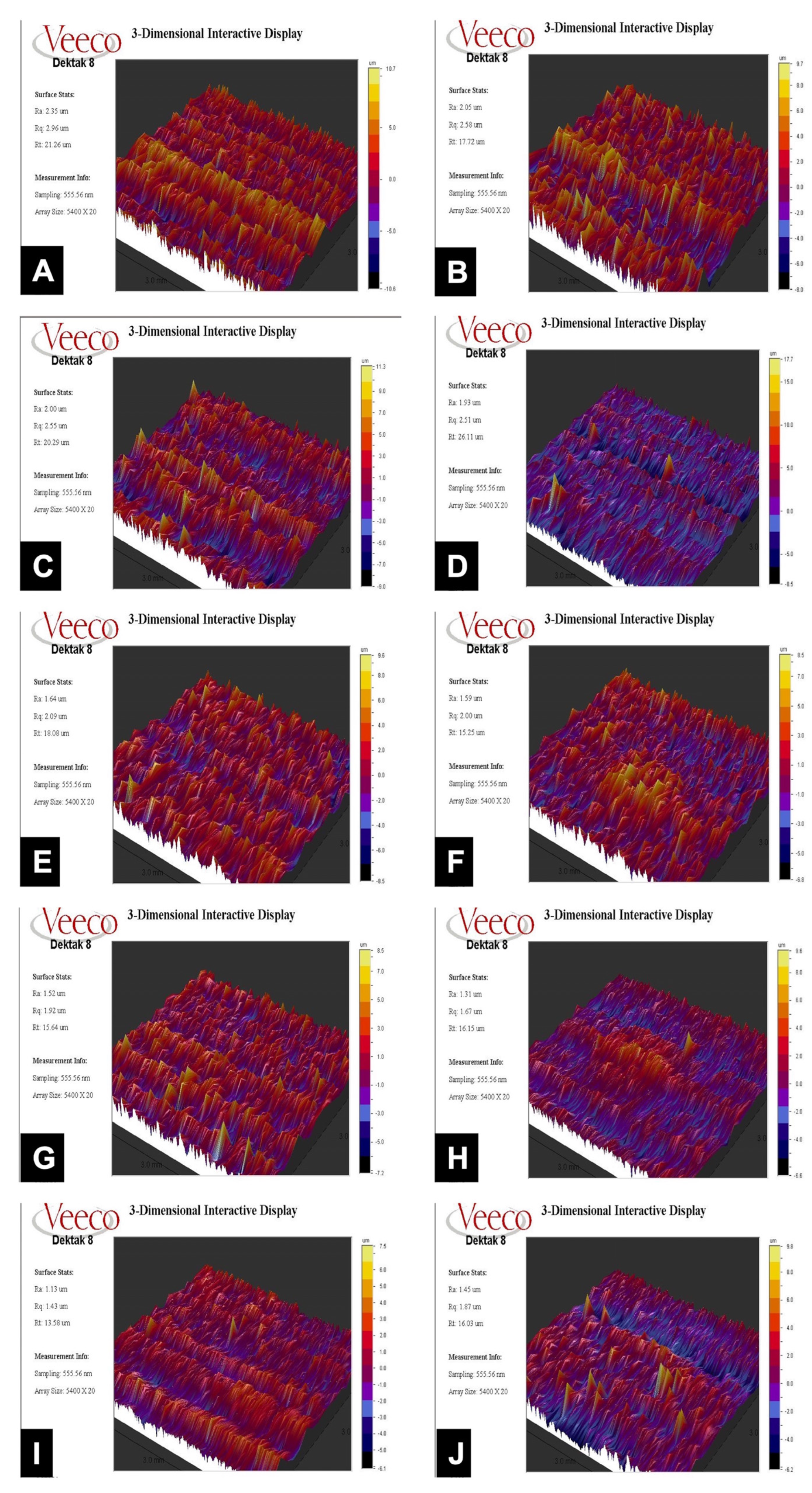
2.3.2. Surface Roughness Measurement
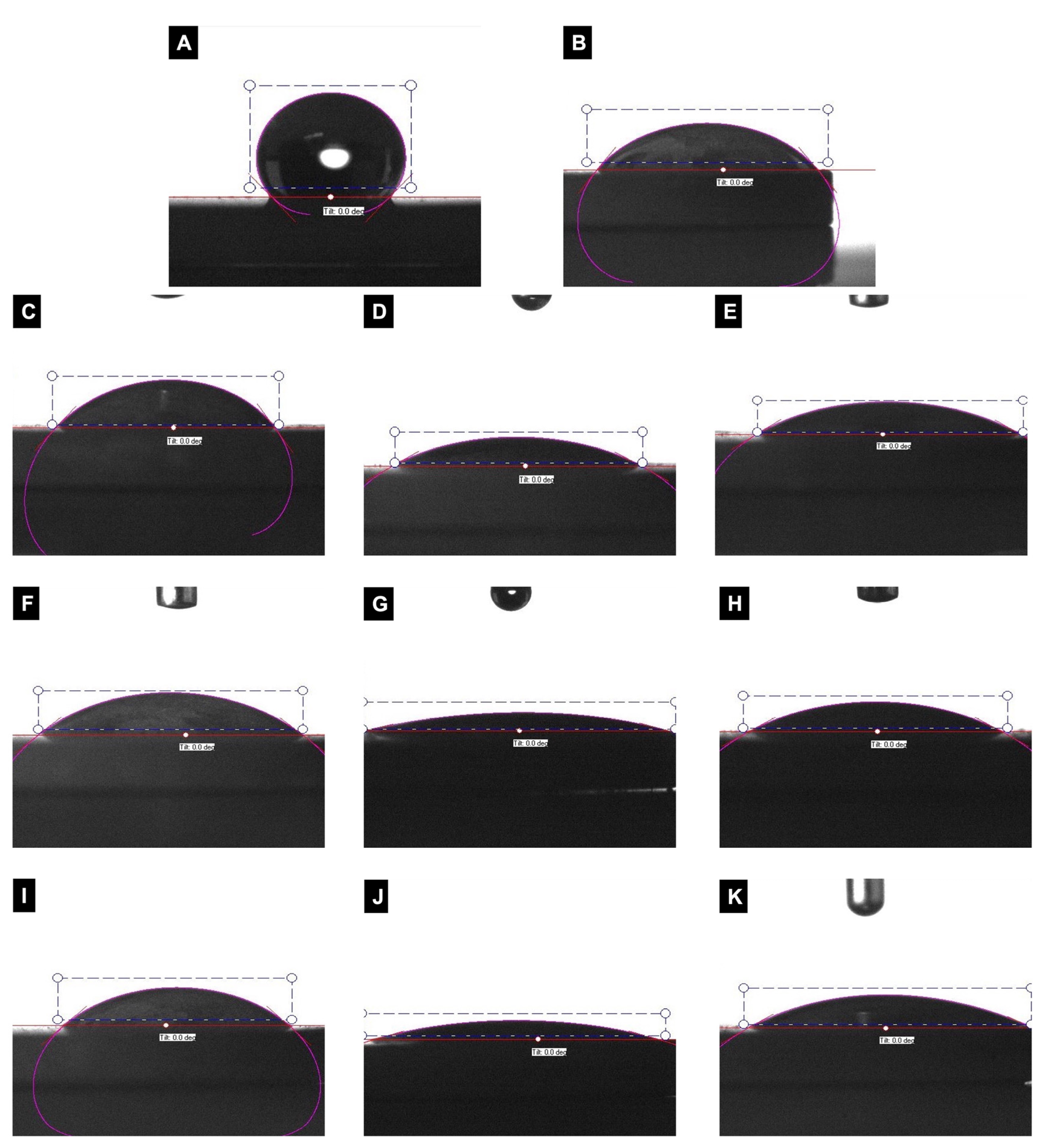
2.3.3. Contact Angle Measurement
2.4. Statistical Analysis
3. Results
3.1. Influence of Decontamination Treatment on Surface Topography
3.2. Surface Roughness Changes with Implant Decontamination
3.3. Surface Decontamination Alters Implant Wettability
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lindhe, J.; Meyle, J. Peri-implant diseases: Consensus report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 282–285. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Gulati, K.; Arora, H.; Han, P.; Fournier, B.; Ivanovski, S. Race to invade: Understanding soft tissue integration at the transmucosal region of titanium dental implants. Dent. Mater. 2021, 37, 816–831. [Google Scholar] [CrossRef] [PubMed]
- Mombelli, A.; Van Oosten, M.A.C.; Schürch, E., Jr.; Lang, N.P. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol. Immunol. 1987, 2, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Papanicolau, P.; Rothamel, D.; Beck, B.; Herten, M.; Becker, J. Influence of plaque biofilm removal on reestablishment of the biocompatibility of contaminated titanium surfaces. J. Biomed. Mater. Res. A 2006, 77, 437–444. [Google Scholar] [CrossRef]
- Schwarz, F.; Rothamel, D.; Sculean, A.; Georg, T.; Scherbaum, W.; Becker, J. Effects of an Er:YAG laser and the Vector ultrasonic system on the biocompatibility of titanium implants in cultures of human osteoblast-like cells. Clin. Oral Implant. Res. 2003, 14, 784–792. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Sculean, A.; Romanos, G.; Herten, M.; Horn, N.; Scherbaum, W.; Becker, J. Influence of different treatment approaches on the removal of early plaque biofilms and the viability of SAOS2 osteoblasts grown on titanium implants. Clin. Oral Investig. 2005, 9, 111–117. [Google Scholar] [CrossRef]
- Fox, S.C.; Moriarty, J.D.; Kusy, R.P. The Effects of Scaling a Titanium Implant Surface with Metal and Plastic Instruments: An in vitro Study. J. Periodontol. 1990, 61, 485–490. [Google Scholar] [CrossRef]
- Kreisler, M.; Götz, H.; Duschner, H. Effect of Nd:YAG, Ho:YAG, Er:YAG, CO2, and GaAIAs laser irradiation on surface properties of endosseous dental implants. Int. J. Oral Maxillofac. Implant. 2002, 17, 202–211. [Google Scholar]
- Kreisler, M.; Kohnen, W.; Christoffers, A.-B.; Götz, H.; Jansen, B.; Duschner, H.; D’Hoedt, B. In vitro evaluation of the biocompatibility of contaminated implant surfaces treated with an Er: YAG laser and an air powder system. Clin. Oral Implant. Res. 2004, 16, 36–43. [Google Scholar] [CrossRef]
- Kotsakis, G.A.; Black, R.; Kum, J.; Berbel, L.; Sadr, A.; Karoussis, I.; Simopoulou, M.; Daubert, D. Effect of implant cleaning on titanium particle dissolution and cytocompatibility. J. Periodontol. 2021, 92, 580–591. [Google Scholar] [CrossRef]
- Giannelli, M.; Landini, G.; Materassi, F.; Chellini, F.; Antonelli, A.; Tani, A.; Zecchi-Orlandini, S.; Rossolini, G.M.; Bani, D. The effects of diode laser on Staphylococcus aureus biofilm and Escherichia coli lipopolysaccharide adherent to titanium oxide surface of dental implants. An in vitro study. Lasers Med. Sci. 2016, 31, 1613–1619. [Google Scholar] [CrossRef] [PubMed]
- Chellini, F.; Giannelli, M.; Tani, A.; Ballerini, L.; Vallone, L.; Nosi, D.; Zecchi-Orlandini, S.; Sassoli, C. Mesenchymal stromal cell and osteoblast responses to oxidized titanium surfaces pre-treated with λ = 808 nm GaAlAs diode laser or chlorhexidine: In vitro study. Lasers Med. Sci. 2017, 32, 1309–1320. [Google Scholar] [CrossRef] [PubMed]
- Galli, C.; Macaluso, G.M.; Elezi, E.; Ravanetti, F.; Cacchioli, A.; Gualini, G.; Passeri, G. The Effects of Er:YAG Laser Treatment on Titanium Surface Profile and Osteoblastic Cell Activity: An in vitro Study. J. Periodontol. 2011, 82, 1169–1177. [Google Scholar] [CrossRef] [PubMed]
- Wennerberg, A.; Albrektsson, T. Effects of titanium surface topography on bone integration: A systematic review. Clin. Oral Implant. Res. 2009, 20 (Suppl. 4), 172–184. [Google Scholar] [CrossRef] [PubMed]
- Bollenl, C.M.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef] [PubMed]
- Toma, S.; Lasserre, J.; Brecx, M.C.; Nyssen-Behets, C. In vitro evaluation of peri-implantitis treatment modalities on Saos-2osteoblasts. Clin. Oral Implant. Res. 2016, 27, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Homayouni, A.; Bahador, A.; Moharrami, M.; Pourhajibagher, M.; Rasouli-Ghahroudi, A.A.; Alikhasi, M. Effect of 5 Popular Disinfection Methods on Microflora of Laboratory: Customized Implant Abutments. Implant Dent. 2019, 28, 437–446. [Google Scholar] [CrossRef]
- Moharrami, M.; Perrotti, V.; Iaculli, F.; Love, R.M.; Quaranta, A. Effects of air abrasive decontamination on titanium surfaces: A systematic review of in vitro studies. Clin. Implant. Dent. Relat. Res. 2019, 21, 398–421. [Google Scholar] [CrossRef]
- Lang, N.P.; Salvi, G.E.; Huynh-Ba, G.; Ivanovski, S.; Donos, N.; Bosshardt, D.D. Early osseointegration to hydrophilic and hydrophobic implant surfaces in humans. Clin. Oral Implant. Res. 2011, 22, 349–356. [Google Scholar] [CrossRef]
- Berglundh, T.; Gotfredsen, K.; Zitzmann, N.U.; Lang, N.P.; Lindhe, J. Spontaneous progression of ligature induced peri-implantitis at implants with different surface roughness: An experimental study in dogs. Clin. Oral Implant. Res. 2007, 18, 655–661. [Google Scholar] [CrossRef]
- Sartoretto, S.C.; Alves, A.T.N.N.; Resende, R.F.B.; Calasans-Maia, J.; Granjeiro, J.; Calasans-Maia, M.D. Early osseointegration driven by the surface chemistry and wettability of dental implants. J. Appl. Oral Sci. 2015, 23, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Chopra, D.; Jayasree, A.; Guo, T.; Gulati, K.; Ivanovski, S. Advancing dental implants: Bioactive and therapeutic modifications of zirconia. Bioact. Mater. 2022, 13, 161–178. [Google Scholar] [CrossRef] [PubMed]
- Shalabi, M.; Gortemaker, A.; Hof, M.V.; Jansen, J.; Creugers, N. Implant Surface Roughness and Bone Healing: A Systematic Review. J. Dent. Res. 2006, 85, 496–500. [Google Scholar] [CrossRef]
- Chambrone, L.; Shibli, J.A.; Mercúrio, C.E.; Cardoso, B.; Preshaw, P.M. Efficacy of standard (SLA) and modified sandblasted and acid-etched (SLActive) dental implants in promoting immediate and/or early occlusal loading protocols: A systematic review of prospective studies. Clin. Oral Implant. Res. 2015, 26, 359–370. [Google Scholar] [CrossRef] [PubMed]
- Bowers, K.T.; Keller, J.C.; Randolph, B.A.; Wick, D.G.; Michaels, C.M. Optimization of surface micromorphology for enhanced osteoblast responses in vitro. Int. J. Oral Maxillofac. Implants 1992, 7, 302–310. [Google Scholar]
- Heitz-Mayfield, L.J.; Mombelli, A. The therapy of peri-implantitis: A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 325–345. [Google Scholar] [CrossRef] [PubMed]
- Al-Hashedi, A.A.; Laurenti, M.; Benhamou, V.; Tamimi, F. Decontamination of titanium implants using physical methods. Clin. Oral Implant. Res. 2017, 28, 1013–1021. [Google Scholar] [CrossRef]
- Lee, B.-S.; Shih, K.-S.; Lai, C.-H.; Takeuchi, Y.; Chen, Y.-W. Surface property alterations and osteoblast attachment to contaminated titanium surfaces after different surface treatments: An in vitro study. Clin. Implant Dent. Relat. Res. 2018, 20, 583–591. [Google Scholar] [CrossRef]
- Lee, J.-B.; Jo, Y.-H.; Choi, J.-Y.; Seol, Y.-J.; Lee, Y.-M.; Ku, Y.; Rhyu, I.-C.; Yeo, I.-S.L. The Effect of Ultraviolet Photofunctionalization on a Titanium Dental Implant with Machined Surface: An In Vitro and In Vivo Study. Materials 2019, 12, 2078. [Google Scholar] [CrossRef]
- Secgin-Atar, A.; Aykol-Sahin, G.; Kocak-Oztug, N.A.; Yalcin, F.; Gokbuget, A.; Baser, U. Evaluation of Surface Change and Roughness in Implants Lost Due to Peri-Implantitis Using Erbium Laser and Various Methods: An In Vitro Study. Nanomaterials 2021, 11, 2602. [Google Scholar] [CrossRef]
- Mahato, N.; Wu, X.; Wang, L. Management of peri-implantitis: A systematic review, 2010–2015. SpringerPlus 2016, 5, 105. [Google Scholar] [CrossRef] [PubMed]
- Sahm, N.; Becker, J.; Santel, T.; Schwarz, F. Non-surgical treatment of peri-implantitis using an air-abrasive device or mechanical debridement and local application of chlorhexidine: A prospective, randomized, controlled clinical study. J. Clin. Periodontol. 2011, 38, 872–878. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Lessem, J.; Dahlén, G.; Renvert, H.; Lindahl, C. Mechanical and Repeated Antimicrobial Therapy Using a Local Drug Delivery System in the Treatment of Peri-Implantitis: A Randomized Clinical Trial. J. Periodontol. 2008, 79, 836–844. [Google Scholar] [CrossRef] [PubMed]
- Mettraux, G.R.; Sculean, A.; Bürgin, W.B.; Salvi, G.E. Two-year clinical outcomes following non-surgical mechanical therapy of peri-implantitis with adjunctive diode laser application. Clin. Oral Implant. Res. 2016, 27, 845–849. [Google Scholar] [CrossRef]
- Stübinger, S.; Etter, C.; Miskiewicz, M.; Homann, F.; Saldamli, B.; Wieland, M.; Sader, R. Surface alterations of polished and sandblasted and acid-etched titanium implants after Er:YAG, carbon dioxide, and diode laser irradiation. Int. J. Oral Maxillofac. Implant. 2010, 25, 104–111. [Google Scholar]
- Castro, G.L.; Gallas, M.; Núñez, I.R.; Borrajo, J.L.L.; Álvarez, J.C.; Varela, L.G. Scanning Electron Microscopic Analysis of Diode Laser-Treated Titanium Implant Surfaces. Photomed. Laser Surg. 2007, 25, 124–128. [Google Scholar] [CrossRef]
- Wehner, C.; Laky, M.; Shokoohi-Tabrizi, H.A.; Behm, C.; Moritz, A.; Rausch-Fan, X.; Andrukhov, O. Effects of Er:YAG laser irradiation of different titanium surfaces on osteoblast response. J. Mater. Sci. Mater. Med. 2021, 32, 22. [Google Scholar] [CrossRef]
- Deppe, H.; Horch, H.-H.; Neff, A. Conventional versus CO2 laser-assisted treatment of peri-implant defects with the concomitant use of pure-phase beta-tricalcium phosphate: A 5-year clinical report. Int. J. Oral Maxillofac. Implants 2007, 22, 79–86. [Google Scholar]
- Romanos, G.; Nentwig, G.-H. Diode Laser (980 nm) in Oral and Maxillofacial Surgical Procedures: Clinical Observations Based on Clinical Applications. J. Clin. Laser Med. Surg. 1999, 17, 193–197. [Google Scholar] [CrossRef]
- Lollobrigida, M.; Fortunato, L.; Serafini, G.; Mazzucchi, G.; Bozzuto, G.; Molinari, A.; Serra, E.; Menchini, F.; Vozza, I.; De Biase, A. The Prevention of Implant Surface Alterations in the Treatment of Peri-Implantitis: Comparison of Three Different Mechanical and Physical Treatments. Int. J. Environ. Res. Public Health 2020, 17, 2624. [Google Scholar] [CrossRef]
- Aoki, A.; Mizutani, K.; Schwarz, F.; Sculean, A.; Yukna, R.A.; Takasaki, A.A.; Romanos, G.E.; Taniguchi, Y.; Sasaki, K.M.; Zeredo, J.L.; et al. Periodontal and peri-implant wound healing following laser therapy. Periodontology 2000 2015, 68, 217–269. [Google Scholar] [CrossRef] [PubMed]
- Schwarz, F.; Aoki, A.; Sculean, A.; Becker, J. The impact of laser application on periodontal and peri-implant wound healing. Periodontology 2000 2009, 51, 79–108. [Google Scholar] [CrossRef] [PubMed]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and/or surface topography on biofilm development. Clin. Oral Implants Res. 2006, 17, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Größner-Schreiber, B.; Teichmann, J.; Hannig, M.; Dörfer, C.; Wenderoth, D.F.; Ott, S.J. Modified implant surfaces show different biofilm compositions under in vivo conditions. Clin. Oral Implant. Res. 2009, 20, 817–826. [Google Scholar] [CrossRef]
- Mendoza-Arnau, A.; Vallecillo-Capilla, M.F.; Cabrerizo-Vílchez, M.Á.; Rosales-Leal, J.I. Topographic characterisation of dental implants for commercial use. Med. Oral Patol. Oral Cir. Bucal. 2016, 21, e631-6. [Google Scholar] [CrossRef]
- Park, J.-B.; Jeon, Y.; Ko, Y. Effects of titanium brush on machined and sand-blasted/acid-etched titanium disc using confocal microscopy and contact profilometry. Clin. Oral Implant. Res. 2015, 26, 130–136. [Google Scholar] [CrossRef]
- Bachle, M.; Kohal, R. A systematic review of the influence of different titanium surfaces on proliferation, differentiation and protein synthesis of osteoblast-like MG63 cells. Clin. Oral Implant. Res. 2004, 15, 683–692. [Google Scholar] [CrossRef]
- Albrektsson, T.; Wennerberg, A. Oral implant surfaces: Part 1—Review focusing on topographic and chemical properties of different surfaces and in vivo responses to them. Int. J. Prosthodont 2004, 17, 536–543. [Google Scholar]
- Buser, D.; Broggini, N.; Wieland, M.; Schenk, R.K.; Denzer, A.J.; Cochran, D.L.; Hoffmann, B.; Lussi, A.; Steinemann, S.G. Enhanced Bone Apposition to a Chemically Modified SLA Titanium Surface. J. Dent. Res. 2004, 83, 529–533. [Google Scholar] [CrossRef]
- Rupp, F.; Scheideler, L.; Eichler, M.; Geis-Gerstorfer, J. Wetting behavior of dental implants. Int. J. Oral Maxillofac. Implant 2011, 26, 1256–1266. [Google Scholar]
- Palmquist, A.; Engqvist, H.; Lausmaa, J.; Thomsen, P. Commercially Available Dental Implants: Review of Their Surface Characteristics. J. Biomater. Tissue Eng. 2012, 2, 112–124. [Google Scholar] [CrossRef]
- Kozlovsky, A.; Artzi, Z.; Moses, O.; Kamin-Belsky, N.; Greenstein, R.B.-N. Interaction of Chlorhexidine With Smooth and Rough Types of Titanium Surfaces. J. Periodontol. 2006, 77, 1194–1200. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, A.H.; Mutsaers, C.A.H.A. Adsorption of hydrogen peroxide on the surface of titanium dioxide. J. Phys. Chem. 1975, 79, 1940–1943. [Google Scholar] [CrossRef]
- Matthes, R.; Jablonowski, L.; Pitchika, V.; Holtfreter, B.; Eberhard, C.; Seifert, L.; Gerling, T.; Scholten, L.V.; Schlüter, R.; Kocher, T. Efficiency of biofilm removal by combination of water jet and cold plasma: An in-vitro study. BMC Oral Health 2022, 22, 157. [Google Scholar] [CrossRef] [PubMed]
| Group Name | Treatment | Details |
|---|---|---|
| Control | No treatment | Sterilized as-received SLA (Sandblasted-acid-etched) surface grade 4 Ti discs. |
| Group 1 | Diode laser | Diode laser (Biolase, California, USA) was applied to Ti discs at a wavelength of λ = 808 ± 10 nm, 1 W (power) under continuous mode for 60 s. The laser tip was kept at a distance of 2–5 mm from the discs to prevent overheating, and saline cooling was applied to the entire surface during treatment [11,12]. |
| Group 2 | Diode laser + 3% H2O2 | After laser treatment, the discs were immersed in 3% H2O2 solution for 60 s [17]. |
| Group 3 | Diode Laser + 0.2% CHX | After laser treatment, the discs were immersed in 0.2% CHX solution for 60 s [12]. |
| Group 4 | Ti brush | Ti brush (Ti-Brush, Straumann, Basel, Switzerland) was applied to Ti discs at 920 rpm under saline irrigation for 60 s. A new brush was used for each disc [27]. |
| Group 5 | Ti Brush + 3% H2O2 | After Ti brush treatment, the discs were immersed in 3% H2O2 solution for 60 s. |
| Group 6 | Ti Brush + 0.2% CHX | After Ti brush treatment, the discs were immersed in 0.2% CHX solution for 60 s. |
| Group 7 | Ti curette | Ti discs were instrumented with a Ti curette (LM-ErgoMix™, Planmeca Group, Pargas, Finland) for 60 s in one direction at an angle of 45 degrees, and saline irrigation was applied to prevent surface heating [28] |
| Group 8 | Ti Curette + 3% H2O2 | After Ti-curette instrumentation, the discs were immersed in 3% H2O2 solution for 60 s. |
| Group 9 | Ti Curette + 0.2% CHX | After Ti-curette instrumentation, the discs were immersed in 0.2% CHX solution for 60 s. |
| Groups | Ra | Rq | Rt | |
|---|---|---|---|---|
| Control | Mean ± SD | 2.25 ± 0.14 | 2.84 ± 0.17 | 24.39 ± 5.87 |
| Median (Min–Max) | 2.3 (2.1–2.4) | 3 (2.6–3) | 22.1 (17.7–31.9) | |
| Laser | Mean ± SD | 2.08 ± 0.14 | 2.75 ± 0.31 | 32.23 ± 7.57 |
| Median (Min–Max) | 2.1 (1.9–2.3) | 2.7 (2.5–3.3) | 31.3 (26.1–44.7) | |
| Laser + H2O2 | Mean ± SD | 1.91 ± 0.32 | 2.51 ± 0.44 | 28.47 ± 6.36 |
| Median (Min–Max) | 2 (1.5–2.4) | 2.6 (1.9–3.1) | 29.6 (18.4–35.7) | |
| Laser + CHX | Mean ± SD | 1.92 ± 0.10 | 2.53 ± 0.15 | 30.69 ± 8.57 |
| Median (Min–Max) | 1.9 (1.8–2) | 2.6 (2.3–2.7) | 34.4 (20.3–38.4) | |
| Ti Brush | Mean ± SD | 1.62 ± 0.05 | 2.06 ± 0.09 | 16.68 ± 1.69 |
| Median (Min–Max) | 1.6 (1.6–1.7) | 2.1 (1.9–2.1) | 17.5 (13.8–18.1) | |
| Ti Brush + H2O2 | Mean ± SD | 1.68 ± 0.12 | 2.22 ± 0.25 | 20.27 ± 5.49 |
| Median (Min–Max) | 1.7 (1.5–1.8) | 2.3 (1.9–2.5) | 18.6 (15.3–29.6) | |
| Ti Brush + CHX | Mean ± SD | 1.47 ± 0.06 | 1.87 ± 0.09 | 17.84 ± 4.40 |
| Median (Min–Max) | 1.5 (1.4–1.5) | 1.8 (1.8–2) | 16.6 (13.4–25) | |
| Ti Curette | Mean ± SD | 1.22 ± 0.18 | 1.58 ± 0.24 | 18.13 ± 4.95 |
| Median (Min–Max) | 1.2 (1–1.5) | 1.6 (1.4–1.9) | 16.2 (13.6–24) | |
| Ti Curette + H2O2 | Mean ± SD | 1.14 ± 0.17 | 1.51 ± 0.29 | 15.99 ± 2.88 |
| Median (Min–Max) | 1.1 (0.9–1.3) | 1.4 (1.2–1.9) | 14.5 (13.6–19.3) | |
| Ti Curette+ CHX | Mean ± SD | 1.42 ± 0.21 | 1.85 ± 0.25 | 20.75 ± 3.62 |
| Median (Min–Max) | 1.4 (1.2–1.7) | 1.9 (1.5–2.2) | 22.6 (16–23.7) | |
| p | a 0.001 ** | a 0.001 ** | a 0.001 ** |
| Contact Angle | p | |||
|---|---|---|---|---|
| Mean ± SD | Median (Min–Max) | |||
| Groups | Negative control | 129.20 ± 10.03 | 131 (112–138) | a 0.001 ** |
| Positive control | 41.40 ± 8.91 | 37 (33–52) | ||
| 1. Laser | 53.40 ± 8.20 | 50 (44–63) | ||
| 2. Laser + H2O2 | 23.80 ± 2.86 | 24 (20–27) | ||
| 3. Laser + CHX | 36.20 ± 4.66 | 35 (31–42) | ||
| 4. Ti Brush | 45.80 ± 3.70 | 46 (41–51) | ||
| 5. Ti Brush+ H2O2 | 10.40 ± 2.97 | 10 (6–14) | ||
| 6. Ti Brush + CHX | 24.40 ± 4.16 | 25 (19–30) | ||
| 7. Ti Curette | 46.80 ± 4.97 | 46 (40–53) | ||
| 8. Ti Curette + H2O2 | 12.60 ± 3.05 | 12 (9–17) | ||
| 9. Ti Curette + CHX | 21.40 ± 5.03 | 20 (17–30) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bayrak, M.; Kocak-Oztug, N.A.; Gulati, K.; Cintan, S.; Cifcibasi, E. Influence of Clinical Decontamination Techniques on the Surface Characteristics of SLA Titanium Implant. Nanomaterials 2022, 12, 4481. https://doi.org/10.3390/nano12244481
Bayrak M, Kocak-Oztug NA, Gulati K, Cintan S, Cifcibasi E. Influence of Clinical Decontamination Techniques on the Surface Characteristics of SLA Titanium Implant. Nanomaterials. 2022; 12(24):4481. https://doi.org/10.3390/nano12244481
Chicago/Turabian StyleBayrak, Meltem, Necla Asli Kocak-Oztug, Karan Gulati, Serdar Cintan, and Emine Cifcibasi. 2022. "Influence of Clinical Decontamination Techniques on the Surface Characteristics of SLA Titanium Implant" Nanomaterials 12, no. 24: 4481. https://doi.org/10.3390/nano12244481
APA StyleBayrak, M., Kocak-Oztug, N. A., Gulati, K., Cintan, S., & Cifcibasi, E. (2022). Influence of Clinical Decontamination Techniques on the Surface Characteristics of SLA Titanium Implant. Nanomaterials, 12(24), 4481. https://doi.org/10.3390/nano12244481







