Improved Activity of Herbal Medicines through Nanotechnology
Abstract
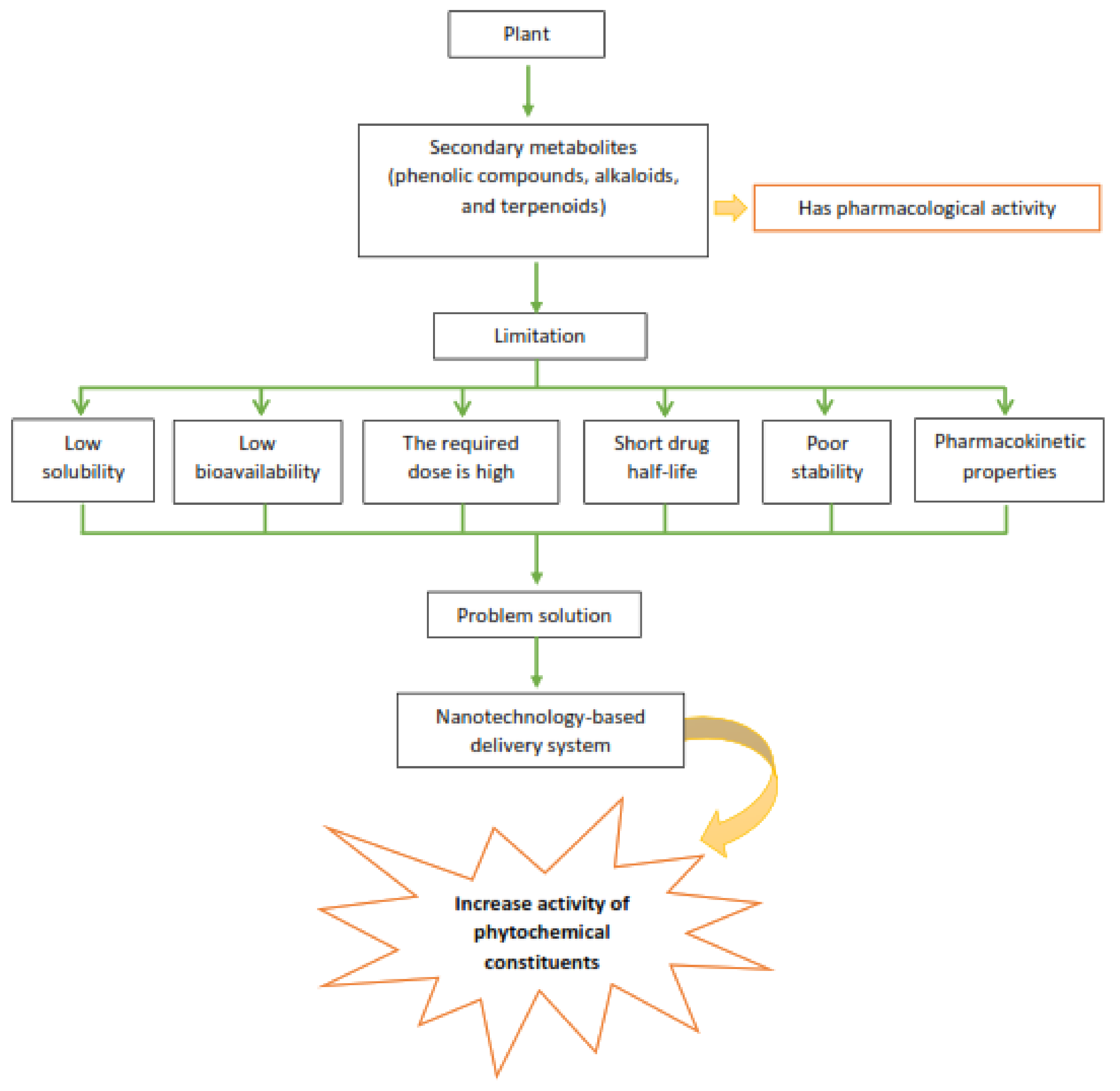
1. Introduction
2. Nanotechnology
3. Nanotechnology-Based Drug Delivery System for Phytochemical Compounds
| Bioactive Compound | Nanoparticle Type | Method of Preparation | Nanoparticle Characteristics * | Drug Release/Pharmacokinetic Properties | Experiment/Model/Dose/Route | Improvement Activity | Toxicity | Ref |
|---|---|---|---|---|---|---|---|---|
| Sinigrin | Phytosomes | Antisolvent precipitation | PS: 153 ± 39 nm | - | Dose: 0.14 mg/mL. In vitro, evaluated on HaCaT cells. | Wound-healing | Sinigrin, phytosome, and phytosome blank (without drug) showed minimal cytotoxicity to HaCaT cells at all concentrations (0.048 mg/mL–0.14 mg/mL). | [49] |
| ZP: 10.09 ± 0.98mV | ||||||||
| %EE: 69.5 ± 5 | ||||||||
| Taxifolin-rich ethyl acetate fraction | Phytosomes | Antisolvent precipitation | PS: (544 nm) | - | In vitro antioxidant activity and ex vivo anticancer investigation by MTT and TB assay using MCF7 cell lines | Antioxidant | - | [50] |
| ZP: −28.1 | ||||||||
| PDI: 0.141 | ||||||||
| %EE: 75.40 ± 0.53% | ||||||||
| Silybins | Phytosomes-nanosuspension | Antisolvent precipitation- high-pressure homogenization | PS: 223.50 ± 4.80 nm | Increased dissolution rate in vitro increased plasma concentration in vivo | In vivo: carbon tetrachloride (CCl4) induced hepatic injury model mice | Hepatoprotection | - | [51] |
| PDI: 0.217 ± 0.011 | ||||||||
| ZP: −23.14 ± 2.73 mV | ||||||||
| Apigenin | Phytosomes | Solvent evaporation | PS: 107.08 ± 1.30 nm | 36-fold increase in water solubility and increase in oral bioavailability | Dose: 25 mg/kg | Antioxidant | - | [52] |
| PDI: 0.37 ± 0.012 | Carbon tetrachloride-induced liver function of a rat model | |||||||
| Quercetin | Phytosomes | Thin film hydration method | PS: 70 ± 7.44 nm | The estrogenic activity of Quercetin-phytosome was investigated in an ovariectomized rat model using 10 and 50 mg/kg/oral doses for 4 weeks | Hormone replacement therapy | - | [53] | |
| %EE: 98.4% | IC50 quercetin: 13.9 μg/mL | |||||||
| ZP: −44.6 ± | IC50 quercetin-phytosome: 11.4 μg/mL | |||||||
| 4.1 mv | ||||||||
| Gingerol | Phytosome | Antisolvent precipitation | PS: 431.21 ± 0.90 nm | Drug release: sustained release | In vitro microbial study: agar well diffusion and dilution method. In vitro Anti-inflammatory Study: study the HRBC membrane lysis and albumin denaturation | Respiratory infection | - | [54] |
| ZP: −17.53 mV | In vitro release: 86.03 ± 0.06% | |||||||
| %EE: 84.36% ± 0.42% | ||||||||
| Phytosome complexed with chitosan | Antisolvent precipitation | PS: 254.01 ± 0.05 nm | Drug release: sustained release | |||||
| ZP: −13.11 mV | In vitro release: 88.93 ± 0.33% | |||||||
| %EE: 86.02% ± 0.72% | ||||||||
| Moringa oleifera leaf extract | Phytosome | Thin film (solvent evaporation) | PS: 198 ± 21 nm | Cytotoxicity assay: MTT assay | Wound dressing | Does not cause cytotoxicity at concentrations <1.5 mg/mL | [55] | |
| ZP: −28.30 ± 1.31 mV | Cell migration assay: NHDF cells | |||||||
| Lantana camara extract | Phytosome | Solvent evaporation | %EE: 82.80% | In vitro drug release of 23% drug at 60 min | Dose: 20 mg/mL | Antibacterial and antifungal | [56] | |
| Murraya koenigii extract | Phytosome | Antisolvent precipitation | PS: 236 nm | Sustain released: | Streptozotocin-nicotinamide induced diabetes model in male Wistar rats | Antidiabetic | [57] | |
| %EE: 75.1% | Release in 6 h: | |||||||
| ZP: −16.85 mV | Phytosome: 30% | |||||||
| Crude extract: 50% |
| Bioactive Compound | Nanoparticle Type | Method of Preparation | Nanoparticle Characteristics * | Drug Release | Experiment/Model/Dose/Route | Application | Toxicity | Ref |
|---|---|---|---|---|---|---|---|---|
| Jatropha pelargoniifolia extract | Chitosan nanoparticles | Ionic gelation | PS: 185.5 nm, | JP-CSNPs: depend on pH of the medium | Antioxidant: DPPH | Antimicrobial and anticancer | - | [58] |
| ZP: 44 mV, | Anticancer: In vitro cytotoxicity studies using A549 | |||||||
| %EE: 78.5% | JP extract: showed controlled release | Human lung adenocarcinoma cells | ||||||
| Piperin | Nanocapsule | Emulsion-diffusion | PS: 168.2 nm | Drug release: sustained release | In vitro (tested for growth inhibition study in axenic culture for 3 days) | Antitrypanosomal | Piperine-nanocapsule showed a safer index of safety against horse peripheral blood mononuclear cells (PBMC) compared to pure piperine. | [59] |
| ZP: −20.3 mV | IC50 PNCs 5,04 uM; IC50 piperin 14,45 uM | |||||||
| PDI: 0.265 | ||||||||
| Argyreia pierreana ethanolic crude extract (APEECE) | Mixed Micelles | Film dispersion | PS: 163 ± 10 nm | Type 2 diabetes induced rats using a high-fat diet (HFD) and low-dose (35 mg/kg) streptozotocin (STZ) injection | Antidiabetic and antihyperlipidemic | [60,61] | ||
| PDI: 0.271 ± 0.07 | dose APEECE & MDECE: 400 mg/kg | |||||||
| Matelea denticulata ethanolic crude extract (MDECE) | PS: 145 ± 8 nm | Dose APEECE-Micelles & MDECE-Micelles: 200 mg/kg | ||||||
| PDI: 0.226 ± 0.08 | ||||||||
| Curcumin | Chitosan/PEG blended PLGA nanoparticles | Emulsion solvent evaporation | PS: 264 nm | Apoptosis analysis: Annexin V assay by flow cytometer | Pancreatic cancer | [61] | ||
| PDI: 0.181 | ||||||||
| ZP: 19.1 mV | ||||||||
| %EE: 60% |
3.1. Phytosomes Increasing the Activity of Phytochemical Compounds
3.2. Polymeric Nanoparticle to Increase the Activity of Phytochemical Compounds
4. Challenges of Phytochemical Formulations via Nanotechnology
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ijaz, S.; Akhtar, N.; Khan, M.S.; Hameed, A.; Irfan, M.; Arshad, M.A.; Ali, S.; Asrar, M. Plant Derived Anticancer Agents: A Green Approach towards Skin Cancers. Biomed. Pharmacother. 2018, 103, 1643–1651. [Google Scholar] [CrossRef] [PubMed]
- Enrico, C. Nanotechnology-Based Drug Delivery of Natural Compounds and Phytochemicals for the Treatment of Cancer and Other Diseases. In Studies in Natural Products Chemistry; Elsevier: Amsterdam, The Netherlands, 2019; Volume 62. [Google Scholar]
- Martins-Gomes, C.; Souto, E.B.; Silva, A.M. Nanophytosomes: A Novel Approach for the Delivery of Herbal Drugs. In Systems of Nanovesicular Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2022; pp. 239–257. [Google Scholar]
- Hussein, R.A.; El-Anssary, A.A. Plants Secondary Metabolites: The Key Drivers of the Pharmacological Actions of Medicinal Plants. In Herbal Medicine; IntechOpen: London, UK, 2019. [Google Scholar]
- Mendoza, N.; Silva, E.M.E. Introduction to Phytochemicals: Secondary Metabolites from Plants with Active Principles for Pharmacological Importance. In Phytochemicals-Source of Antioxidants and Role in Disease Prevention; InTech: London, UK, 2018. [Google Scholar]
- Ahmed, H.M.; Nabavi, S.; Behzad, S. Herbal Drugs and Natural Products in the Light of Nanotechnology and Nanomedicine for Developing Drug Formulations. Mini-Rev. Med. Chem. 2020, 21, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, H.M. Ethnopharmacobotanical Study on the Medicinal Plants Used by Herbalists in Sulaymaniyah Province, Kurdistan, Iraq. J. Ethnobiol. Ethnomed. 2016, 12, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Su, R.; Nie, S.; Sun, M.; Zhang, J.; Wu, D.; Moustaid-Moussa, N. Application of Nanotechnology in Improving Bioavailability and Bioactivity of Diet-Derived Phytochemicals. J. Nutr. Biochem. 2014, 25, 363–376. [Google Scholar] [CrossRef] [PubMed]
- Gunasekaran, T.; Haile, T.; Nigusse, T.; Dhanaraju, M.D. Nanotechnology: An Effective Tool for Enhancing Bioavailability and Bioactivity of Phytomedicine. Asian Pac. J. Trop Biomed. 2014, 4, S1–S7. [Google Scholar] [CrossRef]
- Saraf, S.A. Applications of Novel Drug Delivery System for Herbal Formulations. Fitoterapia 2010, 81, 680–689. [Google Scholar] [CrossRef]
- Singh, V.K.; Arora, D.; Ansari, M.I.; Sharma, P.K. Phytochemicals Based Chemopreventive and Chemotherapeutic Strategies and Modern Technologies to Overcome Limitations for Better Clinical Applications. Phytother. Res. 2019, 33, 3064–3089. [Google Scholar] [CrossRef]
- Zhou, Y.X.; Zhang, H.; Peng, C. Puerarin: A Review of Pharmacological Effects. Phytother. Res. 2014, 28, 961–975. [Google Scholar] [CrossRef]
- Quan, D.Q.; Xu, G.X.; Wu, X.G. Studies on Preparation and Absolute Bioavailability of a Self-Emulsifying System Containing Puerarin. Chem. Pharm. Bull 2007, 55, 800–803. [Google Scholar] [CrossRef]
- Li, H.; Dong, L.; Liu, Y.; Wang, G.; Wang, G.; Qiao, Y. Biopharmaceutics Classification of Puerarin and Comparison of Perfusion Approaches in Rats. Int. J. Pharm. 2014, 466, 133–138. [Google Scholar] [CrossRef]
- Luo, C.F.; Yuan, M.; Chen, M.S.; Liu, S.M.; Zhu, L.; Huang, B.Y.; Liu, X.W.; Xiong, W. Pharmacokinetics, Tissue Distribution and Relative Bioavailability of Puerarin Solid Lipid Nanoparticles Following Oral Administration. Int. J. Pharm. 2011, 410, 138–144. [Google Scholar] [CrossRef]
- Luo, C.F.; Hou, N.; Tian, J.; Yuan, M.; Liu, S.M.; Xiong, L.G.; Luo, J.D.; Chen, M.S. Metabolic Profile of Puerarin in Rats after Intragastric Administration of Puerarin Solid Lipid Nanoparticles. Int. J. Nanomed. 2013, 8, 933–940. [Google Scholar] [CrossRef]
- Bonifácio, B.V.; da Silva, P.B.; Aparecido dos Santos Ramos, M.; Maria Silveira Negri, K.; Maria Bauab, T.; Chorilli, M. Nanotechnology-Based Drug Delivery Systems and Herbal Medicines: A Review. Int. J. Nanomed. 2013, 9, 1–15. [Google Scholar]
- Ambwani, S.; Tandon, R.; Ambwani, T.K.; Malik, Y.S. Current Knowledge on Nanodelivery Systems and their beneficial Applications in Enhancing the Efficacy of Herbal Drugs. J. Exp. Biol. Agric. Sci. 2018, 6, 87–107. [Google Scholar] [CrossRef]
- Sandhiya, V.; Ubaidulla, U. A Review on Herbal Drug Loaded into Pharmaceutical Carrier Techniques and Its Evaluation Process. Futur. J. Pharm. Sci. 2020, 6, 1–16. [Google Scholar] [CrossRef]
- Souto, E.B.; Sampaio, A.C.; Campos, J.R.; Martins-Gomes, C.; Aires, A.; Silva, A.M. Polyphenols for Skin Cancer: Chemical Properties, Structure-Related Mechanisms of Action and New Delivery Systems. In Studies in Natural Products Chemistry; Elsevier: Amsterdam, The Netherlands, 2019; Volume 63. [Google Scholar]
- Karaś, M.; Jakubczyk, A.; Szymanowska, U.; Złotek, U.; Zielińska, E. Digestion and Bioavailability of Bioactive Phytochemicals. Int. J. Food Sci. Technol. 2017, 52, 291–305. [Google Scholar] [CrossRef]
- Fangueiro, J.F.; Souto, E.B.; Silva, A.M. Encapsulation of Nutraceuticals in Novel Delivery Systems. In Nutraceuticals; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar]
- Mathur, M. Herbal Medicines and Their Improvement through Novel Drug Delivery System. Asian Agri-Hist. 2014, 18, 249–256. [Google Scholar]
- Souto, E.B.; Dias-Ferreira, J.; Oliveira, J.; Sanchez-Lopez, E.; Lopez-Machado, A.; Espina, M.; Garcia, M.L.; Souto, S.B.; Martins-Gomes, C.; Silva, A.M. Trends in Atopic Dermatitis—From Standard Pharmacotherapy to Novel Drug Delivery Systems. Int. J. Mol. Sci. 2019, 20, 5659. [Google Scholar] [CrossRef]
- Paroha, S.; Dewangan, R.P.; Sahoo, P.K. Pharmaceutical Technology for Improving the Bioavailability of Natural Products. In Sustainable Agriculture Reviews 43; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Mukherjee, P.K.; Harwansh, R.K.; Bhattacharyya, S. Bioavailability of Herbal Products: Approach Toward Improved Pharmacokinetics. In Evidence-Based Validation of Herbal Medicine; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Tapadiya, G.G.; Kale, M.A.; Saboo, S.S. Impact of Nanotechnology on Global Trade of Herbal Drugs: An Overview. Int. J. Green Pharm. 2017, 11, S371–S376. [Google Scholar]
- Jain, S.; Jain, V.; Mahajan, S.C. Lipid Based Vesicular Drug Delivery Systems. Adv. Pharm. 2014, 2014, 574673. [Google Scholar] [CrossRef]
- Sakellari, G.I.; Zafeiri, I.; Batchelor, H.; Spyropoulos, F. Formulation Design, Production and Characterisation of Solid Lipid Nanoparticles (SLN) and Nanostructured Lipid Carriers (NLC) for the Encapsulation of a Model Hydrophobic Active. Food Hydrocoll. Health 2021, 1, 100024. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Bishnoi, R.S.; Shukla, A.K.; Jain, C.P. Techniques for Formulation of Nanoemulsion Drug Delivery System: A Review. Prev. Nutr. Food Sci. 2019, 24, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Németh, Z.; Pallagi, E.; Dobó, D.G.; Kozma, G.; Kónya, Z.; Csóka, I. An Updated Risk Assessment as Part of the QbD-Based Liposome Design and Development. Pharmaceutics 2021, 13, 1071. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Castro Bravo, K.M.; Liu, J. Targeted Liposomal Drug Delivery: A Nanoscience and Biophysical Perspective. Nanoscale Horiz. 2021, 6, 78–94. [Google Scholar] [CrossRef] [PubMed]
- Chavda, V.P.; Vihol, D.; Mehta, B.; Shah, D.; Patel, M.; Vora, L.K.; Pereira-Silva, M.; Paiva-Santos, A.C. Phytochemical-Loaded Liposomes for Anticancer Therapy: An Updated Review. Nanomedicine 2022, 17, 547–568. [Google Scholar] [CrossRef]
- Kyriakoudi, A.; Spanidi, E.; Mourtzinos, I.; Gardikis, K. Innovative Delivery Systems Loaded with Plant Bioactive Ingredients: Formulation Approaches and Applications. Plants 2021, 10, 1238. [Google Scholar] [CrossRef]
- Su, W.; Liang, Y.; Meng, Z.; Chen, X.; Lu, M.; Han, X.; Deng, X.; Zhang, Q.; Zhu, H.; Fu, T. Inhalation of Tetrandrine-Hydroxypropyl-β-Cyclodextrin Inclusion Complexes for Pulmonary Fibrosis Treatment. Mol. Pharm. 2020, 17, 1596–1607. [Google Scholar] [CrossRef]
- Zhang, L.; Yang, S.; Wong, L.R.; Xie, H.; Ho, P.C.-L. In Vitro and in Vivo Comparison of Curcumin-Encapsulated Chitosan-Coated Poly (Lactic- Co-Glycolic Acid) Nanoparticles and Curcumin/Hydroxypropyl-β-Cyclodextrin Inclusion Complexes Administered Intranasally as Therapeutic Strategies for Alzheimer’s Disease. Mol. Pharm. 2020, 17, 4256–4269. [Google Scholar] [CrossRef]
- Blasi, P.; Giovagnoli, S.; Schoubben, A.; Ricci, M.; Rossi, C. Solid Lipid Nanoparticles for Targeted Brain Drug Delivery. Adv. Drug Deliv. Rev. 2007, 59, 454–477. [Google Scholar] [CrossRef]
- Song, J.-W.; Liu, Y.-S.; Guo, Y.-R.; Zhong, W.-X.; Guo, Y.-P.; Guo, L. Nano–Liposomes Double Loaded with Curcumin and Tetrandrine: Preparation, Characterization, Hepatotoxicity and Anti–Tumor Effects. Int. J. Mol. Sci. 2022, 23, 6858. [Google Scholar] [CrossRef]
- Souto, E.B.; Fernandes, A.R.; Martins-Gomes, C.; Coutinho, T.E.; Durazzo, A.; Lucarini, M.; Souto, S.B.; Silva, A.M.; Santini, A. Nanomaterials for Skin Delivery of Cosmeceuticals and Pharmaceuticals. Appl. Sci. 2020, 10, 1594. [Google Scholar] [CrossRef]
- Li, A.; Tyson, J.; Patel, S.; Patel, M.; Katakam, S.; Mao, X.; He, W. Emerging Nanotechnology for Treatment of Alzheimer’s and Parkinson’s Disease. Front. Bioeng. Biotechnol. 2021, 9, 322. [Google Scholar] [CrossRef]
- Liechty, W.B.; Kryscio, D.R.; Slaughter, B.v.; Peppas, N.A. Polymers for Drug Delivery Systems. Annu. Rev. Chem. Biomol. Eng. 2010, 1, 149–173. [Google Scholar] [CrossRef]
- Siegal, T. Which Drug or Drug Delivery System Can Change Clinical Practice for Brain Tumor Therapy? Neuro Oncol. 2013, 15, 656–669. [Google Scholar] [CrossRef]
- Preethi, R.; Dutta, S.; Moses, J.A.; Anandharamakrishnan, C. Green Nanomaterials and Nanotechnology for the Food Industry. In Green Functionalized Nanomaterials for Environmental Applications; Elsevier: Amsterdam, The Netherlands, 2022; pp. 215–256. [Google Scholar]
- Lu, H.; Zhang, S.; Wang, J.; Chen, Q. A Review on Polymer and Lipid-Based Nanocarriers and Its Application to Nano-Pharmaceutical and Food-Based Systems. Front. Nutr. 2021, 8. [Google Scholar] [CrossRef]
- Pyo, S.M.; Müller, R.H.; Keck, C.M. Encapsulation by Nanostructured Lipid Carriers. In Nanoencapsulation Technologies for the Food and Nutraceutical Industries; Academic Press: Cambridge, MA, USA, 2017. [Google Scholar]
- Barani, M.; Sangiovanni, E.; Angarano, M.; Rajizadeh, M.A.; Mehrabani, M.; Piazza, S.; Gangadharappa, H.V.; Pardakhty, A.; Mehrbani, M.; Dell’agli, M.; et al. Phytosomes as Innovative Delivery Systems for Phytochemicals: A Comprehensive Review of Literature. Int. J. Nanomed. 2021, 16, 6983–7022. [Google Scholar] [CrossRef]
- Bhattacharya, S. Phytosomes: The New Technology for Enhancement of Bioavailability of Botanicals and Nutraceuticals. Int. J. Health Res. 2009, 2, 225–232. [Google Scholar] [CrossRef]
- Kidd, P.; Head, K. A Review of the Bioavailability and Clinical Efficacy of Milk Thistle Phytosome: A Silybin-Phosphatidylcholine Complex (Siliphos®). Altern. Med. Rev. 2005, 10, 193–203. [Google Scholar]
- Mazumder, A.; Dwivedi, A.; du Preez, J.L.; du Plessis, J. In Vitro Wound Healing and Cytotoxic Effects of Sinigrin-Phytosome Complex. Int. J. Pharm. 2016, 498, 283–293. [Google Scholar] [CrossRef]
- Kumar, S.; Baldi, A.; Sharma, D.K. In Vitro Antioxidant Assay Guided Ex Vivo Investigation of Cytotoxic Effect of Phytosomes Assimilating Taxifolin Rich Fraction of Cedrus Deodara Bark Extract on Human Breast Cancer Cell Lines (MCF7). J. Drug Deliv. Sci. Technol. 2021, 63, 102486. [Google Scholar] [CrossRef]
- Chi, C.; Zhang, C.; Liu, Y.; Nie, H.; Zhou, J.; Ding, Y. Phytosome-Nanosuspensions for Silybin-Phospholipid Complex with Increased Bioavailability and Hepatoprotection Efficacy. Eur. J. Pharm. Sci. 2020, 144, 105212. [Google Scholar] [CrossRef] [PubMed]
- Telange, D.R.; Patil, A.T.; Pethe, A.M.; Fegade, H.; Anand, S.; Dave, V.S. Formulation and Characterization of an Apigenin-Phospholipid Phytosome (APLC) for Improved Solubility, in Vivo Bioavailability, and Antioxidant Potential. Eur. J. Pharm. Sci. 2017, 108, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Fattah, A.I.; Fathy, M.M.; Ali, Z.Y.; El-Garawany, A.E.R.A.; Mohamed, E.K. Enhanced Therapeutic Benefit of Quercetin-Loaded Phytosome Nanoparticles in Ovariectomized Rats. Chem. Biol. Interact 2017, 271, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Gangadharappa, H.V.; Mruthunjaya, K. Phytosome Complexed with Chitosan for Gingerol Delivery in the Treatment of Respiratory Infection: In Vitro and in Vivo Evaluation. Eur. J. Pharm. Sci. 2018, 122, 214–229. [Google Scholar] [CrossRef] [PubMed]
- Lim, A.W.; Ng, P.Y.; Chieng, N.; Ng, S.F. Moringa Oleifera Leaf Extract–Loaded Phytophospholipid Complex for Potential Application as Wound Dressing. J. Drug. Deliv. Sci. Technol. 2019, 54, 101329. [Google Scholar] [CrossRef]
- Chime, S.A.; Akpa, P.A.; Onyishi, I.V.; Ezenduka, D.E. Phytosomes Enhanced The Antibacterial And Antifungal Properties of Lantana Camara. Innovare J. Ayurvedic Sci. 2020, 8, 1–5. [Google Scholar]
- Rani, A.; Kumar, S.; Khar, R.K. Murraya Koenigii Extract Loaded Phytosomes Prepared Using Antisolvent Precipitation Technique for Improved Antidiabetic and Hypolidemic Activity. Indian J. Pharm. Educ. Res. 2022, 56, s326–s338. [Google Scholar] [CrossRef]
- Alqahtani, M.S.; Al-Yousef, H.M.; Alqahtani, A.S.; Tabish Rehman, M.; AlAjmi, M.F.; Almarfidi, O.; Amina, M.; Alshememry, A.; Syed, R. Preparation, Characterization, and in Vitro-in Silico Biological Activities of Jatropha Pelargoniifolia Extract Loaded Chitosan Nanoparticles. Int. J. Pharm. 2021, 606, 120867. [Google Scholar] [CrossRef]
- Rani, R.; Kumar, S.; Dilbaghi, N.; Kumar, R. Nanotechnology Enabled the Enhancement of Antitrypanosomal Activity of Piperine against Trypanosoma Evansi. Exp. Parasitol. 2020, 219, 108018. [Google Scholar] [CrossRef]
- Gudise, V.; Chowdhury, B.; Manjappa, A.S. Antidiabetic and Antihyperlipidemic Effects of Argyreia Pierreana and Matelea Denticulata: Higher Activity of the Micellar Nanoformulation over the Crude Extract. J. Tradit. Complement. Med. 2021, 11, 259–267. [Google Scholar] [CrossRef]
- Arya, G.; Das, M.; Sahoo, S.K. Evaluation of Curcumin Loaded Chitosan/PEG Blended PLGA Nanoparticles for Effective Treatment of Pancreatic Cancer. Biomed. Pharmacother. 2018, 102, 555–566. [Google Scholar] [CrossRef]
- Jie, M.; Cheung, W.M.; Yu, V.; Zhou, Y.; Tong, P.H.; Ho, J.W.S. Anti-Proliferative Activities of Sinigrin on Carcinogen-Induced Hepatotoxicity in Rats. PLoS ONE 2014, 9, e110145. [Google Scholar] [CrossRef]
- Weidmann, A.E. Dihydroquercetin: More than Just an Impurity? Eur. J. Pharmacol. 2012, 684, 19–26. [Google Scholar] [CrossRef]
- Luo, H.; Jiang, B.H.; King, S.M.; Chen, Y.C. Inhibition of Cell Growth and VEGF Expression in Ovarian Cancer Cells by Flavonoids. Nutr. Cancer 2008, 60, 800–809. [Google Scholar] [CrossRef]
- Hasibi, F.; Nasirpour, A.; Varshosaz, J.; García-Manrique, P.; Blanco-López, M.C.; Gutiérrez, G.; Matos, M. Formulation and Characterization of Taxifolin-Loaded Lipid Nanovesicles (Liposomes, Niosomes, and Transfersomes) for Beverage Fortification. Eur. J. Lipid Sci. Technol. 2020, 122. [Google Scholar] [CrossRef]
- Mondal, R.; Bobde, Y.; Ghosh, B.; Giri, T.K. Development and Characterization of a Phospholipid Complex for Effective Delivery of Capsaicin. Indian J. Pharm. Sci. 2019, 81, 1011–1019. [Google Scholar] [CrossRef]
- Theodosiou, E.; Purchartová, K.; Stamatis, H.; Kolisis, F.; Křen, V. Bioavailability of Silymarin Flavonolignans: Drug Formulations and Biotransformation. Phytochem. Rev. 2014, 13, 1–18. [Google Scholar] [CrossRef]
- Shukla, S.; Gupta, S. Apigenin: A Promising Molecule for Cancer Prevention. Pharm. Res. 2010, 27, 962–978. [Google Scholar] [CrossRef]
- Rithidech, K.N.; Tungjai, M.; Reungpatthanaphong, P.; Honikel, L.; Simon, S.R. Attenuation of Oxidative Damage and Inflammatory Responses by Apigenin given to Mice after Irradiation. Mutat. Res. Genet. Toxicol. Environ. Mutagen. 2012, 749, 29–38. [Google Scholar] [CrossRef]
- Shibata, C.; Ohno, M.; Otsuka, M.; Kishikawa, T.; Goto, K.; Muroyama, R.; Kato, N.; Yoshikawa, T.; Takata, A.; Koike, K. The Flavonoid Apigenin Inhibits Hepatitis C Virus Replication by Decreasing Mature MicroRNA122 Levels. Virology 2014, 462–463, 42–48. [Google Scholar] [CrossRef]
- Choi, J.S.; Nurul Islam, M.; Yousof Ali, M.; Kim, E.J.; Kim, Y.M.; Jung, H.A. Effects of C-Glycosylation on Anti-Diabetic, Anti-Alzheimer’s Disease and Anti-Inflammatory Potential of Apigenin. Food Chem. Toxicol. 2014, 64, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Liu, D.; Huang, Y.; Gao, Y.; Qian, S. Biopharmaceutics Classification and Intestinal Absorption Study of Apigenin. Int. J. Pharm. 2012, 436, 311–317. [Google Scholar] [CrossRef]
- Chen, Z.; Kong, S.; Song, F.; Li, L.; Jiang, H. Pharmacokinetic Study of Luteolin, Apigenin, Chrysoeriol and Diosmetin after Oral Administration of Flos Chrysanthemi Extract in Rats. Fitoterapia 2012, 83, 1616–1622. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.P.; Chien, M.H. Phytoestrogens Induce Differential Effects on Both Normal and Malignant Human Breast Cells in Vitro. Climacteric 2014, 17, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Cury Rodrigues, M.F.; Stotzer, U.S.; Domingos, M.M.; Deminice, R.; Shiguemoto, G.E.; Tomaz, L.M.; de Sousa, N.M.F.; Ferreira, F.C.; Leite, R.D.; Selistre-de-Araújo, H.S.; et al. Effects of Ovariectomy and Resistance Training on Oxidative Stress Markers in the Rat Liver. Clinics 2013, 68, 1247–1254. [Google Scholar] [CrossRef]
- Rahmani, A.H.; al Shabrmi, F.M.; Aly, S.M. Active Ingredients of Ginger as Potential Candidates in the Prevention and Treatment of Diseases via Modulation of Biological Activities. Int. J. Physiol. Pathophysiol. Pharmacol. 2014, 6, 125–136. [Google Scholar]
- Singh, R.P.; Gangadharappa, H.V.; Narke, R.M.; Jadhav, P.V. Stability-Indicating rp-hplc Method Development for the Estimation of Gingerol. Int. Res. J. Pharm. 2017, 8, 56–61. [Google Scholar] [CrossRef]
- Kubra, I.R.; Jaganmohanrao, L. An Overview on Inventions Related to Ginger Processing and Products for Food and Pharmaceutical Applications. Recent Pat. Food Nutr. Agric. 2012, 4, 31–49. [Google Scholar] [CrossRef]
- Muhammad, A.A.; Pauzi, N.A.S.; Arulselvan, P.; Abas, F.; Fakurazi, S. In Vitro Wound Healing Potential and Identification of Bioactive Compounds from Moringa Oleifera Lam. Biomed. Res. Int. 2013, 2013, 1–10. [Google Scholar] [CrossRef]
- Chin, C.Y.; Jalil, J.; Ng, P.Y.; Ng, S.F. Development and Formulation of Moringa Oleifera Standardised Leaf Extract Film Dressing for Wound Healing Application. J. Ethnopharmacol. 2018, 212, 188–199. [Google Scholar] [CrossRef]
- Waterman, C.; Cheng, D.M.; Rojas-Silva, P.; Poulev, A.; Dreifus, J.; Lila, M.A.; Raskin, I. Stable, Water Extractable Isothiocyanates from Moringa Oleifera Leaves Attenuate Inflammation in Vitro. Phytochemistry 2014, 103, 114–122. [Google Scholar] [CrossRef]
- Bagdas, D.; Etoz, B.C.; Gul, Z.; Ziyanok, S.; Inan, S.; Turacozen, O.; Gul, N.Y.; Topal, A.; Cinkilic, N.; Tas, S.; et al. In Vivo Systemic Chlorogenic Acid Therapy under Diabetic Conditions: Wound Healing Effects and Cytotoxicity/Genotoxicity Profile. Food Chem. Toxicol. 2015, 81, 54–61. [Google Scholar] [CrossRef]
- Gopalakrishnan, A.; Ram, M.; Kumawat, S.; Tandan, S.K.; Kumar, D. Quercetin Accelerated Cutaneous Wound Healing in Rats by Increasing Levels of VEGF and TGF-Β1. Indian J. Exp. Biol. 2016, 54, 187–195. [Google Scholar]
- Muhammad, A.A.; Arulselvan, P.; Cheah, P.S.; Abas, F.; Fakurazi, S. Evaluation of Wound Healing Properties of Bioactive Aqueous Fraction from Moringa Oleifera Lam on Experimentally Induced Diabetic Animal Model. Drug Des. Dev. Ther. 2016, 10, 1715–1730. [Google Scholar] [CrossRef]
- Yang, C.S.; Sang, S.; Lambert, J.D.; Lee, M.J. Bioavailability Issues in Studying the Health Effects of Plant Polyphenolic Compounds. Mol. Nutr. Food Res. 2008, 52, S139–S151. [Google Scholar] [CrossRef]
- Kalita, S.; Kumar, G.; Karthik, L.; Rao, K.V.B. A Review on Medicinal Properties of Lantana Camara Linn. Res. J. Pharm. Technol. 2012, 5, 711–715. [Google Scholar]
- Yankuzo, H.; Ahmed, Q.U.; Santosa, R.I.; Akter, S.F.U.; Talib, N.A. Beneficial Effect of the Leaves of Murraya Koenigii (Linn.) Spreng (Rutaceae) on Diabetes-Induced Renal Damage in Vivo. J. Ethnopharmacol. 2011, 135, 88–94. [Google Scholar] [CrossRef]
- Ferreira, C.; Soares, D.C.; Barreto-Junior, C.B.; Nascimento, M.T.; Freire-De-Lima, L.; Delorenzi, J.C.; Lima, M.E.F.; Atella, G.C.; Folly, E.; Carvalho, T.M.U.; et al. Leishmanicidal Effects of Piperine, Its Derivatives, and Analogues on Leishmania Amazonensis. Phytochemistry 2011, 72, 2155–2164. [Google Scholar] [CrossRef]
- Gorgani, L.; Mohammadi, M.; Najafpour, G.D.; Nikzad, M. Piperine—The Bioactive Compound of Black Pepper: From Isolation to Medicinal Formulations. Compr. Rev. Food Sci. Food Saf. 2017, 16, 124–140. [Google Scholar] [CrossRef]
- Pachauri, M.; Gupta, E.D.; Ghosh, P.C. Piperine Loaded PEG-PLGA Nanoparticles: Preparation, Characterization and Targeted Delivery for Adjuvant Breast Cancer Chemotherapy. J. Drug Deliv. Sci. Technol. 2015, 29, 269–282. [Google Scholar] [CrossRef]
- Zhu, J.Y.; Zhang, C.Y.; Dai, J.J.; Rahman, K.; Zhang, H. Diterpenoids with Thioredoxin Reductase Inhibitory Activities from Jatropha Multifida. Nat. Prod. Res. 2017, 31, 2753–2758. [Google Scholar] [CrossRef] [PubMed]
- Teng, Z.; Yuan, C.; Zhang, F.; Huan, M.; Cao, W.; Li, K.; Yang, J.; Cao, D.; Zhou, S.; Mei, Q. Intestinal Absorption and First-Pass Metabolism of Polyphenol Compounds in Rat and Their Transport Dynamics in Caco-2 Cells. PLoS ONE 2012, 7, e29647. [Google Scholar] [CrossRef] [PubMed]
- Karakaya, S. Bioavailability of Phenolic Compounds. Crit. Rev. Food Sci. Nutr. 2004, 44, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Manach, C.; Williamson, G.; Morand, C.; Scalbert, A.; Rémésy, C. Bioavailability and Bioefficacy of Polyphenols in Humans. I. Review of 97 Bioavailability Studies. Am. J. Clin. Nutr. 2005, 81, 230S–242S. [Google Scholar] [CrossRef] [PubMed]
- Manjappa, A.S.; Kumbhar, P.S.; Patil, A.B.; Disouza, J.I.; Patravale, V.B. Polymeric Mixed Micelles: Improving the Anticancer Efficacy of Single-Copolymer Micelles. Crit. Rev. Ther. Drug Carrier Syst. 2019, 36, 1–58. [Google Scholar] [CrossRef] [PubMed]
- Srinivasan, S.; Pari, L. Antihyperlipidemic Effect of Diosmin: A Citrus Flavonoid on Lipid Metabolism in Experimental Diabetic Rats. J. Funct. Foods 2013, 5, 484–492. [Google Scholar] [CrossRef]
- Touiss, I.; Khatib, S.; Bekkouch, O.; Amrani, S.; Harnafi, H. Phenolic Extract from Ocimum Basilicum Restores Lipid Metabolism in Triton WR-1339-Induced Hyperlipidemic Mice and Prevents Lipoprotein-Rich Plasma Oxidation. Food Sci. Hum. Wellness 2017, 6, 28–33. [Google Scholar] [CrossRef]
- Subedi, L.; Timalsena, S.; Duwadi, P.; Thapa, R.; Paudel, A.; Parajuli, K. Antioxidant Activity and Phenol and Flavonoid Contents of Eight Medicinal Plants from Western Nepal. J. Tradit. Chin. Med. 2014, 34, 584–590. [Google Scholar] [CrossRef]
- Wojdyło, A.; Nowicka, P.; Carbonell-Barrachina, Á.A.; Hernández, F. Phenolic Compounds, Antioxidant and Antidiabetic Activity of Different Cultivars of Ficus Carica L. Fruits. J. Funct. Foods 2016, 25, 421–432. [Google Scholar] [CrossRef]
- Giordano; Tommonaro Curcumin and Cancer. Nutrients 2019, 11, 2376. [CrossRef]
- Bimonte, S.; Barbieri, A.; Palma, G.; Luciano, A.; Rea, D.; Arra, C. Curcumin Inhibits Tumor Growth and Angiogenesis in an Orthotopic Mouse Model of Human Pancreatic Cancer. Biomed. Res. Int. 2013, 2013, 810423. [Google Scholar] [CrossRef]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of Curcumin: Problems and Promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef]
- Panzarini, E.; Mariano, S.; Tacconi, S.; Carata, E.; Tata, A.M.; Dini, L. Novel Therapeutic Delivery of Nanocurcumin in Central Nervous System Related Disorders. Nanomaterials 2020, 11, 2. [Google Scholar] [CrossRef]
- Arifin, S.F.; Al-Shami, A.K.; Omar, S.S.S.; Jalil, M.A.A.; Khalid, K.A.; Hadi, H. Impact of Modern Technology on the Development of Natural-Based Products. J. Ayurvedic Herb. Med. 2019, 5, 133–142. [Google Scholar] [CrossRef]
- Singla, A.K.; Garg, A.; Aggarwal, D. Paclitaxel and Its Formulations. Int. J. Pharm. 2002, 235, 179–192. [Google Scholar] [CrossRef]
- Kiss, L.; Walter, F.R.; Bocsik, A.; Veszelka, S.; Ózsvári, B.; Puskás, L.G.; Szabó-Révész, P.; Deli, M.A. Kinetic Analysis of the Toxicity of Pharmaceutical Excipients Cremophor EL and RH40 on Endothelial and Epithelial Cells. J. Pharm. Sci. 2013, 102, 1173–1181. [Google Scholar] [CrossRef]
- Venditto, V.J.; Szoka, F.C. Cancer Nanomedicines: So Many Papers and so Few Drugs! Adv. Drug. Deliv. Rev. 2013, 65, 80–88. [Google Scholar] [CrossRef]
- Jones, T.; Saba, N. Nanotechnology and Drug Delivery: An Update in Oncology. Pharmaceutics 2011, 3, 171–185. [Google Scholar] [CrossRef]
- Jin, Y.; Wen, J.; Garg, S.; Liu, D.; Zhou, Y.; Teng, L.; Zhang, W. Development of a Novel Niosomal System for Oral Delivery of Ginkgo Biloba Extract. Int. J. Nanomed. 2013, 8, 421–430. [Google Scholar] [CrossRef]
- Drago, F.; Floriddia, M.L.; Cro, M.; Giuffrida, S. Pharmacokinetics and Bioavailability of a Ginkgo Biloba Extract. J. Ocul. Pharmacol. Ther. 2002, 18, 197–202. [Google Scholar] [CrossRef]
- Devaraj, G.N.; Parakh, S.R.; Devraj, R.; Apte, S.S.; Rao, B.R.; Rambhau, D. Release Studies on Niosomes Containing Fatty Alcohols as Bilayer Stabilizers Instead of Cholesterol. J. Colloid. Interface Sci. 2002, 251, 360–365. [Google Scholar] [CrossRef] [PubMed]
- Yeo, Y. Nanoparticulate Drug Delivery Systems: Strategies, Technologies, and Applications; Wiley: Hoboken, NJ, USA, 2013; ISBN 9781118148877. [Google Scholar]
- Bosetti, R. Cost–Effectiveness of Nanomedicine: The Path to a Future Successful and Dominant Market? Nanomedicine 2015, 10, 1851–1853. [Google Scholar]


| Lipid-Based Nanocarrier | Composition | Structure | Application | Administration |
|---|---|---|---|---|
| Liposome | Phospholipid and cholesterol | Rigid | Drug (synthetic and naturally derived) and gene therapy | Oral, parenteral, topical, and transdermal |
| Phytosome | Phospholipid and polyphenolic phytoconstituents | Rigid | Phyto delivery | Oral, parenteral, topical, and transdermal |
| Transfersome | Phospholipid and surfactant | Ultra-deformable | Skin delivery | Topical and transdermal |
| Niosome | Nonionic surfactant and cholesterol | Rigid | Drug (synthetic and naturally derived) delivery and cosmetics | Oral, parenteral, topical, and transdermal |
| Ethosome | Phospholipid, alcohol, polyglycol, and water | Elasticity | Skin delivery | Topical and transdermal |
| SLN | Solid lipid | Ordered | Drug (synthetic and naturally derived), gene therapy, and cosmetics | Oral, parenteral, topical, and transdermal |
| NLC | Solid lipid and liquid lipid | Less ordered | Drug (synthetic and naturally derived), gene therapy, and cosmetics | Oral, parenteral, topical, and transdermal |
| Method | IC50 | ||
|---|---|---|---|
| Gingerol | GP | GPLC | |
| DPPH assay | 57.74 µg/mL | 46.23 µg/mL | 17.70 µg/mL |
| H2O2 assay | 53.52 µg/mL | 40.48 µg/mL | 19.46 µg/mL |
| Organism | MIC | ||
|---|---|---|---|
| Gingerol | GP | GPLC | |
| Gram positive (S. aureus) | 400 ± 0.23 µg/mL | 200 ± 0.06 µg/mL | 100 ± 0.07 µg/mL |
| Gram Negative (E. coli) | 400 ± 0.12 µg/mL | 200 ± 0.79 µg/ml | 100 ± 0.08 µg/mL |
| Organism | IC50 | ||
|---|---|---|---|
| Gingerol | GP | GPLC | |
| Against HRBC membrane lysis | 74.68 µg/mL | 70.86 µg/mL | 59.84 µg/mL |
| Denaturation of protein | 67.03 µg/mL | 64.54 µg/mL | 61.88 µg/mL |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dewi, M.K.; Chaerunisaa, A.Y.; Muhaimin, M.; Joni, I.M. Improved Activity of Herbal Medicines through Nanotechnology. Nanomaterials 2022, 12, 4073. https://doi.org/10.3390/nano12224073
Dewi MK, Chaerunisaa AY, Muhaimin M, Joni IM. Improved Activity of Herbal Medicines through Nanotechnology. Nanomaterials. 2022; 12(22):4073. https://doi.org/10.3390/nano12224073
Chicago/Turabian StyleDewi, Mayang Kusuma, Anis Yohana Chaerunisaa, Muhaimin Muhaimin, and I Made Joni. 2022. "Improved Activity of Herbal Medicines through Nanotechnology" Nanomaterials 12, no. 22: 4073. https://doi.org/10.3390/nano12224073
APA StyleDewi, M. K., Chaerunisaa, A. Y., Muhaimin, M., & Joni, I. M. (2022). Improved Activity of Herbal Medicines through Nanotechnology. Nanomaterials, 12(22), 4073. https://doi.org/10.3390/nano12224073







