Curcumin Nanoformulations with Metal Oxide Nanomaterials for Biomedical Applications
Abstract
:1. Introduction
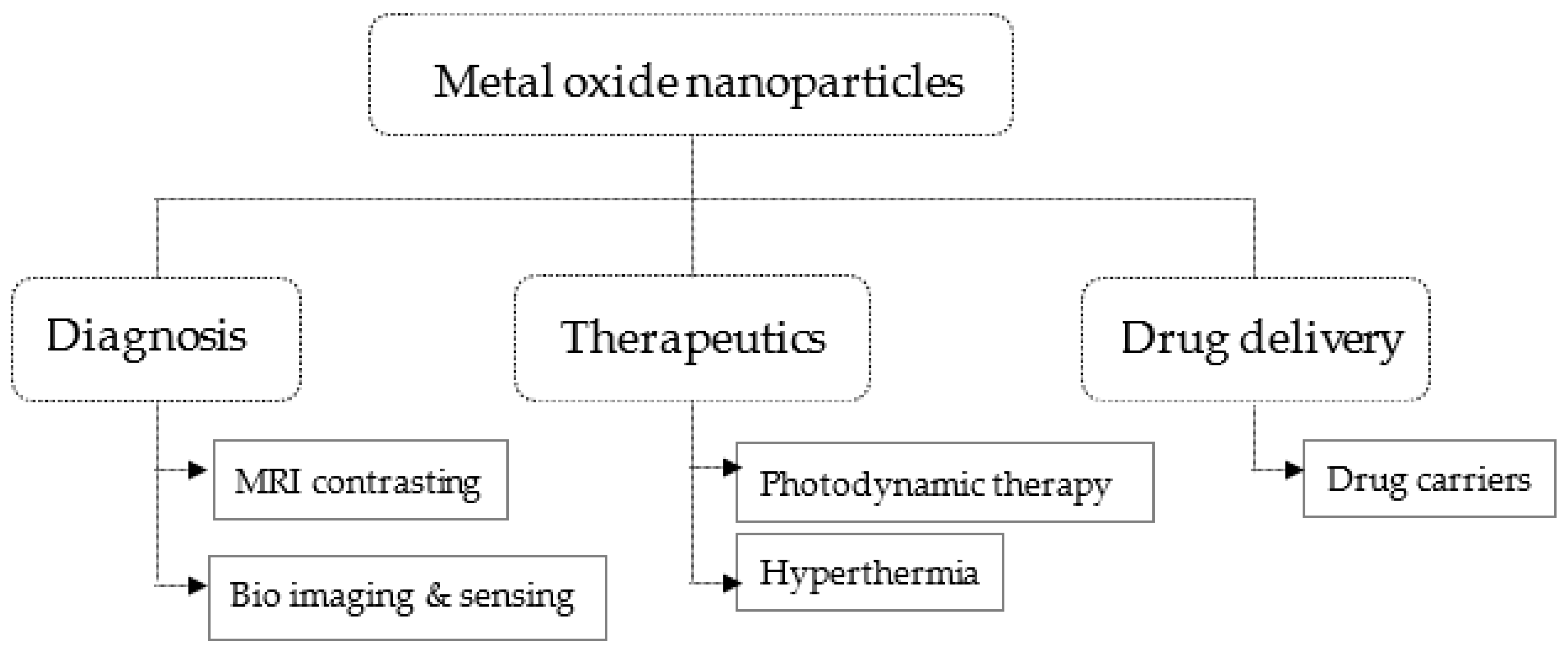
2. Features of Metal Oxides Related to Biomedical Applications
2.1. Titanium Dioxides Nanoparticles
2.2. Zinc Oxide Nanoparticles
2.3. Iron Oxide Nanoparticles
2.4. Cerium Oxide (Ceria) Nanoparticles
2.5. Copper Oxide Nanoparticles
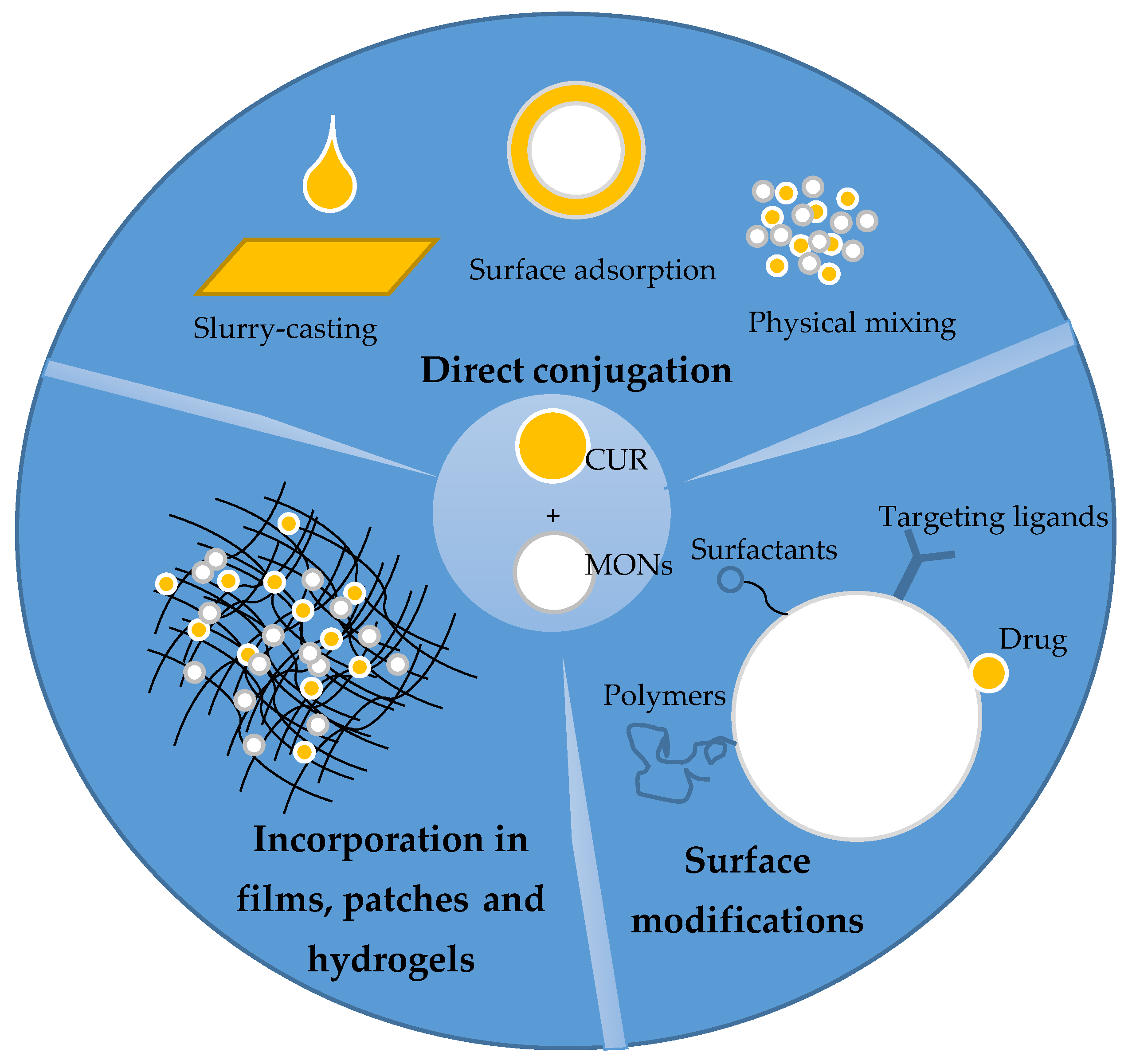
3. Metal Oxides as Curcumin Carriers
3.1. Metal Oxide–curcumin Direct Combination
3.2. Surface-Modified Metal Oxides as Curcumin Carriers
3.2.1. Targeting Ligands Modification
3.2.2. Surfactant and Other Organic and Inorganic Compounds Modification
3.3. Curcumin-Metal Oxide Incorporated Films and Patches
3.4. Curcumin-Metal Oxides Incorporated Hydrogels
3.5. Curcumin-Ameliorated Metal Oxide Toxicities
4. Concluding Remarks
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Wanninger, S.; Lorenz, V.; Subhan, A.; Edelmann, F.T. Metal complexes of curcumin—Synthetic strategies, structures and medicinal applications. Chem. Soc. Rev. 2015, 44, 4986–5002. [Google Scholar] [CrossRef] [Green Version]
- Karthikeyan, A.; Senthil, N.; Min, T. Nanocurcumin: A Promising Candidate for Therapeutic Applications. Front. Pharmacol. 2020, 11, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Sharifi, S.; Fathi, N.; Memar, M.Y.; Hosseiniyan Khatibi, S.M.; Khalilov, R.; Negahdari, R.; Zununi Vahed, S.; Maleki Dizaj, S. Anti-microbial activity of curcumin nanoformulations: New trends and future perspectives. Phyther. Res. 2020, 34, 1926–1946. [Google Scholar] [CrossRef] [PubMed]
- Moniruzzaman, M.; Min, T. Curcumin, curcumin nanoparticles and curcumin nanospheres: A review on their pharmacodynamics based on monogastric farm animal, poultry and fish nutrition. Pharmaceutics 2020, 12, 447. [Google Scholar] [CrossRef] [PubMed]
- Basnet, P.; Skalko-Basnet, N. Curcumin: An anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules 2011, 16, 4567–4598. [Google Scholar] [CrossRef] [Green Version]
- Dejonckheere MRCVS, V. Turmeric for Osteoarthritis in Veterinary Medicine: A Review. 2013, 11–16. Available online: http://www.herbalvets.org.uk/wp-content/uploads/2016/10/turmeric-dejonckheere.pdf (accessed on 9 February 2021).
- Nelson, K.M.; Dahlin, J.L.; Bisson, J.; Graham, J.; Pauli, G.F.; Walters, M.A. The Essential Medicinal Chemistry of Curcumin. J. Med. Chem. 2017, 60, 1620–1637. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, Q.; Liu, Y.; Ju, F.; Ma, Q.; He, Q. In vivo evaluation of enhanced drug carrier efficiency and cardiac anti-hypertrophy therapeutic potential of nano-curcumin encapsulated photo-plasmonic nanoparticles combined polymerized nano-vesicles: A novel strategy. J. Photochem. Photobiol. B Biol. 2019, 199. [Google Scholar] [CrossRef]
- Baldwin, P.R.; Reeves, A.Z.; Powell, K.R.; Napier, R.J.; Swimm, A.I.; Sun, A.; Giesler, K.; Bommarius, B.; Shinnick, T.M.; Snyder, J.P.; et al. Monocarbonyl analogs of curcumin inhibit growth of antibiotic sensitive and resistant strains of Mycobacterium tuberculosis. Eur. J. Med. Chem. 2015, 92, 693–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burgos-Morón, E.; Calderón-Montaño, J.M.; Salvador, J.; Robles, A.; López-Lázaro, M. The dark side of curcumin Estefanía. Int. J. Cancer 2010, 126, 1771–1775. [Google Scholar]
- Yallapu, M.M.; Jaggi, M.; Chauhan, S.C. Curcumin Nanomedicine: A Road to Cancer Therapeutics; Bentham Science Publishers: Sharjah, United Arab Emirates, 2013; Volume 19. [Google Scholar]
- Montazerabadi, A.; Beik, J.; Irajirad, R.; Attaran, N.; Khaledi, S.; Ghaznavi, H.; Shakeri-Zadeh, A. Folate-modified and curcumin-loaded dendritic magnetite nanocarriers for the targeted thermo-chemotherapy of cancer cells. Artif. Cells Nanomed. Biotechnol. 2019, 47, 330–340. [Google Scholar] [CrossRef] [Green Version]
- Yavarpour-Bali, H.; Pirzadeh, M.; Ghasemi-Kasman, M. Curcumin-loaded nanoparticles: A novel therapeutic strategy in treatment of central nervous system disorders. Int. J. Nanomed. 2019, 14, 4449–4460. [Google Scholar] [CrossRef] [Green Version]
- Kurien, B.T.; Singh, A.; Matsumoto, H.; Scofield, R.H. Improving the solubility and pharmacological efficacy of curcumin by heat treatment. Assay Drug Dev. Technol. 2007, 5, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Gomez, I.J.; Arnaiz, B.; Cacioppo, M.; Arcudi, F.; Prato, M. Nitrogen-doped Carbon Nanodots for bioimaging and delivery of paclitaxel. J. Mater. Chem. B 2018, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jakubek, M.; Kejík, Z.; Kaplánek, R.; Hromádka, R.; Šandriková, V.; Sýkora, D.; Antonyová, V.; Urban, M.; Dytrych, P.; Mikula, I.; et al. Strategy for improved therapeutic efficiency of curcumin in the treatment of gastric cancer. Biomed. Pharmacother. 2019, 118, 109278. [Google Scholar] [CrossRef] [PubMed]
- Senapati, S.; Mahanta, A.K.; Kumar, S.; Maiti, P. Controlled drug delivery vehicles for cancer treatment and their performance. Signal Transduct. Target. Ther. 2018, 3, 1–19. [Google Scholar] [CrossRef] [Green Version]
- Naz, S.; Shamoon, M.; Wang, R.; Zhang, L.; Zhou, J.; Chen, J. Advances in therapeutic implications of inorganic drug delivery nano-platforms for cancer. Int. J. Mol. Sci. 2019, 20, 965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikolova, M.P.; Chavali, M.S. Metal oxide nanoparticles as biomedical materials. Biomimetics 2020, 5, 27. [Google Scholar] [CrossRef]
- Perera, W.P.T.D.; Dissanayake, R.K.; Ranatunga, U.I.; Hettiarachchi, N.M.; Perera, K.D.C.; Unagolla, J.M.; De Silva, R.T.; Pahalagedara, L.R. Curcumin loaded zinc oxide nanoparticles for activity-enhanced antibacterial and anticancer applications. RSC Adv. 2020, 10, 30785–30795. [Google Scholar] [CrossRef]
- Jin, S.E.; Jin, H.E. Synthesis, characterization, and three-dimensional structure generation of zinc oxide-based nanomedicine for biomedical applications. Pharmaceutics 2019, 11, 575. [Google Scholar] [CrossRef] [Green Version]
- Waris, A.; Din, M.; Ali, A.; Ali, M.; Afridi, S.; Baset, A.; Ullah Khan, A. A Comprehensive Review of Green Synthesis of Copper Oxide Nanoparticles and Their Diverse Biomedical Applications. Inorg. Chem. Commun. 2020, 123, 108369. [Google Scholar] [CrossRef]
- Dylla, A.G.; Xiao, P.; Henkelman, G.; Stevenson, K.J. Morphological Dependence of Lithium Insertion in Nanocrystalline. J Phys. Chem. Lett. 2015, 2, 2015–2019. [Google Scholar]
- Mishra, P.K.; Mishra, H.; Ekielski, A.; Talegaonkar, S.; Vaidya, B. Zinc oxide nanoparticles: A promising nanomaterial for biomedical applications. Drug Discov. Today 2017, 22, 1825–1834. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.; Chen, X.; Zhang, J.; Schwank, J.W. A review on TiO2-based nanotubes synthesized via hydrothermal method: Formation mechanism, structure modification, and photocatalytic applications. Catal. Today 2014, 225, 34–51. [Google Scholar] [CrossRef]
- Yin, M.; Ju, E.; Chen, Z.; Li, Z.; Ren, J.; Qu, X. Upconverting nanoparticles with a mesoporous TiO2 shell for near-infrared-triggered drug delivery and synergistic targeted cancer therapy. Chem. A Eur. J. 2014, 20, 14012–14017. [Google Scholar] [CrossRef]
- Akasaka, H.; Mukumoto, N.; Nakayama, M.; Wang, T.; Yada, R.; Shimizu, Y.; Inubushi, S.; Kyotani, K.; Okumura, K.; Miyamoto, M.; et al. Investigation of the potential of using TiO2 nanoparticles as a contrast agent in computed tomography and magnetic resonance imaging. Appl. Nanosci. 2020, 10, 3143–3148. [Google Scholar] [CrossRef]
- Hasanzadeh Kafshgari, M.; Kah, D.; Mazare, A.; Nguyen, N.T.; Distaso, M.; Peukert, W.; Goldmann, W.H.; Schmuki, P.; Fabry, B. Anodic Titanium Dioxide Nanotubes for Magnetically Guided Therapeutic Delivery. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lanone, S.; Rogerieux, F.; Geys, J.; Dupont, A.; Maillot-Marechal, E.; Boczkowski, J.; Lacroix, G.; Hoet, P. Comparative toxicity of 24 manufactured nanoparticles in human alveolar epithelial and macrophage cell lines. Part. Fibre Toxicol. 2009, 6, 1–12. [Google Scholar] [CrossRef]
- Zhang, X.Q.; Yin, L.H.; Tang, M.; Pu, Y.P. ZnO, TiO 2, SiO 2, and Al 2O 3 nanoparticles-induced toxic effects on human fetal lung fibroblasts. Biomed. Environ. Sci. 2011, 24, 661–669. [Google Scholar] [CrossRef]
- Raman, R.; Thomas, R.G.; Weiner, M.W.; Jack, C.R.; Ernstrom, K.; Aisen, P.S.; Tariot, P.N.; Quinn, J.F. Comparison of the Mechanism of Toxicity of Zinc Oxide and Cerium Oxide Nanoparticles Based on Dissolution and Oxidative Stress Properties. ACS Nano 2008, 2, 2121–2134. [Google Scholar] [CrossRef]
- Karlsson, H.L.; Gustafsson, J.; Cronholm, P.; Möller, L. Size-dependent toxicity of metal oxide particles-A comparison between nano- and micrometer size. Toxicol. Lett. 2009, 188, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Pi, J.; Cai, J. The Advancing of Zinc Oxide Nanoparticles for Biomedical Applications. Bioinorg. Chem. Appl. 2018, 2018, 18. [Google Scholar] [CrossRef]
- Simeone, F.C.; Costa, A.L. Assessment of cytotoxicity of metal oxide nanoparticles on the basis of fundamental physical-chemical parameters: A robust approach to grouping. Environ. Sci. Nano 2019, 6, 3102–3112. [Google Scholar] [CrossRef]
- Wehmas, L.C.; Anders, C.; Chess, J.; Punnoose, A.; Pereira, C.B.; Greenwood, J.A.; Tanguay, R.L. Comparative metal oxide nanoparticle toxicity using embryonic zebrafish. Toxicol. Rep. 2015, 2, 702–715. [Google Scholar] [CrossRef] [Green Version]
- Arias, L.S.; Pessan, J.P.; Vieira, A.P.M.; De Lima, T.M.T.; Delbem, A.C.B.; Monteiro, D.R. Iron oxide nanoparticles for biomedical applications: A perspective on synthesis, drugs, antimicrobial activity, and toxicity. Antibiotics 2018, 7, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, W.; Wu, Z.; Yu, T.; Jiang, C.; Kim, W.S. Recent progress on magnetic iron oxide nanoparticles: Synthesis, surface functional strategies and biomedical applications. Sci. Technol. Adv. Mater. 2015, 16, 23501. [Google Scholar] [CrossRef]
- Xiao, Y.; Du, J. Superparamagnetic nanoparticles for biomedical applications. J. Mater. Chem. B 2020, 8, 354–367. [Google Scholar] [CrossRef]
- Li, H.; Xia, P.; Pan, S.; Qi, Z.; Fu, C.; Yu, Z.; Kong, W.; Chang, Y.; Wang, K.; Wu, D.; et al. The advances of ceria nanoparticles for biomedical applications in orthopaedics. Int. J. Nanomedicine 2020, 15, 7199–7214. [Google Scholar] [CrossRef] [PubMed]
- Sahu, T.; Bisht, S.; Das, K.; Kerkar, S. Nanoceria: Synthesis and Biomedical Applications. Curr. Nanosci. 2013, 9, 588–593. [Google Scholar] [CrossRef]
- Singh, K.R.B.; Nayak, V.; Sarkar, T.; Singh, R.P. Cerium oxide nanoparticles: Properties, biosynthesis and biomedical application. RSC Adv. 2020, 10, 27194–27214. [Google Scholar] [CrossRef]
- Xu, C.; Qu, X. Cerium oxide nanoparticle: A remarkably versatile rare earth nanomaterial for biological applications. NPG Asia Mater. 2014, 6. [Google Scholar] [CrossRef]
- Rajeshkumar, S.; Naik, P. Synthesis and biomedical applications of Cerium oxide nanoparticles—A Review. Biotechnol. Rep. 2018, 17, 1–5. [Google Scholar] [CrossRef]
- Verma, N.; Kumar, N. Synthesis and Biomedical Applications of Copper Oxide Nanoparticles: An Expanding Horizon. ACS Biomater. Sci. Eng. 2019, 5, 1170–1188. [Google Scholar] [CrossRef] [PubMed]
- Rabiee, N.; Bagherzadeh, M.; Kiani, M.; Ghadiri, A.M.; Etessamifar, F.; Jaberizadeh, A.H.; Shakeri, A. Biosynthesis of copper oxide nanoparticles with potential biomedical applications. Int. J. Nanomedicine 2020, 15, 3983–3999. [Google Scholar] [CrossRef] [PubMed]
- Grigore, M.E.; Biscu, E.R.; Holban, A.M.; Gestal, M.C.; Grumezescu, A.M. Methods of synthesis, properties and biomedical applications of CuO nanoparticles. Pharmaceuticals 2016, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Attarilar, S.; Yang, J.; Ebrahimi, M.; Wang, Q.; Liu, J.; Tang, Y.; Yang, J. The Toxicity Phenomenon and the Related Occurrence in Metal and Metal Oxide Nanoparticles: A Brief Review From the Biomedical Perspective. Front. Bioeng. Biotechnol. 2020, 8. [Google Scholar] [CrossRef]
- Karlsson, H.L.; Cronholm, P.; Gustafsson, J.; Möller, L.; Mo, L. Copper Oxide Nanoparticles Are Highly Toxic A Comparison between Metal Oxide Nanoparticles and Carbon Nanotubes—Chemical Research in Toxicology (ACS Publications). Chem. Res. Toxicol. 2008, 21, 1726–1732. [Google Scholar] [CrossRef]
- Qin, Q.; Li, J.; Wang, J. Antibacterial Activity Comparison of Three Metal Oxide Nanoparticles and their Dissolved Metal Ions. Water Environ. Res. 2017, 89, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Sarfraz, S.; Javed, A.; Mughal, S.S.; Bashir, M.; Rehman, A.; Parveen, S.; Khushi, A.; Khan, M.K. Copper Oxide Nanoparticles: Reactive Oxygen Species Generation and Biomedical Applications. Int. J. Comput. Theor. Chem. 2020, 8, 40–46. [Google Scholar] [CrossRef]
- Sherin, S.; Sheeja, S.; Sudha Devi, R.; Balachandran, S.; Soumya, R.S.; Abraham, A. In vitro and in vivo pharmacokinetics and toxicity evaluation of curcumin incorporated titanium dioxide nanoparticles for biomedical applications. Chem. Biol. Interact. 2017, 275, 35–46. [Google Scholar] [CrossRef]
- Saha, S.; Pramanik, K.; Biswas, A. Antibacterial activity and biocompatibility of curcumin/TiO2 nanotube array system on Ti6Al4V bone implants. Mater. Technol. 2020, 00, 1–12. [Google Scholar] [CrossRef]
- Aljubouri, F. The Formation, Structure, and Electronic Properties of TiO2 Nanoparticles Drug Delivery Conjugated with Curcumin (Theoretical and Experimental Study) Address for Correspondence. Indian J. Nat. Sci. 2018, 8, 14354. [Google Scholar]
- Oh, S.; Na, I.Y.; Choi, K.H. The effect of curcumin against in vitro adhesion of implant device-associated bacteria on nanosized titanium dioxide. J. Nano Res. 2013, 23, 83–90. [Google Scholar] [CrossRef]
- Varaprasad, K.; Yallapu, M.M.; Núñez, D.; Oyarzún, P.; López, M.; Jayaramudu, T.; Karthikeyan, C. Generation of engineered core-shell antibiotic nanoparticles. RSC Adv. 2019, 9, 8326–8332. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atef, H.A.; Mansour, M.K.; Ibrahim, E.M.; Sayed El-Ahl, R.M.H.; Al-Kalamawey, N.M.; El Kattan, Y.A.; Ali, M.A. Efficacy of Zinc Oxide Nanoparticles and Curcumin in Amelioration the Toxic Effects in Aflatoxicated Rabbits. Int. J. Curr. Microbiol. Appl. Sci. 2016, 5, 795–818. [Google Scholar] [CrossRef]
- Varaprasad, K.; López, M.; Núñez, D.; Jayaramudu, T.; Sadiku, E.R.; Karthikeyan, C.; Oyarzúnc, P. Antibiotic copper oxide-curcumin nanomaterials for antibacterial applications. J. Mol. Liq. 2020, 300. [Google Scholar] [CrossRef]
- Al-Senosy, Y.; Prince, A.E.-B.; Abd El Zaher, A. Biochemical study on the potential therapeutic use of novel curcumin copper oxide nanocomposite in diabetic complications in rats. Benha Vet. Med. J. 2018, 34, 182–190. [Google Scholar] [CrossRef]
- Bhandari, R.; Gupta, P.; Dziubla, T.; Hilt, J.Z. Single step synthesis, characterization and applications of curcumin functionalized iron oxide magnetic nanoparticles. Mater. Sci. Eng. C 2016, 67, 59–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Navya, P.N.; Kaphle, A.; Srinivas, S.P.; Bhargava, S.K.; Rotello, V.M.; Daima, H.K. Current trends and challenges in cancer management and therapy using designer nanomaterials. Nano Converg. 2019, 6, 1–30. [Google Scholar] [CrossRef] [Green Version]
- Ding, L.; Li, J.; Huang, R.; Liu, Z.; Li, C.; Yao, S.; Wang, J.; Qi, D.; Li, N.; Pi, J. Salvianolic acid B protects against myocardial damage caused by nanocarrier TiO2; and synergistic anti-breast carcinoma effect with curcumin via codelivery system of folic acid-targeted and polyethylene glycol-modified TiO2 nanoparticles. Int. J. Nanomedicine 2016, 11, 5709–5727. [Google Scholar] [CrossRef] [Green Version]
- Hiremath, C.G.; Heggnnavar, G.B.; Kariduraganavar, M.Y.; Hiremath, M.B. Co-delivery of paclitaxel and curcumin to foliate positive cancer cells using Pluronic-coated iron oxide nanoparticles. Prog. Biomater. 2019, 8, 155–168. [Google Scholar] [CrossRef] [Green Version]
- Hiremath, C.G.; Kariduraganavar, M.Y.; Hiremath, M.B. Synergistic delivery of 5-fluorouracil and curcumin using human serum albumin-coated iron oxide nanoparticles by folic acid targeting. Prog. Biomater. 2018, 7, 297–306. [Google Scholar] [CrossRef] [Green Version]
- Saikia, C.; Das, M.K.; Ramteke, A.; Maji, T.K. Evaluation of folic acid tagged aminated starch/ZnO coated iron oxide nanoparticles as targeted curcumin delivery system. Carbohydr. Polym. 2017, 157, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Sherin, S.; Balachandran, S.; Abraham, A. Curcumin incorporated titanium dioxide nanoparticles as MRI contrasting agent for early diagnosis of atherosclerosis- rat model. Vet. Anim. Sci. 2020, 10, 100090. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Zhang, J.; Chen, J.; Zeng, Y.; Zhu, Z.; Wan, Y. Fabrication of Curcumin-Modified TiO2 Nanoarrays via Cyclodextrin Based Polymer Functional Coatings for Osteosarcoma Therapy. Adv. Healthc. Mater. 2019, 8, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Rastegar, R.; Akbari Javar, H.; Khoobi, M.; Dehghan Kelishadi, P.; Hossein Yousefi, G.; Doosti, M.; Hossien Ghahremani, M.; Shariftabrizi, A.; Imanparast, F.; Gholibeglu, E.; et al. Evaluation of a novel biocompatible magnetic nanomedicine based on beta-cyclodextrin, loaded doxorubicin-curcumin for overcoming chemoresistance in breast cancer. Artif. Cells Nanomed. Biotechnol. 2018, 46, 207–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yallapu, M.M.; Othman, S.F.; Curtis, E.T.; Bauer, N.A.; Chauhan, N.; Kumar, D.; Jaggi, M.; Chauhan, S.C. Curcumin-loaded magnetic nanoparticles for breast cancer therapeutics and imaging applications. Int. J. Nanomedicine 2012, 7, 1761–1779. [Google Scholar] [CrossRef] [Green Version]
- Sawant, V.J.; Bamane, S.R. PEG-beta-cyclodextrin functionalized zinc oxide nanoparticles show cell imaging with high drug payload and sustained pH responsive delivery of curcumin in to MCF-7 cells. J. Drug Deliv. Sci. Technol. 2018, 43, 397–408. [Google Scholar] [CrossRef]
- Yallapu, M.M.; Othman, S.F.; Curtis, E.T.; Gupta, B.K.; Jaggi, M.; Chauhan, S.C. Multi-functional magnetic nanoparticles for magnetic resonance imaging and cancer therapy. Biomaterials 2011, 32, 1890–1905. [Google Scholar] [CrossRef] [Green Version]
- Yallapu, M.M.; Ebeling, M.C.; Khan, S.; Sundram, V.; Chauhan, N.; Gupta, B.K.; Puumala, S.E.; Jaggi, M.; Chauhan, S.C. Novel curcumin-loaded magnetic nanoparticles for pancreatic cancer treatment. Mol. Cancer Ther. 2013, 12, 1471–1480. [Google Scholar] [CrossRef] [Green Version]
- Cheung, R.C.F.; Ng, T.B.; Wong, J.H.; Chan, W.Y. Chitosan: An Update on Potential Biomedical and Pharmaceutical Applications. Mar. Drugs 2015, 13, 5156–5186. [Google Scholar] [CrossRef]
- Pham, X.N.; Nguyen, T.P.; Pham, T.N.; Tran, T.T.N.; Tran, T.V.T. Synthesis and characterization of chitosan-coated magnetite nanoparticles and their application in curcumin drug delivery. Adv. Nat. Sci. Nanosci. Nanotechnol. 2016, 7. [Google Scholar] [CrossRef]
- Upadhyaya, L.; Singh, J.; Agarwal, V.; Pandey, A.C.; Verma, S.P.; Das, P.; Tewari, R.P. Efficient water soluble nanostructured ZnO grafted O-carboxymethyl chitosan/curcumin-nanocomposite for cancer therapy. Process Biochem. 2015, 50, 678–688. [Google Scholar] [CrossRef]
- Marulasiddeshwara, R.; Jyothi, M.S.; Soontarapa, K.; Keri, R.S.; Velmurugan, R. Nonwoven fabric supported, chitosan membrane anchored with curcumin/TiO2 complex: Scaffolds for MRSA infected wound skin reconstruction. Int. J. Biol. Macromol. 2020, 144, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Sriram, K.; Maheswari, P.U.; Ezhilarasu, A.; Begum, K.M.M.S.; Arthanareeswaran, G. CuO-loaded hydrophobically modified chitosan as hybrid carrier for curcumin delivery and anticancer activity. Asia Pac. J. Chem. Eng. 2017, 12, 858–871. [Google Scholar] [CrossRef]
- Salarbashi, D.; Tafaghodi, M.; Heydari-Majd, M. Fabrication of curcumin-loaded soluble soy bean polysaccharide/ TiO2 nanoparticles bio-nanocomposite for improved antimicrobial activity. Nanomed. J. 2020, 7. [Google Scholar] [CrossRef]
- Singh, A.; Dutta, P.K. Green synthesis, characterization and biological evaluation of chitin glucan based zinc oxide nanoparticles and its curcumin conjugation. Int. J. Biol. Macromol. 2020, 156, 514–521. [Google Scholar] [CrossRef]
- Longmire, M.R.; Ogawa, M.; Choyke, P.L.; Kobayashi, H. Biologically optimized nanosized molecules and particles: More than just size. Bioconjug. Chem. 2011, 22, 993–1000. [Google Scholar] [CrossRef] [Green Version]
- Chen, Z.; Xu, L.; Gao, X.; Wang, C.; Li, R.; Xu, J.; Zhang, M.; Panichayupakaranant, P.; Chen, H. A multifunctional CeO2@SiO2-PEG nanoparticle carrier for delivery of food derived proanthocyanidin and curcumin as effective antioxidant, neuroprotective and anticancer agent. Food Res. Int. 2020, 137, 109674. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Xu, N.; Xu, L.; Wang, L.; Li, Z.; Ma, W.; Zhu, Y.; Xu, C.; Kotov, N.A. Multifunctional magnetoplasmonic nanoparticle assemblies for cancer therapy and diagnostics (Theranostics). Macromol. Rapid Commun. 2010, 31, 228–236. [Google Scholar] [CrossRef] [Green Version]
- Sorasitthiyanukarn, F.N.; Muangnoi, C.; Thaweesest, W.; Ratnatilaka Na Bhuket, P.; Jantaratana, P.; Rojsitthisak, P.; Rojsitthisak, P. Polyethylene glycol-chitosan oligosaccharide-coated superparamagnetic iron oxide nanoparticles: A novel drug delivery system for curcumin diglutaric acid. Biomolecules 2020, 10, 73. [Google Scholar] [CrossRef] [Green Version]
- Zholobak, N.M.; Shcherbakov, A.B.; Ivanova, O.S.; Reukov, V.; Baranchikov, A.E.; Ivanov, V.K. Nanoceria-curcumin conjugate: Synthesis and selective cytotoxicity against cancer cells under oxidative stress conditions. J. Photochem. Photobiol. B Biol. 2020, 209, 111921. [Google Scholar] [CrossRef]
- Rahimnia, R.; Salehi, Z.; Ardestani, M.S.; Doosthoseini, H. SPION conjugated curcumin nano-imaging probe: Synthesis and bio-physical evaluation. Iran. J. Pharm. Res. 2019, 18, 183–197. [Google Scholar] [CrossRef]
- Pourhajibagher, M.; Salehi Vaziri, A.; Takzaree, N.; Ghorbanzadeh, R. Physico-mechanical and antimicrobial properties of an orthodontic adhesive containing cationic curcumin doped zinc oxide nanoparticles subjected to photodynamic therapy. Photodiagnosis Photodyn. Ther. 2019, 25, 239–246. [Google Scholar] [CrossRef]
- Upadhyaya, L.; Singh, J.; Agarwal, V.; Pandey, A.C.; Verma, S.P.; Das, P.; Tewari, R.P. In situ grafted nanostructured ZnO/carboxymethyl cellulose nanocomposites for efficient delivery of curcumin to cancer. J. Polym. Res. 2014, 21. [Google Scholar] [CrossRef]
- Yu, H.; Guo, Z.; Wang, S.; Fernando, G.S.N.; Channa, S.; Kazlauciunas, A.; Martin, D.P.; Krasnikov, S.A.; Kulak, A.; Boesch, C.; et al. Fabrication of Hybrid Materials from Titanium Dioxide and Natural Phenols for Efficient Radical Scavenging against Oxidative Stress. ACS Biomater. Sci. Eng. 2019, 5, 2778–2785. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, S.B.; Sarrafzadeh, M.H.; Fakhroueian, Z.; Shahriari, S.; Khorramizadeh, M.R. Functionalization of ZnO nanoparticles by 3-mercaptopropionic acid for aqueous curcumin delivery: Synthesis, characterization, and anticancer assessment. Mater. Sci. Eng. C 2017, 79, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Nosrati, H.; Sefidi, N.; Sharafi, A.; Danafar, H.; Kheiri Manjili, H. Bovine Serum Albumin (BSA) coated iron oxide magnetic nanoparticles as biocompatible carriers for curcumin-anticancer drug. Bioorg. Chem. 2018, 76, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Sundar, S.; Mariappan, R.; Piraman, S. Synthesis and characterization of amine modified magnetite nanoparticles as carriers of curcumin-anticancer drug. Powder Technol. 2014, 266, 321–328. [Google Scholar] [CrossRef]
- Sawant, V.J.; Bamane, S.R.; Kanase, D.G.; Patil, S.B.; Ghosh, J. Encapsulation of curcumin over carbon dot coated TiO2 nanoparticles for pH sensitive enhancement of anticancer and anti-psoriatic potential. RSC Adv. 2016, 6, 66745–66755. [Google Scholar] [CrossRef]
- Oves, M.; Rauf, M.A.; Ansari, M.O.; Khan, A.A.P.; Qari, H.A.; Alajmi, M.F.; Sau, S.; Iyer, A.K. Graphene decorated zinc oxide and curcumin to disinfect the methicillin-resistant staphylococcus aureus. Nanomaterials 2020, 10, 1004. [Google Scholar] [CrossRef] [PubMed]
- Sudakaran, S.V.; Venugopal, J.R.; Vijayakumar, G.P.; Abisegapriyan, S.; Grace, A.N.; Ramakrishna, S. Sequel of MgO nanoparticles in PLACL nanofibers for anti-cancer therapy in synergy with curcumin/β-cyclodextrin. Mater. Sci. Eng. C 2017, 71, 620–628. [Google Scholar] [CrossRef]
- Dhivya, R.; Ranjani, J.; Bowen, P.K.; Rajendhran, J.; Mayandi, J.; Annaraj, J. Biocompatible curcumin loaded PMMA-PEG/ZnO nanocomposite induce apoptosis and cytotoxicity in human gastric cancer cells. Mater. Sci. Eng. C 2017, 80, 59–68. [Google Scholar] [CrossRef]
- Roy, S.; Rhim, J.W. Carboxymethyl cellulose-based antioxidant and antimicrobial active packaging film incorporated with curcumin and zinc oxide. Int. J. Biol. Macromol. 2020, 148, 666–676. [Google Scholar] [CrossRef] [PubMed]
- El-Nahhal, I.M.; Salem, J.; Anbar, R.; Kodeh, F.S.; Elmanama, A. Preparation and antimicrobial activity of ZnO-NPs coated cotton/starch and their functionalized ZnO-Ag/cotton and Zn(II) curcumin/cotton materials. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Niranjan, R.; Kaushik, M.; Selvi, R.T.; Prakash, J.; Venkataprasanna, K.S.; Prema, D.; Pannerselvam, B.; Venkatasubbu, G.D. PVA/SA/TiO2-CUR patch for enhanced wound healing application: In vitro and in vivo analysis. Int. J. Biol. Macromol. 2019, 138, 704–717. [Google Scholar] [CrossRef]
- Selvi, R.T.; Prasanna, A.P.S.; Niranjan, R.; Kaushik, M.; Devasena, T.; Kumar, J.; Chelliah, R.; Oh, D.-H.; Swaminathan, S.; Venkatasubbu, G.D. Metal oxide curcumin incorporated polymer patches for wound healing. Appl. Surf. Sci. 2018, 449, 603–609. [Google Scholar] [CrossRef]
- Soumya, K.R.; Snigdha, S.; Sugathan, S.; Mathew, J.; Radhakrishnan, E.K. Zinc oxide–curcumin nanocomposite loaded collagen membrane as an effective material against methicillin-resistant coagulase-negative Staphylococci. 3 Biotech 2017, 7, 1–10. [Google Scholar] [CrossRef]
- Application of different nanocariers for encapsulation of curcumin. Crit. Rev. Food Sci. Nutr. 2019, 59, 3468–3497. [CrossRef]
- George, D.; Maheswari, P.U.; Sheriffa Begum, K.M.M.; Arthanareeswaran, G. Biomass-Derived Dialdehyde Cellulose Cross-linked Chitosan-Based Nanocomposite Hydrogel with Phytosynthesized Zinc Oxide Nanoparticles for Enhanced Curcumin Delivery and Bioactivity. J. Agric. Food Chem. 2019, 67, 10880–10890. [Google Scholar] [CrossRef]
- Andrabi, S.M.; Majumder, S.; Gupta, K.C.; Kumar, A. Dextran based amphiphilic nano-hybrid hydrogel system incorporated with curcumin and cerium oxide nanoparticles for wound healing. Colloids Surf. B Biointerfaces 2020, 195, 111263. [Google Scholar] [CrossRef] [PubMed]
- Sattari, S.; Tehrani, A.D.; Adeli, M. pH-responsive hybrid hydrogels as antibacterial and drug delivery systems. Polymers (Basel) 2018, 10, 660. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khorsandi, L.; Mansouri, E.; Orazizadeh, M.; Jozi, Z. Curcumin attenuates hepatotoxicity induced by zinc oxide nanoparticles in rats. Balkan Med. J. 2016, 33, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Amer, M.G.; Karam, R.A. Morphological and Biochemical Features of Cerebellar Cortex After Exposure to Zinc Oxide Nanoparticles: Possible Protective Role of Curcumin. Anat. Rec. 2018, 301, 1454–1466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Karimi, S.; Khorsandi, L.; Nejaddehbashi, F. Protective effects of curcumin on testicular toxicity induced by titanium dioxide nanoparticles in mice. J. Bras. Reprod. Assist. 2019, 23, 344–351. [Google Scholar] [CrossRef]
- Elkhateeb, S.A.; Ibrahim, T.R.; El-Shal, A.S.; Hamid, O.I.A. Ameliorative role of curcumin on copper oxide nanoparticles-mediated renal toxicity in rats: An investigation of molecular mechanisms. J. Biochem. Mol. Toxicol. 2020, 1–13. [Google Scholar] [CrossRef]
| Therapeutic Agent | Synthesis Approach | Study Models | Outcomes |
|---|---|---|---|
| Curcumin–TiO2 nanoparticles (CNTPs) [51] | Coprecipitation in the presence of curcumin | In vitro: THP1 and H9c2 In vivo: Sprague-Dawley rat model | ↑ Stability curcumin in CTNPs form at pH 7.4 pH-dependent release at pH 6 > pH 7.4 In vitro: no distinct change in cells morphology, viability > 97% → nontoxicity of CTNPs In vivo: better biodistribution with more concentration in liver and kidney, half-life CTNPs > curcumin in all organs 24 h, high life of CN No change in SGPT, SGOT and LDH in CNTPs treated mice serum, no genotoxicity → in vivo nontoxicity of CTNPs |
| Curcumin-coated TiO2 nanotubes (TNTC) [52] | Drop-casting method | E. coli, S. aureus hMSCs | In vitro: ↓ wettability → reduced microbial adhesion, 43.6% E. coli and 38.5% S. aureus growth inhibition, no cytotoxic effect on hMSCs, ↓ ALP expression |
| Curcumin/TiO2 nanocomposites [53] | Adsorption from solution under sonication | HeLa | ↑ Inhibition of HeLa |
| Zinc oxide-grafted curcumin nanocomposites (ZNP-Cs) [20], | Surface adsorption from solution | S. aureus, S. epidermidis, B. cereus, and E. coli HEK293 | Modest curcumin-loading Antibacterial activities rod, RZNP–cur> spherical, SZNP–cur > long petal, LPZNP–cur > javelin, JZNP–cur Oblong particles showed higher activities than spherical ones E. coli less susceptible to antimicrobial activities, SZNP–cur show the most potent against S. epidermidis, RZNP–cur show the most potent against the other three Composites demonstrate better performance than bare curcumin or ZnO |
| Zinc oxide–curcumin core–shell (ZnO–cur) [55] | Precipitation under | S. aureus, S. pneumoniae, E. coli, and S. dysenteriae | ↑ Bacterial inhibition effect than amoxicillin and pure curcumin |
| Copper oxide–curcumin core–shell [57] | Precipitation under ultrasonication | E. coli, S. aureus, S. dysenteriae, and S. pneumoniae | ↑ Water dispersibility, better aqueous solubility of curcumin in core–shell form than in pure form, ↑ Antibacterial effect than nanocurcumin and amoxicillin ↓ Toxicity towards African green monkey kidney cell (Vero) than CuO |
| Curcumin–CuO physical mixture [58] | Grinding together curcumin and CuO powders | Streptozotocin (STZ) induced diabetic mice | ↓ MDA level, ↑ GSH and SOD levels, insulin concentration, mRNA expression level of insulin gene (IR-A and IR2) |
| Curcumin-coated iron oxide (C–IO) [59] | Coprecipitation in the presence of curcumin | HUVEC | ↓ Toxicity compared to uncoated IO or curcumin to HUVEC Show protective effect to HUVEC from PCB126 induced toxicity |
| Therapeutic Agent | Synthesis Approach | Study Models | Outcomes |
|---|---|---|---|
| Folic acid (FA)/polyethylene glycol (PEG)/TiO2 [61] | Emulsion evaporation solidification | In vitro: MCF-7, MDA-MB-231, H9c2 In vivo: MDA-MB-231 tumor-bearing BALB/c mice | In vitro: ↑ viability of H9c2 compared to only TiO2 treatment ↑ Cytotoxicity towards MCF-7 and MDA-MB-231 cells, cellular uptake by MCF-7 cells compared to untargeted NPs In vivo: ↑ drug concentration at the tumor site and better antitumor activity compared to untargeted NPs |
| PTX–cur-OAMNPPF127FA [62] | Fe3O4 by coprecipitation, surface functionalization by deposition from solution | MCF-7 | Lower hemolytic assay 4.1% ↑ Cellular uptake and growth inhibition of MCF-7 for active FA and passive magnetic field targeting Superparamagnetic behavior retained through lower saturation magnetization compared to MNP only |
| 5FU–CUR-C-MNP-HSA-FA [63] | MNPs by coprecipitation | MCF-7 | ↑ Colloidal stability, Superparamagnetic property maintained, but less saturation magnetization ↑ Cytotoxicity against MCF-7 ↑ Cellular uptake ↑Viability of MCF-7 cells, for FA targeted under magnetic field |
| Folic-acid-tagged aminated starch/ZnO-coated Fe3O4 [64] | Stirring together the nanocomposite and curcumin suspension overnight and genipin crosslinking | HepG2 and MCF7 | higher colloidal stability with zeta potential value of 42.9 mV, pH-dependent release profile → higher release rate at acidic pH, biocompatibility with human lymphocytes ↑ Cellular uptake and anticancer effect on MCF-7& HepG2 |
| Curcumin-incorporated TiO2-conjugated with MCP-1 antibody (CTNP-MCP-1) [65] | Suspending presynthesized CTNPs in MCP-1 antibody under stirring | Cholesterol-fed, atherosclerotic Sprague-Dawley rat | Normal ALP, GGT levels, RBC morphology, and aorta architecture for CTNP-MCP-1 treated rats → nontoxic ↑ Aortic concentration of CTNP-MCP-1 compared to CTNP → better targeting ↑ Half-life, distribution, and ↑ hydrolysis of curcumin in CTNPs → better stability MRI image contrast of CTNP-MCP-1 > CTNP due to targeting effect of MCP-1 antibody and ↑ paramagnetic property of TiO2 when combined with carbon compounds |
| FA-mPEG–PAMAM G3-CUR@SPIONs [12] | Coprecipitation for Fe3O4, dispersion of the constituents under sonication and mixing | KB and MCF-7 | ↑ KB cells (with higher FRs) lethality compared to MCF-7 (with lower FRS) |
| TiO2/polydopamine (pDA)/polycyclodextrin (pDC)-curcumin [66] | Hydrothermal synthesis of nanotube array on Ti substrates, followed by pDA and pCD coating and curcumin-loading | In vitro: MG63, In vivo: osteocarcinoma xenografted nude mice | Membrane shrinkage, absence of filopodia and lamellipodia, ↓ Cell density of MG63 Biocompatibility towards MC3T3-E1 cells ↓ Tumor growth on osteocarcinoma xenografted nude mice |
| DOX and curcumin-loaded, HAPA/β-CD/SPION [67] | Fe3O4 by coprecipitation HAPA coating by coprecipitation, loaded β-CD functionalization and drug loading by mixing NPs with components in a suspension | In vitro: MCF-7 In vivo: tumor-bearing BALB/c mice | ↓ Amount of protein corona adsorbed on the nanocomposite ↑ Cellular uptake by MCF-7 cells↑ Hemocompatibility with only 0.1% hemolysis ↑ Toxicity against MCF-7 cells ↓ percent relative tumor volume (% RTV) in the case nanocomposite with magnetic field treatment |
| MNP-CUR [68] | Fe3O4 by coprecipitation in the presence of β-CD and F68, curcumin-loading by diffusion method | MDA-MB-231 | less aggregated nanocomposite Slow and sustained release of curcumin ↑ Drug uptake by the MDA-MB-231 cells ↑ Prevention of serum protein adsorption and colony formation ↓ Viability of MDA-MB-231 cells ↓ T2-weighted signal in MRI imaging analysis |
| Curcumin-loaded PEG/β-CD/ZnO [69] | Wet coprecipitation method | S. aureus, MCF-7 | ↑ Drug encapsulation efficiency, pH-dependent sustained drug release ↑ Antibacterial and anticancer properties compared to free curcumin ↑ Photoluminescence property compared to composite without β-CD |
| Curcumin-loaded β-cyclodextrin and pluronic F127 stabilized iron oxide (MNP–cur) [70] | Fe3O4 by Coprecipitation in the presence of β-cyclodextrin pluronic F127, curcumin-loading precipitation forms a suspension | In vitro: HPNote images cannot be edited for English. Please verify all text carefully.-II, Panc-1 A2780PC, MDA-MB-231, PC-3 In vivo: Note images cannot be edited for English. Please verify all text carefully.AF-II xenograft mice | ↑ Water dispersibility efficient drug encapsulation and sustained release ↑ MRI contrasting during MRI scanning of A2780PC ↑ Inhibition of A2780PC, MDA-MB-231 ↑ Drug uptake by HPAF-II and Panc-1 ↑Proliferation and colony formation of HPAF-II and Panc-1 ↓ Tumor growth of HPAF-II xenograft mice ↑ Serum bioavailability of curcumin (2.5× that of free curcumin) |
| Curcumin-loaded chitosan (CS)–Fe3O4 [73] | Fe3O4 by reverse microemulsion, chitosan coating by stirring together CS in acidic solution and Fe3O4 suspension in the presence of CTAB | A549 | controlled drug release profile, intact paramagnetic property, ↑ Cytotoxicity against A549 cells compared to free curcumin |
| Cur–O–CMCS–ZnO [74] | ZnO NPs using the coprecipitation method, O-CMCS coating using ex situ grafting, curcumin-loading, precipitation from solution | MA104, L929 | ↑ Water solubility of curcumin in the composite form ↑ Accumulation and cytotoxicity towards MA104 compared to L929 |
| Curcumin-loaded, phendione-modified chitosan-coated CuO [76] | CuO by chemical reduction method, CS coating and curcumin-loading by precipitation from solutions | MCF-7, M19-MEL, HeLa | ↑ Drug loading efficiency (96.3%), sustained drug release ↑ Anticancer effect (> 2×) M19-MEL, MCF-7, HeLa compared to free curcumin |
| Curcumin-loaded, chitin–glucan-coated ZnO NPs(Cur–ChGC@ZNONPs) [78] | ChGC@ZnONPs by coprecipitation in the presence of ChGC, curcumin-loading precipitation from solution | E. coli and B. subtilis | Better inhibition effect against E. coli and B. subtilis ↑ Radical scavenging activities → increased antioxidant properties |
| Curcumin-loaded PMMA–PEG/ZnO [94] | ZnO by coprecipitation, PMMA–PEG by double emulsion, curcumin-loading and copolymer coating precipitation from suspension. | AGS | ↑ Drug loading percentage, 47% and loading efficiency, 92%, pronounced DNA fragmentation ↑ Anticancer effect compared to ZnO or curcumin |
| Curcumin-loaded, PEG-functionalized, gold nanoparticle decorated, Fe3O4–silica core–shell [81] | Coprecipitation for Fe3O4, surface modification and drug loading precipitation from solution | HL-60 | Stable composite assembly with a zeta potential of -24.5 mV ↑ T2 value during MRI imaging, ↓ Viability of HL60, 53.4% in 42 h |
| Curcumin and PAC loaded PEG-modified CeO2@SiO2 (CeO2@SiO2–PEG–PAC/Cur) [80] | CeO2@SiO2 by chemical precipitation method, PEG by nanoprecipitation, drugs loading by precipitation from respective solutions | L02, HepG2, HeLa, PC-12 | ↓ Hydrodynamic size of the composite from 421 to 359 nm↓ Cytotoxicity towards L02, Neuroprotective effect against Aβ1-42 mediated PC-12 ↑ Antiproliferative effect against HepG2 and HeLa |
| cCur/ZnONPs [85]. | cCur/ZnO by precipitation from solution | Streptococcus mutans (S. mutans), Streptococcus sobrinus (S. sobrinus), Lactobacillus acidophilus (L. acidophilus) | Antibacterial growth inhibition for 90 days, ↓ bacterial growth rate after 90 days shear bond strength in acceptable range (6–8 Mpa) |
| curcumin-loaded, oleic acid, and citric acid-functionalized Fe3O4 [84] | Fe3O4 by coprecipitation, in the presence of citric acid and oleic acid, curcumin-loading by precipitation from solution | MDA-MB-231 | ↓ Viability of MDA-MB-231 compared to free curcumin treatment superparamagnetic property with saturation magnetization 60–80 emu/g ↑ T2 relaxation time→ MRI contrasting potential |
| Curcumin–ZnO incorporated carboxymethyl cellulose (Cur/ZnO/CMC) [86] | ZnO/CMC by coprecipitation in the presence of CMC, precipitation from solution | L929, MA104 | ↑ Aqueous solubility, loading efficiency of 44%, controlled release profile ↓ Cytotoxic to L929 cells (80% viability) ↑ Cytotoxicity MA104 cells (20%, viability) |
| Curcumin-loaded carboxyl-terminated ZnO NPs [88] | Coprecipitation in the presence of 3-mercaptopropionic acid (MPA), curcumin-loading precipitation from solution | MDA-MB-23 | ↑ In aqueous and ↓ In IC50 against MDA-MB-23 compared to free curcumin |
| bovine serum albumin-coated Fe3O4–curcumin (F@BSA–curcumin) [89] | Desolvation and chemical coprecipitation process | HFF2, MCF-7 | pH-dependent drug release biocompatible to HFF2 cells ↑ Cytotoxic to MCF-7 |
| Curcumin-loaded, carbon dots-coated rutile TiO2 [91] | TiO2 by coprecipitation, carbon dot coating and Curcumin-loading precipitation from solution | HaCaT, MCF-7, McCoy | ↑ Curcumin-loading percentage (89%) ↑ Inhibition of HaCaT comparable to that of the positive control 5-fluorouracil apoptosis on MCF-7, biocompatible to McCoy |
| Therapeutic Agent | Synthesis Approach | Study Models | Outcomes |
|---|---|---|---|
| CMC/curcumin/ZnO film [77] | Solution-casting method | L. monocytogenes and E. coli DPPH• and ABTS•+ | ↓ Visible-light transparency, UV transmittance blocked, ↑ Mechanical strength and stiffness, but ↓ flexibility ↓ WVP, optimal antibacterial and antioxidant properties |
| SSPS/TiO2 nanoparticles/curcumin film [95] | Solution-casting method | P. aeruginosa and S. aureus | ↓ WVP, ↑ mechanical, antimicrobial effect, pH-dependent color change |
| Nonwoven polypropylene/chitosan/curcumin TiO2 (MCUT) [75] | Suspension-casting | In vitro: E. coli and S. aureus In vivo: MRSA-inoculated Sprague–Dawley rats | Moderated water uptake, delayed drug release pattern In vitro ↑ antibacterial effect In vivo: better wound contraction, bacterial growth inhibition, re-epithelialization, and good collagen organization |
| PVA/SA/TiO2–cur [97] | Slurry-casting | In vitro: B. subtilis, K. pneumonia, S. aureus, E. coli, Candida albicans (C. albicans), Aspergillus niger (A. niger) | Anti-fungal effect > clotrimazole, but < fluconazole antibiotics Effective antibacterial effect at 100 µg concentration for all bacteria than streptomycin antibiotics |
| Sodium alginate SA/PVA/TiO2/curcumin patch [98] | Gel-casting method | In vitro: B. subtilis, S. aureus, P. aeruginosa In vivo: incision-wound-induced 18 Wistar albino rats | Good swelling rate → capable of absorbing exudate, water absorption rate and hemolytic assay within optimal limits, antibacterial effect against both Gram-positive and Gram-negative bacteria Nontoxic towards NIH3T3 cells In vivo: ↓ necrosis, complete re-epithelialization, uniform collagen and fibrous tissues |
| ZnO–curcumin incorporated collagen wound dressing [99] | Dip-coating of commercial collagen skin-wound dressing material in curcumin/ZnO suspension | CoNS | ↑ CoNS cell death compared to viable control, CoNS cell clustering and lack of cell integrity |
| ZnO NPs in dimethyl cellulose-crosslinked chitosan hydrogel [101] | Solution-based preparation in the presence of ZnO NPs then soaking dried gel in curcumin solution | L929, A431 | ↑ Drug loading capacity (30% ↑ by incorporating ZnO) enhanced the mechanical properties ↑ Cytotoxicity towards L929↑ Cytotoxicity against A431 |
| Ceria and curcumin in gelatin–glucan-based hydrogel [102] | Dispersion of curcumin and CeO2 in the hydrogel by physical interactions | HaCat | ↑ Mechanical stability, stable elastic behavior, no significant ↓ swelling ratio by incorporating ceria in hydrogel Faster degradation, controlled drug release behavior Biocompatible with HaCat, Show antioxidant property against H2O2 treated HaCat |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Beyene, A.M.; Moniruzzaman, M.; Karthikeyan, A.; Min, T. Curcumin Nanoformulations with Metal Oxide Nanomaterials for Biomedical Applications. Nanomaterials 2021, 11, 460. https://doi.org/10.3390/nano11020460
Beyene AM, Moniruzzaman M, Karthikeyan A, Min T. Curcumin Nanoformulations with Metal Oxide Nanomaterials for Biomedical Applications. Nanomaterials. 2021; 11(2):460. https://doi.org/10.3390/nano11020460
Chicago/Turabian StyleBeyene, Anteneh Marelign, Mohammad Moniruzzaman, Adhimoolam Karthikeyan, and Taesun Min. 2021. "Curcumin Nanoformulations with Metal Oxide Nanomaterials for Biomedical Applications" Nanomaterials 11, no. 2: 460. https://doi.org/10.3390/nano11020460
APA StyleBeyene, A. M., Moniruzzaman, M., Karthikeyan, A., & Min, T. (2021). Curcumin Nanoformulations with Metal Oxide Nanomaterials for Biomedical Applications. Nanomaterials, 11(2), 460. https://doi.org/10.3390/nano11020460








