Nanotechnology Innovations to Enhance the Therapeutic Efficacy of Quercetin
Abstract
1. Introduction
1.1. Quercetin as a Promising Compound
1.2. Natural Sources of Quercetin and Biosynthesis
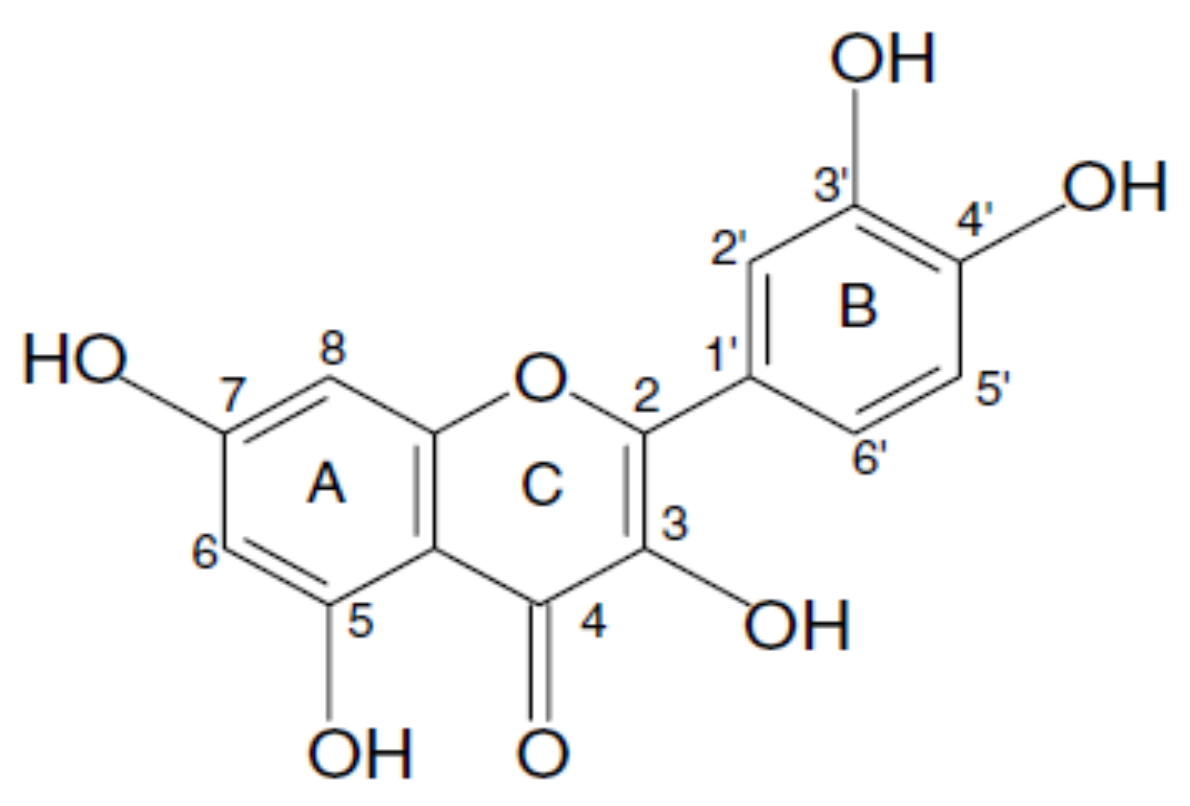
1.3. Chemical Structure and Properties of Quercetin
2. Pharmacokinetics of Quercetin
2.1. Absorption, Distribution, Metabolism, and Elimination
2.2. Toxicity of Quercetin
3. Health Benefits of Quercetin
3.1. Cancer Chemoprevention
3.2. Cardiovascular Protection
3.3. Anti-Inflammatory Action
3.4. Antioxidant Activity
3.5. Neuroprotection Effects
4. Nanoparticles for Quercetin Delivery
4.1. Liposomes
4.2. Lipid Nanoparticles
4.3. Polymeric Nanoparticles
Biopolymeric Nanoparticles
4.4. Magnetic Nanoparticles
4.5. Mesoporous silica Nanoparticles
4.6. Cyclodextrins
5. Clinical Trials and Marketed Formulations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Harborne, J.B. Flavonoids in the environment: Structure-activity relationships. Prog. Clin. Biol. Res. 1988, 280, 17–27. [Google Scholar] [PubMed]
- Havsteen, B. Flavonoids, a class of natural products of high pharmacological potency. Biochem. Pharmacol. 1983, 32, 1141–1148. [Google Scholar] [CrossRef]
- Formica, J.; Regelson, W. Review of the biology of quercetin and related bioflavonoids. Food Chem. Toxicol. 1995, 33, 1061–1080. [Google Scholar] [CrossRef]
- Murota, K.; Terao, J. Antioxidative flavonoid quercetin: Implication of its intestinal absorption and metabolism. Arch. Biochem. Biophys. 2003, 417, 12–17. [Google Scholar] [CrossRef]
- Mukhopadhyay, P.; Prajapati, A.K. Quercetin in anti-diabetic research and strategies for improved quercetin bioavailability using polymer-based carriers—A review. RSC Adv. 2015, 5, 97547–97562. [Google Scholar] [CrossRef]
- Zang, X.; Cheng, M.; Zhang, X.; Chen, X. Quercetin nanoformulations: A promising strategy for tumor therapy. Food Funct. 2021, 12, 6664–6681. [Google Scholar] [CrossRef]
- Wach, A.; Pyrzyńska, K.; Biesaga, M. Quercetin content in some food and herbal samples. Food Chem. 2007, 100, 699–704. [Google Scholar] [CrossRef]
- Harnly, J.M.; Doherty, R.F.; Beecher, G.R.; Holden, J.M.; Haytowitz, D.B.; Bhagwat, S.; Gebhardt, S. Flavonoid Content of U.S. Fruits, Vegetables, and Nuts. J. Agric. Food Chem. 2006, 54, 9966–9977. [Google Scholar] [CrossRef]
- Day, A.J.; Williamson, G. Human metabolism of dietary quercetin glycosides. Basic Life Sci. 1999, 66, 415–434. [Google Scholar] [CrossRef]
- Bonaccorsi, P.; Caristi, C.; Gargiulli, C.; Leuzzi, U. Flavonol Glucoside Profile of Southern Italian Red Onion (Allium cepaL.). J. Agric. Food Chem. 2005, 53, 2733–2740. [Google Scholar] [CrossRef] [PubMed]
- Häkkinen, S.H.; Kärenlampi, S.O.; Heinonen, I.M.; Mykkänen, H.M.; Törrönen, A.R. Content of the Flavonols Quercetin, Myricetin, and Kaempferol in 25 Edible Berries. J. Agric. Food Chem. 1999, 47, 2274–2279. [Google Scholar] [CrossRef]
- Urbánek, M.; Blechtová, L.; Pospíšilová, M.; Polášek, M. On-line coupling of capillary isotachophoresis and capillary zone electrophoresis for the determination of flavonoids in methanolic extracts of Hypericum perforatum leaves or flowers. J. Chromatogr. A 2002, 958, 261–271. [Google Scholar] [CrossRef]
- Sampson, L.; Rimm, E.; Hollman, P.C.; de Vries, J.H.; Katan, M.B. Flavonol and Flavone Intakes in US Health Professionals. J. Am. Diet. Assoc. 2002, 102, 1414–1420. [Google Scholar] [CrossRef]
- Erlund, I. Review of the flavonoids quercetin, hesperetin, and naringenin. Dietary sources, bioactivities, bioavailability, and epidemiology. Nutr. Res. 2004, 24, 851–874. [Google Scholar] [CrossRef]
- Brown, J. A review of the genetic effects of naturally occurring flavonoids, anthraquinones and related compounds. Mutat. Res. Genet. Toxicol. 1980, 75, 243–277. [Google Scholar] [CrossRef]
- Mendoza-Wilson, A.M.; Glossman-Mitnik, D. CHIH-DFT study of the electronic properties and chemical reactivity of quercetin. J. Mol. Struct. THEOCHEM 2005, 716, 67–72. [Google Scholar] [CrossRef]
- Codorniu-Hernández, E.; Mesa-Ibirico, A.; Montero-Cabrera, L.A.; Martínez-Luzardo, F.; Borrmann, T.; Stohrer, W.-D. Theoretical study of flavonoids and proline interactions. Aqueous and gas phases. J. Mol. Struct. THEOCHEM 2003, 623, 63–73. [Google Scholar] [CrossRef]
- Kim, M.K.; Park, K.-S.; Yeo, W.-S.; Choo, H.; Chong, Y. In vitro solubility, stability and permeability of novel quercetin–amino acid conjugates. Bioorganic Med. Chem. 2009, 17, 1164–1171. [Google Scholar] [CrossRef]
- Althans, D.; Schrader, P.; Enders, S. Solubilisation of quercetin: Comparison of hyperbranched polymer and hydrogel. J. Mol. Liq. 2014, 196, 86–93. [Google Scholar] [CrossRef]
- Gao, L.; Liu, G.; Wang, X.; Liu, F.; Xu, Y.; Ma, J. Preparation of a chemically stable quercetin formulation using nanosuspension technology. Int. J. Pharm. 2011, 404, 231–237. [Google Scholar] [CrossRef]
- Dall’Acqua, S.; Miolo, G.; Innocenti, G.; Caffieri, S. The Photodegradation of Quercetin: Relation to Oxidation. Molecules 2012, 17, 8898–8907. [Google Scholar] [CrossRef] [PubMed]
- Buchner, N.; Krumbein, A.; Rohn, S.; Kroh, L.W. Effect of thermal processing on the flavonols rutin and quercetin. Rapid Commun. Mass Spectrom. 2006, 20, 3229–3235. [Google Scholar] [CrossRef]
- Murota, K.; Nakamura, Y.; Uehara, M. Flavonoid metabolism: The interaction of metabolites and gut microbiota. Biosci Biotechnol Biochem. 2018, 82, 600–610. [Google Scholar] [CrossRef]
- Chen, X.; Yin, O.Q.P.; Zuo, Z.; Chow, M.S.S. Pharmacokinetics and Modeling of Quercetin and Metabolites. Pharm. Res. 2005, 22, 892–901. [Google Scholar] [CrossRef] [PubMed]
- Walle, T.; Walle, U.K.; Halushka, P.V. Carbon Dioxide Is the Major Metabolite of Quercetin in Humans. J. Nutr. 2001, 131, 2648–2652. [Google Scholar] [CrossRef]
- Petri, N.; Tannergren, C.; Holst, B.; Mellon, F.A.; Bao, Y.; Plumb, G.W.; Bacon, J.; O’Leary, K.A.; Kroon, P.; Knutson, L.; et al. Absorption/Metabolism of Sulforaphane and Quercetin, and Regulation of Phase Ii Enzymes, in human jejunum In Vivo. Drug Metab. Dispos. 2003, 31, 805–813. [Google Scholar] [CrossRef]
- Rechner, A.R.; Kuhnle, G.; Bremner, P.; Hubbard, G.P.; Moore, K.P.; Rice-Evans, C.A. The metabolic fate of dietary polyphenols in humans. Free Radic. Biol. Med. 2002, 33, 220–235. [Google Scholar] [CrossRef]
- Murota, K.; Terao, J. Quercetin appears in the lymph of unanesthetized rats as its phase II metabolites after administered into the stomach. FEBS Lett. 2005, 579, 5343–5346. [Google Scholar] [CrossRef] [PubMed]
- Graf, B.A.; Ameho, C.; Dolnikowski, G.; Milbury, P.E.; Chen, C.-Y.; Blumberg, J.B. Rat Gastrointestinal Tissues Metabolize Quercetin. J. Nutr. 2006, 136, 39–44. [Google Scholar] [CrossRef]
- Crespy, V.; Morand, C.; Manach, C.; Besson, C.; Demigne, C.; Remesy, C. Part of quercetin absorbed in the small intestine is conjugated and further secreted in the intestinal lumen. Am. J. Physiol. 1999, 277, G120–G126. [Google Scholar] [CrossRef]
- O’Leary, K.A.; Day, A.J.; Needs, P.W.; Mellon, F.A.; O’Brien, N.M.; Williamson, G. Metabolism of quercetin-7- and quercetin-3-glucuronides by an in vitro hepatic model: The role of human β-glucuronidase, sulfotransferase, catechol-O-methyltransferase and multi-resistant protein 2 (MRP2) in flavonoid metabolism. Biochem. Pharmacol. 2003, 65, 479–491. [Google Scholar] [CrossRef]
- De Santi, C.; Pietrabissa, A.; Mosca, F.; Pacifici, G. Methylation of quercetin and fisetin, flavonoids widely distributed in edible vegetables, fruits and wine, by human liver. Int. J. Clin. Pharmacol. Ther. 2002, 40, 207–212. [Google Scholar] [CrossRef]
- Boulton, D.W.; Walle, U.K.; Walle, T. Extensive Binding of the Bioflavonoid Quercetin to Human Plasma Proteins. J. Pharm. Pharmacol. 2011, 50, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.-H.; Nakata, R.; Oshima, S.; Inakuma, T.; Terao, J. Accumulation of quercetin conjugates in blood plasma after the short-term ingestion of onion by women. Am. J. Physiol. Integr. Comp. Physiol. 2000, 279, R461–R467. [Google Scholar] [CrossRef] [PubMed]
- De Boer, V.; Dihal, A.A.; Van Der Woude, H.; Arts, I.; Wolffram, S.; Alink, G.M.; Rietjens, I.; Keijer, J.; Hollman, P.C.H. Tissue Distribution of Quercetin in Rats and Pigs. J. Nutr. 2005, 135, 1718–1725. [Google Scholar] [CrossRef] [PubMed]
- Abrahamse, S.L.; Kloots, W.J.; Van Amelsvoort, J.M. Absorption, distribution, and secretion of epicatechin and quercetin in the rat. Nutr. Res. 2005, 25, 305–317. [Google Scholar] [CrossRef]
- Gugler, R.; Leschik, M.; Dengler, H.J. Disposition of quercetin in man after single oral and intravenous doses. Eur. J. Clin. Pharmacol. 1975, 9, 229–234. [Google Scholar] [CrossRef]
- De Vries, J.H.; Hollman, P.C.; Meyboom, S.; Buysman, M.N.; Zock, P.; Van Staveren, W.A.; Katan, M.B. Plasma concentrations and urinary excretion of the antioxidant flavonols quercetin and kaempferol as biomarkers for dietary intake. Am. J. Clin. Nutr. 1998, 68, 60–65. [Google Scholar] [CrossRef]
- Young, J.F.; Nielsen, S.E.; Haraldsdottir, J.; Daneshvar, B.; Lauridsen, S.T.; Knuthsen, P.; Crozier, A.; Sandstrom, B.; Dragsted, L.O. Effect of fruit juice intake on urinary quercetin excretion and biomarkers of antioxidative status. Am. J. Clin. Nutr. 1999, 69, 87–94. [Google Scholar] [CrossRef]
- Ueno, I.; Nakano, N.; Hirono, I. Metabolic fate of [14C] quercetin in the ACI rat. Jpn. J. Exp. Med. 1983, 53, 41–50. [Google Scholar]
- Bjeldanes, L.; Chang, G. Mutagenic activity of quercetin and related compounds. Science 1977, 197, 577–578. [Google Scholar] [CrossRef]
- Hardigree, A.; Epler, J. Comparative mutagenesis of plant flavonoids in microbial systems. Mutat. Res. Toxicol. 1978, 58, 231–239. [Google Scholar] [CrossRef]
- Brown, J.P.; Dietrich, P.S. Mutagenicity of plant flavonols in the Salmonella/mammalian microsome test: Activation of flavonol glycosides by mixed glycosidases from rat cecal bacteria and other sources. Mutat. Res. Toxicol. 1979, 66, 223–240. [Google Scholar] [CrossRef]
- Rueff, J.; Laires, A.; Gaspar, J.; Borba, H.; Rodrigues, A.S. Oxygen species and the genotoxicity of quercetin. Mutat. Res. Mol. Mech. Mutagen. 1992, 265, 75–81. [Google Scholar] [CrossRef]
- Yoshida, M.A.; Sasaki, M.; Sugimura, K.; Kawachi, T. Cytogenetic Effects of Quercetin on Cultured Mammalian Cells. Proc. Jpn. Acad. Ser. B 1980, 56, 443–447. [Google Scholar] [CrossRef][Green Version]
- Meltz, M.L.; MacGregor, J.T. Activity of the plant flavanol quercetin in the mouse lymphoma L5178Y TK+/− mutation, DNA single-strand break, and Balb/c 3T3 chemical transformation assays. Mutat. Res. Toxicol. 1981, 88, 317–324. [Google Scholar] [CrossRef]
- Cierniak, A.; Papiez, M.; Kapiszewska, M. Modulatory effect of quercetin on DNA damage, induced by etoposide in bone marrow cells and on changes in the activity of antioxidant enzymes in rats. Rocz. Akad. Med. Bialymst. 2004, 49 (Suppl. 1), 167–169. [Google Scholar]
- Ngomuo, A.J.; Jones, R.S. Genotoxicity studies of quercetin and shikimate in vivo in the bone marrow of mice and gastric mucosal cells of rats. Vet. Hum. Toxicol. 1996, 38, 176–180. [Google Scholar] [PubMed]
- Takanashi, H.; Aiso, S.; Hirono, I.; Matsushima, T.; Sugimura, T. Carcinogenicity Test of Quercetin and Kaempferol in Rats by Oral Administration. J. Food Saf. 1983, 5, 55–60. [Google Scholar] [CrossRef]
- Hosaka, S.; Hirono, I. Carcinogenicity test of quercetin by pulmonary-adenoma bioassay in strain A mice. Gan 1981, 72, 327–328. [Google Scholar]
- Davis, J.M.; Murphy, E.A.; Carmichael, M.D. Effects of the Dietary Flavonoid Quercetin Upon Performance and Health. Curr. Sports Med. Rep. 2009, 8, 206–213. [Google Scholar] [CrossRef] [PubMed]
- Murakami, A.; Ashida, H.; Terao, J. Multitargeted cancer prevention by quercetin. Cancer Lett. 2008, 269, 315–325. [Google Scholar] [CrossRef]
- Ashida, H.; Fukuda, I.; Yamashita, T.; Kanazawa, K. Flavones and flavonols at dietary levels inhibit a transformation of aryl hydrocarbon receptor induced by dioxin. FEBS Lett. 2000, 476, 213–217. [Google Scholar] [CrossRef]
- Chen, W.; Wang, X.; Zhuang, J.; Zhang, L.; Lin, Y. Induction of death receptor 5 and suppression of survivin contribute to sensitization of TRAIL-induced cytotoxicity by quercetin in non-small cell lung cancer cells. Carcinogenesis 2007, 28, 2114–2121. [Google Scholar] [CrossRef]
- Kim, W.K.; Bang, M.H.; Kim, E.S.; Kang, N.E.; Jung, K.C.; Cho, H.J.; Park, J.H. Quercetin decreases the expression of ErbB2 and ErbB3 proteins in HT-29 human colon cancer cells. J. Nutr. Biochem. 2005, 16, 155–162. [Google Scholar] [CrossRef]
- Xing, N.; Chen, Y.; Mitchell, S.H.; Young, C.Y.F. Quercetin inhibits the expression and function of the androgen receptor in LNCaP prostate cancer cells. Carcinogenesis 2001, 22, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Galindo, P.; Manzano, S.G.; Zarzuelo, M.J.; Gómez-Guzmán, M.; Quintela, A.M.; González-Paramás, A.; Santos-Buelga, C.; Perez-Vizcaino, F.; Duarte, J.; Jimenez, R. Different cardiovascular protective effects of quercetin administered orally or intraperitoneally in spontaneously hypertensive rats. Food Funct. 2012, 3, 643. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, M.; Galisteo, M.; Vera, R.; Villar, I.C.; Zarzuelo, A.; Tamargo, J.; Perez-Vizcaino, F.; Duarte, J. Quercetin downregulates NADPH oxidase, increases eNOS activity and prevents endothelial dysfunction in spontaneously hypertensive rats. J. Hypertens. 2006, 24, 75–84. [Google Scholar] [CrossRef]
- Booyse, F.M.; Pan, W.; Grenett, H.E.; Parks, D.A.; Darley-Usmar, V.; Bradley, K.M.; Tabengwa, E.M. Mechanism by which Alcohol and Wine Polyphenols Affect Coronary Heart Disease Risk. Ann. Epidemiol. 2007, 17, S24–S31. [Google Scholar] [CrossRef]
- Edwards, R.L.; Lyon, T.; Litwin, S.E.; Rabovsky, A.; Symons, J.D.; Jalili, T. Quercetin Reduces Blood Pressure in Hypertensive Subjects. J. Nutr. 2007, 137, 2405–2411. [Google Scholar] [CrossRef]
- Mamani-Matsuda, M.; Kauss, T.; Al-Kharrat, A.; Rambert, J.; Fawaz, F.; Thiolat, D.; Moynet, D.; Coves, S.; Malvy, D.; Mossalayi, M.D. Therapeutic and preventive properties of quercetin in experimental arthritis correlate with decreased macrophage inflammatory mediators. Biochem. Pharmacol. 2006, 72, 1304–1310. [Google Scholar] [CrossRef]
- Rogerio, A.D.P.; Kanashiro, A.; Fontanari, C.; Da Silva, E.V.G.; Lucisano-Valim, Y.M.; Soares, E.G.; Faccioli, L.H. Anti-inflammatory activity of quercetin and isoquercitrin in experimental murine allergic asthma. Inflamm. Res. 2007, 56, 402–408. [Google Scholar] [CrossRef]
- Min, Y.-D.; Choi, C.-H.; Bark, H.; Son, H.-Y.; Park, H.-H.; Lee, S.; Park, J.-W.; Park, E.-K.; Shin, H.-I.; Kim, S.-H. Quercetin inhibits expression of inflammatory cytokines through attenuation of NF-κB and p38 MAPK in HMC-1 human mast cell line. Inflamm. Res. 2007, 56, 210–215. [Google Scholar] [CrossRef]
- Kimata, M.; Shichijo, M.; Miura, T.; Serizawa, I.; Inagaki, N.; Nagai, H. Effects of luteolin, quercetin and baicalein on immunoglobulin E-mediated mediator release from human cultured mast cells. Clin. Exp. Allergy 2000, 30, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Afanas’Ev, I.B.; Dcrozhko, A.I.; Brodskii, A.V.; Kostyuk, V.; Potapovitch, A.I. Chelating and free radical scavenging mechanisms of inhibitory action of rutin and quercetin in lipid peroxidation. Biochem. Pharmacol. 1989, 38, 1763–1769. [Google Scholar] [CrossRef]
- Van Acker, S.A.; van Balen, G.P.; Berg, D.-J.V.D.; Bast, A.; van der Vijgh, W.J. Influence of iron chelation on the antioxidant activity of flavonoids. Biochem. Pharmacol. 1998, 56, 935–943. [Google Scholar] [CrossRef]
- Harwood, M.; Danielewska-Nikiel, B.; Borzelleca, J.; Flamm, G.; Williams, G.; Lines, T. A critical review of the data related to the safety of quercetin and lack of evidence of in vivo toxicity, including lack of genotoxic/carcinogenic properties. Food Chem. Toxicol. 2007, 45, 2179–2205. [Google Scholar] [CrossRef] [PubMed]
- Kim, G.-N.; Jang, H.-D. Protective Mechanism of Quercetin and Rutin Using Glutathione Metabolism on H2O2-induced Oxidative Stress in HepG2 Cells. Ann. N. Y. Acad. Sci. 2009, 1171, 530–537. [Google Scholar] [CrossRef]
- Chen, J.-C.; Ho, F.-M.; Chao, P.-D.L.; Chen, C.-P.; Jeng, K.-C.G.; Hsu, H.-B.; Lee, S.-T.; Wu, W.T.; Lin, W.W. Inhibition of iNOS gene expression by quercetin is mediated by the inhibition of IκB kinase, nuclear factor-kappa B and STAT1, and depends on heme oxygenase-1 induction in mouse BV-2 microglia. Eur. J. Pharmacol. 2005, 521, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Heo, H.J.; Lee, C.Y. Protective Effects of Quercetin and Vitamin C against Oxidative Stress-Induced Neurodegeneration. J. Agric. Food Chem. 2004, 52, 7514–7517. [Google Scholar] [CrossRef]
- Zhang, Z.J.; Cheang, L.C.; Wang, M.W.; Lee, S.M. Quercetin exerts a neuroprotective effect through inhibition of the iNOS/NO system and pro-inflammation gene expression in PC12 cells and in zebrafish. Int. J. Mol. Med. 2011, 27, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Dok-Go, H.; Lee, K.H.; Kim, H.J.; Lee, E.H.; Lee, J.; Song, Y.S.; Lee, Y.H.; Jin, C.; Lee, Y.S.; Cho, J. Neuroprotective effects of antioxidative flavonoids, quercetin, (+)-dihydroquercetin and quercetin 3-methyl ether, isolated from Opuntia ficus-indica var. saboten. Brain Res. 2003, 965, 130–136. [Google Scholar] [CrossRef]
- Sagara, Y.; Vanhnasy, J.; Maher, P. Induction of PC12 cell differentiation by flavonoids is dependent upon extracellular signal-regulated kinase activation. J. Neurochem. 2004, 90, 1144–1155. [Google Scholar] [CrossRef]
- Ansari, M.A.; Abdul, H.M.; Joshi, G.; Opii, W.O.; Butterfield, D.A. Protective effect of quercetin in primary neurons against Aβ(1–42): Relevance to Alzheimer’s disease. J. Nutr. Biochem. 2009, 20, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Park, B.-S.; Lee, K.-G.; Choi, C.Y.; Jang, S.S.; Kim, Y.-H.; Lee, S.-E. Effects of Naturally Occurring Compounds on Fibril Formation and Oxidative Stress of β-Amyloid. J. Agric. Food Chem. 2005, 53, 8537–8541. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.M.; Murphy, E.A.; Carmichael, M.D.; Davis, B. Quercetin increases brain and muscle mitochondrial biogenesis and exercise tolerance. Am. J. Physiol. Integr. Comp. Physiol. 2009, 296, R1071–R1077. [Google Scholar] [CrossRef]
- Sharma, V.; Mishra, M.; Ghosh, S.; Tewari, R.; Basu, A.; Seth, P.; Sen, E. Modulation of interleukin-1β mediated inflammatory response in human astrocytes by flavonoids: Implications in neuroprotection. Brain Res. Bull. 2007, 73, 55–63. [Google Scholar] [CrossRef]
- Priprem, A.; Watanatorn, J.; Sutthiparinyanont, S.; Phachonpai, W.; Muchimapura, S. Anxiety and cognitive effects of quercetin liposomes in rats. Nanomedicine 2008, 4, 70–78. [Google Scholar] [CrossRef]
- Shaji, J.; Iyer, S. Preparation, optimization and in-vivo hepatoprotective evaluation of quercetin liposomes. Int. J. Curr. Pharm. Res. 2012, 4, 24–32. [Google Scholar]
- Yuan, Z.-P.; Chen, L.-J.; Fan, L.-Y.; Tang, M.-H.; Yang, G.-L.; Yang, H.-S.; Du, X.-B.; Wang, G.-Q.; Yao, W.-X.; Zhao, Q.-M.; et al. Liposomal Quercetin Efficiently Suppresses Growth of Solid Tumors in Murine Models. Clin. Cancer Res. 2006, 12, 3193–3199. [Google Scholar] [CrossRef]
- Long, Q.; Xiel, Y.; Huang, Y.; Wu, Q.; Zhang, H.; Xiong, S.; Liu, Y.; Chen, L.; Wei, Y.; Zhao, X.; et al. Induction of Apoptosis and Inhibition of Angiogenesis by PEGylated Liposomal Quercetin in Both Cisplatin-Sensitive and Cisplatin-Resistant Ovarian Cancers. J. Biomed. Nanotechnol. 2013, 9, 965–975. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Hu, H.; Lin, Z.; Chen, D.; Zhu, Y.; Hou, S.; Shi, X. Quercetin deformable liposome: Preparation and efficacy against ultraviolet B induced skin damages in vitro and in vivo. J. Photochem. Photobiol. B 2013, 127, 8–17. [Google Scholar] [CrossRef]
- Wong, M.-Y.; Chiu, G.N. Liposome formulation of co-encapsulated vincristine and quercetin enhanced antitumor activity in a trastuzumab-insensitive breast tumor xenograft model. Nanomedicine 2011, 7, 834–840. [Google Scholar] [CrossRef]
- Goniotaki, M.; Hatziantoniou, S.; Dimas, K.; Wagner, M.; Demetzos, C. Encapsulation of naturally occurring flavonoids into liposomes: Physicochemical properties and biological activity against human cancer cell lines. J. Pharm. Pharmacol. 2010, 56, 1217–1224. [Google Scholar] [CrossRef]
- Caddeo, C.; Gabriele, M.; Fernàndez-Busquets, X.; Valenti, D.; Fadda, A.M.; Pucci, L.; Manconi, M. Antioxidant activity of quercetin in Eudragit-coated liposomes for intestinal delivery. Int. J. Pharm. 2019, 565, 64–69. [Google Scholar] [CrossRef]
- Li, H.; Zhao, X.; Ma, Y.; Zhai, G.; Li, L.; Lou, H. Enhancement of gastrointestinal absorption of quercetin by solid lipid nanoparticles. J. Control. Release 2009, 133, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Chen-Yu, G.; Chun-Fen, Y.; Qi-Lu, L.; Qi, T.; Yan-Wei, X.; Wei-Na, L.; Guang-Xi, Z. Development of a Quercetin-loaded nanostructured lipid carrier formulation for topical delivery. Int. J. Pharm. 2012, 430, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Du, Y.; Takhistov, P.; Michniak-Kohn, B. Formulation optimization and topical delivery of quercetin from solid lipid based nanosystems. Int. J. Pharm. 2013, 441, 56–66. [Google Scholar] [CrossRef]
- Sun, M.; Nie, S.; Pan, X.; Zhang, R.; Fan, Z.; Wang, S. Quercetin-nanostructured lipid carriers: Characteristics and anti-breast cancer activities in vitro. Colloids Surf. B Biointerfaces 2014, 113, 15–24. [Google Scholar] [CrossRef]
- Dhawan, S.; Kapil, R.; Singh, B. Formulation development and systematic optimization of solid lipid nanoparticles of quercetin for improved brain delivery. J. Pharm. Pharmacol. 2011, 63, 342–351. [Google Scholar] [CrossRef]
- Rishitha, N.; Muthuraman, A. Therapeutic evaluation of solid lipid nanoparticle of quercetin in pentylenetetrazole induced cognitive impairment of zebrafish. Life Sci. 2018, 199, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, R.; Granja, A.; Loureiro, J.; Pereira, M.; Pinheiro, M.; Neves, A.; Reis, S. Quercetin lipid nanoparticles functionalized with transferrin for Alzheimer’s disease. Eur. J. Pharm. Sci. 2020, 148, 105314. [Google Scholar] [CrossRef]
- Pinheiro, R.; Granja, A.; Loureiro, J.; Pereira, M.; Pinheiro, M.; Neves, A.; Reis, S. RVG29-Functionalized Lipid Nanoparticles for Quercetin Brain Delivery and Alzheimer’s Disease. Pharm. Res. 2020, 37, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kumari, A.; Yadav, S.K.; Pakade, Y.B.; Singh, B.; Yadav, S.C. Development of biodegradable nanoparticles for delivery of quercetin. Colloids Surf. B Biointerfaces 2010, 80, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Khoee, S.; Rahmatolahzadeh, R. Synthesis and characterization of pH-responsive and folated nanoparticles based on self-assembled brush-like PLGA/PEG/AEMA copolymer with targeted cancer therapy properties: A comprehensive kinetic study. Eur. J. Med. Chem. 2012, 50, 416–427. [Google Scholar] [CrossRef]
- Elgogary, R.; Rubio, N.; Wang, T.-W.; Al-Jamal, W.T.; Bourgognon, M.; Kafa, H.; Naeem, M.; Klippstein, R.; Abbate, V.; Leroux, F.; et al. Polyethylene Glycol Conjugated Polymeric Nanocapsules for Targeted Delivery of Quercetin to Folate-Expressing Cancer Cells in Vitro and in Vivo. ACS Nano 2014, 8, 1384–1401. [Google Scholar] [CrossRef]
- Bishayee, K.; Khuda-Bukhsh, A.R.; Huh, A.S.-O. PLGA-Loaded Gold-Nanoparticles Precipitated with Quercetin Downregulate HDAC-Akt Activities Controlling Proliferation and Activate p53-ROS Crosstalk to Induce Apoptosis in Hepatocarcinoma Cells. Mol. Cells 2015, 38, 518–527. [Google Scholar] [CrossRef]
- Pandey, S.K.; Patel, D.K.; Thakur, R.; Mishra, D.P.; Maiti, P.; Haldar, C. Anti-cancer evaluation of quercetin embedded PLA nanoparticles synthesized by emulsified nanoprecipitation. Int. J. Biol. Macromol. 2015, 75, 521–529. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Li, N.; Zhang, W.; Zhao, Z.; Mou, Z.; Huang, D.; Liu, J.; Wang, W. Design of PLGA-functionalized quercetin nanoparticles for potential use in Alzheimer’s disease. Colloids Surf. B Biointerfaces 2016, 148, 116–129. [Google Scholar] [CrossRef]
- Suksiriworapong, J.; Phoca, K.; Ngamsom, S.; Sripha, K.; Moongkarndi, P.; Junyaprasert, V.B. Comparison of poly(ε-caprolactone) chain lengths of poly(ε-caprolactone)-co-d-α-tocopheryl-poly(ethylene glycol) 1000 succinate nanoparticles for enhancement of quercetin delivery to SKBR3 breast cancer cells. Eur. J. Pharm. Biopharm. 2016, 101, 15–24. [Google Scholar] [CrossRef]
- Zhu, X.; Zeng, X.; Zhang, X.; Cao, W.; Wang, Y.; Chen, H.; Wang, T.; Tsai, H.-I.; Zhang, R.; Chang, D.; et al. The effects of quercetin-loaded PLGA-TPGS nanoparticles on ultraviolet B-induced skin damages in vivo. Nanomedicine 2016, 12, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Sunoqrot, S.; Abujamous, L. pH-sensitive polymeric nanoparticles of quercetin as a potential colon cancer-targeted nanomedicine. J. Drug Deliv. Sci. Technol. 2019, 52, 670–676. [Google Scholar] [CrossRef]
- Pedro, R.D.O.; Goycoolea, F.M.; Pereira, S.; Schmitt, C.C.; Neumann, M.G. Synergistic effect of quercetin and pH-responsive DEAE-chitosan carriers as drug delivery system for breast cancer treatment. Int. J. Biol. Macromol. 2018, 106, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.-X.; Li, X.-X.; Chen, L.; Li, L.; Janaswamy, S. Carriers Based on Zein-Dextran Sulfate Sodium Binary Complex for the Sustained Delivery of Quercetin. Front. Chem. 2020, 8, 662. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Pérez, A.A.; Rivero, H.C.; Hernández, M.D.C.P.; Pagán, A.; Montalbán, M.G.; Víllora, G.; Cénis, J.L. Silk fibroin nanoparticles: Efficient vehicles for the natural antioxidant quercetin. Int. J. Pharm. 2017, 518, 11–19. [Google Scholar] [CrossRef]
- Diez-Echave, P.; Ruiz-Malagón, A.J.; Molina-Tijeras, J.A.; Hidalgo-García, L.; Vezza, T.; Cenis-Cifuentes, L.; Rodríguez-Sojo, M.J.; Cenis, J.L.; Rodríguez-Cabezas, M.E.; Rodríguez-Nogales, A.; et al. Silk fibroin nanoparticles enhance quercetin immunomodulatory properties in DSS-induced mouse colitis. Int. J. Pharm. 2021, 606, 120935. [Google Scholar] [CrossRef]
- Pedro, R.D.O.; Pereira, S.; Goycoolea, F.M.; Schmitt, C.C.; Neumann, M.G. Self-aggregated nanoparticles of N -dodecyl,N ′-glycidyl(chitosan) as pH-responsive drug delivery systems for quercetin. J. Appl. Polym. Sci. 2018, 135, 45678. [Google Scholar] [CrossRef]
- Barreto, A.C.H.; Santiago, V.R.; Mazzetto, S.E.; Denardin, J.C.; Lavín, R.; Mele, G.; Ribeiro, M.E.N.P.; Vieira, I.G.P.; Gonçalves, T.; Ricardo, N.M.P.S.; et al. Magnetic nanoparticles for a new drug delivery system to control quercetin releasing for cancer chemotherapy. J. Nanoparticle Res. 2011, 13, 6545–6553. [Google Scholar] [CrossRef]
- Verma, N.K.; Crosbie-Staunton, K.; Satti, A.; Gallagher, S.; Ryan, K.B.; Doody, T.; McAtamney, C.; MacLoughlin, R.; Galvin, P.; Burke, C.S.; et al. Magnetic core-shell nanoparticles for drug delivery by nebulization. J. Nanobiotechnol. 2013, 11, 1. [Google Scholar] [CrossRef]
- Kumar, S.R.; Priyatharshni, S.; Babu, V.; Mangalaraj, D.; Viswanathan, C.; Kannan, S.; Ponpandian, N. Quercetin conjugated superparamagnetic magnetite nanoparticles for in-vitro analysis of breast cancer cell lines for chemotherapy applications. J. Colloid Interface Sci. 2014, 436, 234–242. [Google Scholar] [CrossRef]
- Akal, Z.; Alpsoy, L.; Baykal, A. Superparamagnetic iron oxide conjugated with folic acid and carboxylated quercetin for chemotherapy applications. Ceram. Int. 2016, 42, 9065–9072. [Google Scholar] [CrossRef]
- Sapino, S.; Ugazio, E.; Gastaldi, L.; Miletto, I.; Berlier, G.; Zonari, D.; Oliaro-Bosso, S. Mesoporous silica as topical nanocarriers for quercetin: Characterization and in vitro studies. Eur. J. Pharm. Biopharm. 2015, 89, 116–125. [Google Scholar] [CrossRef]
- Sarkar, A.; Ghosh, S.; Chowdhury, S.; Pandey, B.; Sil, P.C. Targeted delivery of quercetin loaded mesoporous silica nanoparticles to the breast cancer cells. Biochim. Biophys. Acta BBA 2016, 1860, 2065–2075. [Google Scholar] [CrossRef] [PubMed]
- Jullian, C.; Moyano, L.; Yañez, C.; Olea-Azar, C. Complexation of quercetin with three kinds of cyclodextrins: An antioxidant study. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2007, 67, 230–234. [Google Scholar] [CrossRef]
- Liu, M.; Dong, L.; Chen, A.; Zheng, Y.; Sun, D.; Wang, X.; Wang, B. Inclusion complexes of quercetin with three β-cyclodextrins derivatives at physiological pH: Spectroscopic study and antioxidant activity. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2013, 115, 854–860. [Google Scholar] [CrossRef]
- Aytac, Z.; Kusku, S.I.; Durgun, E.; Uyar, T. Quercetin/β-cyclodextrin inclusion complex embedded nanofibres: Slow release and high solubility. Food Chem. 2016, 197, 864–871. [Google Scholar] [CrossRef]
- Kale, R.; Saraf, M.; Juvekar, A.; Tayade, P. Decreased B16F10 melanoma growth and impaired tumour vascularization in BDF1 mice with quercetin-cyclodextrin binary system. J. Pharm. Pharmacol. 2010, 58, 1351–1358. [Google Scholar] [CrossRef]
- Akbarzadeh, A.; Rezaei-Sadabady, R.; Davaran, S.; Joo, S.W.; Zarghami, N.; Hanifehpour, Y.; Samiei, M.; Kouhi, M.; Nejati-Koshki, K. Liposome: Classification, preparation, and applications. Nanoscale Res. Lett. 2013, 8, 102. [Google Scholar] [CrossRef] [PubMed]
- Immordino, M.L.; Dosio, F.; Cattel, L. Stealth liposomes: Review of the basic science, rationale, and clinical applications, existing and potential. Int. J. Nanomed. 2006, 1, 297–315. [Google Scholar]
- Phachonpai, W.; Wattanathorn, J.; Muchimapura, S.; Tong-Un, T.; Preechagoon, D. Neuroprotective Effect of Quercetin Encapsulated Liposomes: A Novel Therapeutic Strategy against Alzheimer’s Disease. Am. J. Appl. Sci. 2010, 7, 480–485. [Google Scholar] [CrossRef]
- Weber, S.; Zimmer, A.; Pardeike, J. Solid Lipid Nanoparticles (SLN) and Nanostructured Lipid Carriers (NLC) for pulmonary application: A review of the state of the art. Eur. J. Pharm. Biopharm. 2014, 86, 7–22. [Google Scholar] [CrossRef] [PubMed]
- Wissing, S.; Kayser, O.; Müller, R. Solid lipid nanoparticles for parenteral drug delivery. Adv. Drug Deliv. Rev. 2004, 56, 1257–1272. [Google Scholar] [CrossRef] [PubMed]
- Mehnert, W. Solid lipid nanoparticles Production, characterization and applications. Adv. Drug Deliv. Rev. 2001, 47, 165–196. [Google Scholar] [CrossRef]
- Rieux, A.D.; Fievez, V.; Garinot, M.; Schneider, Y.-J.; Préat, V. Nanoparticles as potential oral delivery systems of proteins and vaccines: A mechanistic approach. J. Control. Release 2006, 116, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Hu, M.J.; Wang, Y.Q.; Cui, Y.L. Antioxidant Activities of Quercetin and Its Complexes for Medicinal Application. Molecules 2019, 24, 1123. [Google Scholar] [CrossRef]
- Quiñones, J.P.; Peniche, H.; Peniche, C. Chitosan Based Self-Assembled Nanoparticles in Drug Delivery. Polymers 2018, 10, 235. [Google Scholar] [CrossRef]
- Alexiou, C.; Schmid, R.J.; Jurgons, R.; Kremer, M.; Wanner, G.; Bergemann, C.; Huenges, E.; Nawroth, T.; Arnold, W.; Parak, F.G. Targeting cancer cells: Magnetic nanoparticles as drug carriers. Eur. Biophys. J. 2006, 35, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Lu, A.-H.; Salabas, E.-L.; Schüth, F. Magnetic Nanoparticles: Synthesis, Protection, Functionalization, and Application. Angew. Chem. Int. Ed. 2007, 46, 1222–1244. [Google Scholar] [CrossRef]
- Cauda, V.; Mühlstein, L.; Onida, B.; Bein, T. Tuning drug uptake and release rates through different morphologies and pore diameters of confined mesoporous silica. Microporous Mesoporous Mater. 2009, 118, 435–442. [Google Scholar] [CrossRef]
- Vallet-Regí, M.; Balas, F.; Arcos, D. Mesoporous Materials for Drug Delivery. Angew. Chem. Int. Ed. 2007, 46, 7548–7558. [Google Scholar] [CrossRef]
- Manzano, M.; Colilla, M.; Vallet-Regí, M. Drug delivery from ordered mesoporous matrices. Expert Opin. Drug Deliv. 2009, 6, 1383–1400. [Google Scholar] [CrossRef]
- Di Pasqua, A.J.; Sharma, K.K.; Shi, Y.-L.; Toms, B.B.; Ouellette, W.; Dabrowiak, J.C.; Asefa, T. Cytotoxicity of mesoporous silica nanomaterials. J. Inorg. Biochem. 2008, 102, 1416–1423. [Google Scholar] [CrossRef]
- Lu, J.; Liong, M.; Li, Z.; Zink, J.I.; Tamanoi, F. Biocompatibility, Biodistribution, and Drug-Delivery Efficiency of Mesoporous Silica Nanoparticles for Cancer Therapy in Animals. Small 2010, 6, 1794–1805. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Sun, C.; Mao, L.; Ma, P.; Liu, F.; Yang, J.; Gao, Y. The biological activities, chemical stability, metabolism and delivery systems of quercetin: A review. Trends Food Sci. Technol. 2016, 56, 21–38. [Google Scholar] [CrossRef]
- Lucas-Abellán, C.; Fortea, I.; López-Nicolás, J.M.; Núñez-Delicado, E. Cyclodextrins as resveratrol carrier system. Food Chem. 2007, 104, 39–44. [Google Scholar] [CrossRef]
- Han, M.K.; Barreto, T.A.; Martinez, F.J.; Comstock, A.T.; Sajjan, U.S. Randomised clinical trial to determine the safety of quercetin supplementation in patients with chronic obstructive pulmonary disease. BMJ Open Respir. Res. 2020, 7, e000392. [Google Scholar] [CrossRef] [PubMed]
- ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ (accessed on 8 October 2021).
- Saeedi-Boroujeni, A.; Mahmoudian-Sani, M.-R. Anti-inflammatory potential of Quercetin in COVID-19 treatment. J. Inflamm. 2021, 18, 1–9. [Google Scholar] [CrossRef]
- Beneficial Effects of Quercetin in Chronic Obstructive Pulmonary Disease (COPD) (Quercetin). Available online: https://clinicaltrials.gov/show/NCT01708278 (accessed on 8 October 2021).
- Vafadar, A.; Shabaninejad, Z.; Movahedpour, A.; Fallahi, F.; Taghavipour, M.; Ghasemi, Y.; Akbari, M.; Shafiee, A.; Hajighadimi, S.; Moradizarmehri, S.; et al. Quercetin and cancer: New insights into its therapeutic effects on ovarian cancer cells. Cell Biosci. 2020, 10, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Ferenczyova, K.; Kalocayova, B.; Bartekova, M. Potential Implications of Quercetin and its Derivatives in Cardioprotection. Int. J. Mol. Sci. 2020, 21, 1585. [Google Scholar] [CrossRef] [PubMed]
- Boots, A.W.; Veith, C.; Albrecht, C.; Bartholome, R.; Drittij, M.-J.; Claessen, S.M.H.; Bast, A.; Rosenbruch, M.; Jonkers, L.; van Schooten, F.-J.; et al. The dietary antioxidant quercetin reduces hallmarks of bleomycin-induced lung fibrogenesis in mice. BMC Pulm. Med. 2020, 20, 112. [Google Scholar] [CrossRef]
- Li, Y.; Yao, J.; Han, C.; Yang, J.; Chaudhry, M.T.; Wang, S.; Liu, H.; Yin, Y. Quercetin, Inflammation and Immunity. Nutrients 2016, 8, 167. [Google Scholar] [CrossRef] [PubMed]
- Chondrogianni, N.; Kapeta, S.; Chinou, I.; Vassilatou, K.; Papassideri, I.; Gonos, E.S. Anti-ageing and rejuvenating effects of quercetin. Exp. Gerontol. 2010, 45, 763–771. [Google Scholar] [CrossRef] [PubMed]

| Sources | Total Quercetin (mg/Kg) |
|---|---|
| White onion bulbs | 2604 |
| Onion dry outer skin | 960 |
| Spring onion leaves | 450 |
| Chili powder | 400 |
| Bog whortleberry | 158 |
| Lingonberry | 146 |
| Cranberry | 121 |
| Kale | 110 |
| Chokeberry | 89 |
| Sweet rowan | 85 |
| Rowanberry | 63 |
| Sea buckthorn berry | 62 |
| Apples red delicious | 58 |
| Crowberry | 56 |
| Broccoli | 30 |
| Green beans | 25 |
| Apple peel | 21 |
| Tomato | 13 |
| NPs Type | Composition | Morphology | Particle Size (nm) | Zeta Potential (mV) | Encapsulation Efficiency (EE) (%) | Administration Route | In Vitro/In Vivo Results | Reference |
|---|---|---|---|---|---|---|---|---|
| Liposomes | PC/Chol; EPC/Chol/PEG; lecithin/Chol/PEG; ESM/Chol/PEG P90G/STA/Eudragit S100 | spherical | 90 to 450 | +7 to −30 | 65 to 95 | oral, intranasal, intravenous, topical | - anxiolytic and cognitive-enhancing effects in rats (in vivo); - hepatoprotective effects in rodents (in vivo); - attenuation of edema and inflammation in irradiated mice (in vivo); - inhibition of tumor angiogenesis, inhibition of tumor cell growth and induction of tumor cell apoptosis (cell lines and mice) (in vitro and in vivo); - protection against intestinal oxidative stress in intestinal cell lines (in vitro); | [78,79,80,81,82,83,84,85] |
| Lipid nanoparticles | GMS/soya lecithin/PEG; GMS/SA/MCT/soya lecithin; Compritol; GT/TG/soya lecithin SA/P-188; cetyl palmitate, mygliol-812 and tween 80 | spherical | 35 to 550 | −10 to −35 | 75 to 95 | oral, intravenous, topical, intraperitoneal | - enhancement of the oral absorption in rats (in vivo); - increase of drug penetration in skin and anti-oxidation and anti-inflammation effect (in vivo); - improvement of memory retention in rats with aluminum-induced dementia (in vivo); - induction of tumor cell apoptosis in breast cancer cell lines (in vitro). - improvements of cognition and memory impairments in zebrafish model of neurodegenerative disorders (in vivo). - inhibition of amyloid-beta aggregation and fibril formation in vitro, being suitable for brain applications (in vitro). | [86,87,88,89,90,91,92,93] |
| Polymeric nanoparticles | PLA; PLGA; PLGA/PEG/AEMA; PLGA/PEG/FA; PCL/TPGS; PLGA/TPGS Eudragit S100 L-CS/DEAE | spherical, bean-like shape | 30 to 415 | +42 to −40 | 40 to 98 | intravenous, topical | - enhancement of cancer cell uptake in tumor-bearing mice (in vivo); - increase of cytotoxicity and induction of apoptosis in breast, colon and liver hepatocellular carcinoma cell lines (in vitro); - block/reduce of histological alterations in irradiated mice (in vivo); - enhancement of neuron cells viability due to inhibition of aβ-42 peptide neurotoxicity in cell lines (in vitro); - improvements of cognition and memory impairments in APP/PS1 mice model of Alzheimer’s disease (in vivo). | [94,95,96,97,98,99,100,101,102,103] |
| Biopolymeric nanoparticles | Zein-Dextran sulfate sodium; Skin Fibroin; Chitosan | spherical | 140 to 300 | −16 to −39; +14 to +30 | 20 to 78 | oral, intravenous | - promising favorable and sustained delivery of quercetin (in vitro); - controlled release in the pH of intestinal fluid; suitable for gastrointestinal delivery (in vitro); - improving pathological inflammation and preserving normal crypt architecture in model mouse of colitis (in vivo); - pH-responsive sustained release for cancer therapy; reducing side effects upon systematic administration (in vitro). | [104,105,106,107] |
| Magnetic nanoparticles | Fe3O4; Fe3O4/E137S18E137; Fe3O4/APTS/PEG/FA; Fe3O4/PLGA | spherical | 10 to 300 | around +6 | around 80 | intranasal | - induction of cytotoxicity in human lung carcinoma, breast cancer and glioblastoma cell lines (in vitro). | [108,109,110,111] |
| Mesoporous silica nanoparticles | TEOS/APTS; TEOS/FA | spherical | 200 to 250 | −25 to +13 | around 99 | n.i. | - inhibition of tumor cell proliferation and induction of tumor cell apoptosis (cell lines) (in vitro). | [112,113] |
| Cyclodextrins | βCD; HP-βCD; SBE-βCD; SBE-7βCD | truncated cone; fibers | around 270 | n.i. | n.i. | oral | - increase of quercetin solubility and photostability; - enhancement of quercetin antioxidant capacity (in vivo); - inhibition of tumor cell proliferation in cell lines (in vitro); - impairment of tumor growth in B16F10 mouse melanoma model (in vivo). | [114,115,116,117] |
| Country | Study | Condition | Intervention | Phase | Status | Results |
|---|---|---|---|---|---|---|
| U.S.—Michigan | Phase I Study to Determine the Safety of Quercetin in COPD Patients | Chronic Obstructive Pulmonary Disease | Quercetin | 1 | Completed with results | Decreased lung inflammation and prevented progression |
| U.S.—Massachusetts | Hypoxia-inducible Transcription Factor 1 (HIF-1) in Vascular Aging |
Stroke; Problem of Aging | Quercetin | Early phase 1 | completed | Not Indicated |
| U.S.—Ohio | Quercetin in Children with Fanconi Anemia; a Pilot Study | Fanconi Anemia | Quercetin | 1 | Recruiting | There are no results |
| U.S.—North Carolina | Can Quercetin Increase Claudin-4 and Improve Esophageal Barrier Function in GERD? |
Gastroesophageal Reflux Disease (GERD); Acid Reflux; Reflux | quercetin | 1 | completed | Not indicated |
| U.S.—California | A Phase 1 Study of Quercetin in Patients with Hepatitis C | Chronic Hepatitis C | quercetin | 1 | completed | Not indicated |
| The Netherlands | The Effect of Quercetin on the Increased Inflammatory and Decreased Antioxidant Status in Sarcoidosis | Sarcoidosis | quercetin | - | completed | Not indicated |
| The Netherlands | Study on the Effects of Epicatechin and Quercetin Supplementation on Vascular Function and Blood Pressure in Untreated (Pre)Hypertensive Subjects |
Hypertension Endothelial Dysfunction | Epicatechin; quercetin | - | completed | Not indicated |
| Islamic Republic of Iran | Effect of Quercetin in Prevention and Treatment of Chemotherapy Induced Oral Mucositis in Blood Dyscrasias | Chemotherapy Induced Oral Mucositis | oral quercetin capsules | 1,2 | completed | Not indicated |
| U.S.—New Mexico | Effect of Combined Exercise, Heat, and Quercetin Supplementation on Whole Body Stress Response | Heat Acclimation and Thermotolerance | Quercetin | - | completed | Not indicated |
| U.S.—California | Phase I Randomized, Double-Blind, Placebo-Controlled Two-Arm Study of Quercetin and Green Tea to Enhance the Bioavailability of Green Tea Polyphenols in Men Scheduled for Prostatectomy |
Adenocarcinoma of the Prostate; Recurrent Prostate Cancer; Stage I Prostate Cancer; Stage IIA Prostate Cancer; Stage IIB Prostate Cancer; Stage III Prostate Cancer; Stage IV Prostate Cancer; | Dietary Supplement: green tea extract Drug: quercetin Other: placebo Procedure: therapeutic conventional surgery Other: laboratory biomarker analysis | 1 | Active, not recruiting | There are no results |
| U.S.—Massachusetts | Pharmacokinetic and Pharmacodynamic Study of Oral Quercetin and Isoquercetin in Healthy Adults and Patients with Elevated Anti-phospholipid Antibodies | Healthy | Drug: isoquercetin or quercetin | - | Active, not recruiting | There are no results |
| U.S.—Washington | Evaluation of Quercetin in Type 2 Diabetes: Impact on Glucose Tolerance and Postprandial Endothelial Function. | Diabetes Mellitus, Type 2 | Dietary Supplement: Quercetin Drug: Acarbose Drug: placebo | 2 | completed | Not indicated |
| Islamic Republic of Iran | Therapeutic Effect of Quercetin and the Current Treatment of Erosive and Atrophic Oral Lichen Planus |
Atrophic Oral Lichen Planus; Erosive Oral Lichen Planus | Drug: placebo Drug: Quercetin | 1 | unknow | There is no information |
| Germany | Clinical Trial on the Effectiveness of the Flavonoids Genistein and Quercetin in Men with Rising Prostate-specific Antigen | Primary Prevention of Prostate Cancer | Dietary Supplement: Quercetin supplement Dietary Supplement: Genistein supplement Dietary Supplement: Placebo | - | unknown | There is no information |
| U.S.—Texas | Prospective Open Labeled Pilot Trial of Quercetin in the Treatment and Prevention of Chemotherapy-induced Neuropathic Pain in Cancer Patients | Polyneuropathies and Other Disorders of the Peripheral Nervous System Chemotherapy Induced Neuropathic Pain | Behavioral: Questionnaires Drug: Quercetin | Early Phase 1 | Not yet recruiting | There are no results |
| U.S.—Maryland | Inhibition of Intestinal Glucose Absorption by the Bioflavonoid Quercetin in the Obese and in Obese Type 2 Diabetics |
Diabetes Mellitus; Obesity |
Procedure: Oral glucose tolerance test; coadministration of 1 or 2 g of quercetin with glucose | 2 | recruiting | There are no results |
| United Kingdom | A Double-Blind, Cross-Over, Placebo-Controlled Study Evaluating the Effect of Quercetin 500 mg Tablets on Blood Uric Acid in Healthy Males |
Hyperuricemia; Gout; Kidney Calculi; Diabetes; Cardiovascular Disease |
Dietary Supplement: Treatment Dietary Supplement: Control | Early Phase 1 | completed | There are no results |
| U.S.—Pennsylvania | Advancing Niacin by Inhibiting FLUSHing: (ANTI-FLUSH) | Flushing | Dietary Supplement: Quercetin Dietary Supplement: Placebo | 4 | Completed, has results | Not indicated |
| Greece | Effects of the Anti-inflammatory Flavonoid Luteolin on Behavior in Children with Autism Spectrum Disorders | Autism Spectrum Disorders | Dietary Supplement: Luteolin, Quercetin and Rutin combined in a capsule | 2 | completed | There are no results |
| U.S.—Alabama | Nasal Potential Studies Utilizing CFTR Modulators (UAB Center for Clinical and Translational Science) | Cystic Fibrosis | Other: quercetin | 2 | completed | There are no results |
| U.S.—North Carolina | Targeted Removal of Pro-Inflammatory Cells: An Open Label Human Pilot Study in Idiopathic Pulmonary Fibrosis | Idiopathic Pulmonary Fibrosis (IPF) | Drug: Dasatinib + Quercetin | 1 | recruiting | There are no results |
| U.S.—Minnesota | Senescence, Frailty, and Mesenchymal Stem Cell Functionality in Chronic Kidney Disease: Effect of Senolytic Agents | Chronic Kidney Disease | Drug: Group 2: Dasatinib Drug: Group 2: Quercetin | 2 | recruiting | There are no results |
| U.S.—Minnesota | Hematopoietic Stem Cell Transplant Survivors Study (HTSS Study) | Stem Cell Transplant | Drug: Quercetin Other: Standard of Care—Observation Only Drug: Dasatinib | - | recruiting | There are no results |
| U.S.—Utah | A Double-Blind, Placebo-Controlled, Crossover Evaluation of a Grape Seed Extract and Quercetin Supplement (Provex CV) to Reduce Markers of Inflammatory Cytokines and Blood Pressure in Subjects with Metabolic Syndrome | Blood Pressure |
Drug: Provex CV Other: placebo | 1 | Completed | There are no results |
| U.S.—New York | The Effect of Plant Phenolic Compounds on Human Colon Epithelial Cells | Colorectal Cancer | Dietary Supplement: curcumin Dietary Supplement: rutin Drug: quercetin Drug: sulindac | - | terminated | There are no results |
| U.S.—Massachusetts | Absorption Kinetics of Polyphenols in Angel’s Plant (Angelica Keiskei) | Oxidative Stress | Dietary Supplement: angel’s plant (Angelica keiskei) Dietary Supplement: Angel’s plant (Angelica keiskei) | Early Phase 1 | unknown | There is no information |
| U.S.—Michigan | Three New Ideas to Protect Special Forces from the Stress of High Altitude | Mountain Sickness | Dietary Supplement: Quercetin Drug: Nifedipine extended release Drug: Methazolamide Drug: Metformin Drug: Placebo Drug: Nitrite | 4 | recruiting | There are no results |
| The Netherlands | The Inflammatory and Antioxidant Status in Pulmonary Sarcoidosis, Idiopathic Pulmonary Fibrosis and COPD: a Potential Role for Antioxidants |
Interstitial Lung Diseases; Sarcoidosis; Idiopathic Pulmonary Fibrosis; COPD; | quercetin | - | completed | There are no results |
| Republic of Korea | Effect of Onion Peel Extract on Endothelial Function and Endothelial Progenitor Cells in Overweight and Obese Subjects | Healthy Overweight Obese | Drug: Placebo Drug: Onion peel extract | 4 | completed | There are no results |
| United Kingdom | The Impact of Isoquercetin and Aspirin on Platelet Function | Cardiovascular Disease | Drug: Vehicle control Drug: Isoquercetin Drug: Aspirin Drug: Isoquercetin plus Aspirin | - | withdrawn | There are no results |
| U.S.—California | Randomized, Placebo-controlled, Double-blind Phase II/III Trial of Oral Isoquercetin to Prevent Venous Thromboembolic Events in Cancer Patients. | Thromboembolism of Vein VTE in Colorectal Cancer; Thromboembolism of Vein in Pancreatic Cancer; Thromboembolism of Vein in Non-small Cell Lung Cancer | Drug: Isoquercetin | 2,3 | recruiting | There are no results |
| Germany | Pilot Study Evaluating Broccoli Sprouts in Advanced Pancreatic Cancer [POUDER Trial] | Pancreatic Ductal Adenocarcinoma | Dietary Supplement: Verum, broccoli sprout grain Dietary Supplement: placebo | - | recruiting | There are no results |
| - | An Open, Uncontrolled Trial in Healthy Volunteers to Explore the Plasma and Urinary Pharmacokinetics of a Single Oral Dose of 1800 mg Red Vine Leaf Extract (Antistax®) | Healthy | Drug: Red Vine Leaf Extract | 1 | completed | There are no results |
| U.S.—North Carolina | Influence of Ingesting a Flavonoid-rich Supplement on the Human Metabolome and Concentration of Urine Phenolics | Inflammation | Dietary Supplement: Flavonoid Dietary Supplement: Placebo | - | Active, not recruiting | There are no results |
| Italy | Isoquercetin as an Adjunct Therapy in Patients with Kidney Cancer Receiving First-line Sunitinib: a Phase I/II Trial | Renal Cell Carcinoma; Kidney Cancer | Drug: Sunitinib Drug: Isoquercetin Drug: Placebo | 1,2 | Recruiting | There are no results |
| U.S.—Illinois, New Jersey and Ohio | Open-Label Study to Evaluate the Effect of Elimune Capsules on Biomarkers in Patients with Plaque Psoriasis | Plaque Psoriasis | Dietary Supplement: Elimune Capsules | 1 | completed | There are no results |
| France | Randomized Controlled Double-blind Clinical Trial for the Effect of Yoghurts Enriched in XXS vs without XXS on the Evolution of Weight in Overweight Subjects Aged 50 to 65 Years. | Obesity Overweight | Dietary Supplement: yoghurts enriched with XXS Dietary Supplement: yoghurts non enriched with XXS | - | completed | There are no results |
| Brazil | Evaluation of Clinical Efficacy Capsules Containing Standardized Extract of Bauhinia Forficata (Pata- De-vaca) in Diabetic Patients | Diabetes | Drug: B. forficata Drug: Placebo | - | recruiting | There are no results |
| Egypt?? | Effects of Oral Ginkgo Biloba Extract on Pregnancy Complicated by Asymmetrically Intrauterine Growth Restriction: a Double-blinded Randomized Placebo-controlled Trial | Intrauterine Growth Restriction (IUGR) | Drug: Ginkgo Biloba Extract Other: Placebo | 2 | completed | There are no results |
| Italy | Physiological Effects of New Polyphenol-enriched Foods in Healthy Humans | Healthy | Other: free curcumin Other: encapsulated curcumin Other: encapsulated curcumin + PQG Other: free cocoa polyphenol Other: encapsulated cocoa polyphenols Other: control nut cream Encapsulada a quercetina | - | Completed Has Results | There are no results |
| U.S.—Missouri | Can Fish Oil and Phytochemical Supplements Mimic Anti-Aging Effects of Calorie Restriction? | Healthy Volunteers | Dietary Supplement: Supplement | - | completed | There are no results |
| U.S.—Michigan | GRAPe Seed Extract and Ventriculovascular Investigation in Normal Ejection-Fraction Heart Failure | Diastolic Heart Failure; Hypertensive; Heart Disease; ;Heart Failure with Preserved Ejection Fraction; Hypertension; Oxidative Stress | Drug: grape seed extract (MegaNatural BP, Polyphenolics, Inc.) | 1 | Active, not recruiting | There are no results |
| U.S.—South Carolina | Effects of Short-term Curcumin and Multi-polyphenol Supplementation on the Anti-inflammatory Properties of HDL (PSI) | Inflammation; Atherosclerosis; Cardiovascular Disease | Dietary Supplement: PolyResveratrol Supplementation Dietary Supplement: Curcumin Supplementation | 2 | Recruiting | There are no results |
| Canada, Alberta | Orthomolecular Treatment as add-on Therapy for Childhood Asthma | Asthma | Dietary Supplement: Orthomolecular Therapy or Placebo Comparator | 2 | unknown | There are no results |
| U.S.—California | Effects of Plant Concentrate Blend on Oxidative Stress in Healthy Humans | Healthy | Dietary Supplement: AOX blend Dietary Supplement: Placebo | - | completed | There are no results |
| U.S.—Ohio | Phytochemical Release Rate from Black Raspberry Confections Alters Gene Expression and Chemical Profiles Relevant to Inhibition of Oral Carcinogenesis | Healthy Volunteers | Other: Fast release BRB confection Other: Intermed release BRBconfect Other: Prolong release BRB confect | 1 | Active, not recruiting | There are no results |
| Norway | Dietary Intervention in Stage III/IV Follicular Lymphoma. Impact on Markers of Cell Proliferation, Apoptosis, Host Immune Cell Infiltrate and Oxidative Stress | Follicular Lymphoma | Drug: Omega 3 fatty acids (EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid)) Drug: Selenium (L-Selenomethionine), Drug: Garlic extract (Allicin) Drug: Pomegranate juice (ellagic acid) Drug: Grape juice (resveratrol, quercetin) Drug: Green Tea (Epigallocathechin gallate | 2 | unknown | There are no results |
| U.S.—Florida | Open Label, Crossover, Pilot Study to Assess the Efficacy & Safety of Perispinal Admin. of Etanercept(Enbrel®) in Comb. w/Nutritional Supplements vs. Nutritional Supplements Alone in Subj. w/Mild to Mod. Alzheimer’s Disease Receiving Std. Care | Alzheimer’s Disease | Biological: Etanercept Dietary Supplement: Curcum. Luteol. Theaflav. Lip. Acid, FishOil, Quercet, Resveratr. | 1 | Completed | There are no results |
| U.S.—California | Proof of Concept Study to Evaluate the Effect of Oxidative Stress Response of Plant Concentrate Blends in Healthy Men | Healthy | Dietary Supplement: Plant concentrate A Dietary Supplement: Plant concentrate B Dietary Supplement: Plant concentrate C Dietary Supplement: Plant concentrate D | - | completed | There are no results |
| U.S.—Ohio | Quercetin chemoprevention for squamous cell carcinoma in patients with Fanconi anemia | Fanconi anemia Squamous cell carcinoma | Dietary supplement | Phase 2 | Recruiting | There are no results |
| U.S.—Pennsylvania | Impact of quercetin on inflammatory and oxidative stress markers in COPD | Chronic obstructive pulmonary disease | Quercetin | Phase 1/Phase 2 | Not yet recruiting | There are no results |
| Not indicated | Serum concentration and gene expression of sirtuin-1 and advanced glycation End-products in postmenopausal women with atherosclerotic coronary disease after administration of atorvastatin and supplementation with quercetin: Randomized trial sirtuin-1 and advanced glycation End-products in postmenopausal women with coronary disease | Coronary artery disease progression | Quercetin | Phase 3 | Not yet recruiting | There are no results |
| Brand | Dosage | Pharmaceutical Form | Application |
|---|---|---|---|
| Quercetin 500 mg (Nature’s Best) | 500 mg | Tablets | Supplement |
| Rutin and vitamin c 500 mg (Nature’s Best) | 50 mg | Tablets | supplement |
| Glucosamine Plus (Nature’s Best) | 25 mg | Tablets | supplement |
| Glucosamine Gold (Nature’s Best) | 20 mg | Tablets | supplement |
| Quercetin with bromelain (Biovea) | 500 mg | Capsules | Vegan supplement |
| Neuroprotek Low Phenol (algonot) | 70 mg | capsules | Dietary supplement |
| Neuroprotek (algonot) | 70 mg | capsules | Dietary supplement |
| Algonot plus (algonot) | 150 mg | capsules | Dietary supplement |
| ArthroSoft (algonot) | 150 mg | capsules | Dietary supplement |
| CystoProtek (algonot) | 150 mg | capsules | Dietary supplement |
| FibroProtek (algonot) | 85 mg | capsules | Dietary supplement |
| ProstaProtek (algonot) | - | capsules | Dietary supplement |
| Quercetin (Natrol) | 250 mg | capsules | Dietary supplement |
| Quercetin (Desert Harvest) | 250 mg | capsules | Dietary supplements |
| Quercetin and vitamin (Vitacost) | 250 mg | capsules | Dietary supplements |
| Aller-Aid with quercetin (Wild Harvest) | 137,5 mg | capsules | Herbal supplement |
| Advan-c (Vitacost) | 100 mg | capsules | Vitamin supplement |
| Quercetin and Bromelain (Vitacost) | 250 mg | capsules | Dietary supplement |
| Quercetin (Jarrow formulas) | 500 mg | capsules | Dietary supplement |
| Quercetin (solaray) | 500 mg | capsules | Dietary supplement |
| Quercetin and Bromelain (Now) | 400 mg | capsules | Vegan supplement |
| Activated quercetin complex (Vitacost) | 333 mg | capsules | Dietary supplement |
| Quercetin complex (solgar) | 250 mg | capsules | Dietary supplement |
| Mega quercetin (solaray) | 600 mg | capsules | Dietary supplement |
| Quercetin strength (megaFood) | 500 mg | capsules | Dietary supplement |
| Activated quercetin (source naturals | 333 mg | capsules | Dietary supplement |
| Optimized quercetin LifeExtension | 250 mg | capsules | Dietary supplement |
| Nettle quercetin (eclectic institute) | 175 mg | capsules | Dietary supplement |
| Quercetin (natural factors) | 235 mg | capsules | Dietary supplement |
| Quercetin (nature’s life) | 400 mg | capsules | Antioxidant supplement |
| Quercetin (Pure encapsulations) | 250 mg | capsules | Dietary supplement |
| Quercetin bioflavonoids (NutriCology) | 50 mg | capsules | Dietary supplement |
| Quercetin (MRM) | 500 mg | capsules | Dietary supplement |
| Quercetin (Kal) | 1000 mg | tablets | Dietary supplement |
| Quercetin plus (Olympian labs) | 500 mg | capsules | Dietary supplements |
| ALLER-C (Vital Nutrients) | 250 mg | capsules | Dietary supplements |
| Quercetin Bromelain (Doctor’s BEST) | 250 mg | capsules | Dietary supplement |
| Rose Plus Anti-Ageing Face (The organic Pharmacy) | n.i | Cream | anti-ageing cream |
| Flash Defense Anti-Pollution Mist (REN) | n.i | cream | skincare |
| Antiwrinkle Firming and Lifting serum (Korres) | n.i | serum | skincare |
| Tightening eye contour gel (Alchimie forever) | n.i | gel | Make up |
| Firming gel for neck and bust (Alchimie forever) | n.i | gel | skincare |
| Kantic calming cream (Alchimie forever) | n.i | cream | skincare |
| Rejuvenating eye balm (Alchimie forever) | n.i | cream | skincare |
| Antioxidant skin repair gel (Alchimie forever) | n.i | gel | skincare |
| Gentle cream cleanser (Alchimie forever) | n.i | cream | skincare |
| Resist advanced replenishing toner (Paula’s choice) | n.i | cream | skincare |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pinheiro, R.G.R.; Pinheiro, M.; Neves, A.R. Nanotechnology Innovations to Enhance the Therapeutic Efficacy of Quercetin. Nanomaterials 2021, 11, 2658. https://doi.org/10.3390/nano11102658
Pinheiro RGR, Pinheiro M, Neves AR. Nanotechnology Innovations to Enhance the Therapeutic Efficacy of Quercetin. Nanomaterials. 2021; 11(10):2658. https://doi.org/10.3390/nano11102658
Chicago/Turabian StylePinheiro, Rúben G. R., Marina Pinheiro, and Ana Rute Neves. 2021. "Nanotechnology Innovations to Enhance the Therapeutic Efficacy of Quercetin" Nanomaterials 11, no. 10: 2658. https://doi.org/10.3390/nano11102658
APA StylePinheiro, R. G. R., Pinheiro, M., & Neves, A. R. (2021). Nanotechnology Innovations to Enhance the Therapeutic Efficacy of Quercetin. Nanomaterials, 11(10), 2658. https://doi.org/10.3390/nano11102658






