Evaluation of Acetaminophen Release from Biodegradable Poly (Vinyl Alcohol) (PVA) and Nanocellulose Films Using a Multiphase Release Mechanism
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
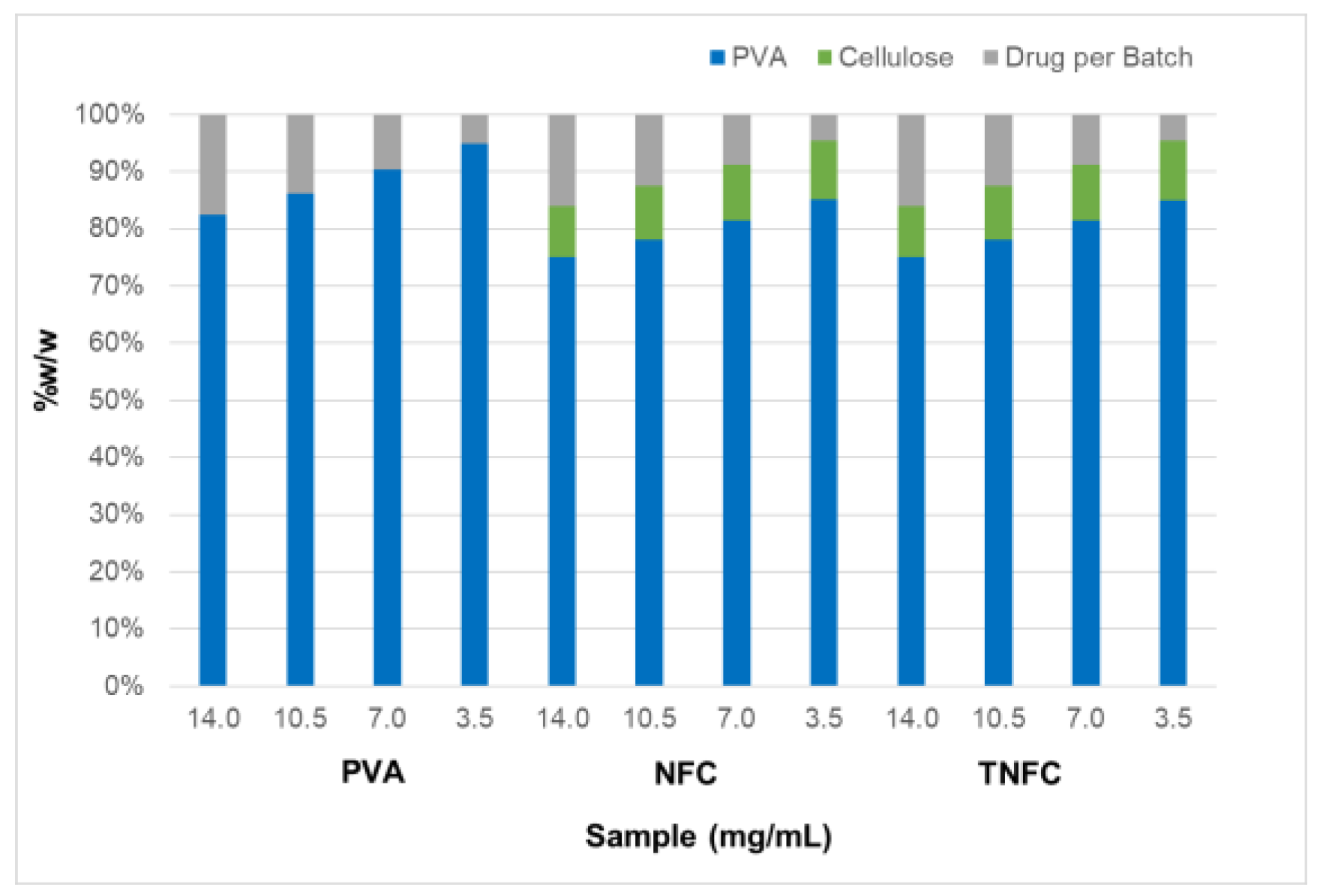
2.2. Film Formulations
2.3. Drug Release Studies
2.4. Drug Release Quantification
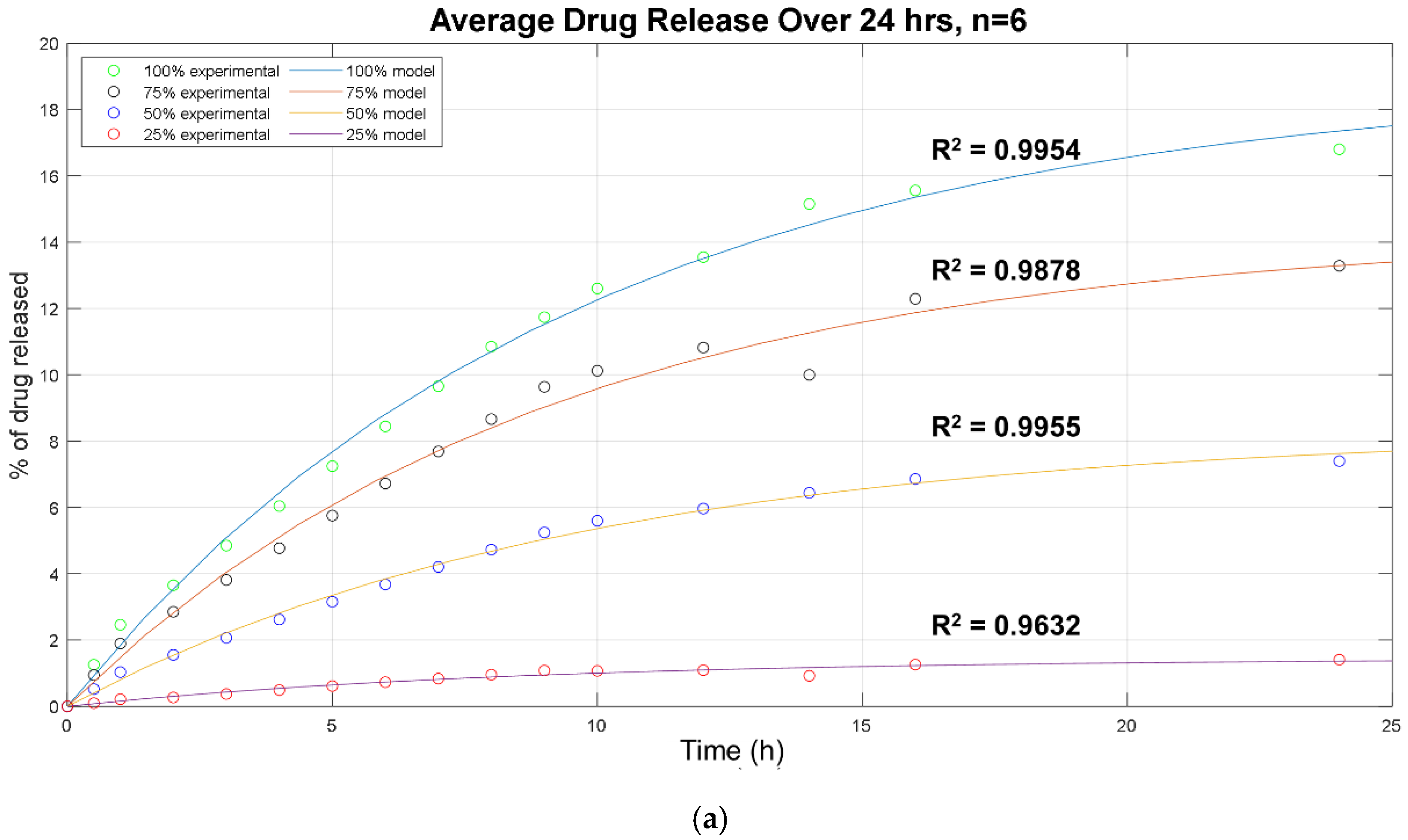
2.5. Drug Release Modeling
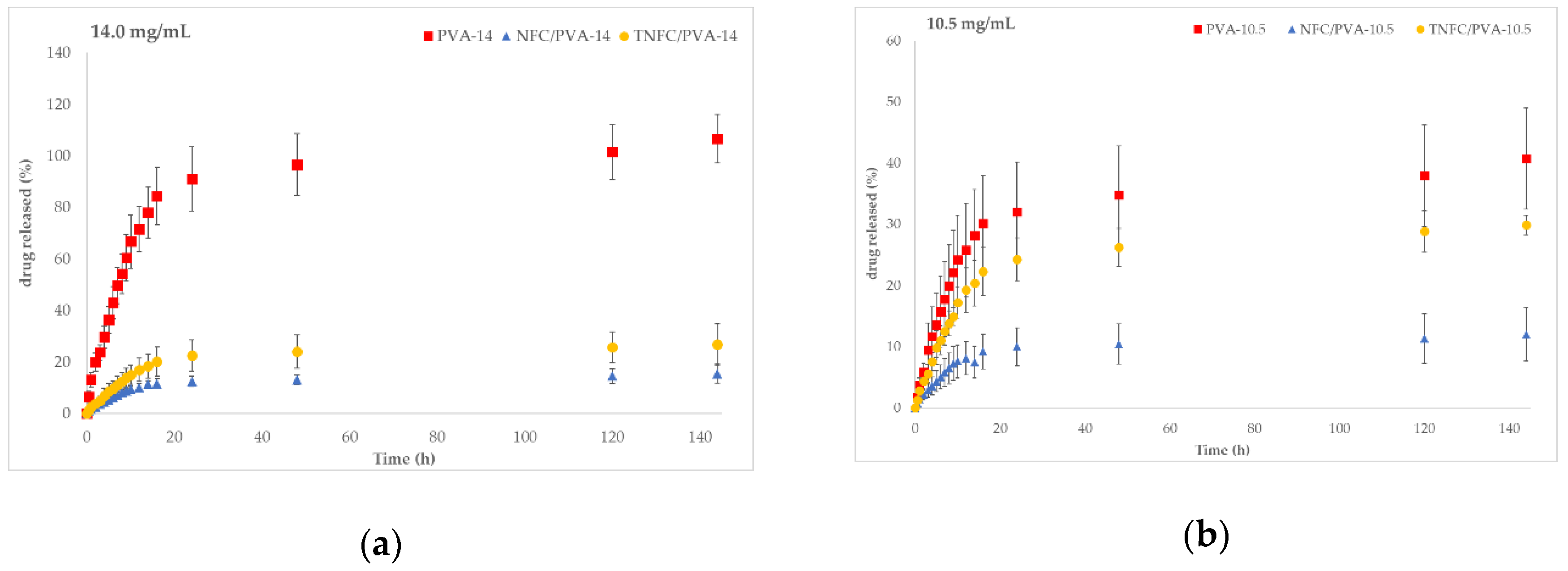
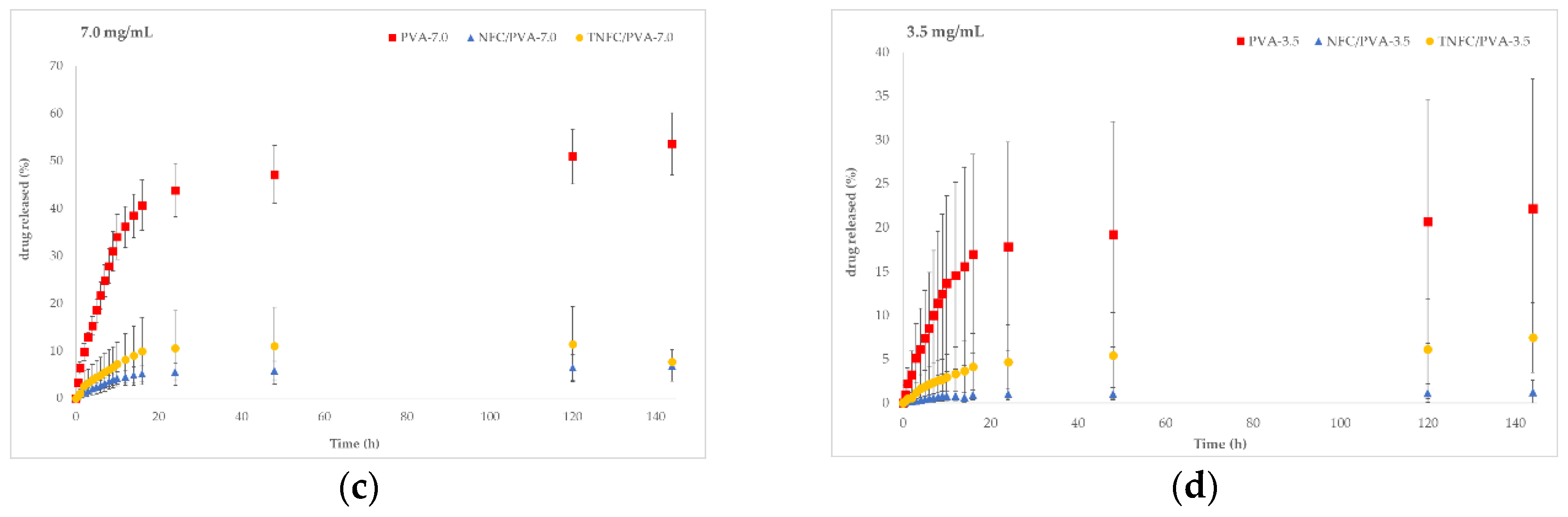
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lao, L.L.; Venkatraman, S.S.; Peppas, N.A. Modeling of drug release from biodegradable polymer blends. Eur. J. Pharm. Biopharm 2008, 70, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Duncan, T.V.; Pillai, K. Release of Engineered Nanomaterials from Polymer Nanocomposites: Diffusion, Dissolution, and Desorption. ACS Appl. Mater. Interfaces 2015, 7, 2–19. [Google Scholar] [CrossRef] [PubMed]
- Endes, C.; Camarero-Espinosa, S.; Mueller, S.; Foster, E.J.; Petri-Fink, A.; Rothen-Rutishauser, B.; Weder, C.; Clift, M.J.D. A critical review of the current knowledge regarding the biological impact of nanocellulose. J. Nanobiotechnol. 2016, 14, 78. [Google Scholar] [CrossRef] [PubMed]
- Klemm, D.; Cranston, E.D.; Fischer, D.; Gama, M.; Kedzior, S.A.; Kralisch, D.; Kramer, F.; Kondo, T.; Lindström, T.; Nietzsche, S.; et al. Nanocellulose as a natural source for groundbreaking applications in materials science: Today’s state. Mater. Today 2018, 21, 720–748. [Google Scholar] [CrossRef]
- Rol, F.; Belgacem, M.N.; Gandini, A.; Bras, J. Recent advances in surface-modified cellulose nanofibrils. Prog. Polym. Sci. 2019, 88, 241–264. [Google Scholar] [CrossRef]
- Abitbol, T.; Rivkin, A.; Cao, Y.; Nevo, Y.; Abraham, E.; Ben-Shalom, T.; Lapidot, S.; Shoseyov, O. Nanocellulose, a tiny fiber with huge applications. Curr. Opin. Biotechnol. 2016, 39, 76–88. [Google Scholar] [CrossRef]
- Kargarzadeh, H.; Huang, J.; Lin, N.; Ahmad, I.; Mariano, M.; Dufresne, A.; Thomas, S.; Gałęski, A. Recent developments in nanocellulose-based biodegradable polymers, thermoplastic polymers, and porous nanocomposites. Prog. Polym. Sci. 2018, 87, 197–227. [Google Scholar] [CrossRef]
- Lin, N.; Dufresne, A. Nanocellulose in biomedicine: Current status and future prospect. Eur. Polym. J. 2014, 59, 302–325. [Google Scholar] [CrossRef]
- Kolakovic, R.; Peltonen, L.; Laukkanen, A.; Hirvonen, J.; Laaksonen, T. Nanofibrillar cellulose films for controlled drug delivery. Eur. J. Pharm. Biopharm. 2012, 82, 308–315. [Google Scholar] [CrossRef]
- Klemm, D.; Kramer, F.; Moritz, S.; Lindström, T.; Ankerfors, M.; Gray, D.; Dorris, A. Nanocelluloses: A new family of nature-based materials. Angew. Chemie. Int. Ed. 2011, 50, 5438–5466. [Google Scholar] [CrossRef]
- Nechyporchuk, O.; Belgacem, M.N.; Bras, J. Production of cellulose nanofibrils: A review of recent advances. Ind. Crop. Prod. 2016, 93, 2–25. [Google Scholar] [CrossRef]
- Jiang, C.; Oporto, G.S.; Zhong, T.; Jaczynski, J. TEMPO nanofibrillated cellulose as template for controlled release of antimicrobial copper from PVA films. Cellulose 2016, 23, 713–722. [Google Scholar] [CrossRef]
- Shefa, A.A.; Amirian, J.; Kang, J.; Bae, S.H.; Jung, H.; Choi, H.; Lee, S.Y.; Lee, B. In vitro and in vivo evaluation of effectiveness of a novel TEMPO-oxidized cellulose nanofiber-silk fibroin scaffold in wound healing. Carbohydr. Polym. 2017, 177, 284–296. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.; Lue, A.; Zhang, L. Effects of Crosslinking Methods on Structure and Properties of Cellulose/PVA Hydrogels. Macromol. Chem. Phys. 2008, 209, 1266–1273. [Google Scholar] [CrossRef]
- Weishaupt, R.; Siqueira, G.; Schubert, M.; Tingaut, P.; Maniura-Weber, K.; Zimmermann, T.; Thöny-Meyer, L.; Faccio, G.; Ihssen, J. TEMPO-Oxidized Nanofibrillated Cellulose as a High Density Carrier for Bioactive Molecules. Biomacromolecules 2015, 16, 3640–3650. [Google Scholar] [CrossRef]
- Letchford, J.K.; Jackson, K.; Wasserman, B.; Ye, L.; Hamad, W.; Burt, H. The use of nanocrystalline cellulose for the binding and controlled release of drugs. Int. J. Nanomed. 2011, 6, 321. [Google Scholar] [CrossRef]
- Xie, J.; Li, J. Smart Drug Delivery System Based on Nanocelluloses. J. Bioresour. Bioprod. 2017, 2, 1–3. Available online: www.Bioresources-Bioproducts.com (accessed on 25 April 2019).
- Zhang, F.; Wu, W.; Zhang, X.; Meng, X.; Tong, G.; Deng, Y. Temperature-sensitive poly-NIPAm modified cellulose nanofibril cryogel microspheres for controlled drug release. Cellulose 2016, 23, 415–425. [Google Scholar] [CrossRef]
- Jorfi, M.; Foster, E.J. Recent advances in nanocellulose for biomedical applications. J. Appl. Polym. Sci. 2015, 132, 1–19. [Google Scholar] [CrossRef]
- Peppas, N.A.; Narasimhan, B. Mathematical models in drug delivery: How modeling has shaped the way we design new drug delivery systems. J. Controlled Release 2014, 190, 75–81. [Google Scholar] [CrossRef]
- Bruschi, M.L. Mathematical models of drug release. Strategies to Modify the Drug Release from Pharmaceutical Systems; Woodhead Publishing: Cambridge, UK, 2015; pp. 63–86. Available online: https://www.sciencedirect.com/book/9780081000922/strategies-to-modify-the-drug-release-from-pharmaceutical-systems#book-info (accessed on 1 December 2019).
- Lao, L.L.; Peppas, N.A.; Yin, F.; Boey, C.; Venkatramavn, S.S. Modeling of drug release from bulk-degrading polymers. Int. J. Pharm. 2010, 418, 28–41. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, J.; Siepmann, F. Modeling of diffusion controlled drug delivery. J. Control. Release 2012, 161, 351–362. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, J.; Gopferich, A. Mathematical Modeling of Bioerodible, Polymeric Drug Delivery Systems. Adv. Drug Delivery Rev. 2001, 48, 229–247. [Google Scholar] [CrossRef]
- Siepmann, J.; Siepmann, F. Mathematical modeling of drug dissolution. Int. J. Pharm. 2013, 453, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, J.; Peppas, N.A. Modeling of drug release from delivery systems based on hydroxypropyl methylcellulose (HPMC). Adv. Drug Deliv. Rev. 2012, 64, 163–174. [Google Scholar] [CrossRef]
- Panaitescu, D.M.; Frone, A.N.; Ghiurea, M.; Chiulan, I. Influence of storage conditions on starch/PVA films containing cellulose nanofibers. Ind Crops Prod. 2015, 70, 170–177. [Google Scholar] [CrossRef]
- Saito, T.; Hirota, M.; Tamura, N.; Kimura, S.; Fukuzumi, H.; Heux, L.; Isogai, A. Individualization of nano-sized plant cellulose fibrils achieved by direct surface carboxylation using TEMPO catalyst under neutral conditions. Biomacromolecules 2009, 10, 1992–1996. [Google Scholar] [CrossRef]
- Huang, M.; Chen, F.; Jiang, Z.; Li, Y. Preparation of TEMPO-oxidized cellulose/amino acid/nanosilver biocomposite film and its antibacterial activity. Int. J. Biol Macromol. 2013, 62, 608–613. [Google Scholar] [CrossRef]
- Asad, M.; Saba, N.; Asiri, A.M.; Jawaid, M.; Indarti, E.; Wanrosli, W.D. Preparation and characterization of nanocomposite films from oil palm pulp nanocellulose/poly (Vinyl alcohol) by casting method. Carbohydr. Polym. 2018, 191, 103–111. [Google Scholar] [CrossRef]
- Lee, K.Y.; Aitomäki, Y.; Berglund, L.A.; Oksman, K.; Bismarck, A. On the use of nanocellulose as reinforcement in polymer matrix composites. Compos. Sci. Technol. 2014, 105, 15–27. [Google Scholar] [CrossRef]
- George, A.; Shah, P.A.; Shrivastav, P.S. Natural biodegradable polymers based nano-formulations for drug delivery: A review. Int. J. Pharm. 2019, 561, 244–264. [Google Scholar] [CrossRef] [PubMed]

| Drug (mg) | dI-H2O (mL) | Stock (mg/mL) |
|---|---|---|
| 4203.0 | 300.0 | 14.0 |
| 3154.0 | 300.0 | 10.5 |
| 2106.0 | 300.0 | 7.0 |
| 1050.0 | 300.0 | 3.5 |
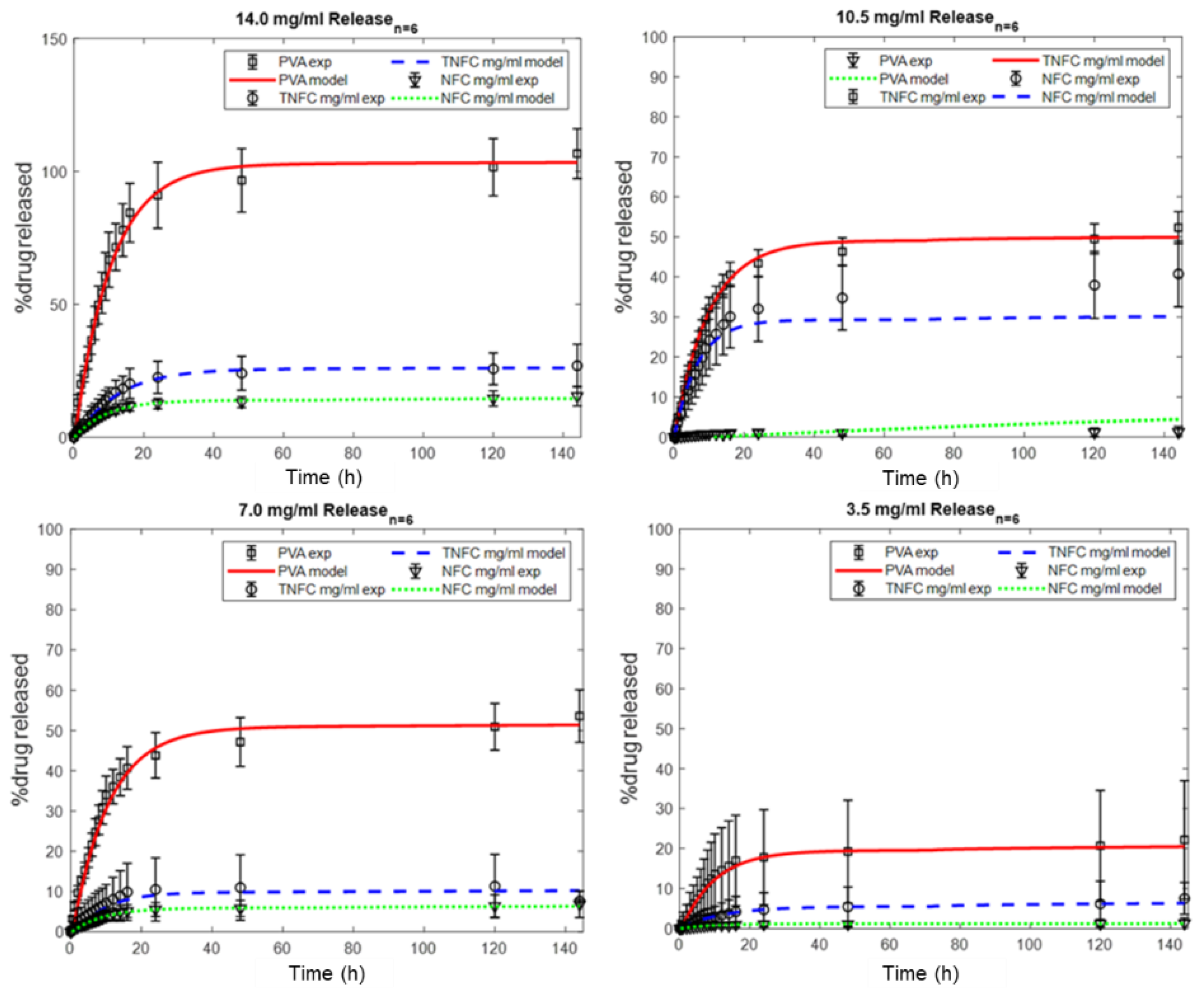
| Sample | 14.0 mg/mL | 10.5 mg/mL | 7.0 mg/mL | 3.5 mg/mL |
|---|---|---|---|---|
| PVA | 106.7% ± 9.4% | 40.7% ± 8.2% | 53.5% ± 6.5% | 22.2% ± 14.8% |
| NFC | 15.5% ± 3.7% | 12.0% ± 4.4% | 6.8% ± 3.3% | 1.3% ± 1.3% |
| TNFC | 26.9% ± 8.0% | 29.8% ± 1.6% | 7.6% ± 0.4% | 7.5% ± 3.9% |
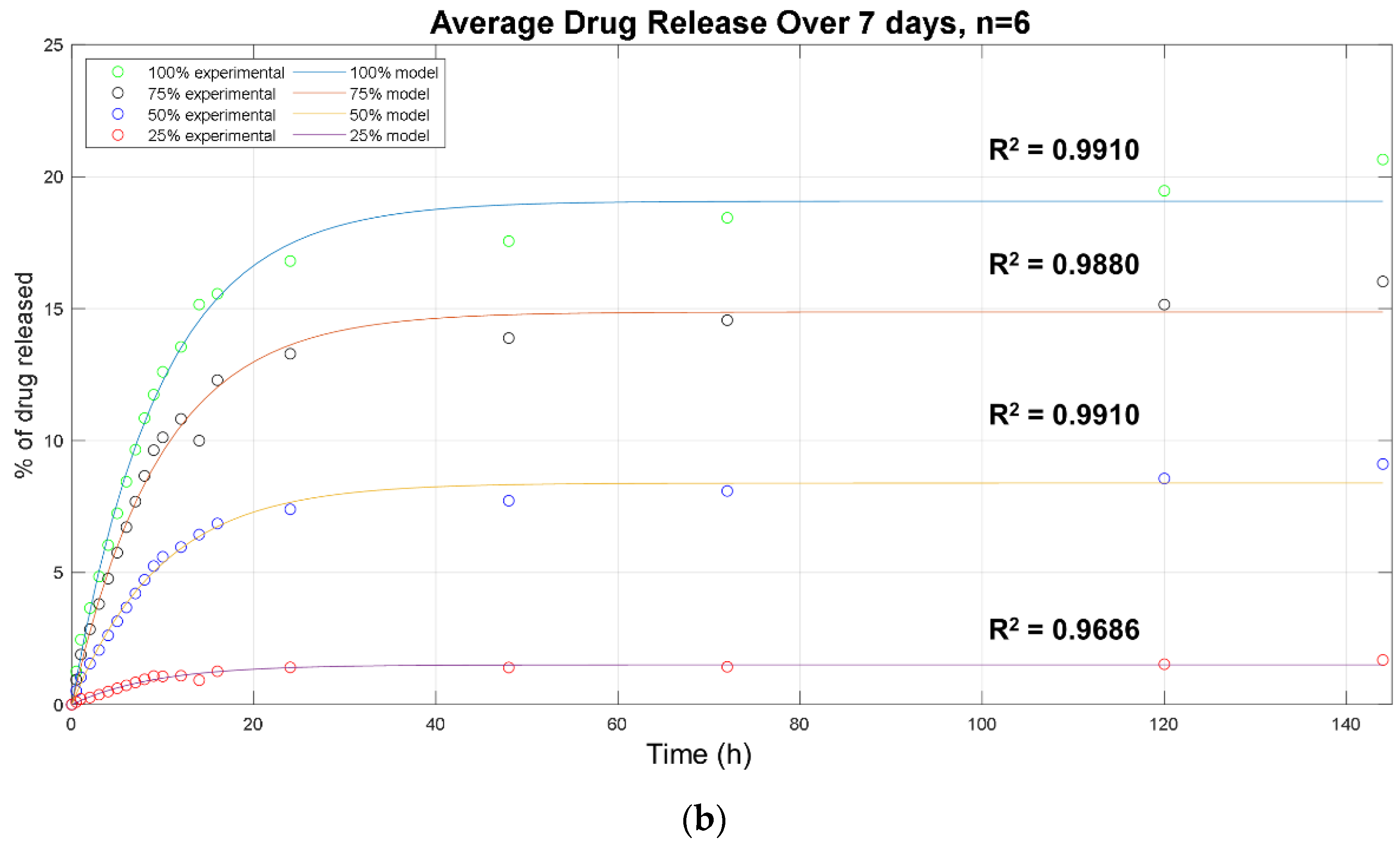
| Sample | Φb | kb | R2 |
|---|---|---|---|
| PVA-14.0 | 105.5 | 0.09 | 0.99 |
| PVA-10.5 | 49.4 | 0.10 | 1.00 |
| PVA-7.0 | 53.6 | 0.10 | 0.99 |
| PVA-3.5 | 20.7 | 0.10 | 0.99 |
| NFC/PVA-14.0 | 14.2 | 0.10 | 1.00 |
| NFC/PVA-10.5 | 10.7 | 0.11 | 0.99 |
| NFC/PVA-7.0 | 6.2 | 0.10 | 1.00 |
| NFC/PVA-3.5 | 1.2 | 0.11 | 0.99 |
| TNFC/PVA-14.0 | 27.5 | 0.08 | 1.00 |
| TNFC/PVA-10.5 | 29.3 | 0.08 | 0.99 |
| TNFC/PVA-7.0 | 12.2 | 0.09 | 0.99 |
| TNFC/PVA-3.5 | 5.5 | 0.08 | 0.99 |
| Sample | kb (day−1) | Φb (%) | kr (day−1) | Φr (%) | D (10−12cm2/s) | Φd (%) | Total (%) |
|---|---|---|---|---|---|---|---|
| PVA-14.0 | 3.7 | 105.5 | 0.1 | 0.1 | 0.63 | 0.0 | 141.2 |
| PVA-10.5 | 3.9 | 49.4 | 0.0 | 0.0 | 62.9 | 0.1 | 50.8 |
| PVA-7.0 | 3.5 | 53.6 | 0.0 | 0.0 | 62.9 | 0.1 | 65.8 |
| PVA-3.5 | 2.2 | 20.7 | 0.0 | 0.1 | 0.63 | 0.0 | 12.2 |
| NFC/PVA-14.0 | 2.6 | 14.2 | 0.0 | 0.0 | 62.9 | 0.1 | 14.3 |
| NFC/PVA-10.5 | 2.7 | 10.7 | 0.0 | 0.0 | 62.9 | 0.1 | 10.8 |
| NFC/PVA-7.0 | 2.6 | 6.2 | 0.5 | 0.0 | 33.3 | 0.1 | 6.3 |
| NFC/PVA-3.5 | 2.9 | 1.2 | 0.5 | 0.0 | 1.4 | 0.1 | 1.2 |
| TNFC/PVA-14.0 | 1.9 | 27.5 | 0.7 | 0.0 | 0.7 | 0.0 | 27.5 |
| TNFC/PVA-10.5 | 2.1 | 29.3 | 0.6 | 0.0 | 62.8 | 0.1 | 29.4 |
| TNFC/PVA-7.0 | 2.4 | 12.2 | 0.9 | 0.0 | 0.6 | 0.0 | 12.2 |
| TNFC/PVA-3.5 | 1.9 | 5.5 | 0.0 | 0.0 | 62.9 | 0.1 | 5.6 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Donnell, K.L.; Oporto-Velásquez, G.S.; Comolli, N. Evaluation of Acetaminophen Release from Biodegradable Poly (Vinyl Alcohol) (PVA) and Nanocellulose Films Using a Multiphase Release Mechanism. Nanomaterials 2020, 10, 301. https://doi.org/10.3390/nano10020301
O’Donnell KL, Oporto-Velásquez GS, Comolli N. Evaluation of Acetaminophen Release from Biodegradable Poly (Vinyl Alcohol) (PVA) and Nanocellulose Films Using a Multiphase Release Mechanism. Nanomaterials. 2020; 10(2):301. https://doi.org/10.3390/nano10020301
Chicago/Turabian StyleO’Donnell, Kelsey L., Gloria S. Oporto-Velásquez, and Noelle Comolli. 2020. "Evaluation of Acetaminophen Release from Biodegradable Poly (Vinyl Alcohol) (PVA) and Nanocellulose Films Using a Multiphase Release Mechanism" Nanomaterials 10, no. 2: 301. https://doi.org/10.3390/nano10020301
APA StyleO’Donnell, K. L., Oporto-Velásquez, G. S., & Comolli, N. (2020). Evaluation of Acetaminophen Release from Biodegradable Poly (Vinyl Alcohol) (PVA) and Nanocellulose Films Using a Multiphase Release Mechanism. Nanomaterials, 10(2), 301. https://doi.org/10.3390/nano10020301






