Comparison of Commercial and Experimental Fibre-Reinforced Composites in Restoring Endodontically Treated Teeth with Minimal Coronal Dentine: An In Vitro Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation
2.2. Preparation of Experimental Composite
2.3. Testing of Fracture Strength
2.3.1. Two-Body Wear Test—Chewing Simulation
2.3.2. Fracture Resistance Test
2.4. Statistical Analysis
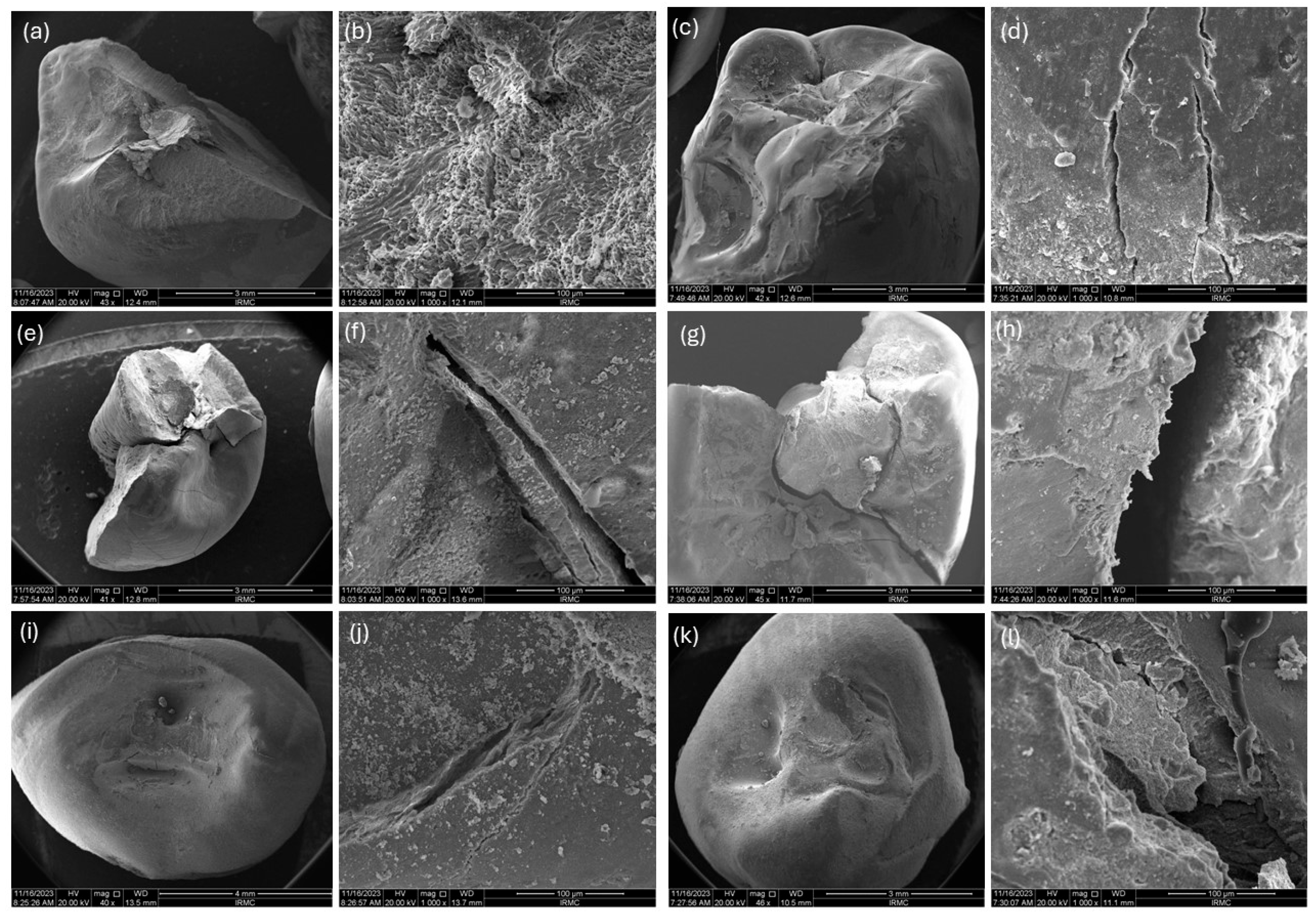
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- López-Valverde, I.; Vignoletti, F.; Vignoletti, G.; Martin, C.; Sanz, M. Long-term tooth survival and success following primary root canal treatment: A 5- to 37-year retrospective observation. Clin. Oral Investig. 2023, 27, 3233–3244. [Google Scholar] [CrossRef]
- Garlapati, T.G.; Krithikadatta, J.; Natanasabapathy, V. Fracture resistance of endodontically treated teeth restored with short fiber composite used as a core material—An in vitro study. J. Prosthodont. Res. 2017, 61, 464–470. [Google Scholar] [CrossRef]
- Gök, T.; Durdu, E.; Atik, M.R.; Konuş, F.; Gök, A. Evaluation of Fracture Resistance and Failure Modes of Maxillary Premolars Restored with Different Coronal Designed Fiber Posts: In Vitro Study. Eur. Endod. J. 2025, 10, 58–65. [Google Scholar] [CrossRef]
- Santos, J.M.; Palma, P.J.; Ramos, J.C.; Cabrita, A.S.; Friedman, S. Periapical inflammation subsequent to coronal inoculation of dog teeth root filled with resilon/epiphany in 1 or 2 treatment sessions with chlorhexidine medication. J. Endod. 2014, 40, 837–841. [Google Scholar] [CrossRef]
- de Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral Res. 2018, 32, 147–158. [Google Scholar] [CrossRef]
- Eskitaşcioğlu, G.; Belli, S.; Kalkan, M. Evaluation of two post core systems using two different methods (fracture strength test and a finite elemental stress analysis). J. Endod. 2002, 28, 629–633. [Google Scholar] [CrossRef]
- Escobar, L.B.; Pereira da Silva, L.; Manarte-Monteiro, P. Fracture resistance of fiber-reinforced composite restorations: A systematic review and meta-analysis. Polymers 2023, 15, 3802. [Google Scholar] [CrossRef] [PubMed]
- Mena-Álvarez, J.; Agustín-Panadero, R.; Zubizarreta-Macho, A. Effect of fiber-reinforced composite and elastic post on the fracture resistance of premolars with root canal treatment—An in vitro pilot study. Appl. Sci. 2020, 10, 7616. [Google Scholar] [CrossRef]
- Selvaraj, H.; Krithikadatta, J.; Shrivastava, D.; Onazi, M.A.; Algarni, H.A.; Munaga, S.; Hamza, M.O.; Al-Fridy, T.S.; Teja, K.V.; Janani, K.; et al. Systematic review fracture resistance of endodontically treated posterior teeth restored with fiber reinforced composites—A systematic review. BMC Oral Health 2023, 23, 566. [Google Scholar] [CrossRef] [PubMed]
- Puska, M.; Zhang, M.; Matinlinna, J.P.; Vallittu, P.K. Silane-Treated E-Glass Fiber-Reinforced Telechelic Macromer-Based Polymer-Matrix Composites. Silicon 2013, 6, 57–63. [Google Scholar] [CrossRef]
- Safwat, E.M.; Khater, A.G.A.; Abd-Elsatar, A.G.; Khater, G.A. Glass fiber-reinforced composites in dentistry. Bull. Natl. Res. Cent. 2021, 45, 190. [Google Scholar] [CrossRef]
- Ramakrishna, S.; Mayer, J.; Wintermantel, E.; Leong, K.W. Biomedical applications of polymer-composite materials: A review. Compos. Sci. Technol. 2001, 61, 1189–1224. [Google Scholar] [CrossRef]
- Abdulmajeed, A.A.; Närhi, T.O.; Vallittu, P.K.; Lassila, L.V. The effect of high fiber fraction on some mechanical properties of unidirectional glass fiber-reinforced composite. Dent. Mater. 2011, 27, 313–321. [Google Scholar] [CrossRef]
- Tsue, F.; Takahashi, Y.; Shimizu, H. Reinforcing effect of glass-fiber-reinforced composite on flexural strength at the proportional limit of denture base resin. Acta Odontol. Scand. 2007, 65, 141–148. [Google Scholar] [CrossRef]
- Abouelleil, H.; Pradelle, N.; Villat, C.; Attik, N.; Colon, P.; Grosgogeat, B. Comparison of mechanical properties of a new fiber reinforced composite and bulk filling composites. Restor. Dent. Endod. 2015, 40, 262. [Google Scholar] [CrossRef] [PubMed]
- Zhang, M.; Matinlinna, J.P. E-Glass Fiber Reinforced Composites in Dental Applications. Silicon 2011, 4, 73–78. [Google Scholar] [CrossRef]
- Garoushi, S.; Vallittu, P.K.; Watts, D.C.; Lassila, L.V. Polymerization shrinkage of experimental short glass fiber-reinforced composite with semi-inter penetrating polymer network matrix. Dent. Mater. 2008, 24, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Lassila, L.; Säilynoja, E.; Prinssi, R.; Vallittu, P.; Garoushi, S. Characterization of a new fiber-reinforced flowable composite. Odontology 2019, 107, 342–352. [Google Scholar] [CrossRef]
- Alshabib, A.; Jurado, C.A.; Tsujimoto, A. Short fiber-reinforced resin-based composites (SFRCs); Current status and future perspectives. Dent. Mater. J. 2022, 41, 647–654. [Google Scholar] [CrossRef]
- Garoushi, S.; Säilynoja, E.; Frater, M.; Keulemans, F.; Vallittu, P.K.; Lassila, L. A comparative evaluation of commercially available short fiber-reinforced composites. BMC Oral Health 2024, 24, 1573. [Google Scholar] [CrossRef]
- Surana, P.; Dhull, K.S.; Arya, A.; Samreen, S.; Rajan, M.; Parihar, A.S. Bio-ceramics application in Dentistry. Bioinformation 2024, 20, 136. [Google Scholar] [CrossRef]
- Melo, M.A.S.; Garcia, I.M.; Mokeem, L.; Weir, M.D.; Xu, H.H.K.; Montoya, C.; Orrego, S. Developing bioactive dental resins for restorative dentistry. J. Dent. Res. 2023, 102, 1180–1190. [Google Scholar] [CrossRef]
- Kumar, S.; Gautam, C.; Chauhan, B.S.; Srikrishna, S.; Yadav, R.S.; Rai, S.B. Enhanced mechanical properties and hydrophilic behavior of magnesium oxide added hydroxyapatite nanocomposite: A bone substitute material for load bearing applications. Ceram. Int. 2020, 46 Pt B, 16235–16248. [Google Scholar] [CrossRef]
- Siddiqui, U.; Khalid, H.; Ghafoor, S.; Javaid, A.; Asif, A.; Khan, A.S. Analyses on mechanical and physical performances of nano-apatite grafted glass fibers based dental composites. Mater. Chem. Phys. 2021, 263, 124188. [Google Scholar] [CrossRef]
- Saleem, M.; Zahid, S.; Ghafoor, S.; Khalid, H.; Iqbal, H.; Zeeshan, R.; Ahmad, S.; Asif, A.; Khan, A.S. Physical, mechanical, and in vitro biological analysis of bioactive fibers-based dental composite. J. Appl. Polym. Sci. 2021, 138, 50336. [Google Scholar] [CrossRef]
- Khan, A.S.; AlMaimouni, Y.K.; Benrashed, M.A.; Alyousef, N.I.; Siddiqui, U.; Ahmad, N.; Ateeq, I.S.; Hakeem, A.S. A laboratory study to assess the physical, mechanical, and 3-D structural properties of nano-apatite grafted glass fibre-based endodontic posts. Int. Endod. J. 2021, 54, 2307–2320. [Google Scholar] [CrossRef]
- Khan, A.S.; Alshaia, A.; AlDubayan, A.; Alarifi, S.; Alamri, A.; Aldossary, H.; Ahmed, S.Z.; Ateeq, I.S.; Hakeem, A.S.; Rehman, S. Preparation of Nano-Apatite Grafted Glass-Fiber-Reinforced Composites for Orthodontic Application: Mechanical and In Vitro Biofilm Analysis. Materials 2022, 15, 3504. [Google Scholar] [CrossRef]
- Khalid, H.; Suhaib, F.; Zahid, S.; Ahmed, S.; Jamal, A.; Kaleem, M.; Khan, A.S. Microwave-assisted synthesis and in vitro osteogenic analysis of novel bioactive glass fibers for biomedical and dental applications. Biomed. Mater. 2018, 14, 015005. [Google Scholar] [CrossRef]
- Syed, M.R.; Bano, N.Z.; Ghafoor, S.; Khalid, H.; Zahid, S.; Siddiqui, U.; Hakeem, A.S.; Asif, A.; Kaleem, M.; Khan, A.S. Synthesis and characterization of bioactive glass fiber-based dental restorative composite. Ceram. Int. 2020, 46, 21623–21631. [Google Scholar] [CrossRef]
- Haralur, S.B.; Al-Qahtani, A.S.; Al-Qarni, M.M.; Al-Homrany, R.M.; Aboalkhair, A.E. Influence of remaining dentin wall thickness on the fracture strength of endodontically treated tooth. J. Conserv. Dent. Endod. 2016, 19, 63–67. [Google Scholar] [CrossRef]
- Baba, N.Z.; Goodacre, C.J. Restoration of endodontically treated teeth: Contemporary concepts and future perspectives. Endod. Top. 2014, 31, 68–83. [Google Scholar] [CrossRef]
- Hansen, E.K.; Asmussen, E.; Christiansen, N.C. In vivo fractures of endodontically treated posterior teeth restored with amalgam. Dent. Traumatol. 1990, 6, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Soares, L.M.; Razaghy, M.; Magne, P. Optimization of large MOD restorations: Composite resin inlays vs. short fiber-reinforced direct restorations. Dent. Mater. 2018, 34, 587–597. [Google Scholar] [CrossRef] [PubMed]
- Eapen, A.M.; Amirtharaj, L.V.; Sanjeev, K.; Mahalaxmi, S. Fracture resistance of endodontically treated teeth restored with 2 different fiber-reinforced composite and 2 conventional composite resin core buildup materials: An in vitro study. J. Endod. 2017, 43, 1499–1504. [Google Scholar] [CrossRef]
- Daher, R.; Ardu, S.; Di Bella, E.; Rocca, G.T.; Feilzer, A.J.; Krejci, I. Fracture strength of non-invasively reinforced MOD cavities on endodontically treated teeth. Odontology 2021, 109, 368–375. [Google Scholar] [CrossRef]
- Salis, S.G.; Hood, J.A.A.; Kirk, E.E.J.; Stokes, A.N.S. Impact-fracture energy of human premolar teeth. J. Prosthet. Dent. 1987, 58, 43–48. [Google Scholar] [CrossRef]
- Sorensen, J.A.; Engelman, M.J. Effect of post adaptation on fracture resistance of endodontically treated teeth. J. Prosthet. Dent. 1990, 64, 419–424. [Google Scholar] [CrossRef]
- Sedrez-Porto, J.A.; da Rosa, W.L.; Da Silva, A.F.; Münchow, E.A.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef]
- Pantvisai, P.; Messer, H.H. Cuspal deflection in molars in relation to endodontic and restorative procedures. J. Endod. 1995, 21, 57–61. [Google Scholar] [CrossRef]
- Mannocci, F.; Bertelli, E.; Sherriff, M.; Watson, T.F.; Ford, T.P. Three-year clinical comparison of survival of endodontically treated teeth restored with either full cast coverage or with direct composite restoration. J. Prosthet. Dent. 2002, 88, 297–301. [Google Scholar] [CrossRef]
- Monga, P.; Sharma, V.; Kumar, S. Comparison of fracture resistance of endodontically treated teeth using different coronal restorative materials: An in vitro study. J. Conserv. Dent. Endod. 2009, 12, 154–159. [Google Scholar] [CrossRef]
- Rosentritt, M.; Plein, T.; Kolbeck, C.; Behr, M.; Handel, G. In vitro fracture force and marginal adaptation of ceramic crowns fixed on natural and artificial teeth. Int. J. Prosthodont. 2000, 13, 387–391. [Google Scholar] [PubMed]
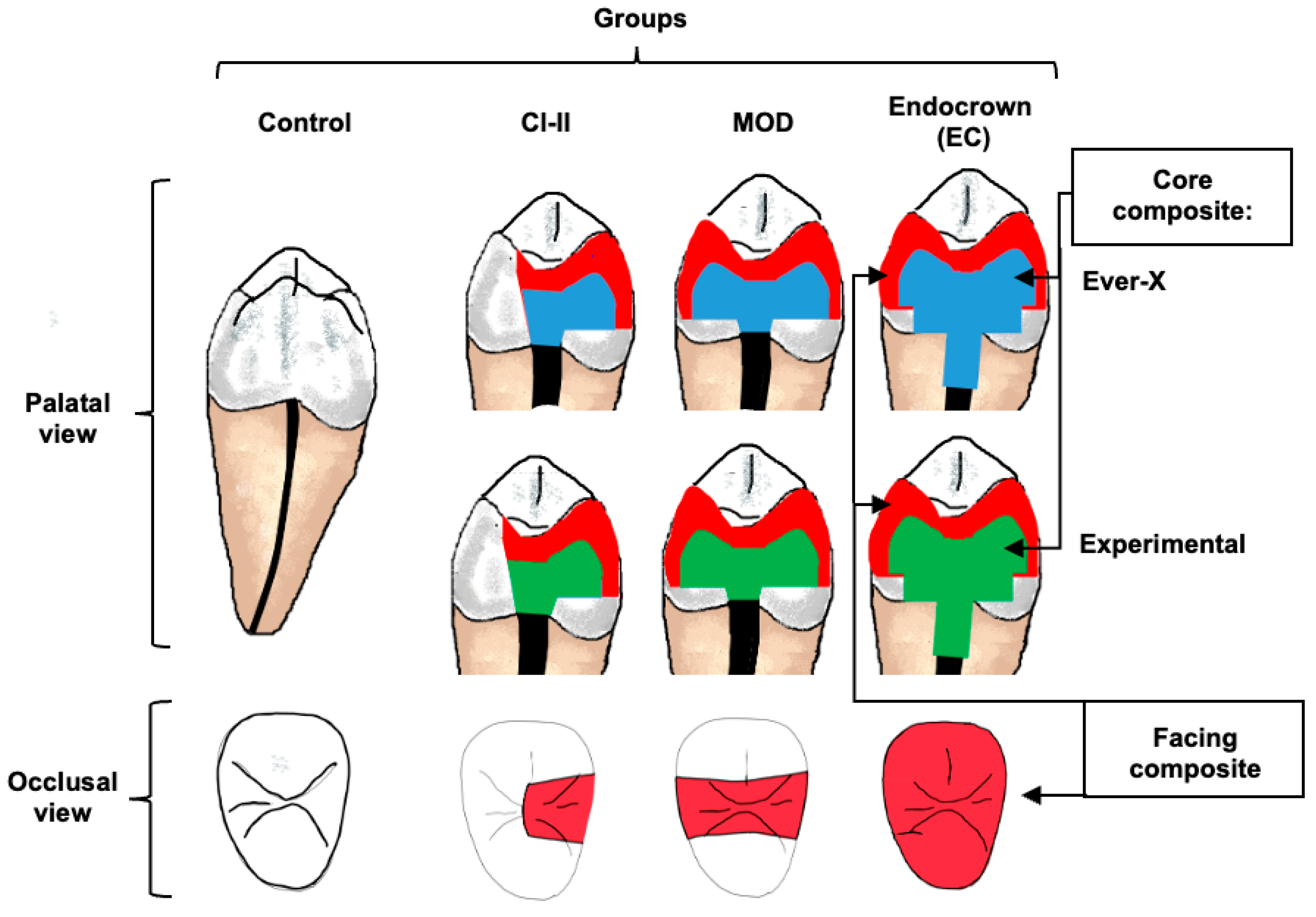
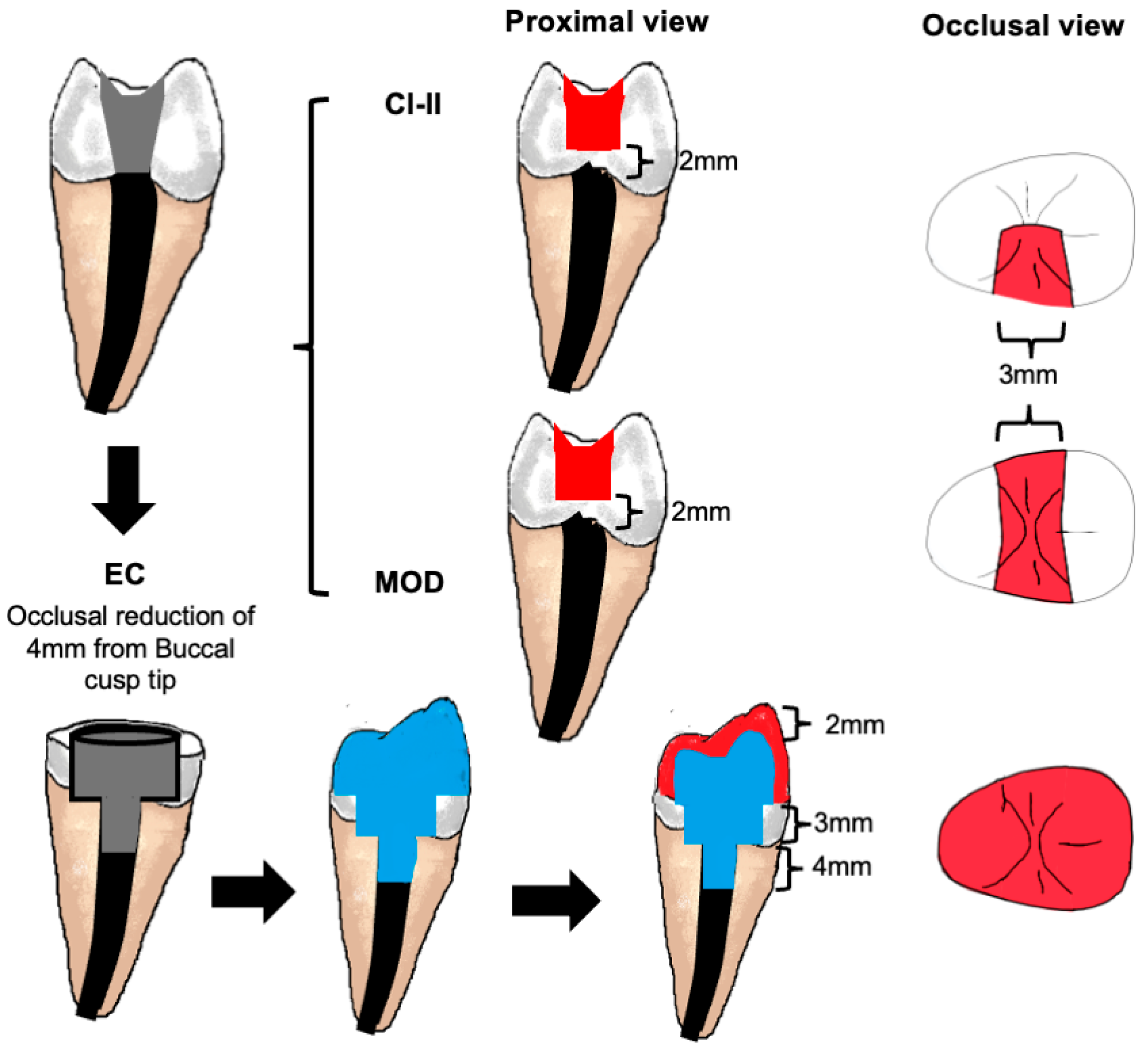
| Group | Extent of Residual Coronal Dental Tissues | Restoration Design |
|---|---|---|
| Control | Sound tooth | None |
| Cl-II | Access cavity + 1 missing proximal wall. | Core: Fibre-reinforced composite Facing: Occlusal + 1 proximal wall with conventional posterior composite |
| MOD | Access cavity + 2 missing proximal walls. | Core: Fibre-reinforced composite Facing: Occlusal + 2 proximal walls with conventional posterior composite |
| EC | Minimal remaining coronal dental tissues. | Core + 3 mm Nayyar post: Fibre-reinforced composite Facing: Full coverage with conventional posterior composite |
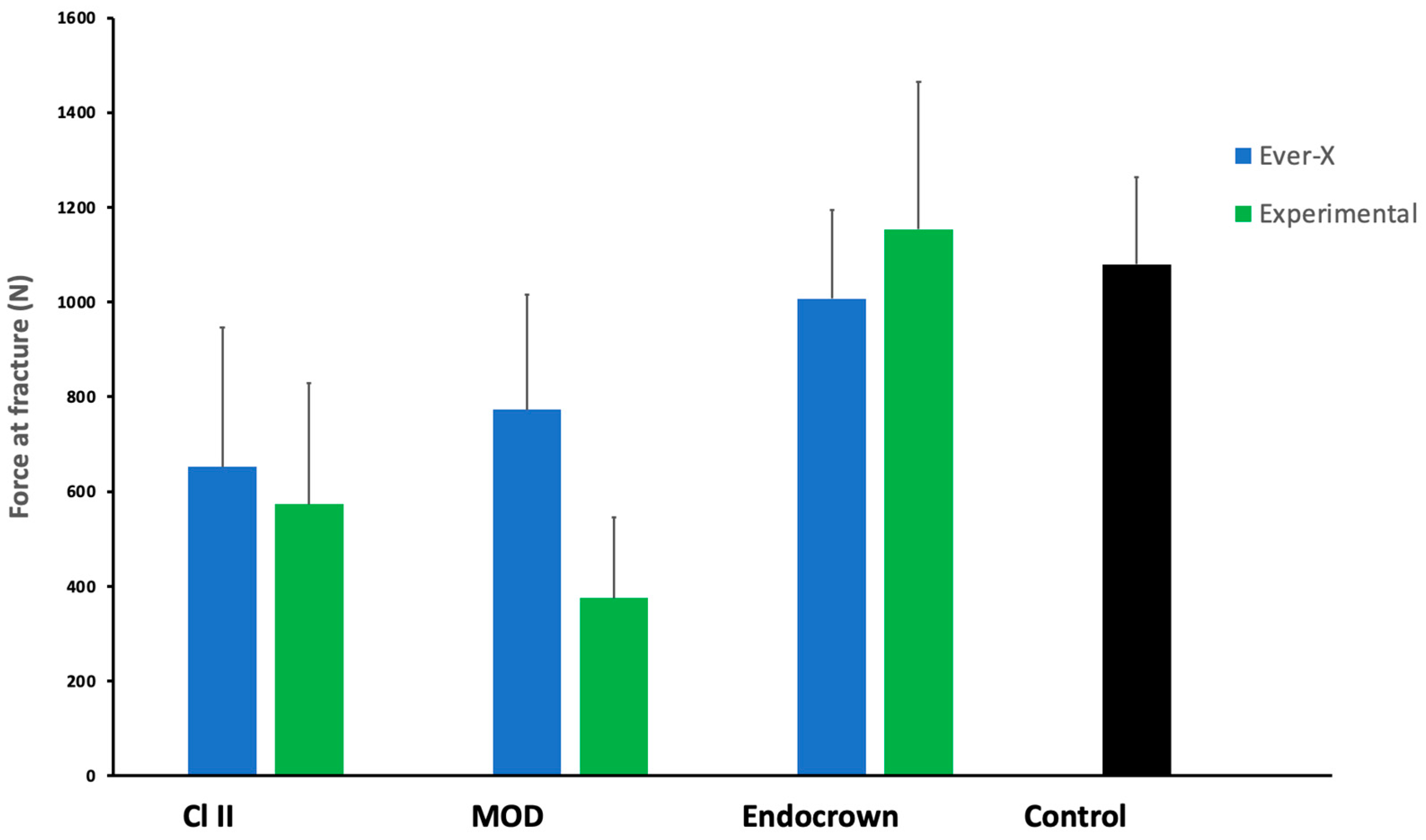
| Variables | Sum of Squares | df | Mean Square | F | Sig. |
|---|---|---|---|---|---|
| Type of material | 125,967.588 | 1 | 911,284.639 | 1.77 | 0.190 |
| Cavity design | 2,559,628.470 | 2 | 838,041.046 | 18.01 | 0.000 * |
| Interaction | 576,416.872 | 2 | 359,430.853 | 4.06 | 0.024 * |
| EverX | Exp | p-Value | |
|---|---|---|---|
| Cl II | 652.48 ± 314.04 a* | 573.53 ± 273.68 a* | |
| MOD | 773.02 ± 261.18 a,b* | 374.96 ± 168.85 a* | 0.190 |
| EC | 1006.89 ± 200.51 b | 1153.43 ± 332.52 b | |
| p-value | 0.014 | 0.0001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atmeh, A.R.; Masaud, F.; AlMuhaish, L.; Alanazi, A.; Almutiri, H.; Ali, S.; Almoqhawi, H.; Khan, A.S. Comparison of Commercial and Experimental Fibre-Reinforced Composites in Restoring Endodontically Treated Teeth with Minimal Coronal Dentine: An In Vitro Study. J. Funct. Biomater. 2025, 16, 335. https://doi.org/10.3390/jfb16090335
Atmeh AR, Masaud F, AlMuhaish L, Alanazi A, Almutiri H, Ali S, Almoqhawi H, Khan AS. Comparison of Commercial and Experimental Fibre-Reinforced Composites in Restoring Endodontically Treated Teeth with Minimal Coronal Dentine: An In Vitro Study. Journal of Functional Biomaterials. 2025; 16(9):335. https://doi.org/10.3390/jfb16090335
Chicago/Turabian StyleAtmeh, Amre R, Faisal Masaud, Luba AlMuhaish, Abdulkarim Alanazi, Hadeel Almutiri, Saqib Ali, Hassan Almoqhawi, and Abdul Samad Khan. 2025. "Comparison of Commercial and Experimental Fibre-Reinforced Composites in Restoring Endodontically Treated Teeth with Minimal Coronal Dentine: An In Vitro Study" Journal of Functional Biomaterials 16, no. 9: 335. https://doi.org/10.3390/jfb16090335
APA StyleAtmeh, A. R., Masaud, F., AlMuhaish, L., Alanazi, A., Almutiri, H., Ali, S., Almoqhawi, H., & Khan, A. S. (2025). Comparison of Commercial and Experimental Fibre-Reinforced Composites in Restoring Endodontically Treated Teeth with Minimal Coronal Dentine: An In Vitro Study. Journal of Functional Biomaterials, 16(9), 335. https://doi.org/10.3390/jfb16090335








