Shear Bond Strength of Self-Adhesive and Self-Etching Resin Cements to Dentin for Indirect Restorations
Abstract
1. Introduction
2. Materials and Methods
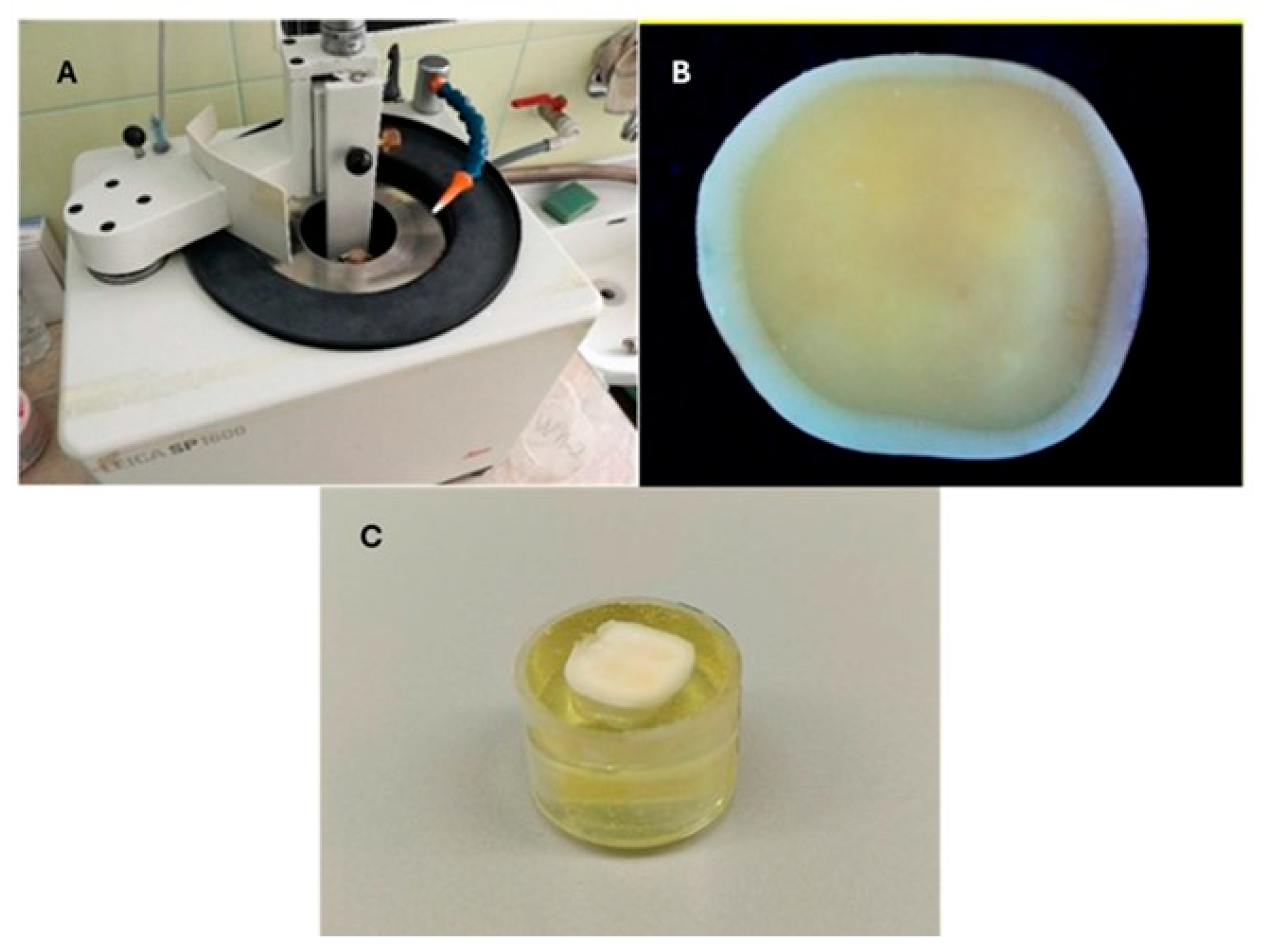
2.1. Dentin Specimen Preparation
2.2. Preparation of Samples from Different Materials
- -
- Dentin—cleaned with H2O2 and alcohol.
- -
- Samples of Cerasmart 270 and Crowntec NextDent—sandblasting with Al2O3 and silane, Silan IT (ITENA, Paris, France).
- -
- Samples of Katana Zr Noritake—sandblasting with Al2O3.
- -
- Samples of Initial LiSi Block—hydrofluoric acid (HF) and silane.
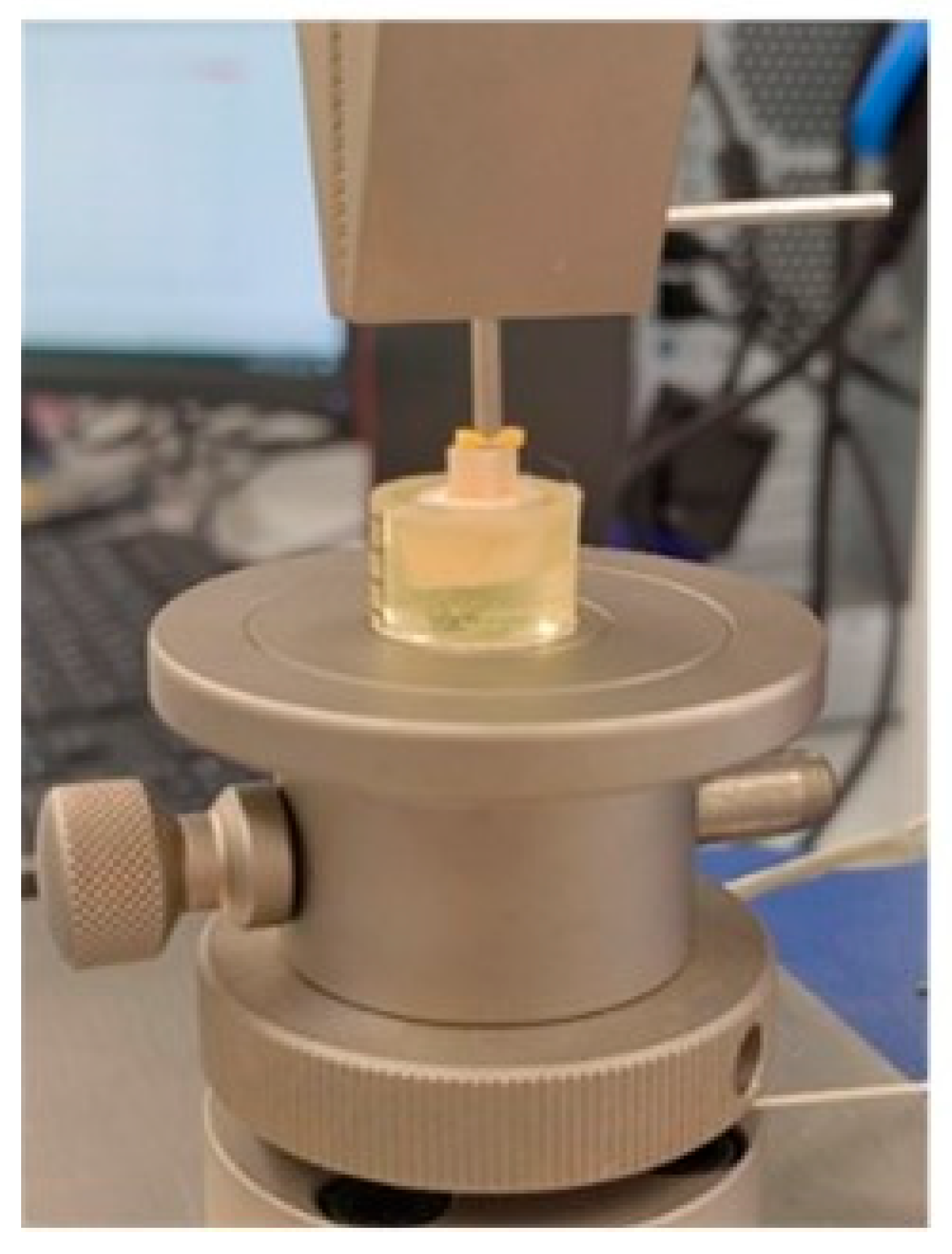
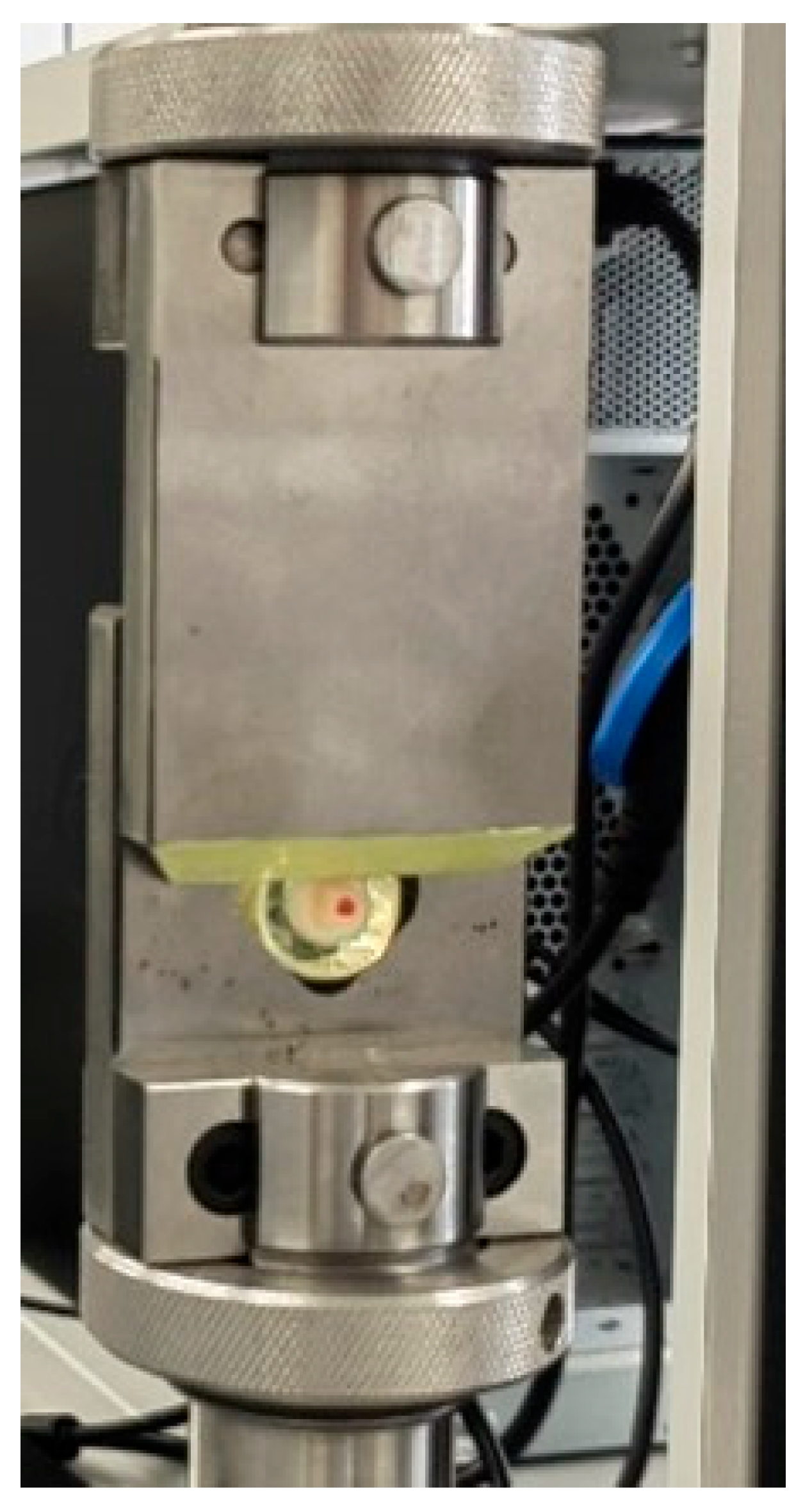
2.3. Method for Physical–Mechanical Testing of Shear Bond
- -
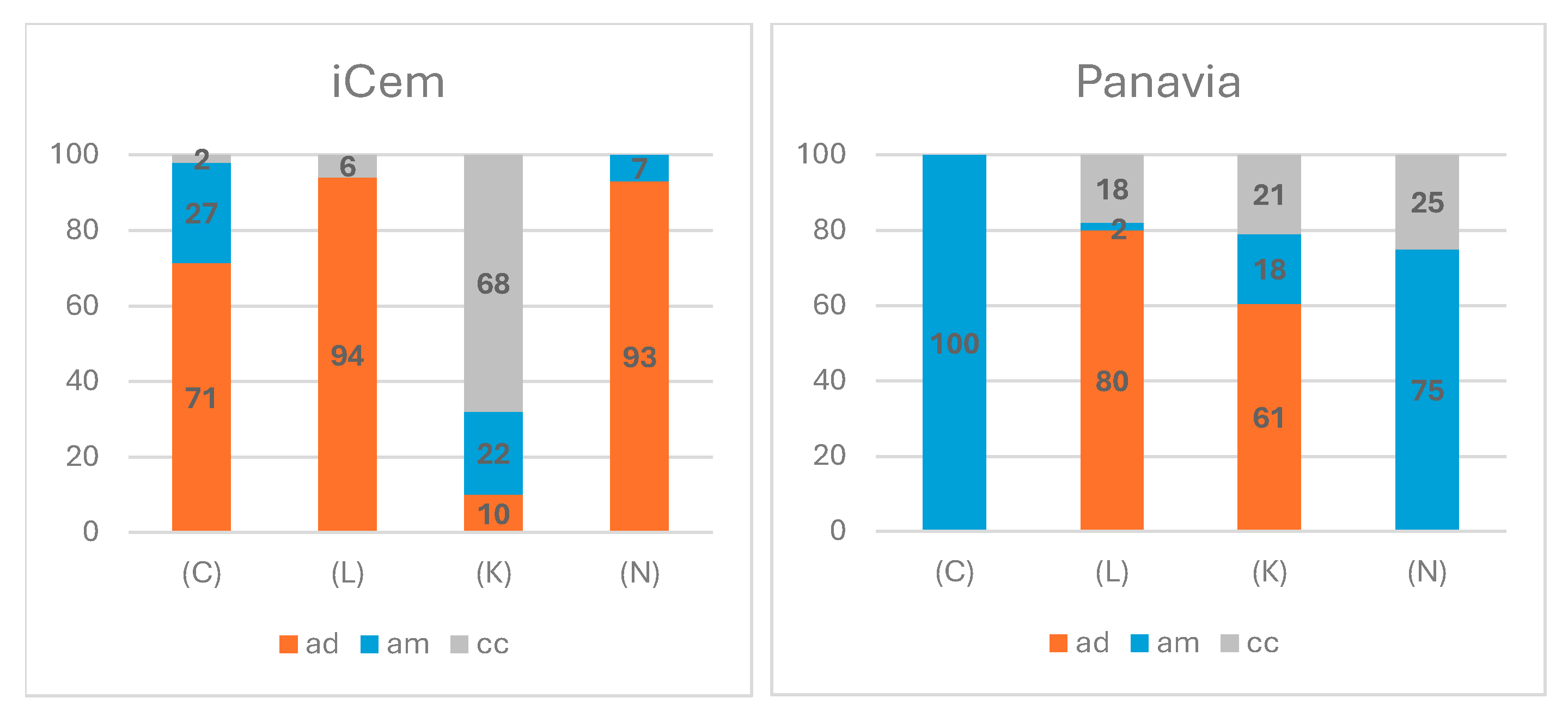
- Adhesive-type—between the cement and dentin/material surface (≥70% of the total area of the two surfaces is not covered by cement);
- -
- Cohesive-type—in the cement (≥60% of the total area of the two surfaces is covered with cement);
- -
- Mixed-type—those that do not fall into the first two groups.
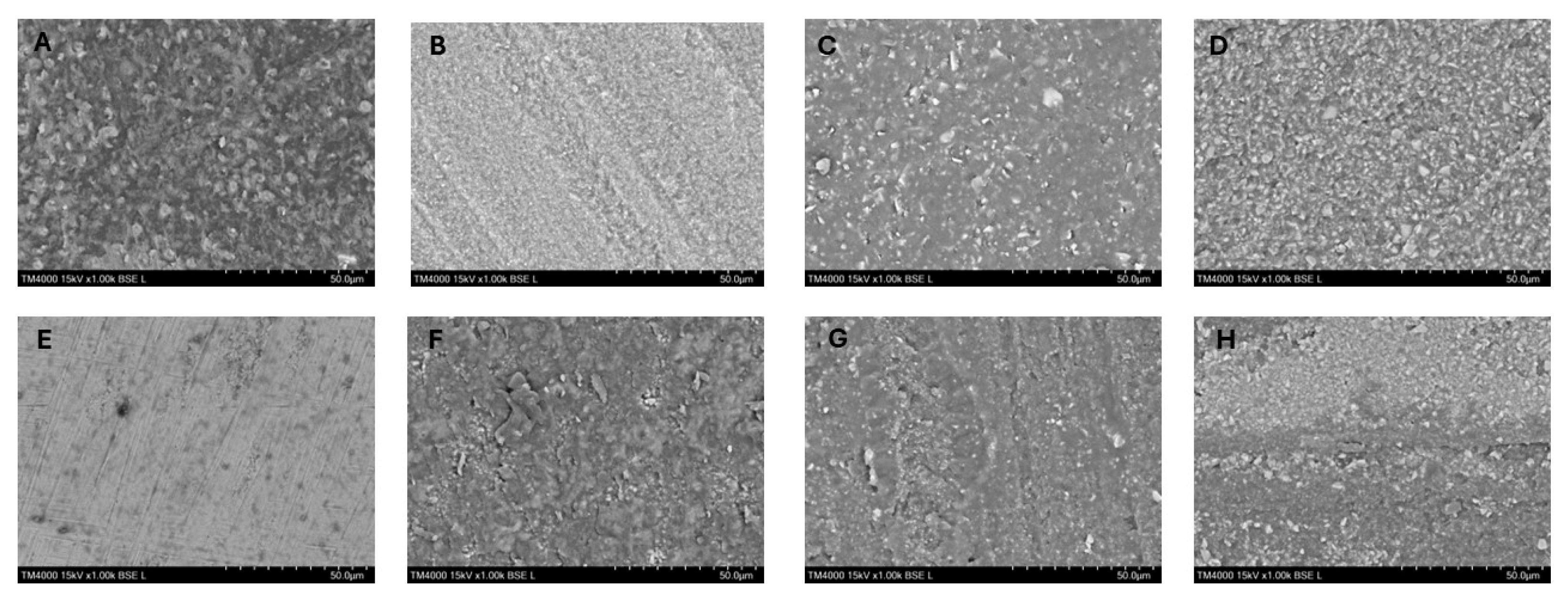
2.4. Scanning Electron Microscopy Evaluation
2.5. Statistical Analysis
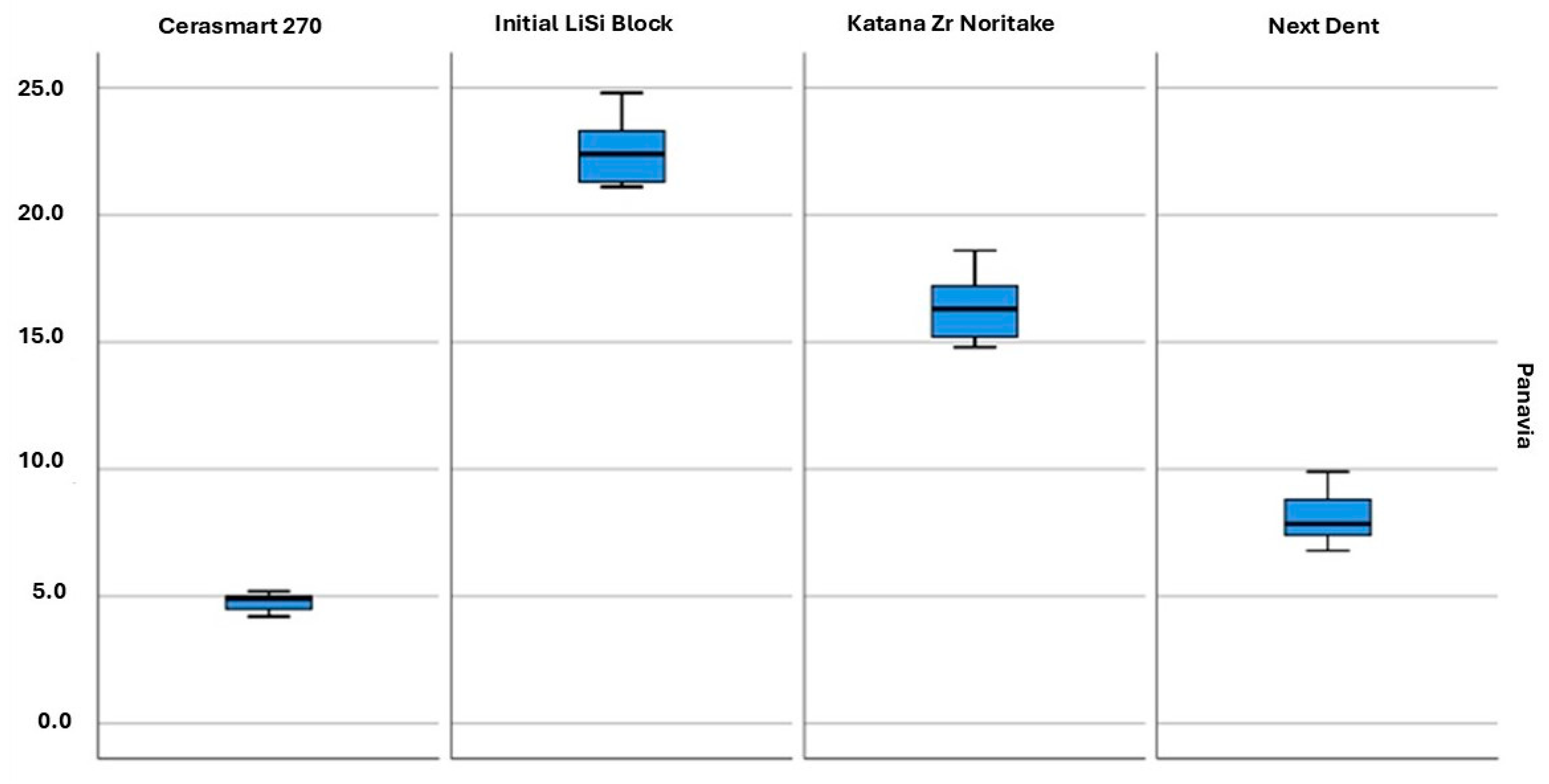
3. Results
3.1. Quantitative Evaluation Results
3.2. Qualitative Evaluation Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Topdağı, B. Optimization of Bond Strength Between Heat-Polymerized PMMA and Contemporary CAD/CAM Framework Materials: A Comparative In Vitro Study. Polymers 2025, 17, 1488. [Google Scholar] [CrossRef] [PubMed]
- Unalan Degirmenci, B.; Degirmenci, A.; Seyfioglu Polat, Z. The Influence of Thermocycling and Ultraviolet Aging on Surface Characteristics and the Repair Bond Strength of CAD/CAM Resin Nanoceramics. J. Funct. Biomater. 2025, 16, 156. [Google Scholar] [CrossRef]
- Hussain, B.; Thieu, M.K.L.; Johnsen, G.F.; Reseland, J.E.; Haugen, H.J. Can CAD/CAM resin blocks be considered as substitute for conventional resins? Dent. Mater. 2017, 33, 1362–1370. [Google Scholar] [CrossRef]
- Bömicke, W.; Rathmann, F.; Pilz, M.; Bermejo, J.L.; Waldecker, M.; Ohlmann, B.; Rammelsberg, P.; Zenthöfer, A. Clinical Performance of Posterior Inlay-Retained and Wing-Retained Monolithic Zirconia Resin-Bonded Fixed Partial Dentures: Stage One Results of a Randomized Controlled Trial. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2021, 30, 384–393. [Google Scholar] [CrossRef]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Proesthet Dent. 2015, 114, 587–589. [Google Scholar] [CrossRef] [PubMed]
- Dikici, B.; Türkeş Başaran, E.; Şirinsükan, N.; Can, E. Repair Bond Strength and Surface Roughness Evaluation of CAD/CAM Materials After Various Surface Pretreatments. Coatings 2025, 15, 432. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L. Effect of three surface treatments on the adhesive properties of indirect composite restorations. J. Adhes. Dent. 2007, 9, 319–326. [Google Scholar] [PubMed]
- Soares, C.J.; Giannini, M.; Oliveira, M.T.; Paulillo, L.A.; Martins, L.R. Effect of surface treatments of laboratory-fabricated composites on the microtensile bond strength to a luting resin cement. J. Appl. Oral Sci. 2004, 12, 45–50. [Google Scholar] [CrossRef]
- Yanakiev, S.; Marinova-Takorova, M. Silane heat treatment could eliminate the hydrofluoric acid etching of lithium disilicate overlays: A four-year follow up. Case Rep. Dent. 2021, 2021, 9961621. [Google Scholar] [CrossRef]
- Gundogdu, M.; Aladag, L.I. Effect of adhesive resin cements on bond strength of ceramic core materials to dentin. Niger. J. Clin. Pract. 2018, 21, 367–374. [Google Scholar] [CrossRef]
- D’Arcangelo, C.; Vanini, L.; Casinelli, M.; Frascaria, M.; De Angelis, F.; Vadini, M.; D’Amario, M. Adhesive cementation of indirect composite inlays and onlays: A literature review. Compend. Contin. Educ. Dent. 2015, 36, 570–577. [Google Scholar]
- Manso, A.P.; Carvalho, R.M. Dental Cements for Luting and Bonding Restorations: Self-Adhesive Resin Cements. Dent. Clin. N. Am. 2017, 61, 821–834. [Google Scholar] [CrossRef] [PubMed]
- Perugia, C.; Ferraro, E.; Docimo, R. Immediate dentin sealing in indirect restorations of dental fractures in paediatric dentistry. Eur. J. Paediatr. Dent. 2013, 14, 146–149. [Google Scholar] [PubMed]
- Magdy, N.; Rabah, A. Evaluation of micro-tensile bond strength of indirect resin composite inlay to dentin. Int. J. Health Sci. Res. 2017, 7, 105–115. [Google Scholar]
- Makkar, S.; Malhotra, N. Self-adhesive resin cements: A new perspective in luting technology. Dent. Update 2013, 40, 758–768. [Google Scholar] [CrossRef]
- Maletin, A.; Knežević, M.J.; Koprivica, D.Đ.; Veljović, T.; Puškar, T.; Milekić, B.; Ristić, I. Dental Resin-Based Luting Materials—Review. Polymers 2023, 15, 4156. [Google Scholar] [CrossRef] [PubMed]
- Ho, Y.; Lai, Y.; Chou, I.; Yang, S.; Lee, S. Effects of light attenuation by fiber posts on polymerization of a dual-cured resin cement and microleakage of post-restored teeth. J. Dent. 2011, 39, 309–315. [Google Scholar] [CrossRef]
- Berzins, D.; Abey, S.; Costache, M.; Wilkie, C.; Roberts, H. Resin-modified Glass-ionomer Setting Reaction Competition. J. Dent. Res. 2009, 89, 82–86. [Google Scholar] [CrossRef]
- Hitz, T.; Stawarczyk, B.; Fischer, J.; Hämmerle, C.; Sailer, I. Are self-adhesive resin cements a valid alternative to conventional resin cements? A laboratory study of the long-term bond strength. Dent. Mater. 2012, 28, 1183–1190. [Google Scholar] [CrossRef]
- Peumans, M.; De Munck, J.; Van Landuyt, K.; Poitevin, A.; Lambrechts, P.; Van Meerbeek, B. Two-year clinical evaluation of a self-adhesive luting agent for ceramic inlays. J. Adhes. Dent. 2010, 12, 151–161. [Google Scholar]
- Christensen, G.J. Choosing an all-ceramic restorative material: Porcelain fused-to-metal or zirconia-based? J. Am. Dent. Assoc. 2007, 138, 662–665. [Google Scholar] [CrossRef]
- Simon, J.F.; Darnell, L.A. Considerations for proper selection of dental cements. Compend. Contin. Educ. Dent. 2012, 33, 28. [Google Scholar]
- Ghodsi, S.; Shekarian, M.; Aghamohseni, M.M.; Rasaeipour, S.; Arzani, S. Resin cement selection for different types of fixed partial coverage restorations: A narrative systematic review. Clin. Exp. Dent. Res. 2023, 9, 1096–1111. [Google Scholar] [CrossRef] [PubMed]
- Kaptan, A.; Bektaş, O.; Eren, D.; Doğan, D. Influence of different surface sreatments to Self-adhesive resin cement to CAD-CAM materials bonding. ODOVTOS Int. J. Dent. Sci. 2023, 25, 22–32. [Google Scholar]
- Papadopoulos, K.; Pahinis, K.; Saltidou, K.; Dionysopoulos, D.; Tsitrou, E. Evaluation of the Surface Characteristics of Dental CAD/CAM Materials after Different Surface Treatments. Materials 2020, 13, 981. [Google Scholar] [CrossRef]
- Alshabib, A.; AlDosary, K.; Algamaiah, H. A comprehensive review of resin luting agents: Bonding mechanisms and polymerisation reactions. Saudi Dent J. 2024, 36, 234–239. [Google Scholar] [CrossRef] [PubMed]
- Pimentel de Oliveira, R.; de Paula, B.L.; Ribeiro, M.E.; Alves, E.; Costi, H.T.; Silva, C. Evaluation of the Bond Strength of Self-Etching Adhesive Systems Containing HEMA and 10-MDP Monomers: Bond Strength of Adhesives Containing HEMA and 10-MDP. Int. J. Dent. 2022, 2022, 5756649. [Google Scholar] [CrossRef] [PubMed]
- Sirisha, K.; Rambabu, T.; Ravishankar, Y.; Ravikumar, P. Validity of bond strength tests: A critical review-Part II. J. Conserv. Dent. 2014, 17, 420–426. [Google Scholar] [CrossRef]
- De Angelis, F.; D’Arcangelo, C.; Buonvivere, M.; Rondoni, G.D.; Vadini, M. Shear bond strength of glass ionomer and resin-based cements to different types of zirconia. J. Esthet. Restor. Dent. 2020, 32, 806–814. [Google Scholar] [CrossRef]
- Inokoshi, M.; Poitevin, A.; De Munck, J.; Minakuchi, S.; Van Meerbeek, B. Bonding effectiveness to different chemically pre-treated dental zirconia. Clin. Oral Investig. 2014, 18, 1803–1812. [Google Scholar] [CrossRef]
- Naiboğlu, P.; Serin Kalay, T.; Aydoğan Ayaz, E. Shear Bond Strength of Chairside Cad-Cam Blocks to Eroded Dentin. Cumhur. Dent. J. 2022, 25, 156–162. [Google Scholar] [CrossRef]
- Cekic-Nagas, I.; Ergun, G.; Egilmez, F.; Vallittu, P.K.; Lassila, L.V. Micro-shear bond strength of different resin cements to ceramic/glass-polymer CAD-CAM block materials. J. Prosthodont. Res. 2016, 60, 265–273. [Google Scholar] [CrossRef]
- Brunner, K.C.; Özcan, M. Load bearing capacity and Weibull characteristics of inlay-retained resin-bonded fixed dental prosthesis made of all-ceramic, fiber-reinforced composite and metal-ceramic after cyclic loading. J. Mech. Behav. Biomed. Mater. 2020, 109, 103855. [Google Scholar] [CrossRef]
- Homsy, F.R.; Özcan, M.; Khoury, M.; Majzoub, Z.A.K. Comparison of fit accuracy of pressed lithium disilicate inlays fabricated from wax or resin patterns with conventional and CAD-CAM technologies. J. Prosthet. Dent. 2018, 120, 530–536. [Google Scholar] [CrossRef]
- Irie, M.; Okada, M.; Maruo, Y.; Nishigawa, G.; Matsumoto, T. Shear Bond Strength of Resin Luting Materials to Lithium Disilicate Ceramic: Correlation between Flexural Strength and Modulus of Elasticity. Polymers 2023, 15, 1128. [Google Scholar] [CrossRef]
- Serichetaphongse, P.; Chitsutheesiri, S.; Chengprapakorn, W. Comparison of the shear bond strength of composite resins with zirconia and titanium using different resin cements. J. Prosthodont. Res. 2022, 66, 109–116. [Google Scholar] [CrossRef]
- Elsaka, S.E. Repair bond strength of resin composite to a novel CAD/CAM hybrid ceramic using different repair systems. Dent. Mater. J. 2015, 34, 161–167. [Google Scholar] [CrossRef]
- Elsaka, S.E. Bond strength of novel CAD/CAM restorative materials to self-adhesive resin cement: The effect of surface treatments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar]
- Flury, S.; Schmidt, S.Z.; Peutzfeldt, A.; Lussi, A. Dentin bond strength of two resin-ceramic computer-aided design/computer-aided manufacturing (CAD/CAM) materials and five cements after six months storage. Dent. Mater. J. 2016, 35, 728–735. [Google Scholar] [CrossRef][Green Version]
- Hattan, M.A.; Pani, S.C.; Alomari, M. Composite bonding to stainless steel crowns using a new universal bonding and single-bottle systems. Int. J. Dent. 2013, 2013, 607405. [Google Scholar] [CrossRef]
- Yoshida, Y.; Inoue, S. Chemical analyses in dental adhesive technology. Jpn. Dent. Sci. Rev. 2012, 48, 141–152. [Google Scholar] [CrossRef]
- de Lucena Pereira, L.; Campos, F.; Dal Piva, A.M.; Gondim, L.D.; Souza, R.O.; Özcan, M. Can application of universal primers alone be a substitute for airborne-particle abrasion to improve adhesion of resin cement to zirconia? J. Adhes. Dent. 2015, 17, 169–174. [Google Scholar]
- Xie, H.; Li, Q.; Zhang, F.; Lu, Y.; Tay, F.R.; Qian, M.; Chen, C. Comparison of resin bonding improvements to zirconia between one-bottle universal adhesives and tribochemical silica coating, which is better? Dent. Mater. Off. Publ. Acad. Dent. Mater. 2016, 32, 403–411. [Google Scholar] [CrossRef]


| Materials (Manufacturer) | Composition | Procedure/Surface Treatment |
|---|---|---|
| Cerasmart 270 (GC Europe, Leuven, Belgium)—milling CAD/CAM block | 71% Silica and barium glass nanoparticles, Bis-MEPP, UDMA, DMA | Sandblasting 50 µm Al2O3 + silane |
| Initial Li Si Block (GC Europe, Leuven, Belgium)—milling CAD/CAM block | 55–80% SiO2, 10–30% Li2O; 5–20% other oxides; pigments: trace | 5% HF + silane |
| Katana Zr Noritake (Kuraray Noritake, Ins, Tokyo, Japan)—milling CAD/CAM disk | 3 mol % Y2O3 tetragonal zirconia polycrystals | Sandblasting 50 µm Al2O3 |
| Crowntec NextDent (SAREMCO Dental AG, Rebstein, Switzerland)—3D printed material | 30–50% silanised dental glass, pyrogenic silica, 4,4′-isopropylidiphenol, ethoxylated and 2-methylprop-2enoic acid, initiators. | Sandblasting 50 µm Al2O3 + silane |
| Cement | Manufacturer | Composition | |
|---|---|---|---|
| i-Cem self-adhesive resin cement | KULZER, Hanau, Germany | Paste | 51 wt% Di-, tri-, and multifunctional acrylates, initiators, stabilizers, 49 wt% filler |
| Panavia V5 self-etching resin cement | Kuraray Noritake, Tokyo, Japan | Clearfil primer | 3-MPS, ethanol, 10-MDP |
| Tooth Primer | 10-Methacryloyloxydecyl dihydrogen phosphate (MDP), 2-Hydroxyethyl methacrylate (HEMA), hydrophilic aliphatic dimethacrylate, accelerators, water. | ||
| Paste | Bis-GMA (bisphenol A-glycidyl methacrylate), TEGDMA (Triethylene glycol dimethacrylate), hydrophobic aromatic dimethacrylate, hydrophilic aliphaticdimethacrylate, initiators, accelerators, silanated barium glass filler, silanated fluoroaluminosilicate glass filler, colloidal silica, silanated aluminum oxide filler, dl-camphorquinone, pigments. | ||
| Luting Agent | CERASMART 270 | Initial LiSi Block | Katana Zr | NextDent |
|---|---|---|---|---|
| i-CEM | 3.3 ± 0.3 A,a,* | 1.8 ± 0.2 A,b | 2.0 ± 0.2 A,b | 1.9 ± 0.3 A,b |
| PANAVIA V5 | 4.8 ± 0.2 B,a | 22.6 ± 1.4 B,b | 16.4 ± 1.3 B,c | 8.1 ± 0.9 B,d |
| p-value (in column) | p < 0.01 | p < 0.01 | p < 0.01 | p < 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kirilova, J.; Iliev, G.V.; Yantcheva, S.; Deliverska, E.; Petrova, V. Shear Bond Strength of Self-Adhesive and Self-Etching Resin Cements to Dentin for Indirect Restorations. J. Funct. Biomater. 2025, 16, 289. https://doi.org/10.3390/jfb16080289
Kirilova J, Iliev GV, Yantcheva S, Deliverska E, Petrova V. Shear Bond Strength of Self-Adhesive and Self-Etching Resin Cements to Dentin for Indirect Restorations. Journal of Functional Biomaterials. 2025; 16(8):289. https://doi.org/10.3390/jfb16080289
Chicago/Turabian StyleKirilova, Janet, Georgi Veselinov Iliev, Sevda Yantcheva, Elitsa Deliverska, and Viktoria Petrova. 2025. "Shear Bond Strength of Self-Adhesive and Self-Etching Resin Cements to Dentin for Indirect Restorations" Journal of Functional Biomaterials 16, no. 8: 289. https://doi.org/10.3390/jfb16080289
APA StyleKirilova, J., Iliev, G. V., Yantcheva, S., Deliverska, E., & Petrova, V. (2025). Shear Bond Strength of Self-Adhesive and Self-Etching Resin Cements to Dentin for Indirect Restorations. Journal of Functional Biomaterials, 16(8), 289. https://doi.org/10.3390/jfb16080289






