Characteristics of Occlusal Force and Masticatory Performance in Female Patients Who Selected Implant Treatment for a Missing Mandibular Second Molar: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
- Patients who had untreated, missing teeth in areas other than the one planned for implant treatment.
- Patients who were undergoing implant treatment in other areas.
- Patients with at least one erupted third molar on the left or right side of the upper or lower jaw.
- Patients who had lost a mandibular second molar within the past 3 months.
- Patients with insufficient bone volume, in whom the distance to the mandibular canal of the second molar where an implant was placed was ≤10 mm.
- Patients wearing a removable prosthetic device.
- Patients with temporomandibular disorders.
- Patients with mobile teeth due to periodontitis.
- Patients who had difficulty communicating due to mental illness.
- Patients with bone metabolic disease (such as osteoporosis and rheumatoid arthritis).
- Patients who had previously received radiation therapy for the jawbone.
- Patients taking bone resorption inhibitors.
- (1)
- Maximal occlusal force (Figure 2)
- (2)
- Masticatory performance (Figure 3)
- (3)
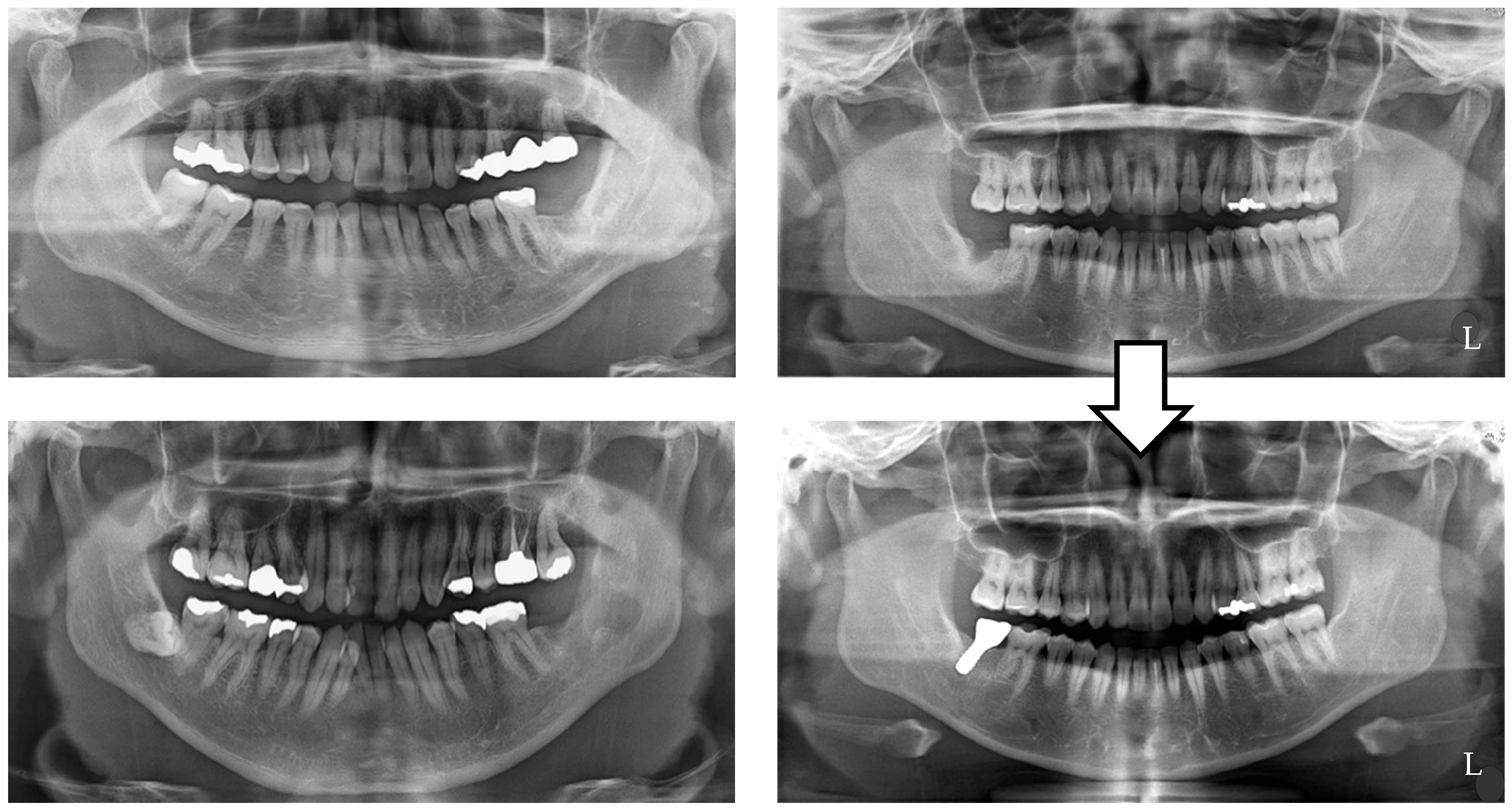
- Gonial angle (Figure 4)
Statistical Analysis
3. Results
- Maximal occlusal force
- 2.
- Masticatory performance
- 3.
- Gonial angle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Howe, M.S.; Keys, W.; Richards, D. Long-term (10-year) dental implant survival: A systematic review and sensitivity meta-analysis. J. Dent. 2019, 84, 9–21. [Google Scholar] [CrossRef] [PubMed]
- Tomasi, C.; Derks, J. Etiology, occurrence, and consequences of implant loss. Periodontol. 2000 2022, 88, 13–35. [Google Scholar] [CrossRef] [PubMed]
- Matos, G.R.M. Surface Roughness of Dental Implant and Osseointegration. J. Maxillofac. Oral. Surg. 2021, 20, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Carosi, P.; Lorenzi, C.; Laureti, M.; Ferrigno, N.; Arcuri, C. Short Dental Implants (≤6 mm) to Rehabilitate Severe Mandibular Atrophy: A Systematic Review. Int. J. Oral Maxillofac. Implant. 2021, 36, 30–37. [Google Scholar] [CrossRef]
- Stacchi, C.; Coyac, B.R.; Helms, J.A. Biomechanical Basis for Bone Healing and Osseointegration of Implants in Sinus Grafts. Clin. Implant. Dent. Relat. Res. 2025, 27, e13424. [Google Scholar] [CrossRef]
- Raghoebar, G.M.; Onclin, P.; Boven, G.C.; Vissink, A.; Meijer, H.J.A. Long-term effectiveness of maxillary sinus floor augmentation: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 307–318. [Google Scholar] [CrossRef]
- Win, K.Z.; Pimkhaokham, A.; Kaboosaya, B. Comparing Bone Graft Success, Implant Survival Rate, and Marginal Bone Loss: A Retrospective Study on Materials and Influential Factors. J. Oral Implantol. 2024, 50, 300–307. [Google Scholar] [CrossRef]
- Yoshida, T.; Masaki, C.; Komai, H.; Misumi, S.; Mukaibo, T.; Kondo, Y.; Nakamoto, T.; Hosokawa, R. Changes in oral health-related quality of life during implant treatment in partially edentulous patients: A prospective study. J. Prosthodont. Res. 2016, 60, 258–264. [Google Scholar] [CrossRef]
- Kanehira, Y.; Arai, K.; Kanehira, T.; Nagahisa, K.; Baba, S. Oral health-related quality of life in patients with implant treatment. J. Adv. Prosthodont. 2017, 9, 476–481. [Google Scholar] [CrossRef]
- Ting, M.; Suzuki, J.B. Peri-Implantitis. Dent. J. 2024, 12, 251. [Google Scholar] [CrossRef]
- da Silva Bezerra, A.; Ribeiro, A.K.C.; Veríssimo, A.H.; de Almeida, E.O. Prosthetic complications and failures of implant-supported fixed partial dentures: A scoping review. J. Prosthet. Dent. 2023, in press. [CrossRef] [PubMed]
- Smeets, R.; Henningsen, A.; Jung, O.; Heiland, M.; Hammächer, C.; Stein, J.M. Definition, etiology, prevention and treatment of peri-implantitis—A review. Head Face Med. 2014, 10, 34. [Google Scholar] [CrossRef] [PubMed]
- Anderson, N.; Lords, A.; Laux, R.; Woodall, W.; Abubakr, N.H. Retrospective Analysis of the Risk Factors of Peri-implantitis. J. Contemp. Dent. Pract. 2020, 21, 1350–1353. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Qiu, L. Analysis of fractured dental implant body from five different implant systems: A long-term retrospective study. Int. J. Oral Maxillofac. Surg. 2022, 51, 1355–1361. [Google Scholar] [CrossRef]
- Moraschini, V.; Kischinhevsky, I.C.C.; Sartoretto, S.C.; de Almeida Barros Mourão, C.F.; Sculean, A.; Calasans-Maia, M.D.; Shibli, J.A. Does implant location influence the risk of peri-implantitis? Periodontol. 2000 2022, 90, 224–235. [Google Scholar] [CrossRef]
- Campos, F.L.; Rodrigues, L.G.; Campos, J.R.; Rhodes, G.A.C.; Morais, G.F.; Chalub, L.L.F.H.; Ferreira, R.C. Association between shortened dental configurations and health outcomes: A scoping review. BMC Oral Health 2024, 24, 111. [Google Scholar] [CrossRef]
- van de Rijt, L.J.M.; Stoop, C.C.; Weijenberg, R.A.F.; de Vries, R.; Feast, A.R.; Sampson, E.L.; Lobbezoo, F. The Influence of Oral Health Factors on the Quality of Life in Older People: A Systematic Review. Gerontologist 2020, 60, e378–e394. [Google Scholar] [CrossRef]
- Funke, N.; Fankhauser, N.; Mckenna, G.J.; Srinivasan, M. Impact of shortened dental arch therapy on nutritional status and treatment costs in older adults: A systematic review. J Dent. 2023. [Google Scholar] [CrossRef]
- Walter, M.H.; Marré, B.; Dreyhaupt, J.; Heydecke, G.; Rauch, A.; Mundt, T.; Hannak, W.; Kohal, R.J.; Kern, M.; Nothdurft, F.; et al. Rehabilitation of shortened dental arches: A fifteen-year randomised trial. J. Oral Rehabil. 2021, 48, 738–744. [Google Scholar] [CrossRef]
- Sano, M.; Shiga, H. Evaluation of occlusal force and masticatory performance in elderly adults with natural dentition unaffected by occlusal support. J. Oral Sci. 2021, 63, 145–147. [Google Scholar] [CrossRef]
- Nokubi, T.; Yoshimuta, Y.; Nokubi, F.; Yasui, S.; Kusunoki, C.; Ono, T.; Maeda, Y.; Yokota, K. Validity and reliability of a visual scoring method for masticatory ability using test gummy jelly. Gerodontology 2013, 30, 76–82. [Google Scholar] [CrossRef]
- Shiga, H.; Nakajima, K.; Uesugi, H.; Komino, M.; Sano, M.; Arai, S. Reference value of masticatory performance by measuring the amount of glucose extraction from chewing gummy jelly. J. Prosthodont. Res. 2022, 66, 618–622. [Google Scholar] [CrossRef] [PubMed]
- Al-Gunaid, T.H.; Sunitan, A.K.; Alharbi, A.B.; Alhrbei, E.A.; Saito, I. Relationship between mandibular dimensions and bite force: An exploratory study. Orthod. Waves 2021, 80, 117–123. [Google Scholar] [CrossRef]
- Walter, M.H.; Dreyhaupt, J.; Mundt, T.; Kohal, R.; Kern, M.; Rauch, A.; Nothdurft, F.; Hartmann, S.; Böning, K.; Boldt, J.; et al. Periodontal health in shortened dental arches: A 10-year RCT. J. Prosthodont. Res. 2020, 64, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Sharaf, M.; Eskander, A. Attachment-Retained Unilateral Partial Denture versus Tooth Implant-Supported Prosthesis in Mandibular Distal Extension Cases: A Randomized Controlled Trial. Open Dent. J. 2021, 15, 626–635. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr.; Giannakopoulos, N.N.; Listl, S. How strong is the evidence for the need to restore posterior bounded edentulous spaces in adults? Grading the quality of evidence and the strength of recommendations. J. Dent. 2011, 39, 108–116. [Google Scholar] [CrossRef]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 565–577. [Google Scholar] [CrossRef]
- Uesugi, T.; Shimoo, Y.; Munakata, M.; Kataoka, Y.; Sato, D.; Yamaguchi, K.; Sanda, M.; Fujimaki, M.; Nakayama, K.; Watanabe, T.; et al. A Study of the Associated Risk Factors for Early Failure and the Effect of Photofunctionalisation in Full-Arch Immediate Loading Treatment Based on the All-on-Four Concept. Bioengineering 2024, 11, 223. [Google Scholar] [CrossRef]
- Gonçalves, G.S.Y.; de Magalhães, K.M.F.; Rocha, E.P.; Dos Santos, P.H.; Assunção, W.G. Oral health-related quality of life and satisfaction in edentulous patients rehabilitated with implant-supported full dentures all-on-four concept: A systematic review. Clin. Oral Investig. 2022, 26, 83–94. [Google Scholar] [CrossRef]
- Curtis, D.A.; Lin, G.H.; Rajendran, Y.; Gessese, T.; Suryadevara, J.; Kapila, Y.L. Treatment planning considerations in the older adult with periodontal disease. J. Periodontol. 2021, 87, 157–165. [Google Scholar] [CrossRef]
- Diaz, P.; Gonzalo, E.; Villagra, L.J.G.; Miegimolle, B.; Suarez, M.J. What is the prevalence of peri-implantitis? A systematic review and meta-analysis. BMC Oral Health 2022, 22, 449. [Google Scholar] [CrossRef]
- Gobbato, L.; Avila-Ortiz, G.; Sohrabi, K.; Wang, C.W.; Karimbux, N. The Effect of Keratinized Mucosa Width on Peri-implant Health: A Systematic Review. Int. J. Oral Implant. 2013, 28, 1536–1545. [Google Scholar] [CrossRef] [PubMed]
- Monje, A.; Wang, H.L.; Nart, J. Association of Preventive Maintenance Therapy Compliance and Peri-Implant Diseases: A Cross-Sectional Study. J. Periodontol. 2017, 88, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Horibe, Y.; Matsuo, K.; Ikebe, K.; Minakuchi, S.; Sato, Y.; Sakurai, K.; Ueda, T. Relationship between two pressure-sensitive films for testing reduced occlusal force in diagnostic criteria for oral hypofunction. Gerodontology 2022, 39, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Shiga, H.; Komino, M.; Yokoyama, M.; Sano, M.; Arakawa, I.; Nakajima, K.; Fujii, S. Relationship between age and occlusal force in adults with natural dentition. Odontology 2023, 111, 487–492. [Google Scholar] [CrossRef]
- Nimura, K.; Shiga, H.; Yokoyama, M. Relationships of physical constitution with occlusal force and masticatory performance in adults with natural dentition. Odontology 2023, 111, 1018–1024. [Google Scholar] [CrossRef]
- Yokoi, T.; Kusumoto, Y.; Abe, Y.; Watanabe, H.; Sanda, M.; Hara, M.; Matsumoto, T.; Baba, K. Association between the treatment choice of implant-supported fixed partial dentures and oral health-related quality of life in patients with a shortened dental arch: A preliminary observational study. J. Dent. Sci. 2024, 19, 1667–1672. [Google Scholar] [CrossRef]
- Miwa, S.; Wada, M.; Murakami, S.; Suganami, T.; Ikebe, K.; Maeda, Y. Gonial Angle Measured by Orthopantomography as a Predictor of Maximum Occlusal Force. J. Prosthodont. 2019, 28, e426–e430. [Google Scholar] [CrossRef]
- Bakan, A.; Kervancıoğlu, P.; Bahşi, İ.; Yalçın, E.D. Comparison of the Gonial Angle With Age and Gender Using Cone-Beam Computed Tomography Images. Cureus 2022, 14, e24997. [Google Scholar] [CrossRef]
- Akter, T.; Takashima, M.; Arai, Y.; Matsuzaki, N.; Yamazaki, Y.; Nohno, K. Gonial angle and late implant loss: A retrospective clinical study. J. Prosthodont. Res. 2025, 69, 120–126. [Google Scholar] [CrossRef]
- Greenstein, G.; Greenstein, B.; Carpentieri, J. The Need to Replace a Missing Second Molar With a Dental Implant Restoration: Analysis of a Controversial Issue. Compend. Contin. Educ. Dent. 2018, 39, 686–693. [Google Scholar] [PubMed]
- Esposito, M.; Barausse, C.; Pistilli, R.; Checchi, V.; Diazzi, M.; Gatto, M.R.; Felice, P. Posterior jaws rehabilitated with partial prostheses supported by 4.0 × 4.0 mm or by longer implants: Four-month post-loading data from a randomised controlled trial. Eur. J. Oral Implantol. 2015, 8, 221–230. [Google Scholar] [PubMed]
- Nam, D.H.; Lee, D.W.; Chung, C.J.; Kim, K.H.; Park, K.H.; Moon, I.S. Change in masticatory ability with the implant restoration of second molars. J. Prosthet. Dent. 2014, 111, 286–292. [Google Scholar] [CrossRef]
- Abutayyem, H.; Annamma, L.M.; Desai, V.B.; Alam, M.K. Evaluation of occlusal bite force distribution by T-Scan in orthodontic patients with different occlusal characteristics: A cross sectional-observational study. BMC Oral Health 2023, 23, 888. [Google Scholar] [CrossRef] [PubMed]



| IT Group | NT Group | p-Value | |
|---|---|---|---|
| Age | 54.5 ± 7.1 years | 56.0 ± 7.8 years | 0.78 |
| Maximal occlusal force | 739.2 ± 374.9 N | 584.1 ± 293.4 N | 0.021 < 0.05 |
| Masticatory performance | 235.8 ± 127.1 mg/dL | 215.5 ± 76.5 mg/dL | 0.51 |
| Gonial angle | 125.0 ± 5.1° | 121.9 ± 9.8° | 0.314 |
| r | p | |
|---|---|---|
| Maximal occlusal force | ||
| IT group | −0.16 | 0.316 |
| NT group | 0.65 | 0.117 |
| Masticatory performance | ||
| IT group | 0.53 | 0.047 < 0.05 |
| NT group | 0.13 | 0.39 |
| Gonial angle | ||
| IT group | 0.16 | 0.248 |
| NT group | 0.65 | 0.159 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abe, T.; Munakata, M.; Yokoi, T.; Yamaguchi, K.; Sato, D.; Baba, K. Characteristics of Occlusal Force and Masticatory Performance in Female Patients Who Selected Implant Treatment for a Missing Mandibular Second Molar: A Retrospective Study. J. Funct. Biomater. 2025, 16, 211. https://doi.org/10.3390/jfb16060211
Abe T, Munakata M, Yokoi T, Yamaguchi K, Sato D, Baba K. Characteristics of Occlusal Force and Masticatory Performance in Female Patients Who Selected Implant Treatment for a Missing Mandibular Second Molar: A Retrospective Study. Journal of Functional Biomaterials. 2025; 16(6):211. https://doi.org/10.3390/jfb16060211
Chicago/Turabian StyleAbe, Takashi, Motohiro Munakata, Takumi Yokoi, Kikue Yamaguchi, Daisuke Sato, and Kazuyoshi Baba. 2025. "Characteristics of Occlusal Force and Masticatory Performance in Female Patients Who Selected Implant Treatment for a Missing Mandibular Second Molar: A Retrospective Study" Journal of Functional Biomaterials 16, no. 6: 211. https://doi.org/10.3390/jfb16060211
APA StyleAbe, T., Munakata, M., Yokoi, T., Yamaguchi, K., Sato, D., & Baba, K. (2025). Characteristics of Occlusal Force and Masticatory Performance in Female Patients Who Selected Implant Treatment for a Missing Mandibular Second Molar: A Retrospective Study. Journal of Functional Biomaterials, 16(6), 211. https://doi.org/10.3390/jfb16060211








