An Assessment of the Micro-Tensile Bond Strength of Composites for Indirect Restoration to Enamel and Dentin
Abstract
1. Introduction
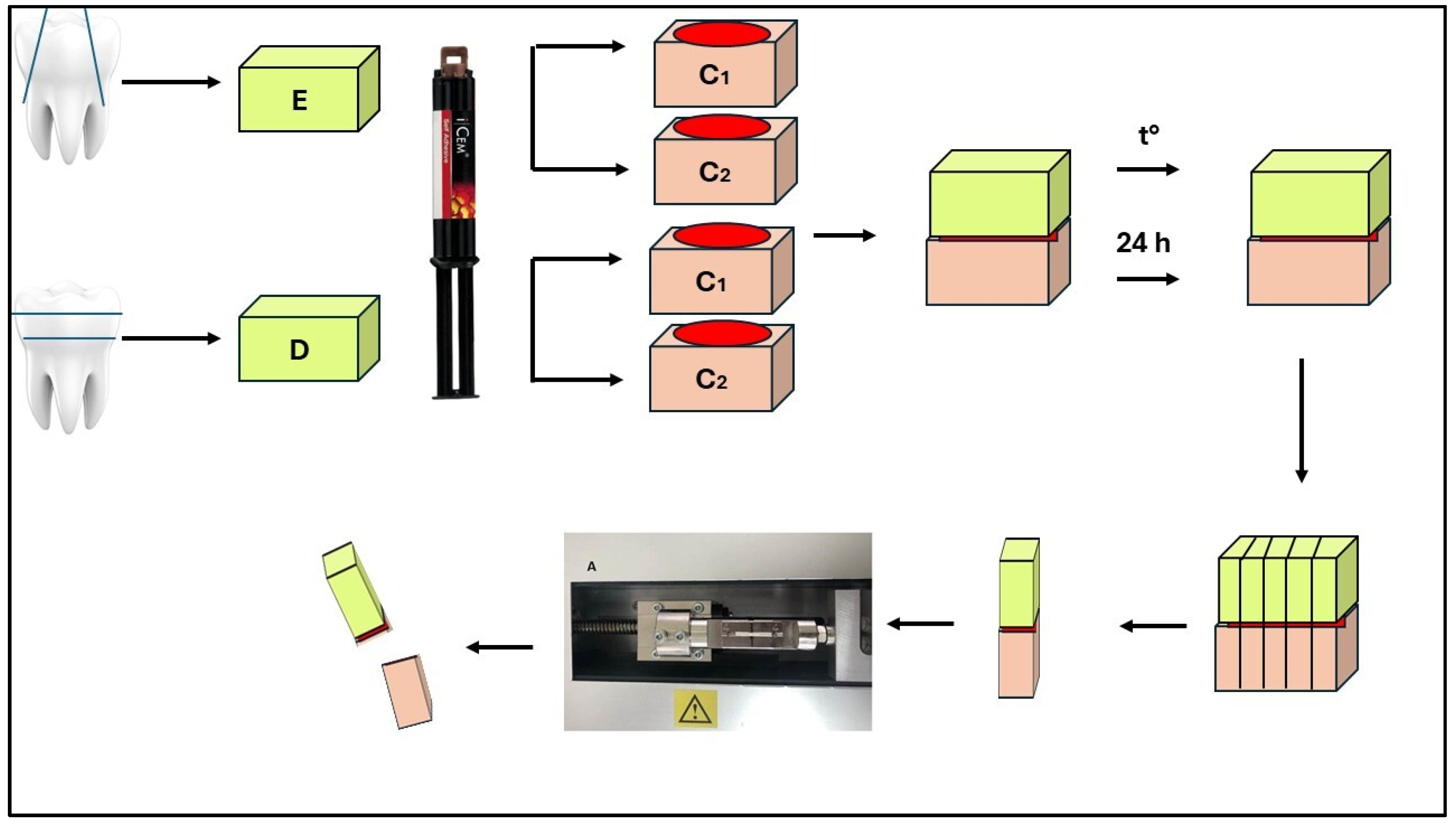
2. Materials and Methods
2.1. Fabrication of Composite Samples
2.2. Preparation of Enamel Specimens
2.3. Preparation of Dentin Specimens
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- El-Askary, F.; Hassanein, A.; Aboalazm, E.; Al-Haj Husain, N.; Özcan, M. A Comparison of Microtensile Bond Strength, Film Thickness, and Microhardness of Photo-Polymerized Luting Composites. Materials 2022, 15, 3050. [Google Scholar] [CrossRef] [PubMed]
- Haruyama, A.; Muramatsu, T.; Kameyama, A. The Effect of Silane Treatment of a Resin-Based Composite on Its Microtensile Bond Strength to a Ceramic Restorative Material. Appl. Sci. 2024, 14, 9178. [Google Scholar] [CrossRef]
- Cassin, A.M.; Pearson, G.J. Microleakage studies comparing a one-visit indirect composite inlay system and a direct composite restorative technique. J. Oral Rehabil. 1992, 19, 265–270. [Google Scholar] [CrossRef] [PubMed]
- De Andrade, O.S.; de Goes, M.F.; Montes, M.A. Marginal adaptation and microtensile bond strength of composite indirect restorations bonded to dentin treated with adhesive and low-viscosity composite. Dent. Mater. 2007, 23, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.J.; Ferrance, J.; Kang, K.; Dhont, J.; Lee, I.B. Spatio-temporal analysis of shrinkage vectors during photo-polymerization of composite. Dent. Mater. 2013, 29, 1236–1243. [Google Scholar] [CrossRef]
- Boaro, L.C.; Goncalves, F.; Guimares, T.C.; Ferracane, J.L.; Pfeifer, C.S.; Braga, R.P. Sorption, solubility, shrinkage and mechanical properties of low-shrinkage commercial resin composites. Dent. Mater. 2013, 29, 398–404. [Google Scholar] [CrossRef]
- Lauvahutanon, S.; Takahashi, H.; Shiozawa, M.; Iwasiki, N.; Asahawa, Y.; Oki, M.; Finger, W.; Arksornnukit, M. Mechanical properties of composite resin blocks for CAD/CAM. Dent. Mater. 2014, 33, 705–710. [Google Scholar] [CrossRef]
- Nguyen, J.F.; Migonney, V.; Ruse, N.D.; Sadoun, M. Resin composite blocks via high-pressure high-temperature polymerization. Dent. Mater. 2012, 28, 529–534. [Google Scholar] [CrossRef]
- Nandini, S. Indirect resin composites. J. Conserv. Dent. 2010, 13, 184–194. [Google Scholar] [CrossRef]
- Mandikos, M.N.; McGivney, G.P.; Davis, E.; Bush, P.J.; Carter, J.M. A comparison of the wear resistance and hardness of indirect composite resins. J. Prost. Dent. 2001, 85, 386–395. [Google Scholar] [CrossRef]
- Dikici, B.; Türkeş Başaran, E.; Can, E. Does the Type of Resin Luting Material Affect the Bonding of CAD/CAM Materials to Dentin? Dent. J. 2025, 13, 41. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, T.; Hotta, Y.; Kunii, J.; Kuriyama, S.; Tamaki, Y. A review of dental CAD/CAM: Current status and future perspectives from 20 years of experience. Dent. Mater. 2009, 28, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Boitile, P.; Mawusii, B.; Tapie, L.; Fromentin, O. A systematic review of CAD/CAM fit restoration evaluations. J. Oral Rehabil. 2014, 41, 853–874. [Google Scholar] [CrossRef]
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef] [PubMed]
- Paradigm™. MZ100 Block: Technical Product Profile; 3M ESPE: St. Paul, MN, USA, 2000. [Google Scholar]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef]
- Antoniou, I.; Mourouzis, P.; Dionysopoulos, D.; Pandoleon, P.; Tolidis, K. Influence of Immediate Dentin Sealing on Bond Strength of Resin-Based CAD/CAM Restoratives to Dentin: A Systematic Review of In Vitro Studies. Biomimetics 2024, 9, 267. [Google Scholar] [CrossRef]
- Bellan, M.C.; Cunha, P.F.J.S.D.; Tavares, J.G.; Spohr, A.M.; Mota, E.G. Microtensile bond strength of CAD/CAM materials to dentin under different adhesive strategies. Braz. Oral Res. 2017, 18, e109. [Google Scholar] [CrossRef]
- Kaptan, A.; Bektaş, O.; Eren, D.; Doğan, D. Influence of different surface sreatments to Self-adhesive resin cement to CAD-CAM materials bonding. ODOVTOS Int. J. Dent. Sc. 2023, 25, 22–32. [Google Scholar]
- Papadopoulos, K.; Pahinis, K.; Saltidou, K.; Dionysopoulos, D.; Tsitrou, E. Evaluation of the Surface Characteristics of Dental CAD/CAM Materials after Different Surface Treatments. Materials 2020, 13, 981. [Google Scholar] [CrossRef]
- Manso, A.P.; Carvalho, R.M. Dental Cements for Luting and Bonding Restorations: Self-Adhesive Resin Cements. Dent. Clin. N. Am. 2017, 61, 821–834. [Google Scholar] [CrossRef]
- Wu, C.-Y.; Nakamura, K.; Miyashita-Kobayashi, A.; Haruyama, A.; Yokoi, Y.; Kuroiwa, A.; Yoshinari, N.; Kameyama, A. The Effect of Additional Silane Pre-Treatment on the Microtensile Bond Strength of Resin-Based Composite Post-and-Core Build-Up Material. Appl. Sci. 2024, 14, 6637. [Google Scholar] [CrossRef]
- Awad, M.M.; Alhalabi, F.; Alshehri, A.; Salem, M.A.; Robaian, A.; Alghannam, S.; Alayad, A.S.; Almutairi, B.; Alrahlah, A. Silane-Containing Universal Adhesives Influence Resin-Ceramic Microtensile Bond Strength. Coatings 2023, 13, 477. [Google Scholar] [CrossRef]
- Bracher, L.; Ozcan, M. Adhesion of resin composite to enamel and dentin: A methodological assessment. J. Adhes. Sci. Technol. 2018, 32, 258–271. [Google Scholar] [CrossRef]
- Chin, A.; Ikeda, M.; Takagaki, T.; Nikaido, T.; Sadr, A.; Shimada, Y.; Tagami, J. Effects of Immediate and Delayed Cementations for CAD/CAM Resin Block after Alumina Air Abrasion on Adhesion to Newly Developed Resin Cement. Materials 2021, 14, 7058. [Google Scholar] [CrossRef] [PubMed]
- Gerdzhikov, I.; Uzunov, T.; Radeva, E. Evaluation of Microtensile Bond Strength of Luting Cements to Zirconia Ceramics. Wulfenia 2021, 28, 2–11. [Google Scholar]
- Nakazawa, M.; Maeno, M.; Komoto, M.; Nara, Y. Appropriate Immediate Dentin Sealing to Improve the Bonding of CAD/CAM Ceramic Crown Restorations. Polymers 2022, 14, 4541. [Google Scholar] [CrossRef]
- Sano, H.; Chowdhury, A.F.M.A.; Saikaew, P.; Matsumoto, M.; Hoshika, S.; Yamauti, M. The microtensile bond strength test: Its historical background and application to bond testing. Jpn. Dent. Sci. Rev. 2020, 56, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Van Meerbeek, B.; Peumans, M.; Poitevin, A.; Mine, A.; Van Ende, A.; Neves, A.; De Munck, J. Relationship between bond-strength tests and clinical outcomes. Dent. Mater. 2010, 26, e100–e121. [Google Scholar] [CrossRef]
- Griffith, A.A. The phenomena of rupture and flow in solids. Philos. Trans. R. Soc. Lond. Ser. A 1920, 221, 168–198. [Google Scholar]
- Armstrong, S.; Breschi, L.; Özcan, M.; Pfefferkorn, F.; Ferrari, M.; Van Meerbeek, B. Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent. Mater. 2017, 33, 133–143. [Google Scholar] [CrossRef]
- Gailani, H.F.A.; Benavides-Reyes, C.; Bolaños-Carmona, M.V.; Rosel-Gallardo, E.; González-Villafranca, P.; González-López, S. Effect of Two Immediate Dentin Sealing Approaches on Bond Strength of Lava™ CAD/CAM Indirect Restoration. Materials 2021, 14, 1629. [Google Scholar] [CrossRef]
- Magdy, N.; Rabah, A. Evaluation of micro-tensile bond strength of indirect resin composite inlay to dentin. Int. J. Health Sci. Res. 2017, 7, 105–115. [Google Scholar]
- Betamar, N.; Cardew, G.; van Noort, R. Influence of specimen designs on the microtensile bond strength to dentin. J. Adhes. Dent. 2007, 9, 159–168. [Google Scholar] [PubMed]
- De Munck, J.; Mine, A.; Poitevin, A.; Van Ende, A.; Cardoso, M.V.; Van Landuyt, K.L.; Peumans, M.; Van Meerbeek, B. Meta-analytical review of parameters involved in dentin bonding. J. Dent. Res. 2012, 91, 351–357. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Cury, A.H.; Cantoro, A.; Papacchini, F.; Tay, F.R.; Ferrari, M. Microtensile bond strength and interfacial properties of self-etching and self-adhesive resin cements used to lute composite onlays under different seating forces. J. Adhes. Dent. 2006, 8, 327–335. [Google Scholar] [PubMed]
- De Angelis, F.; Minnoni, A.; Vitalone, L.M.; Carluccio, F.; Vadini, M.; Paolantonio, M.; D’Arcangelo, C. Bond strength evaluation of three self-adhesive luting systems used for cementing composite and porcelain. Oper. Dent. 2011, 36, 626–634. [Google Scholar] [CrossRef]
- Meredith, N.; Sherriff, M.; Setchell, D.J.; Swanson, S.A. Measurement of the microhardness and young’s modulus of human enamel and dentine using an indentation technique. Arch. Oral Biol. 1996, 41, 539–545. [Google Scholar] [CrossRef]
- De Munck, J.; Vargas, M.; Van Landuyt, K.; Hikita, K.; Lambrechts, P.; Van Meerbeek, B. Bonding of an auto-adhesive luting material to enamel and dentin. Dent. Mater. 2004, 20, 963–971. [Google Scholar] [CrossRef]
- Gamal, R.; Gomaa, Y.; Abdellatif, M. Microtensile bond strength and scanning electron microscopic evaluation of zirconia bonded to dentin using two self-adhesive resin cements; effect of airborne abrasion and aging. Future Dent. J. 2017, 3, 55–60. [Google Scholar] [CrossRef]
- Scherrer, S.S.; Cesar, P.F.; Swain, M.V. Direct comparison of the bond strength results of the different test methods: A critical literature review. Dent. Mater. 2010, 26, 78–93. [Google Scholar] [CrossRef]
- Fuentes, M.V.; Escribano, N.; Baracco, B.; Romero, M.; Ceballos, L. Effect of indirect composite treatment micro effect of indirect composite treatment microtensile bond strength of self-adhesive resin cements. J. Clin. Exp. Dent. 2015, 8, e14. [Google Scholar]
- Roperto, R.; Akkus, A.; Akkus, O.; Lang, L.; Sousa-Neto, M.D.; Teich, S.; Porto, T.S. Effect of different adhesive strategies on microtensile bond strength of computer aided design/computer aided manufacturing blocks bonded to dentin. Dent. Res. J. 2016, 13, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Türkmen, C.; Durkan, M.; Öksüz, M. Shear Bond Strength of Indirect Composites Luted with Three New Self-Adhesive Resin Cements to Dentin. J. Adhes. 2009, 85, 919–931. [Google Scholar] [CrossRef]
- Rodrigues, R.F.; Ramos, C.M.; Francisconi, P.A.; Borges, A.F. The shear bond strength of self-adhesive resin cements to dentin and enamel: An in vitro study. J. Prosthet. Dent. 2015, 113, 220–227. [Google Scholar] [CrossRef]
- Ghodsi, S.; Shekarian, M.; Aghamohseni, M.M.; Rasaeipour, S.; Arzani, S. Resin cement selection for different types of fixed partial coverage restorations: A narrative systematic review. Clin. Exp. Dent. Res. 2023, 9, 1096–1111. [Google Scholar] [CrossRef] [PubMed]
- Tekçe, N.; Tuncer, S.; Demirci, M. The effect of sandblasting duration on the bond durability of dual-cure adhesive cement to CAD/CAM resin restoratives. J. Adv. Prosthodont. 2018, 10, 211–217. [Google Scholar] [CrossRef]
- Kim, B.K.; Bae, H.E.; Shim, J.S.; Lee, K.W. The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials. J. Prosthet. Dent. 2005, 94, 357–362. [Google Scholar] [CrossRef]
- Berkman, M.; Tuncer, S.; Tekçe, N.; Karabay, F.; Demirci, M. Microtensile bond strength between self-adhesive resin cements and resin based ceramic CAD/CAM block. Int. J. Dent. Sci. 2020, 23, 116–125. [Google Scholar] [CrossRef]
- Amaral, F.L.; Colucci, V.; Palma-Dibb, R.G.; Corona, S.A. Assessment of in vitro methods used to promote adhesive interface degradation: A critical review. J. Esthet. Restor. Dent. 2007, 19, 340–354. [Google Scholar] [CrossRef]
- Abo-Hamar, S.E.; Hiller, K.A.; Jung, H.; Federlin, M.; Friedl, K.H.; Schmalz, G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin. Oral Investig. 2005, 9, 161–167. [Google Scholar] [CrossRef]
| Material | Composition | Manufacturer |
|---|---|---|
| Signum ceramis | Monomer: 27 wt% multifunctional methacrylic acid esters, photo initiators, stabilizing agents, and inorganic pigments Filler: 73 wt% silicon dioxide and inorganic fillers | Heraeus Kulzer, Hanau, Germany |
| Cerasmart | Monomer: 29 wt% Bis-MEPP, UDMA, and DMA Filler: 71 wt% silica (20 nm) and barium glass (300 nm) | GC Europe, Leuven, Belgium |
| iCEM | Monomer: 51 wt% Di-, tri-, and multifunctional acrylates, initiators, and stabilizers Filler: 49 wt% filler | Heraeus Kulzer, Hanau, Germany |
| Silan IT | Ethanol (96%) and silane coupling agent (4%) | ITENA, Paris, France |
| Group | Non-Thermocycled Mean ± SD (MPa) | Thermocycled Mean ± SD (MPa) | Group | Non-Thermocycled Mean ± SD (MPa) | Thermocycled Mean ± SD (MPa) |
|---|---|---|---|---|---|
| C1/E | 12.22 ± 2.12 A, a | 8.53 ± 1.93 B, a | C1/D | 18.65 ± 3.98 A, a | 16.96 ± 3.66 A, a |
| C2/E | 14.58 ± 3.37 A, a | 10.60 ± 2.17 B, a | C2/D | 12.08 ± 2.53 A, b | 6.17 ± 1.28 B, b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Petrova, V.; Kirilova, J.; Yantcheva, S. An Assessment of the Micro-Tensile Bond Strength of Composites for Indirect Restoration to Enamel and Dentin. J. Funct. Biomater. 2025, 16, 138. https://doi.org/10.3390/jfb16040138
Petrova V, Kirilova J, Yantcheva S. An Assessment of the Micro-Tensile Bond Strength of Composites for Indirect Restoration to Enamel and Dentin. Journal of Functional Biomaterials. 2025; 16(4):138. https://doi.org/10.3390/jfb16040138
Chicago/Turabian StylePetrova, Viktoria, Janet Kirilova, and Sevda Yantcheva. 2025. "An Assessment of the Micro-Tensile Bond Strength of Composites for Indirect Restoration to Enamel and Dentin" Journal of Functional Biomaterials 16, no. 4: 138. https://doi.org/10.3390/jfb16040138
APA StylePetrova, V., Kirilova, J., & Yantcheva, S. (2025). An Assessment of the Micro-Tensile Bond Strength of Composites for Indirect Restoration to Enamel and Dentin. Journal of Functional Biomaterials, 16(4), 138. https://doi.org/10.3390/jfb16040138






