Accuracy of Dynamic Navigation vs. Freehand Endodontic Access Cavity Preparation in 3-Dimensionally Printed Teeth with Severe Pulp Canal Calcification
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
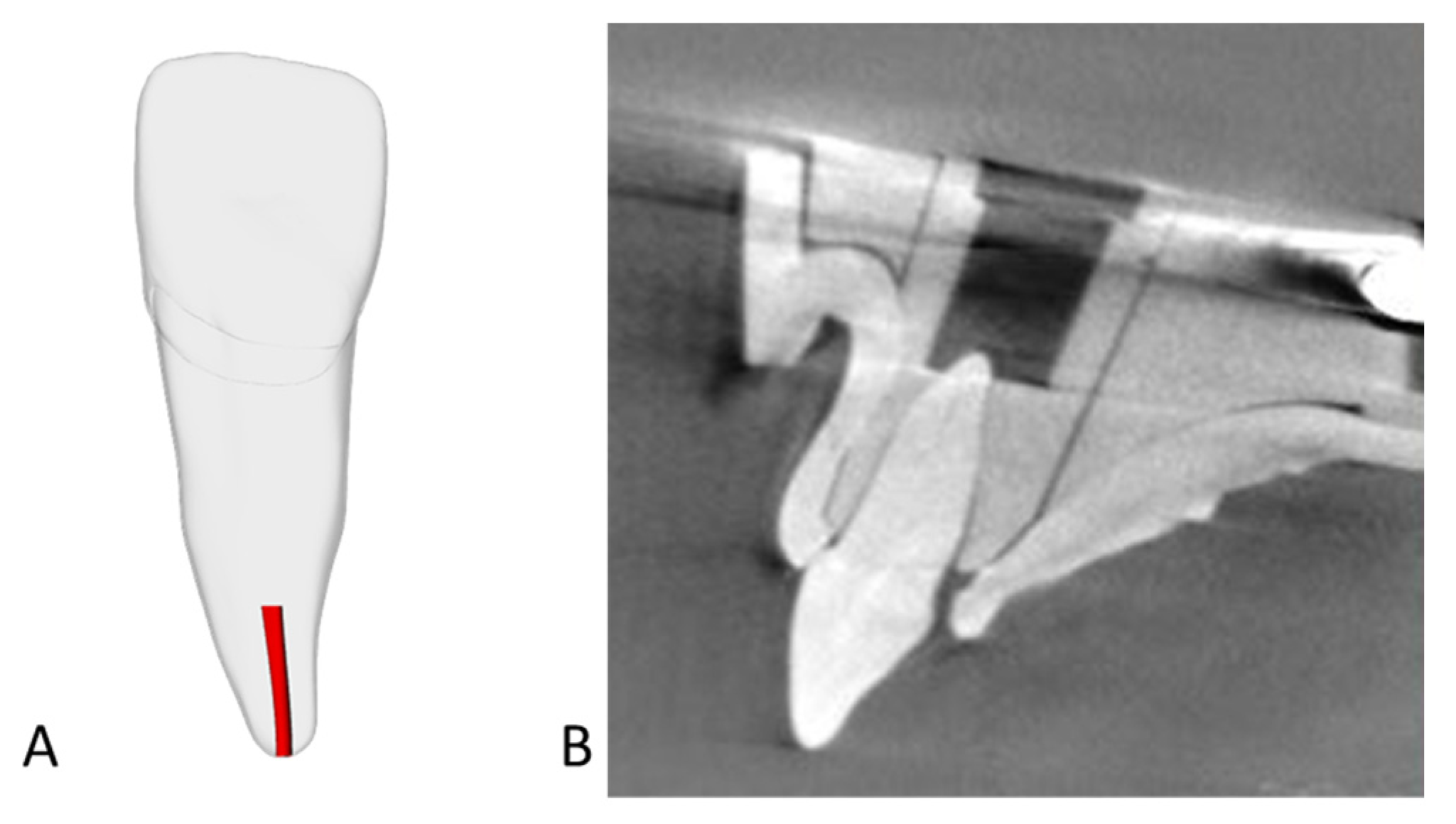
2.2. Teeth Selection
2.3. Planning
2.4. DN Access Cavity Preparation
2.5. FH Access Cavity Preparation
2.6. Accuracy Determination
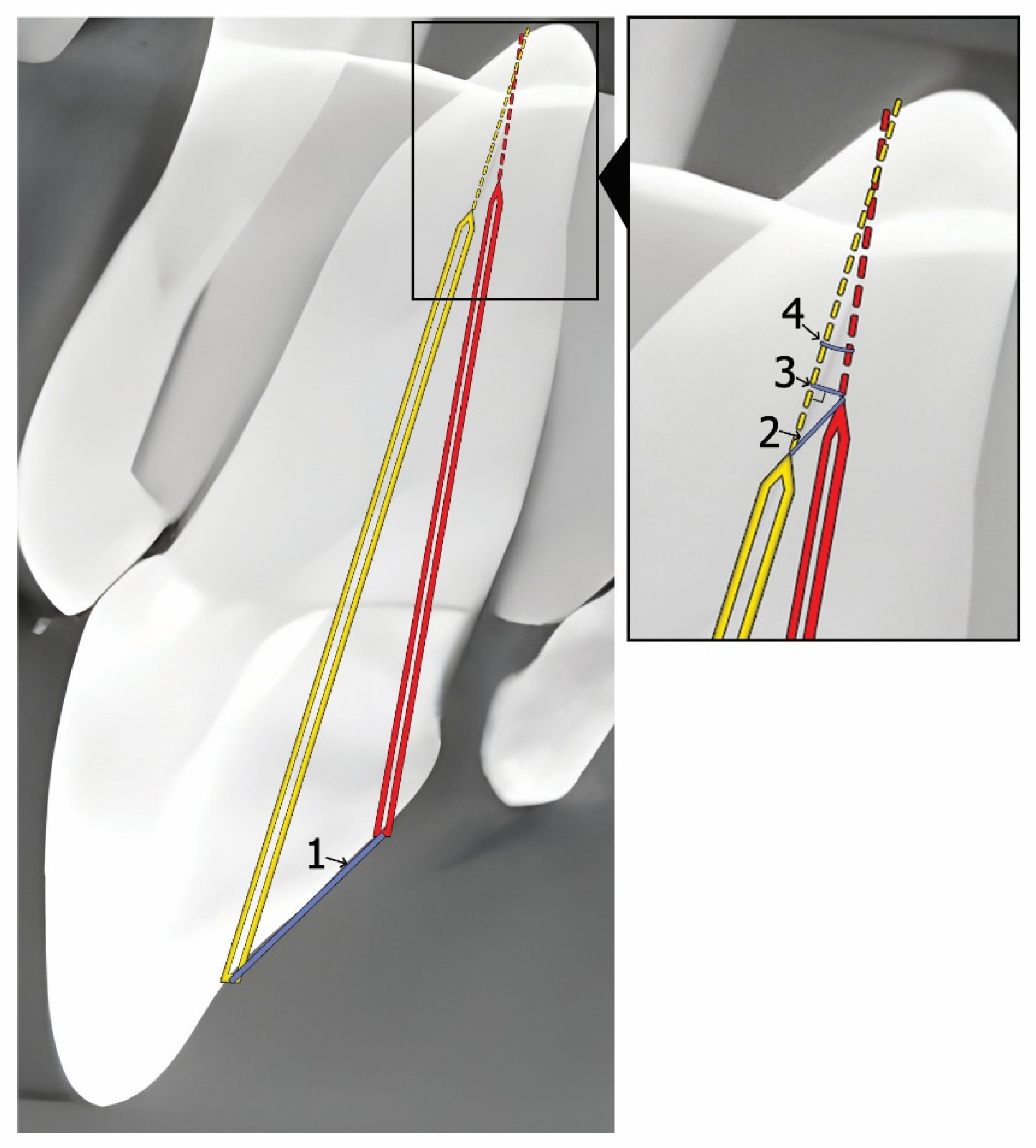
- Endodontic access entry point deviation (mm): the linear deviation at the coronal entry point.
- Apical point 3D deviation (mm): the total linear deviation at the apical endpoint.
- Apical point depth deviation (mm): the vertical deviation measured at the apical endpoint.
- Angular deflection (degrees): the maximal angular difference between the planned and actual cavity trajectory.
2.7. Statistical Analysis
3. Results
3.1. Agreement Between Measurements
3.2. Accuracy
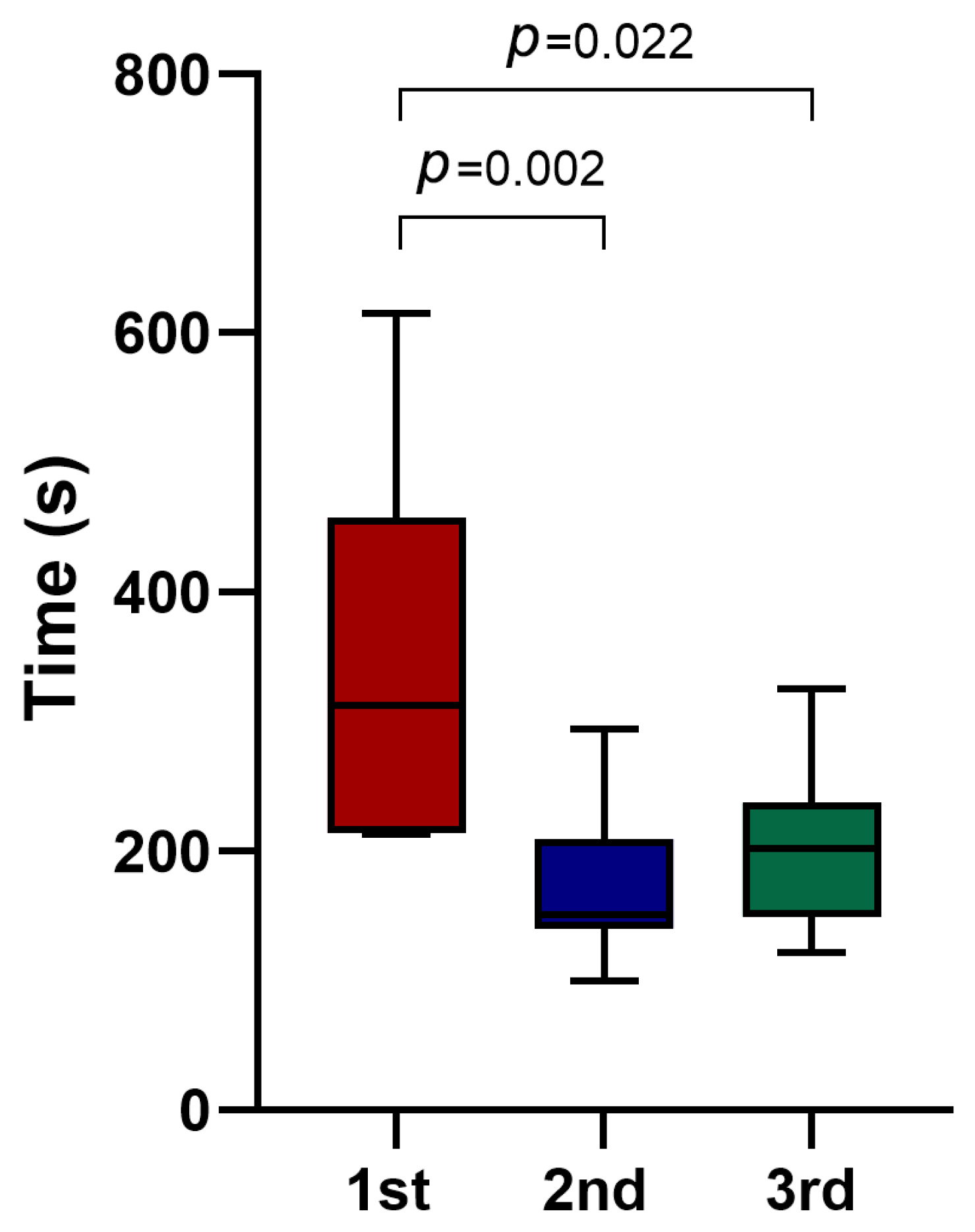
3.3. Procedural Time and Mishaps
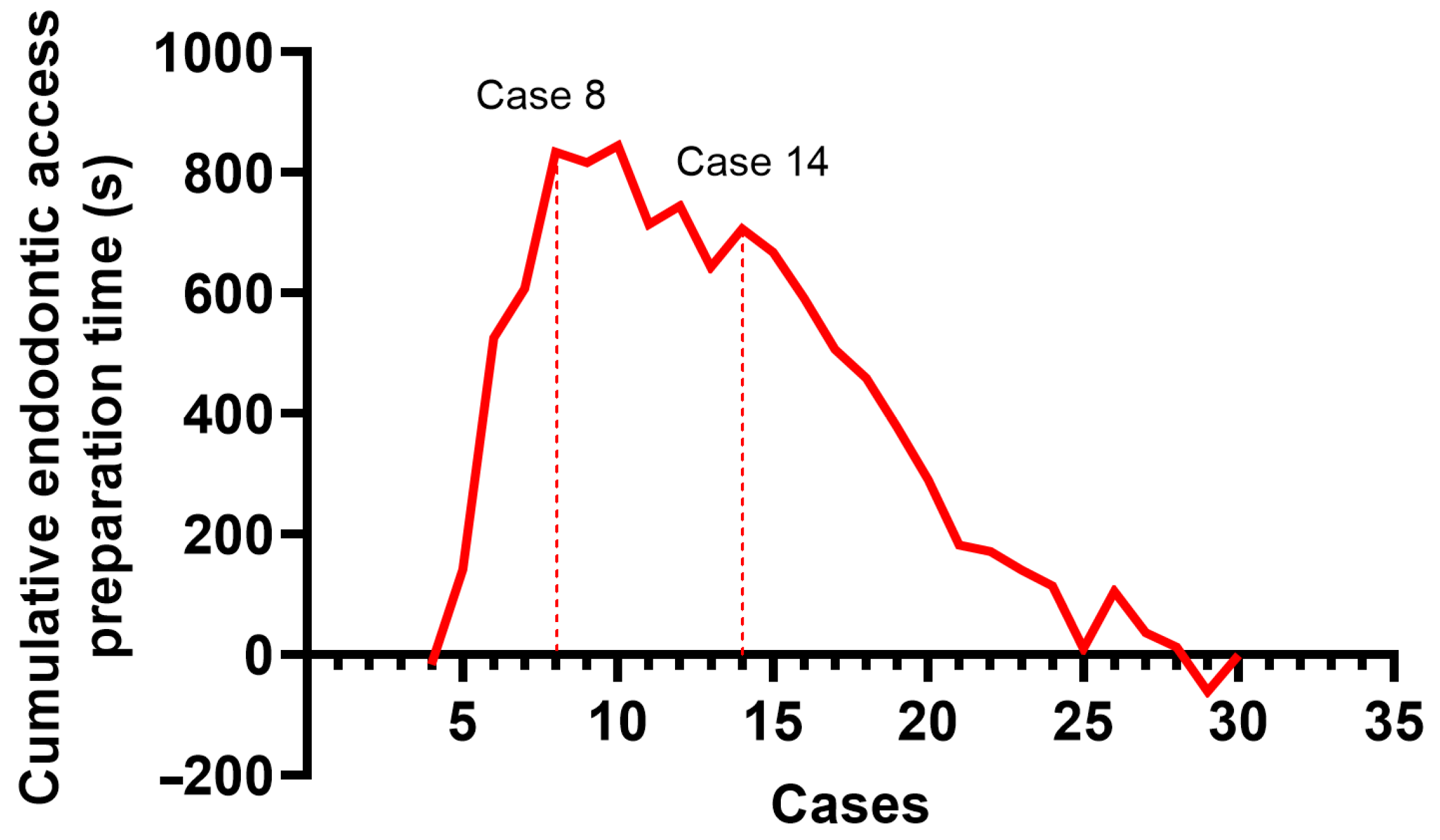
3.4. CUSUM Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| DN | Dynamic Navigation |
| FH | Freehanded |
| DOM | Dental Operating Microscope |
| ICC | Intraclass Correlation Coefficient |
| 3D | Three-dimensionally |
| PCC | Pulp Canal Calcification |
| SN | Static Navigation |
References
- McCabe, P.S.; Dummer, P.M.H. Pulp canal obliteration: An endodontic diagnosis and treatment challenge. Int. Endod. J. 2012, 45, 177–197. [Google Scholar] [CrossRef] [PubMed]
- Fleig, S.; Attin, T.; Jungbluth, H. Narrowing of the radicular pulp space in coronally restored teeth. Clin. Oral. Investig. 2017, 21, 1251–1257. [Google Scholar] [CrossRef]
- Kiefner, P.; Connert, T.; ElAyouti, A.; Weiger, R. Treatment of calcified root canals in elderly people: A clinical study about the accessibility, the time needed and the outcome with a three-year follow-up. Gerodontology 2017, 34, 164–170. [Google Scholar] [CrossRef]
- Näsström, K.; Forsberg, B.; Petersson, A.; Westesson, P.L. Narrowing of the dental pulp chamber in patients with renal diseases. Oral Surg. Oral Med. Oral Pathol. 1985, 59, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Pettiette, M.T.; Zhong, S.; Moretti, A.J.; Khan, A.A. Potential correlation between statins and pulp chamber calcification. J. Endod. 2013, 39, 1119–1123. [Google Scholar] [CrossRef]
- Jiang, X.; Dai, Y.; Liu, H. Evaluation of the characteristics of root canal calcification after regenerative endodontic procedures: A retrospective cohort study over 3 years. Int. J. Paediatr. Dent. 2023, 33, 305–313. [Google Scholar] [CrossRef]
- European Society of Endodontology (ESE); Krastl, G.; Weiger, R.; Filippi, A.; Van Waes, H.; Ebeleseder, K.; Ree, M.; Connert, T.; Widbiller, M.; Tjäderhane, L. European Society of Endodontology position statement: Endodontic management of traumatized permanent teeth. Int. Endod. J. 2021, 54, 1473–1481. [Google Scholar] [CrossRef] [PubMed]
- Oginni, A.O.; Adekoya-Sofowora, C.A.; Kolawole, K.A. Evaluation of radiographs, clinical signs and symptoms associated with pulp canal obliteration: An aid to treatment decision. Dent. Traumatol. 2009, 25, 620–625. [Google Scholar] [CrossRef]
- Karabucak, B.; Bunes, A.; Chehoud, C.; Kohli, M.R.; Setzer, F. Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: A cone-beam computed tomography study. J. Endod. 2016, 42, 538–541. [Google Scholar] [CrossRef]
- Touré, B.; Faye, B.; Kane, A.W.; Lo, C.M.; Niang, B.; Boucher, Y. Analysis of reasons for extraction of endodontically treated teeth: A prospective study. J. Endod. 2011, 37, 1512–1515. [Google Scholar] [CrossRef]
- Selden, H.S. The role of a dental operating microscope in improved nonsurgical treatment of “calcified” canals. Oral. Surg. Oral. Med. Oral. Pathol. 1989, 68, 93–98. [Google Scholar] [CrossRef]
- Patel, S.; Rhodes, J. A practical guide to endodontic access cavity preparation in molar teeth. Br. Dent. J. 2007, 203, 133–140. [Google Scholar] [CrossRef]
- Khabbaz, M.G.; Serefoglou, M.H. The application of the buccal object rule for the determination of calcified root canals. Int. Endod. J. 1996, 29, 284–287. [Google Scholar] [CrossRef]
- Zehnder, M.S.; Connert, T.; Weiger, R.; Krastl, G.; Kühl, S. Guided endodontics: Accuracy of a novel method for guided access cavity preparation and root canal location. Int. Endod. J. 2016, 49, 966–972. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.D.; Carrico, C.K.; Bermanis, I. 3-Dimensional Accuracy of Dynamic Navigation Technology in Locating Calcified Canals. J. Endod. 2020, 46, 839–845. [Google Scholar] [CrossRef] [PubMed]
- Dianat, O.; Nosrat, A.; Tordik, P.A.; Aldahmash, S.A.; Romberg, E.; Price, J.B.; Mostoufi, B. Accuracy and Efficiency of a Dynamic Navigation System for Locating Calcified Canals. J. Endod. 2020, 46, 1719–1725. [Google Scholar] [CrossRef]
- Jain, S.D.; Saunders, M.W.; Carrico, C.K.; Jadhav, A.; Deeb, J.G.; Myers, G.L. Dynamically Navigated versus Freehand Access Cavity Preparation: A Comparative Study on Substance Loss Using Simulated Calcified Canals. J. Endod. 2020, 46, 1745–1751. [Google Scholar] [CrossRef]
- Torres, A.; Dierickx, M.; Lerut, K.; Bleyen, S.; Shaheen, E.; Coucke, W.; Pedano, M.S.; Lambrechts, P.; Jacobs, R. Clinical outcome of guided endodontics versus freehand drilling: A controlled clinical trial, single arm with external control group. Int. Endod. J. 2024, 58, 209–224. [Google Scholar] [CrossRef] [PubMed]
- Jonaityte, E.M.; Bilvinaite, G.; Drukteinis, S.; Torres, A. Accuracy of Dynamic Navigation for Non-Surgical Endodontic Treatment: A Systematic Review. J. Clin. Med. 2022, 11, 3441. [Google Scholar] [CrossRef]
- Panithini, D.B.; Sajjan, G.S.; Kinariwala, N.; Medicharla, U.D.; Varma, K.M.; Kallepalli, M. Real-time guided endodontics: A case report of maxillary central incisor with calcific metamorphosis. J. Conserv. Dent. 2022, 26, 113. [Google Scholar] [CrossRef]
- Yang, X.; Zhang, Y.; Chen, X.; Huang, L.; Qiu, X. Limitations and Management of Dynamic Navigation System for Locating Calcified Canals Failure. J. Endod. 2024, 50, 96–105. [Google Scholar] [CrossRef]
- Xue, P.; Luo, Q.; Huang, Y.; Xu, M.; Qiu, L.; Wang, J.; He, H.; Chen, F. Retreatment and aesthetic restoration of maxillary incisor with calcified root canal using a dynamic navigation system: A case report. BMC Oral. Health 2024, 24, 1358. [Google Scholar] [CrossRef]
- Wu, M.; Liu, M.; Cheng, Y.; Tang, W.; Yan, P.; Jiang, H. Treatment of Pulp Canal Obliteration Using a Dynamic Navigation System: Two Case Reports. J. Endod. 2022, 48, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Villa-Machado, P.A.; Restrepo-Restrepo, F.A.; Sousa-Dias, H.; Tobón-Arroyave, S.I. Application of computer-assisted dynamic navigation in complex root canal treatments: Report of two cases of calcified canals. Aust. Endod. J. 2022, 48, 187–196. [Google Scholar] [CrossRef]
- DRSK Group AB [Internet]. Available online: https://drsk.com/product/2111-1b7-rwh/ (accessed on 23 September 2025).
- Torres, A.; Boelen, G.J.; Lambrechts, P.; Pedano, M.S.; Jacobs, R. Dynamic navigation: A laboratory study on the accuracy and potential use of guided root canal treatment. Int. Endod. J. 2021, 54, 1659–1667. [Google Scholar] [CrossRef]
- Huth, K.C.; Borkowski, L.; Liebermann, A.; Berlinghoff, F.; Hickel, R.; Schwendicke, F.; Reymus, M. Comparing accuracy in guided endodontics: Dynamic real-time navigation, static guides, and manual approaches for access cavity preparation—An in vitro study using 3D printed teeth. Clin. Oral. Investig. 2024, 28, 212. [Google Scholar] [CrossRef]
- Sharma, S.; Haldar, P.; Kumar, V.; Chawla, A.; Logani, A. Learning Curve for Dynamic Navigation Procedure during Endodontic Management of Permanent Maxillary Anterior Teeth with Pulp Canal Calcification: A Risk-Adjusted Cumulative Summation Analysis of a Single Operator’s Experience. J. Endod. 2025, 51, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Dianat, O.; Gupta, S.; Price, J.B.; Mostoufi, B. Guided Endodontic Access in a Maxillary Molar Using a Dynamic Navigation System. J. Endod. 2021, 47, 658–662. [Google Scholar] [CrossRef]
- Jorba-García, A.; González-Barnadas, A.; Camps-Font, O.; Figueiredo, R.; Valmaseda-Castellón, E. Accuracy assessment of dynamic computer–aided implant placement: A systematic review and meta-analysis. Clin. Oral. Investig. 2021, 25, 2479–2494. [Google Scholar] [CrossRef] [PubMed]
- Franco, C.G.; Deglow, E.R.; Montero, J.; Sans, F.A.; Nagendrababu, V.; Dummer, P.M.; Galindo, A.B.L.; Zubizarreta-Macho, Á. Endodontic access with different computer navigation systems in calcified root canals. J. Am. Dent. Assoc. 2024, 155, 1043–1052. [Google Scholar] [CrossRef]
- Zubizarreta-Macho, Á.; Muñoz Ade, P.; Deglow, E.R.; Agustín-Panadero, R.; Álvarez, J.M. Accuracy of Computer-Aided Dynamic Navigation Compared to Computer-Aided Static Procedure for Endodontic Access Cavities: An in Vitro Study. J. Clin. Med. 2020, 9, 129. [Google Scholar] [CrossRef] [PubMed]
- Hildebrand, H.; Krug, R.; Leontiev, W.; Dagassan-Berndt, D.; Krastl, G.; Weiger, R.; Connert, T. Real-time guided endodontics versus conventional freehand access cavity preparation by a specialist– an ex vivo comparative study. Clin. Oral. Investig. 2025, 29, 232. [Google Scholar] [CrossRef] [PubMed]
- Yan, Q.; Wu, X.; Shi, J.; Shi, B. Does dynamic navigation assisted student training improve the accuracy of dental implant placement by postgraduate dental students: An in vitro study. BMC Oral. Health 2024, 24, 600. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Wang, M.; Cheng, X.; Li, Y.; Shi, X.; Liu, F. Evaluation of a dynamic navigation system for training students in dental implant placement. J. Dent. Educ. 2021, 85, 120–127. [Google Scholar] [CrossRef]

| Accuracy Measurements | DN Group | FH Group | p Value |
|---|---|---|---|
| Entry point deviation, mm | 0.60 (0.38–1.06) | 0.55 (0.36–0.79) | 0.395 |
| Apical point 3D deviation, mm | 1.25 (0.71–1.49) | 1.96 (1.43–2.21) | 0.001 |
| Apical point depth deviation, mm | 0.43 (0.22–0.62) | 0.88 (0.54–1.46) | <0.001 |
| Angular deflection, degrees | 1.93 (1.49–3.54) | 5.71 (3.67–8.16) | <0.001 |
| Efficiency Measurements | DN Group | FH Group | p Value |
|---|---|---|---|
| Median time, s | 204 (148–291) | 108.5 (96.25–127) | <0.001 |
| Mean time, s | 230.3 ± 114.92 | 110 ± 23.48 | <0.001 |
| Minimum time, s | 100 | 63 | N/A |
| Maximum time, s | 615 | 160 | N/A |
| Perforation, n (%) | 3 (10.0) | 9 (30.0) | 0.053 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urbone, E.M.; Tusas, P.; Gendviliene, I.; Rutkunas, V.; Drukteinis, S. Accuracy of Dynamic Navigation vs. Freehand Endodontic Access Cavity Preparation in 3-Dimensionally Printed Teeth with Severe Pulp Canal Calcification. J. Funct. Biomater. 2025, 16, 376. https://doi.org/10.3390/jfb16100376
Urbone EM, Tusas P, Gendviliene I, Rutkunas V, Drukteinis S. Accuracy of Dynamic Navigation vs. Freehand Endodontic Access Cavity Preparation in 3-Dimensionally Printed Teeth with Severe Pulp Canal Calcification. Journal of Functional Biomaterials. 2025; 16(10):376. https://doi.org/10.3390/jfb16100376
Chicago/Turabian StyleUrbone, Egle Marija, Paulius Tusas, Ieva Gendviliene, Vygandas Rutkunas, and Saulius Drukteinis. 2025. "Accuracy of Dynamic Navigation vs. Freehand Endodontic Access Cavity Preparation in 3-Dimensionally Printed Teeth with Severe Pulp Canal Calcification" Journal of Functional Biomaterials 16, no. 10: 376. https://doi.org/10.3390/jfb16100376
APA StyleUrbone, E. M., Tusas, P., Gendviliene, I., Rutkunas, V., & Drukteinis, S. (2025). Accuracy of Dynamic Navigation vs. Freehand Endodontic Access Cavity Preparation in 3-Dimensionally Printed Teeth with Severe Pulp Canal Calcification. Journal of Functional Biomaterials, 16(10), 376. https://doi.org/10.3390/jfb16100376








