Surface Modification Strategies for Chrysin-Loaded Iron Oxide Nanoparticles to Boost Their Anti-Tumor Efficacy in Human Colon Carcinoma Cells
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of PEG and Chitosan-Coated Nanoparticles
2.2.2. Characterization of Coated and Drug-Loaded Magnetite Nanoparticles
2.2.3. Calculation of Drug-Loading Efficiency (LE)
2.2.4. Cell Culture and MTT Assay
2.2.5. Apoptosis Assay
2.2.6. Statistical Analysis
2.2.7. Declaration of Generative AI in Writing This Manuscript
3. Results
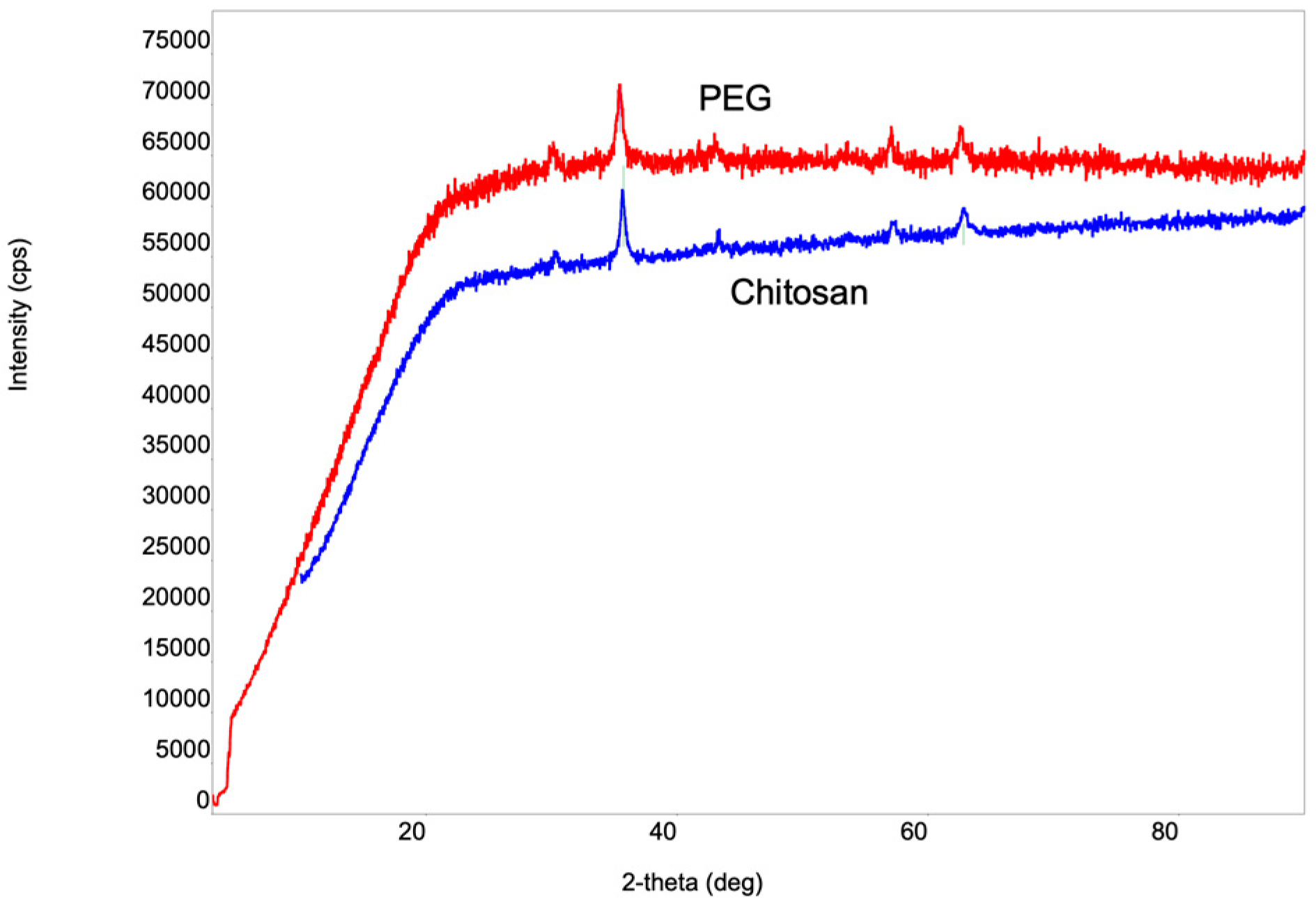
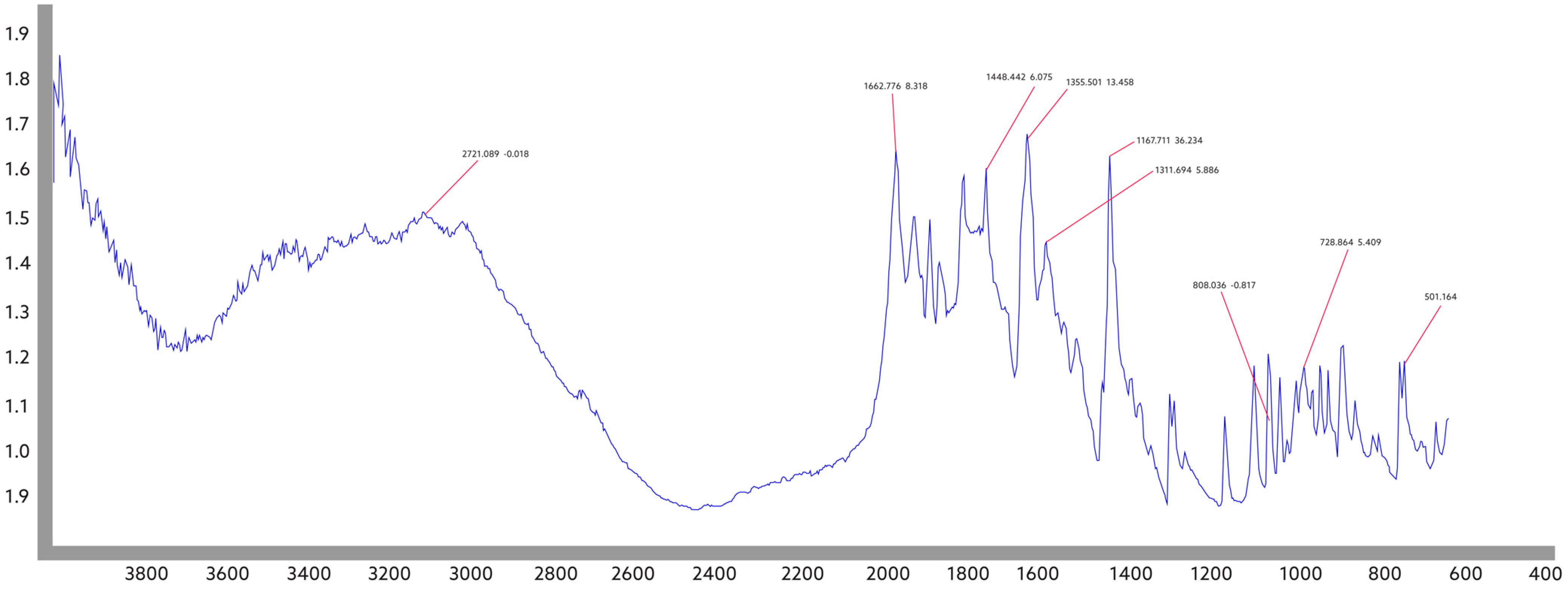
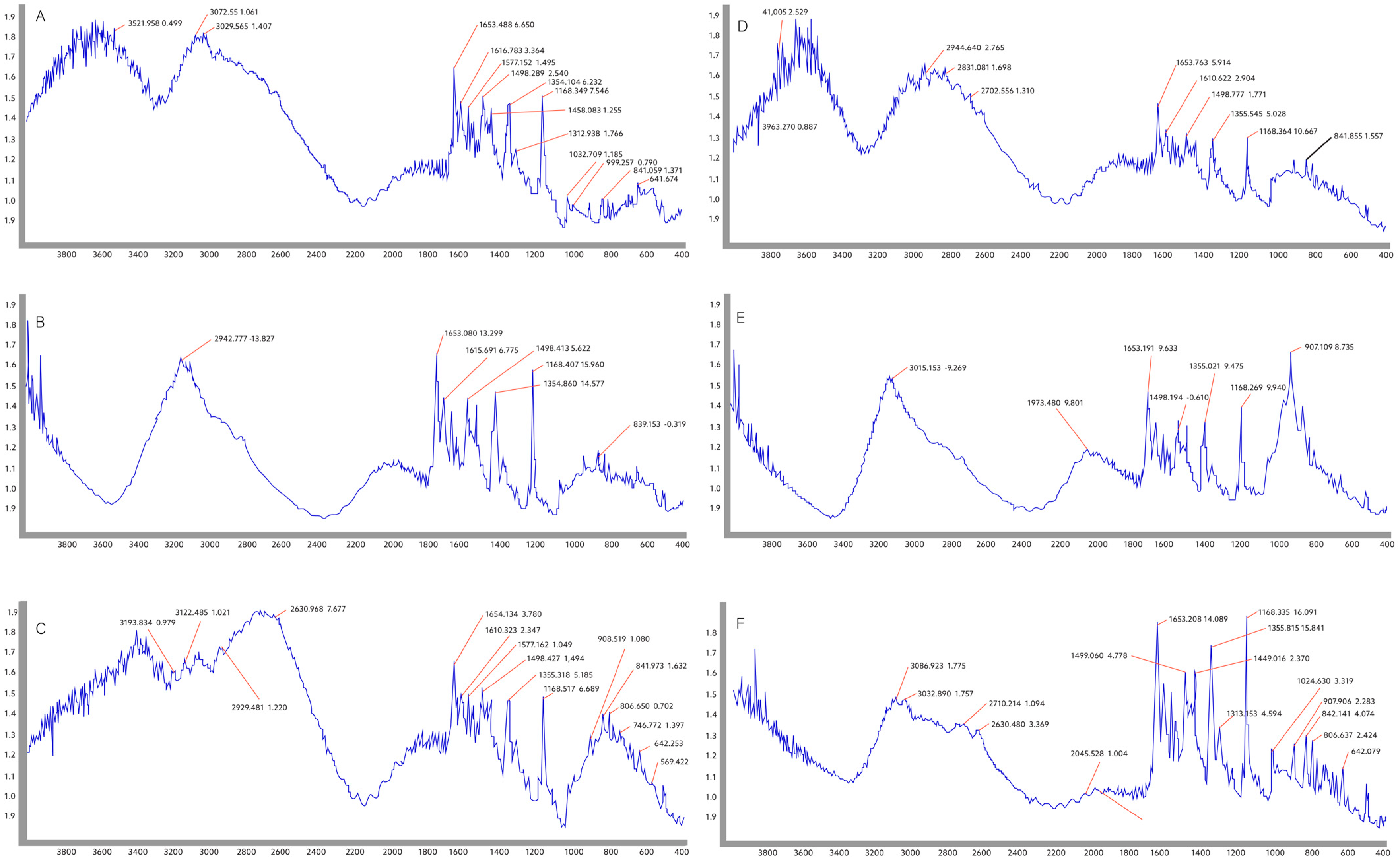
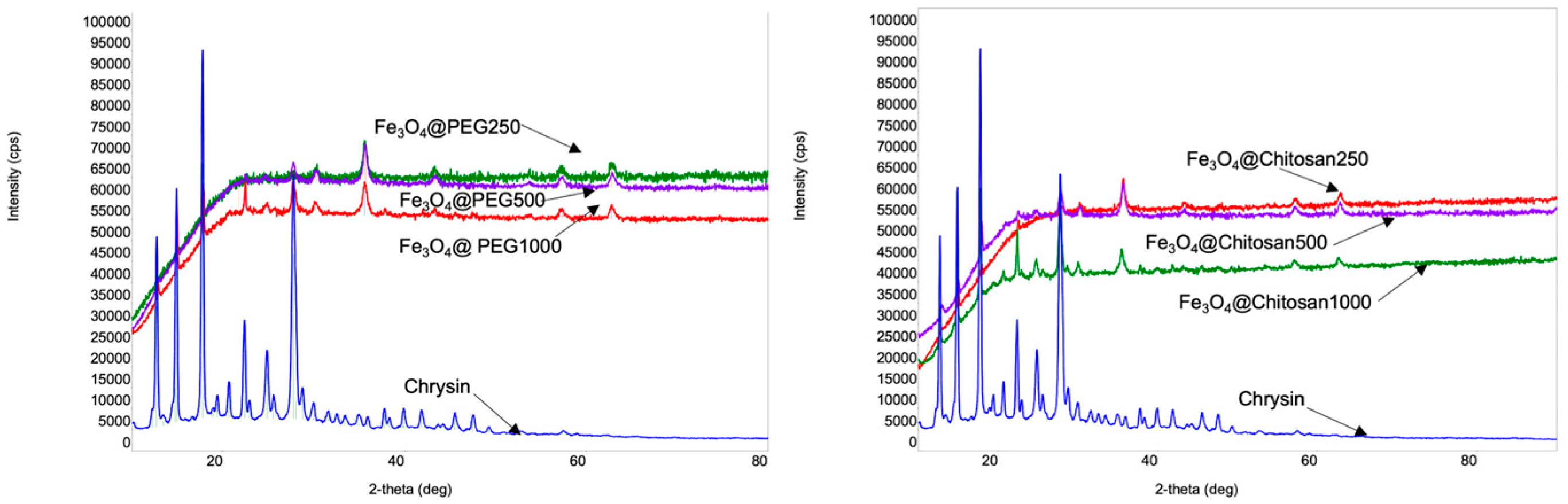
3.1. Characterization and Structural Properties
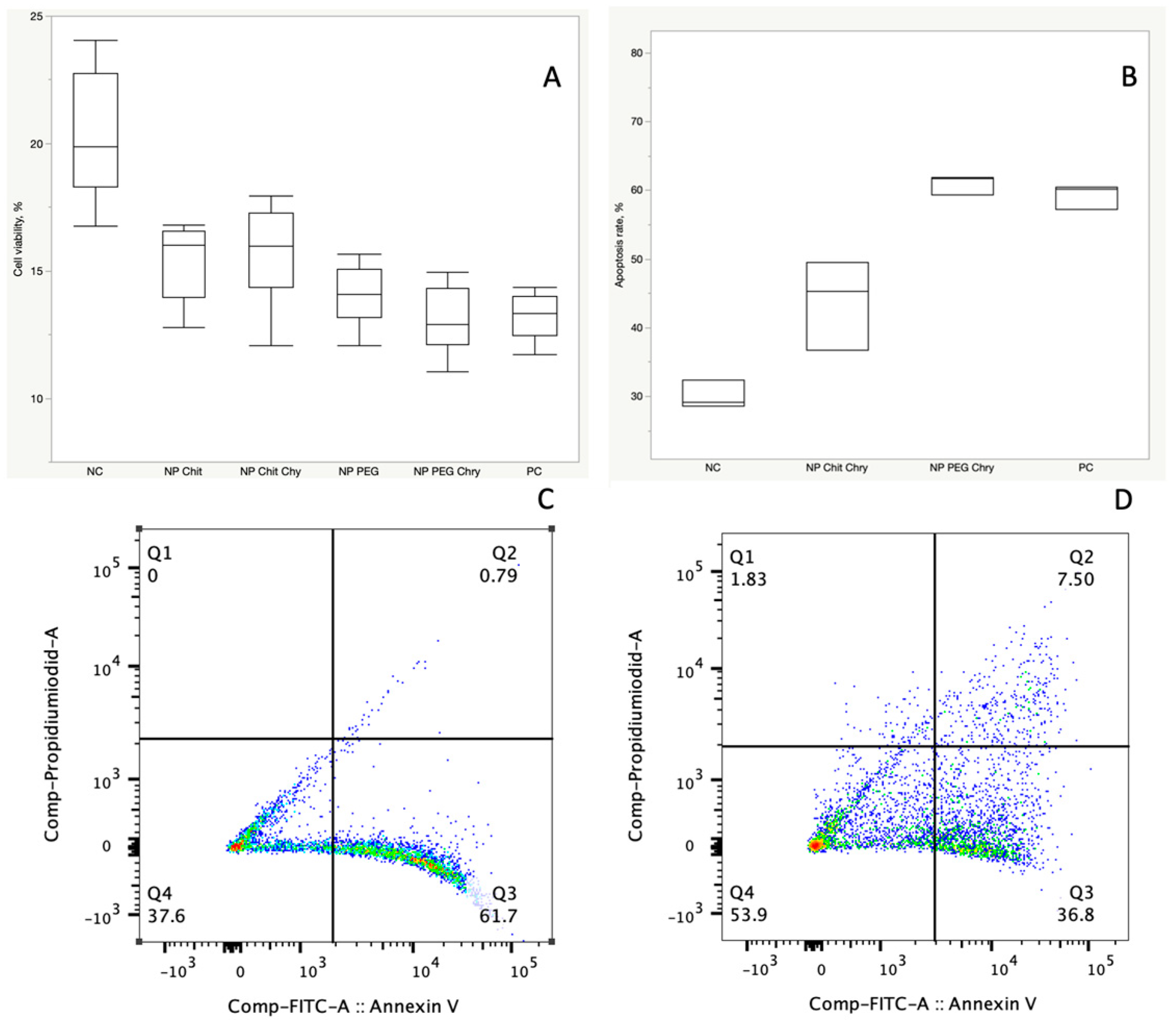
3.2. In-Vitro Cytotoxicity Analysis and Apoptosis Assay
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yao, Y.; Zhou, Y.; Liu, L.; Xu, Y.; Chen, Q.; Wang, Y.; Wu, S.; Deng, Y.; Zhang, J.; Shao, A. Nanoparticle-based drug delivery in cancer therapy and its role in overcoming drug resistance. Front. Mol. Biosci. 2020, 7, 193. [Google Scholar] [CrossRef]
- Yagublu, V.; Karimova, A.; Hajibabazadeh, J.; Reissfelder, C.; Muradov, M.; Bellucci, S.; Allahverdiyev, A. Overview of physicochemical properties of nanoparticles as drug carriers for targeted cancer therapy. J. Funct. Biomater. 2022, 13, 196. [Google Scholar] [CrossRef]
- Guo, X.; Wei, X.; Chen, Z.; Zhang, X.; Yang, G.; Zhou, S. Multifunctional nanoplatforms for subcellular delivery of drugs in cancer therapy. Prog. Mater. Sci. 2020, 107, 100599. [Google Scholar] [CrossRef]
- Ulbrich, K.; Hola, K.; Subr, V.; Bakandritsos, A.; Tucek, J.; Zboril, R. Targeted drug delivery with polymers and magnetic nanoparticles: Covalent and noncovalent approaches, release control, and clinical studies. Chem. Rev. 2016, 116, 5338–5431. [Google Scholar] [CrossRef] [PubMed]
- Ramazanov, M.; Karimova, A.; Shirinova, H. Magnetism for drug delivery, MRI and hyperthermia applications: A review. Biointerface Res. Appl. Chem 2021, 11, 8654–8668. [Google Scholar]
- Włodarczyk, A.; Gorgoń, S.; Radoń, A.; Bajdak-Rusinek, K. Magnetite nanoparticles in magnetic hyperthermia and cancer therapies: Challenges and perspectives. Nanomaterials 2022, 12, 1807. [Google Scholar] [CrossRef] [PubMed]
- Thapa, R.K.; Kim, J.O. Nanomedicine-based commercial formulations: Current developments and future prospects. J. Pharm. Investig. 2023, 53, 19–33. [Google Scholar] [CrossRef] [PubMed]
- Jordan, F.; Naylor, A.; Kelly, C.; Howdle, S.; Lewis, A.; Illum, L. Sustained release hGH microsphere formulation produced by a novel supercritical fluid technology: In vivo studies. J. Control. Release 2010, 141, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Zhou, Z.; Mao, H.; Yang, L. Magnetic nanoparticles for precision oncology: Theranostic magnetic iron oxide nanoparticles for image-guided and targeted cancer therapy. Nanomedicine 2017, 12, 73–87. [Google Scholar] [CrossRef]
- Chrishtop, V.V.; Mironov, V.A.; Prilepskii, A.Y.; Nikonorova, V.G.; Vinogradov, V.V. Organ-specific toxicity of magnetic iron oxide-based nanoparticles. Nanotoxicology 2021, 15, 167–204. [Google Scholar] [CrossRef]
- Malhotra, N.; Lee, J.-S.; Liman, R.A.D.; Ruallo, J.M.S.; Villaflores, O.B.; Ger, T.-R.; Hsiao, C.-D. Potential toxicity of iron oxide magnetic nanoparticles: A review. Molecules 2020, 25, 3159. [Google Scholar] [CrossRef]
- Gong, D.; Celi, N.; Zhang, D.; Cai, J. Magnetic biohybrid microrobot multimers based on chlorella cells for enhanced targeted drug delivery. ACS Appl. Mater. Interfaces 2022, 14, 6320–6330. [Google Scholar] [CrossRef]
- Chrastina, A.; Massey, K.A.; Schnitzer, J.E. Overcoming in vivo barriers to targeted nanodelivery. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2011, 3, 421–437. [Google Scholar] [CrossRef]
- Abbasi, R.; Shineh, G.; Mobaraki, M.; Doughty, S.; Tayebi, L. Structural parameters of nanoparticles affecting their toxicity for biomedical applications: A review. J. Nanoparticle Res. 2023, 25, 43. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.C.; Smith, J.B.; Pham, T.; Whitaker, R.D.; Sucato, C.A.; Hamilton, J.A.; Bartolak-Suki, E.; Wong, J.Y. Effect of PEG molecular weight on stability, T2 contrast, cytotoxicity, and cellular uptake of superparamagnetic iron oxide nanoparticles (SPIONs). Colloids Surf. B Biointerfaces 2014, 119, 106–114. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, S.; Mutalik, S.; Rai, S.; Udupa, N.; Rao, B.S.S. PEGylation of superparamagnetic iron oxide nanoparticle for drug delivery applications with decreased toxicity: An in vivo study. J. Nanoparticle Res. 2015, 17, 412. [Google Scholar] [CrossRef]
- Dadfar, S.M.; Roemhild, K.; Drude, N.I.; von Stillfried, S.; Knüchel, R.; Kiessling, F.; Lammers, T. Iron oxide nanoparticles: Diagnostic, therapeutic and theranostic applications. Adv. Drug Deliv. Rev. 2019, 138, 302–325. [Google Scholar] [CrossRef]
- Szekeres, M.; Tóth, I.Y.; Illés, E.; Hajdú, A.; Zupkó, I.; Farkas, K.; Oszlánczi, G.; Tiszlavicz, L.; Tombácz, E. Chemical and colloidal stability of carboxylated core-shell magnetite nanoparticles designed for biomedical applications. Int. J. Mol. Sci. 2013, 14, 14550–14574. [Google Scholar] [CrossRef]
- Friedrich, B.; Auger, J.-P.; Dutz, S.; Cicha, I.; Schreiber, E.; Band, J.; Boccacccini, A.R.; Krönke, G.; Alexiou, C.; Tietze, R. Hydroxyapatite-coated SPIONs and their influence on cytokine release. Int. J. Mol. Sci. 2021, 22, 4143. [Google Scholar] [CrossRef]
- Tóth, I.Y.; Illés, E.; Szekeres, M.; Zupkó, I.; Turcu, R.; Tombácz, E. Chondroitin-Sulfate-A-Coated Magnetite Nanoparticles: Synthesis, Characterization and Testing to Predict Their Colloidal Behavior in Biological Milieu. Int. J. Mol. Sci. 2019, 20, 4096. [Google Scholar] [CrossRef]
- Giraldo-Villegas, M.; Urquijo, J.; Arnache-Olmos, O.L.; Rojas-López, M. Polyacrylic acid-coated iron oxide nanoparticles could be a useful tool for tracking inflammatory monocytes. Future Sci. OA 2019, 5, FSO423. [Google Scholar] [CrossRef]
- Schubert, J.; Chanana, M. Coating matters: Review on colloidal stability of nanoparticles with biocompatible coatings in biological media, living cells and organisms. Curr. Med. Chem. 2018, 25, 4553–4586. [Google Scholar] [CrossRef]
- Thunemann, A.; Schutt, D.; Kaufner, L.; Pison, U.; Mohwald, H. Maghemite nanoparticles protectively coated with poly (ethylene imine) and poly (ethylene oxide)-block-poly (glutamic acid). Langmuir 2006, 22, 2351–2357. [Google Scholar] [CrossRef]
- McBain, S.C.; Yiu, H.H.; Dobson, J. Magnetic nanoparticles for gene and drug delivery. Int. J. Nanomed. 2008, 3, 169–180. [Google Scholar]
- Nathanael, A.J.; Oh, T.H. Biopolymer coatings for biomedical applications. Polymers 2020, 12, 3061. [Google Scholar] [CrossRef]
- Chang, B.; Sha, X.; Guo, J.; Jiao, Y.; Wang, C.; Yang, W. Thermo and pH dual responsive, polymer shell coated, magnetic mesoporous silica nanoparticles for controlled drug release. J. Mater. Chem. 2011, 21, 9239–9247. [Google Scholar] [CrossRef]
- Langer, R. Drug delivery and targeting. Nature 1998, 392, 5–10. [Google Scholar]
- Cao, J.; Guenther, R.H.; Sit, T.L.; Opperman, C.H.; Lommel, S.A.; Willoughby, J.A. Loading and release mechanism of red clover necrotic mosaic virus derived plant viral nanoparticles for drug delivery of doxorubicin. Small 2014, 10, 5126–5136. [Google Scholar] [CrossRef] [PubMed]
- Wu, W. nanoparticles: Synthesis, surface functional strategies and biomedical applications Recent progress on magnetic iron oxide nanoparticles: Synthesis, surface functional strategies and biomedical applications. Sci. Technol. Adv. Mater. IOP Publ. 2015, 16, 23501. [Google Scholar] [CrossRef] [PubMed]
- Xu, H.; Cheng, L.; Wang, C.; Ma, X.; Li, Y.; Liu, Z. Polymer encapsulated upconversion nanoparticle/iron oxide nanocomposites for multimodal imaging and magnetic targeted drug delivery. Biomaterials 2011, 32, 9364–9373. [Google Scholar] [CrossRef] [PubMed]
- Talebi, M.; Talebi, M.; Farkhondeh, T.; Simal-Gandara, J.; Kopustinskiene, D.M.; Bernatoniene, J.; Samarghandian, S. Emerging cellular and molecular mechanisms underlying anticancer indications of chrysin. Cancer Cell Int. 2021, 21, 214. [Google Scholar] [CrossRef] [PubMed]
- Petcharoen, K.; Sirivat, A. Synthesis and characterization of magnetite nanoparticles via the chemical co-precipitation method. Mater. Sci. Eng. B 2012, 177, 421–427. [Google Scholar] [CrossRef]
- Singh, R.; Lillard Jr, J.W. Nanoparticle-based targeted drug delivery. Exp. Mol. Pathol. 2009, 86, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Devi, S.V.; Prakash, T. Kinetics of cisplatin release by in-vitro using poly (D, L-Lactide) coated Fe3O4 Nanocarriers. IEEE Trans. NanoBioscience 2013, 12, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Wallyn, J.; Anton, N.; Vandamme, T.F. Synthesis, principles, and properties of magnetite nanoparticles for in vivo imaging applications—A review. Pharmaceutics 2019, 11, 601. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Cabanas, M.; López-García, M.; Barriada, J.L.; Herrero, R.; de Vicente, M.E.S. Green synthesis of iron oxide nanoparticles. Development of magnetic hybrid materials for efficient As (V) removal. Chem. Eng. J. 2016, 301, 83–91. [Google Scholar] [CrossRef]
- Antarnusa, G.; Suharyadi, E. A synthesis of polyethylene glycol (PEG)-coated magnetite Fe3O4 nanoparticles and their characteristics for enhancement of biosensor. Mater. Res. Express 2020, 7, 056103. [Google Scholar] [CrossRef]
- Sundararajan, M.; Thomas, P.A.; Venkadeswaran, K.; Jeganathan, K.; Geraldine, P. Synthesis and characterization of chrysin-loaded β-cyclodextrin-based nanosponges to enhance in-vitro solubility, photostability, drug release, antioxidant effects and antitumorous efficacy. J. Nanosci. Nanotechnol. 2017, 17, 8742–8751. [Google Scholar] [CrossRef]
- Gupta, N.; Rajera, R.; Nagpal, M.; Arora, S. Primaquine loaded chitosan nanoparticles for liver targeting. Pharm. Nanotechnol. 2013, 1, 35–43. [Google Scholar] [CrossRef]
- Chadha, R.; Bhalla, Y.; Nandan, A.; Chadha, K.; Karan, M. Chrysin cocrystals: Characterization and evaluation. J. Pharm. Biomed. Anal. 2017, 134, 361–371. [Google Scholar] [CrossRef]
- Saptarshi, S.R.; Duschl, A.; Lopata, A.L. Interaction of nanoparticles with proteins: Relation to bio-reactivity of the nanoparticle. J. Nanobiotechnology 2013, 11, 26. [Google Scholar] [CrossRef]
- Cedervall, T.; Lynch, I.; Foy, M.; Berggård, T.; Donnelly, S.C.; Cagney, G.; Linse, S.; Dawson, K.A. Detailed identification of plasma proteins adsorbed on copolymer nanoparticles. Angew. Chem. Int. Ed. 2007, 46, 5754–5756. [Google Scholar] [CrossRef]
- Malachowski, T.; Hassel, A. Engineering nanoparticles to overcome immunological barriers for enhanced drug delivery. Eng. Regen. 2020, 1, 35–50. [Google Scholar] [CrossRef]
- Siafaka, P.I.; Üstündağ Okur, N.; Karavas, E.; Bikiaris, D.N. Surface modified multifunctional and stimuli responsive nanoparticles for drug targeting: Current status and uses. Int. J. Mol. Sci. 2016, 17, 1440. [Google Scholar] [CrossRef] [PubMed]
- Rafiei, P.; Haddadi, A. A robust systematic design: Optimization and preparation of polymeric nanoparticles of PLGA for docetaxel intravenous delivery. Mater. Sci. Eng. C 2019, 104, 109950. [Google Scholar] [CrossRef] [PubMed]
- Bilal, M.; Iqbal, H.M.; Adil, S.F.; Shaik, M.R.; Abdelgawad, A.; Hatshan, M.R.; Khan, M. Surface-coated magnetic nanostructured materials for robust bio-catalysis and biomedical applications-A review. J. Adv. Res. 2022, 38, 157–177. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, A.; Almotairy, A.R.Z.; Henidi, H.; Alshehri, O.Y.; Aldughaim, M.S. Nanoparticles as Drug Delivery Systems: A Review of the implication of nanoparticles’ physicochemical properties on responses in biological systems. Polymers 2023, 15, 1596. [Google Scholar] [CrossRef] [PubMed]
- Tavano, R.; Gabrielli, L.; Lubian, E.; Fedeli, C.; Visentin, S.; Polverino De Laureto, P.; Arrigoni, G.; Geffner-Smith, A.; Chen, F.; Simberg, D. C1q-mediated complement activation and C3 opsonization trigger recognition of stealth poly (2-methyl-2-oxazoline)-coated silica nanoparticles by human phagocytes. ACS Nano 2018, 12, 5834–5847. [Google Scholar] [CrossRef] [PubMed]
- Qie, Y.; Yuan, H.; Von Roemeling, C.A.; Chen, Y.; Liu, X.; Shih, K.D.; Knight, J.A.; Tun, H.W.; Wharen, R.E.; Jiang, W. Surface modification of nanoparticles enables selective evasion of phagocytic clearance by distinct macrophage phenotypes. Sci. Rep. 2016, 6, 26269. [Google Scholar] [CrossRef] [PubMed]
- Nosrati, H.; Javani, E.; Salehiabar, M.; Manjili, H.K.; Davaran, S.; Danafar, H. Biocompatibility and anticancer activity of L-phenyl alanine-coated iron oxide magnetic nanoparticles as potential chrysin delivery system. J. Mater. Res. 2018, 33, 1602–1611. [Google Scholar] [CrossRef]
- Jahangiri, S.; Amirkhani, L.; Akbarzadeh, A.; Hajimohammadi, R. Encapsulation of Doxorubicin and Chrysin on magnetic PCLPEG-PCL nanoparticles: Optimization of parameters and drug delivery evaluation. Int. J. Nano Dimens. 2021, 12, 380–392. [Google Scholar]
- Sundaresan, V.; Menon, J.U.; Rahimi, M.; Nguyen, K.T.; Wadajkar, A.S. Dual-responsive polymer-coated iron oxide nanoparticles for drug delivery and imaging applications. Int. J. Pharm. 2014, 466, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hauser, A.K.; Mathias, R.; Anderson, K.W.; Hilt, J.Z. The effects of synthesis method on the physical and chemical properties of dextran coated iron oxide nanoparticles. Mater. Chem. Phys. 2015, 160, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Ortega, F.; Delgado, Á.V.; Schneider, E.K.; Checa Fernández, B.; Iglesias, G. Magnetic nanoparticles coated with a thermosensitive polymer with hyperthermia properties. Polymers 2017, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Namikuchi, E.A.; Gaspar, R.D.; da Silva, D.S.; Raimundo, I.M.; Mazali, I.O. PEG size effect and its interaction with Fe3O4 nanoparticles synthesized by solvothermal method: Morphology and effect of pH on the stability. Nano Express 2021, 2, 020022. [Google Scholar] [CrossRef]
- Mohsin, M.H.; Khashan, K.S.; Sulaiman, G.M.; Mohammed, H.A.; Qureshi, K.A.; Aspatwar, A. A novel facile synthesis of metal nitride@ metal oxide (BN/Gd2O3) nanocomposite and their antibacterial and anticancer activities. Sci. Rep. 2023, 13, 22749. [Google Scholar] [CrossRef] [PubMed]
- Abu-Huwaij, R.; Al-Assaf, S.F.; Mousli, F.; Kutkut, M.S.; Al-Bashtawi, A. Perceptive review on properties of iron oxide nanoparticles and their antimicrobial and anticancer activity. Syst. Rev. Pharm. 2020, 11, 418–431. [Google Scholar]
- Suk, J.S.; Xu, Q.; Kim, N.; Hanes, J.; Ensign, L.M. PEGylation as a strategy for improving nanoparticle-based drug and gene delivery. Adv. Drug Deliv. Rev. 2016, 99, 28–51. [Google Scholar] [CrossRef]
- Dunn, S.E.; Brindley, A.; Davis, S.S.; Davies, M.C.; Illum, L. Polystyrene-poly (ethylene glycol)(PS-PEG2000) particles as model systems for site specific drug delivery. 2. The effect of PEG surface density on the in vitro cell interaction and in vivo biodistribution. Pharm. Res. 1994, 11, 1016–1022. [Google Scholar] [CrossRef]
- Uthaman, S.; Lee, S.J.; Cherukula, K.; Cho, C.-S.; Park, I.-K. Polysaccharide-coated magnetic nanoparticles for imaging and gene therapy. BioMed Res. Int. 2015, 2015, 959175. [Google Scholar] [CrossRef]
- Doh, K.-O.; Yeo, Y. Application of polysaccharides for surface modification of nanomedicines. Ther. Deliv. 2012, 3, 1447–1456. [Google Scholar] [CrossRef] [PubMed]
- Aibani, N.; Rai, R.; Patel, P.; Cuddihy, G.; Wasan, E.K. Chitosan nanoparticles at the biological interface: Implications for drug delivery. Pharmaceutics 2021, 13, 1686. [Google Scholar] [CrossRef] [PubMed]
| Sample | Fe3O4 NPs (mg) | Coating Agent | Chrysin (mg) | Ratio of Fe3O4 and Chrysin |
|---|---|---|---|---|
| Fe3O4@PEG250 | 500 | PEG | 250 | 1:0.5 |
| Fe3O4@PEG500 | 500 | PEG | 500 | 1:1 |
| Fe3O4@PEG1000 | 500 | PEG | 1000 | 1:2 |
| Fe3O4@Chitosan250 | 500 | Chitosan | 250 | 1:0.5 |
| Fe3O4@Chitosan500 | 500 | Chitosan | 500 | 1:1 |
| Fe3O4@Chitosan1000 | 500 | Chitosan | 1000 | 1:2 |
| Samples | 2-Theta Angle Values | Crystallite Size | ||||
|---|---|---|---|---|---|---|
| Fe3O4@PEG | 30.30° | 35.66° | 43.29° | 57.17° | 62.81° | 25.30 nm |
| Fe3O4@Chitosan | 30.37° | 35.74° | 43.45° | 57.5° | 62.83° | 25.10 nm |
| Sample | Crystallite Size (XRD) | Loading Efficiency (UV–Vis) |
|---|---|---|
| Fe3O4@PEG250 | 164 Å | 92% |
| Fe3O4@PEG500 | 168 Å | 96% |
| Fe3O4@PEG1000 | 153 Å | 97% |
| Fe3O4@Chtiosan250 | 208 Å | 45% |
| Fe3O4@Chtiosan500 | 192 Å | 50% |
| Fe3O4@Chtiosan1000 | 175 Å | 58% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karimova, A.; Hajizada, S.; Shirinova, H.; Nuriyeva, S.; Gahramanli, L.; Yusuf, M.M.; Bellucci, S.; Reissfelder, C.; Yagublu, V. Surface Modification Strategies for Chrysin-Loaded Iron Oxide Nanoparticles to Boost Their Anti-Tumor Efficacy in Human Colon Carcinoma Cells. J. Funct. Biomater. 2024, 15, 43. https://doi.org/10.3390/jfb15020043
Karimova A, Hajizada S, Shirinova H, Nuriyeva S, Gahramanli L, Yusuf MM, Bellucci S, Reissfelder C, Yagublu V. Surface Modification Strategies for Chrysin-Loaded Iron Oxide Nanoparticles to Boost Their Anti-Tumor Efficacy in Human Colon Carcinoma Cells. Journal of Functional Biomaterials. 2024; 15(2):43. https://doi.org/10.3390/jfb15020043
Chicago/Turabian StyleKarimova, Aynura, Sabina Hajizada, Habiba Shirinova, Sevinj Nuriyeva, Lala Gahramanli, Mohammed M. Yusuf, Stefano Bellucci, Christoph Reissfelder, and Vugar Yagublu. 2024. "Surface Modification Strategies for Chrysin-Loaded Iron Oxide Nanoparticles to Boost Their Anti-Tumor Efficacy in Human Colon Carcinoma Cells" Journal of Functional Biomaterials 15, no. 2: 43. https://doi.org/10.3390/jfb15020043
APA StyleKarimova, A., Hajizada, S., Shirinova, H., Nuriyeva, S., Gahramanli, L., Yusuf, M. M., Bellucci, S., Reissfelder, C., & Yagublu, V. (2024). Surface Modification Strategies for Chrysin-Loaded Iron Oxide Nanoparticles to Boost Their Anti-Tumor Efficacy in Human Colon Carcinoma Cells. Journal of Functional Biomaterials, 15(2), 43. https://doi.org/10.3390/jfb15020043








